Abstract
The late diagnosis of HIV in patients across the UK is an increasing problem. Here, we report on a retrospective case-notes audit carried out to assess the impact of the 2008 UK HIV testing guidelines on clinical practice and identify missed opportunities for HIV testing. The audit was carried out in 2010 and focussed on patients with newly diagnosed HIV at centres providing adult HIV services across the UK. Data were collected on 1,112 patients, of whom 52.2% were found to have a late HIV diagnosis as defined as a CD4 T lymphocyte count of <350 cells/mm3. Most patients (62.6%) were diagnosed in traditional settings, with a significant increase in those diagnosed with HIV in non-traditional settings (33%) compared with the 2003 audit (18.5%) (p<0.001). The most frequent indicator conditions that patients had experienced were chronic diarrhoea or weight loss, sexually transmitted infection, blood dyscrasia or lymphadenopathy. A quarter of patients were identified as having had a missed opportunity for earlier diagnosis. Based on our results, we suggest that HIV testing needs to continue to expand across clinical settings to reduce the number of patients living with undiagnosed HIV infection.
Key Words: HIV, testing, audit, missed opportunity
Introduction
In 2009, the number of people living with HIV in the UK reached an estimated 86,500 and a quarter of these were unaware of their infection.1 Late diagnosis (a CD4 count <350 cells/μl, or AIDS-defining illness at diagnosis)2 remains a problem; for example, in 2009, 52% of adults received a late diagnosis, a feature associated with increased mortality and morbidity, impaired response to highly active antiretroviral therapy (HAART) and increased cost to healthcare services.1,3,4 Indeed, the direct healthcare costs in the year following HIV diagnosis have been shown to be 200% higher for patients who presented late.5
A common feature of those presenting late is that they have often been seen with indicator diseases (ie diagnoses that should prompt the offering of an HIV test)6 in the recent past by healthcare professionals without the diagnosis of HIV having been made. These represent missed opportunities for testing.
In 2008, the UK National Guidelines for HIV Testing (www.bhiva.org.uk)6 were produced with the intention of increasing HIV testing in all healthcare settings as recommended by the Chief Medical and Chief Nursing Officers of the UK to reduce the proportion of individuals with undiagnosed HIV infection and reduce missed opportunities for testing.6 The guidelines were aimed at healthcare professionals who are not routinely involved in HIV care with the hope of expanding testing in non-traditional settings. It was recommended that widespread testing for HIV should occur where diagnosed HIV prevalence in the local population (ie Primary Care Trust and/or Local Authority) exceeds 2 per 1,000 population in particular, in all men and women registering in general practice, and all general medical admissions.
In 2010, as part of the national audit programme of the British HIV Association (BHIVA), we audited the impact that these guidelines have had on clinical practice. Here, we report one aspect of the audit which identified the clinical settings in which patients tested positive for HIV and the circumstances that had led to the test, including any missed opportunities for testing.
Methods
Clinical leads of all UK sites known to BHIVA as providers of adult HIV services were invited to complete a retrospective case-note review for consecutive patients aged 16 or over who attended between 1 August and 30 September 2010 for initial work-up after testing HIV positive, irrespective of the date the test was performed, up to a maximum of 40 per site.
Clinical information was then submitted electronically. This included demographic details (gender and age), date and circumstances of HIV testing (clinical setting and reasons for test), whether primary HIV infection was diagnosed, initial CD4 T lymphocyte and HIV plasma viral load, prior clinical history, including possible HIV indicator conditions6 since January 2008, clinical settings in which these were managed and whether they prompted the offer of an HIV test, previous negative HIV tests and the respondent's opinion as to whether there had been a missed opportunity to test the patient earlier than the actual first positive HIV test. Data regarding the clinical setting of the test were compared with the 2003 BHIVA audit,7 which performed a retrospective case-note review of new HIV diagnoses between January 2003 and March 2003.
Statistical analysis was performed using Microsoft Excel 2010. Odds ratio and 95% confidence intervals (CI) were calculated via the Newcombe-Wilson method without continuity correction using the CI Calculator v4 utility (http://vl.academicdirect.org/applied_statistics/binomial_distribution/ref/CIcalculator.xls).
Results
Data were collected on 1,112 patients from 140 sites. This represents 16.8% of the total new HIV diagnoses in 2009 as reported by the Health Protection Agency (HPA).8 In total, 782 (70.3%) were male, 604 (54.3%) were of white ethnicity and 305 (32.8%) African-Caribbean. Over half (n = 581, 52.2%) were found to have a late HIV diagnosis with a CD4 count of <350 cells/mm.3 Of the patients, 915 (82.2%) were registered with a general practitioner (GP) and at least one-third (366, 32.9%) had attended their GP during the two years before their diagnosis.
Clinical setting of HIV diagnosis
Table 1 shows the clinical areas where patients were found to have HIV, as compared with the results of the 2003 BHIVA audit.11 Most patients continue to have HIV diagnosed in traditional settings and mostly in genitourinary medicine (GUM) (n = 598, 53.8%). However, there was a significant increase in the proportion of patients who had HIV diagnosed in non-traditional settings from 18.5% to 33.3% (p<0.001, 95% CI 1.77, 2.66). In particular, there was a significant increase in new diagnoses made in general practice, with 116 cases (10.4%) being diagnosed in this setting compared with 4.8% in 2003 (p<0.001, 95% CI 1.6, 3.3). There was a small increase in the proportion of new HIV cases diagnosed as medical inpatients (including on acute admission units) and the main specialties where diagnoses were made were general and/or acute medicine, respiratory, infectious diseases, gastroenterology and haematology. A relatively low proportion of patients were found to have HIV in the outpatient setting (n = 79, 7.1%) with the main specialties being haematology, respiratory medicine, dermatology, gastroenterology and infectious diseases.
Table 1.
Comparison between 2003 and 2010 BHIVA audits, including baseline data and the clinical settings where the HIV diagnosis was made.
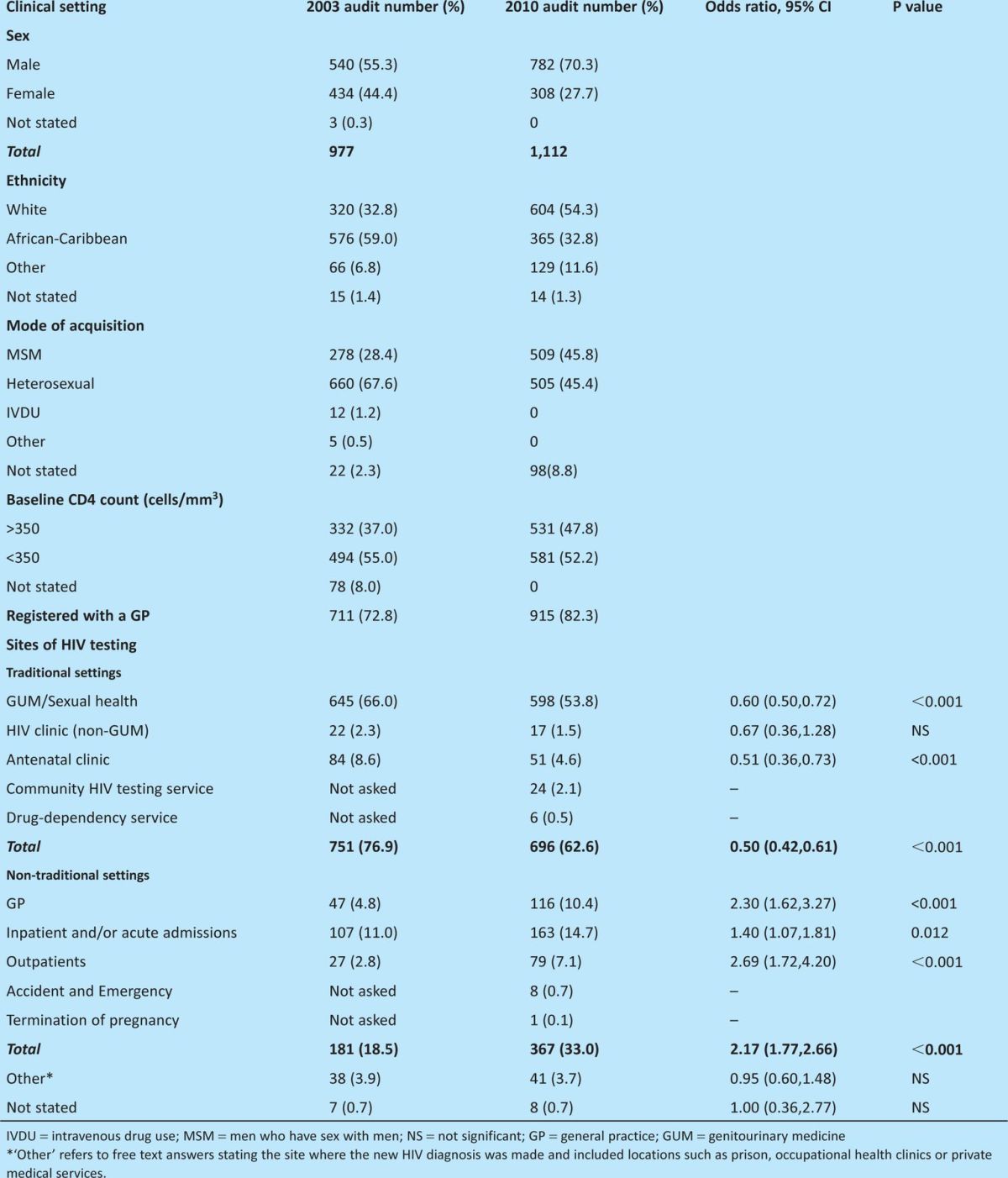
In a subanalysis, 78.3% (n = 126) of patients found to have HIV as an inpatient and/or acute admission had a CD4 count <350 cells/mm3 compared with 47.8% (n = 455) found to have HIV in a non-inpatient setting (including GUM), (OR 3.9, 95% CI 2.6, 5.8). When we compared those cases of HIV diagnosed in traditional settings (ie GUM, antenatal, drugs service or community HIV testing) to those diagnosed in a non-traditional setting (ie general practice, other outpatients, accident and emergency, inpatients and/or acute admissions, or termination of pregnancy), the proportion with a CD4 count <350 cells/mm3 was 71.7% (n = 258) in non-traditional and 42.1% (n = 291) in traditional settings (OR 3.5, 95% CI 2.6, 4.6).
Missed opportunities
There was a history of 632 indicator conditions from 410 (36.9%) patients between 2008 and first testing HIV positive (including presenting conditions that led to HIV diagnosis). Table 2 lists the most frequent indicator conditions experienced and whether an HIV test was known to have been offered. Of patients who had had an indicator condition, 112 were not offered a test at the time of the condition (27.3% of patients with indicator conditions and 10.1% of all patients). A high proportion of patients with chronic diarrhoea and weight loss (n = 42, 44.2%), lymphadenopathy (n = 12, 23.0%), blood dyscrasia (n = 19, 26.8%), mononucleosis-like illness (n = 19, 54.3%) and severe or recalcitrant seborrhoeic dermatitis (n = 8, 57.1%) were known not to have been offered a test and, even where testing was offered, in some cases this was after substantial delay. Although relatively few patients (n = 8) had cervical intraepithelial neoplasia (CIN) grade 2 or above, none of these were known to have been offered a test.
Table 2.
Indicator conditions occurring between January 2008 and the patient testing positive for HIV.
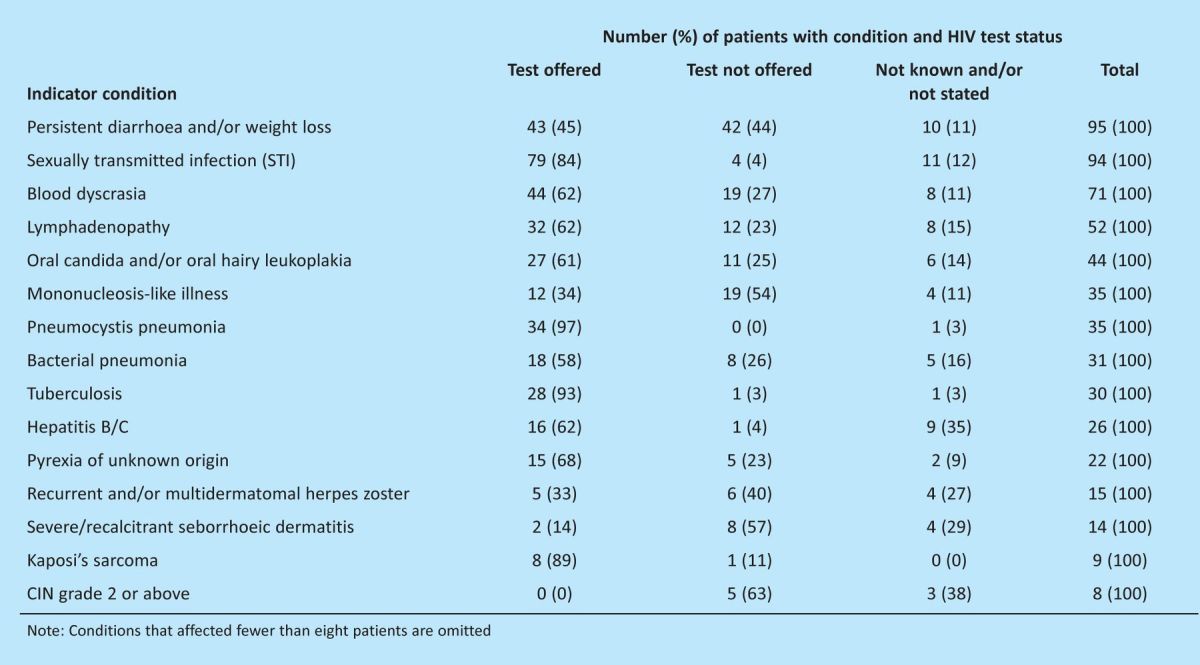
On review of the case notes, respondents assessed a quarter of patients (n = 280, 25.2%) as having had a missed opportunity for earlier testing at some point in the past. Among patients assessed as having a missed opportunity, 71.1% (n = 199) had a CD4 count <350 cells/mm3 compared with 45.9% (n = 382) of those not assessed as having a missed opportunity (OR 2.9, 95% CI 2.2, 3.9).
Discussion
The 2010 BHIVA audit provided the first national data regarding the impact of the 2008 National HIV Testing guidelines on clinical practice in the UK.
It is encouraging that the proportion of individuals found to have HIV in non-traditional settings has significantly increased. In particular, the number of new diagnoses identified through general practice has more than doubled, probably reflecting increased testing. Such testing in this setting is essential as, for many patients, this will be their initial contact with healthcare, providing an ideal opportunity for earlier diagnosis. In contrast, it is of concern that relatively few new diagnoses were made in areas such as medical outpatients, inpatients and termination of pregnancy services, probably reflecting low levels of testing. Several studies have shown that offering testing in acute medical admissions departments, for example, is feasible and highly acceptable to patients.9,10 These findings have been echoed in other clinical areas, such as accident and emergency, dermatology and colposcopy.9, 11,12
Missed opportunities for testing remain a problem, with at least 112 cases identified in the audit. The commonest missed presentations (chronic diarrhoea, weight loss, blood dyscrasias and lymphadenopathy) are conditions that are frequently encountered in general practice and medical outpatients. Missed opportunities not only lead to late diagnoses and associated complications (ie increased morbidity and mortality, impaired response to HAART and increased healthcare costs1,3,4), but also have public health implications in terms of onward transmission of HIV infection. Increased HIV testing in specialties such as gastroenterology and haematology, as well as further increased testing in general practice, provide an important opportunity for earlier diagnosis.
Our data demonstrate that patients tested in a service that adopts a ‘routine offer and recommend’ policy towards HIV testing (such as that widely used in GUM and antenatal settings), have higher CD4 T-lymphocyte counts at diagnosis than those diagnosed in other settings. In areas with a high prevalence of HIV infection (>2 per 1,000) (Figure 1), national recommendations are to offer HIV testing routinely in all general medical admissions and all new patients registering with a GP.6 Clinicians working in areas with lower prevalence should adhere to recommendations for HIV testing, in particular offering testing to those presenting with indicator conditions.
Fig 1.
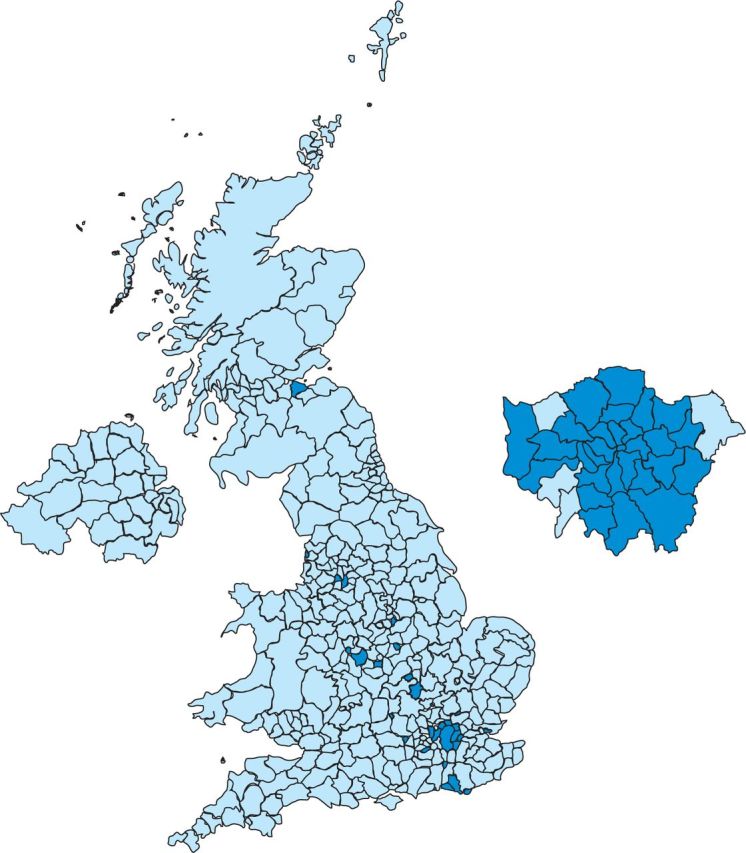
Diagnosed HIV prevalence per 1,000 population aged 15–59 years, by local authority of residence: United Kingdom, 2010. Darker blue shading represents HIV prevalence > 2 per 1000 (HPA 2011 HIV Report).
Since the audit, the National Institute for Health and Clinical Excellence has published guidance on increasing the uptake of HIV testing among men who have sex with men13 and among African-Caribbeans in England.14 Implementation of this guidance, which reflects and expands on the 2008 national HIV testing guidelines, would have a substantial impact on the problems that we have identified. Based on our findings, clinicians and commissioners should prioritise increasing use of HIV testing in general practice, medical inpatient and outpatient settings, especially in gastroenterology and haematology, and on improving pathways to enable patients who test positive to be seen rapidly by a specialist.15
Acknowledgements
Members of the BHIVA audit and standards sub-committee: C Ball (to 2011), G Brook (to 2011), J Catalan, D Churchill, A DeRuiter, M Desai (from 2011), S Edwards (from 2011), S Ellis, K Foster, A Freedman, L Garvey (to 2010), P Gupta, M Johnson (to 2010), A Judd (from 2011), E Monteiro, C O'Mahony (to 2010), D Ogden (from 2011), E Ong, K Orton, R Pebody, F Post, A Rodger (from 2011), C Sabin, A Schwenk, A Sullivan, H Veerakathy, R Weston (to 2011), E Wilkins, D Wilson, and M Yeomans (to 2010). Thanks to clinicians who completed the survey and submitted data.
Competing interests
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work and no financial relationships with any organisations that might have an interest in the submitted work in the previous three years. EO co-chaired the UK National HIV Testing Guidelines 2008 writing committee. SE and HC have no competing interests.
References
- 1.Health Protection Agency. HIV in the United Kingdom: 2010 Report 2010. www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1287145367237 [Accessed 26 July 2012]
- 2.Antinori A, Coenen T, Costagiola D, et al. Late presentation of HIV: a consensus definition. HIV Med 2011;12:61–4 10.1111/j.1468-1293.2010.00857.x [DOI] [PubMed] [Google Scholar]
- 3.Moreno S, Mocroft A, Monforte A. Medical and societal consequences of late presentation. Antivir Ther 2010;15(Suppl.1)9–15 10.3851/IMP1523 [DOI] [PubMed] [Google Scholar]
- 4.Burns FM, Johnson AM, Nazroo J, et al. SONHIA Collaboration Group. Missed opportunities for earlier HIV diagnosis within primary and secondary healthcare settings in the UK. AIDS 2008;1:115–22 [DOI] [PubMed] [Google Scholar]
- 5.Krentz HB, Auld MC, Gill MJ. The high cost of healthcare for patients who present late (CD4<200 cells/μl) with HIV infection. HIV Med 2004;5:93–8 [DOI] [PubMed] [Google Scholar]
- 6.Palfreeman A, Fisher M, Ong E. Testing for HIV: concise guidance. Clin Med 2009;9:471–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.2003 British HIV Association audit. 2003. www.bhiva.org/documents/ClinicalAudit/FindingsandReports/newdiag_preliminary_results.pdf [Accessed 26 July 2012]
- 8.Health Protection Agency. HIV in the United Kingdom: 2009 report 2009. www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1259151891866 [Accessed 26 July 2012]
- 9.Rayment M, Thornton A, Wolz T, et al. HIV testing in non-traditional settings – the HINTS study. HIV Med 2011;12(S1)O7 [Google Scholar]
- 10.Ellis S, Graham L, Price DA, Ong ELC. Offering HIV testing in an acute medical admissions unit in Newcastle upon Tyne. Clin Med 2011;11:541–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rayment M, Ogdens S, Raben D, et al. Routine testing in colposcopy clinic – acceptable and sustainable. HIV Med 2011;12(S1)P133 [Google Scholar]
- 12.Dhairyawan R, Millett D, Creighton S. Routine HIV testing in colposcopy. HIV Med 2011;12(S1)P138. [DOI] [PubMed] [Google Scholar]
- 13. NICE guidance, 2011. Increasing the uptake of HIV testing to reduce undiagnosed infection and prevent transmission among men who have sex with men (PH34). ( http://egap.evidence.nhs.uk/ph34) [Accessed 26 July 2012]
- 14. NICE guidance, 2011. Increasing the uptake of HIV testing to reduce undiagnosed infection and prevent transmission among black African communities living in England (PH33). ( http://egap.evidence.nhs.uk/ph33) [Accessed 26 July 2012]
- 15.Health Protection Agency. Time to test for HIV: expanding HIV testing in healthcare and community services in England. London: HPA, 2011 [Google Scholar]


