ABSTRACT
This study assesses NHS doctors’ experiences of paternity leave and evaluates whether practices have changed since the introduction of additional paternity leave (APL) in April 2011. An anonymised online survey designed to discover experiences and uptake of APL and ordinary paternity leave (OPL) was distributed to all members of the London Deanery Synapse® network. In total, 364 fathers responded. Their seniority ranged from foundation trainees to consultants. Following the formal introduction of OPL in 2003, the number of fathers taking any paternity leave increased (from 50% to 95.6%). The majority of respondents (76.7%) felt well supported by their employer. Since the introduction of APL, 3% of respondents took additional leave. Reasons for the low uptake of APL included the impracticalities of the law, poor awareness and perceived attitudes and implications for training. Problems with OPL included the inadequate provision of cover and difficulties in timing the leave appropriately.
KEY WORDS: Additional paternity leave, ordinary paternity leave
Introduction
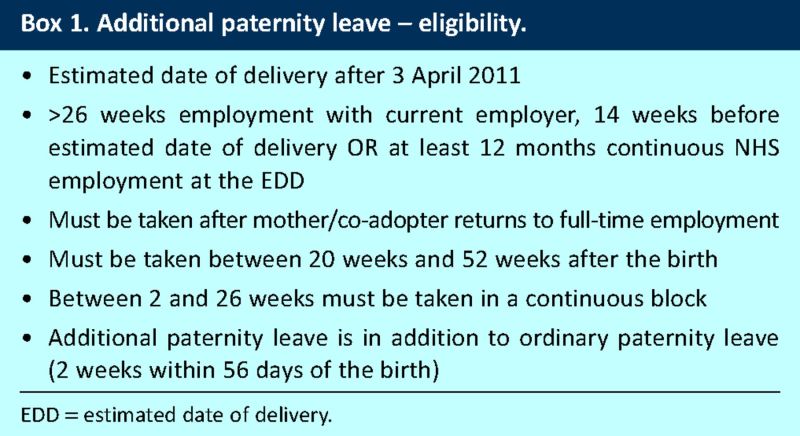
On 3 April 2011, paternity laws within the UK were changed with the introduction of additional paternity leave (APL) (Box 1).1 Up to 26 weeks of leave can now be taken by a father if his partner returns to full-time employment. APL can be taken between 20 and 52 weeks after the child's birth. If this occurs while the mother would still be eligible for statutory maternity pay had she not returned to work, this leave is paid at £135.45 per week. It is otherwise unpaid. The APL allowance is in addition to ordinary paternity leave (OPL), which is 2 weeks to be taken within 56 days of the birth (itself only introduced on 6 April 2003). Harriet Harman, former Minister for Women and Equality, stated that this change would give families ‘radically more choice and flexibility in how they balance work and care of children’.2
Box 1. Additional paternity leave – eligibility.
APL was met with scepticism. The economic feasibility was questioned and even advocates predicted the maximum uptake would be less than 6%.3 Gender stereotypes and men's inability to breastfeed were some of the reasons proffered as to why this policy was unlikely to be widely utilised.4
Use of APL among doctors presents even more complex issues. Many fathers work within training programs. On-call commitments that must fit within a European Working Time Directive compliant rota make internal cover difficult, if not impossible. The high cost of locums renders additional staffing expensive. Human resources departments are not directly involved in arranging specialty training and as such are often unable to provide information regarding changes to training requirements following extended leave.
Many practical hurdles are encountered even in the implementation of OPL within the framework of medical training. There is a lack of clarity regarding qualification for leave, especially among junior doctors who frequently move between different trusts. It is uncertain whether there is an obligation by the prospective father to give specific dates in advance, given the unpredictable nature of birth. Several trusts do not have a clearly accessible paternity policy.
We surveyed the experiences of fathers in both training and non-training posts across specialties who were members of the Synapse® Network (London Deanery). Uptake and attitudes towards APL were assessed, alongside uptake and duration of OPL taken.
Method
An online survey was distributed to all members of the London Deanery Synapse® network. A message directing the survey to doctors who became fathers while working for the NHS and detailing the aims of the project with a link to the survey was sent. The survey questions were framed in a retrospective fashion, using a multiple-choice format. Where more qualitative data were sought, the survey questions were designed to allow more than one response and provided a text box for alternative answers and comments.
The following information was collected: job title/stage of career, specialty, month and year of birth of youngest child, type and duration of leave taken for this birth, interest in and feasibility of taking APL if it had been available, awareness of APL if the birth of the youngest child was after the introduction of APL, attitude of employer towards OPL and hours on return to work.
Results
Demographics of respondents
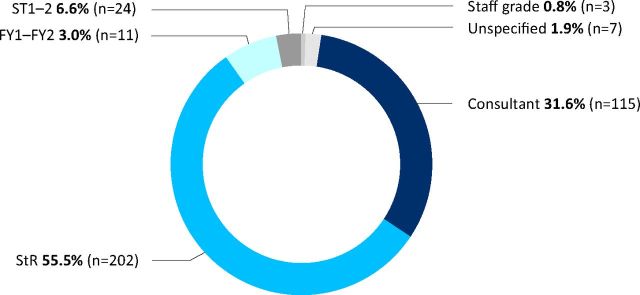
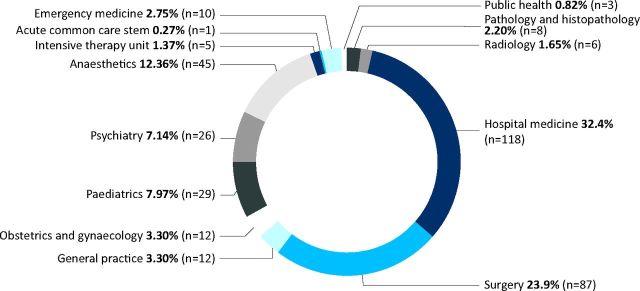
In total, 364 fathers responded to the survey. Respondents included consultants (31.8%), specialist registrars (55.7%) and doctors in more junior training posts (9.7%) (Fig 1). Doctors from a variety of specialties responded (Fig 2). 25 fathers (6.9%) declared that their most recent child was born before the introduction of OPL in 2003. The majority of respondents (56.1%, n = 203) reported that their most recent child had been born after the introduction of OPL but before the introduction of APL (births April 2003 to April 2011). For just over one-third (37.0%, n = 134), the birth of their most recent child occurred following the introduction of APL (after April 2011).
Fig 1.
Stage of training of respondents. FY = foundation year; ST = specialty trainee; StR = specialist registrar.
Fig 2.
Current specialty of respondents.
Duration of paternity leave
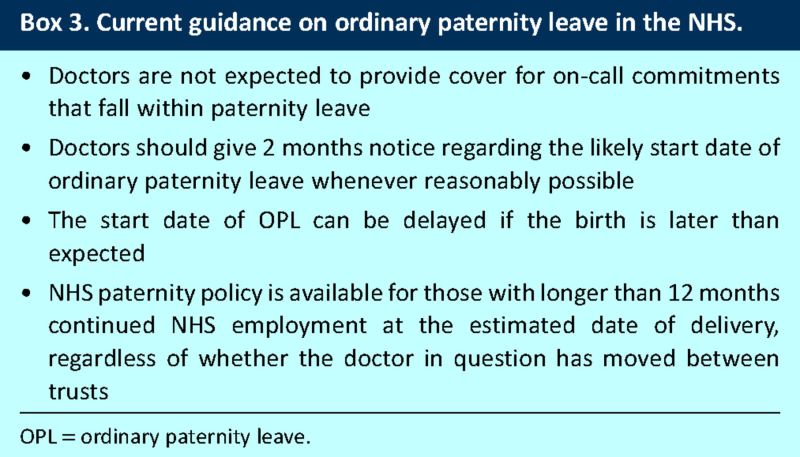
Overall, the majority of doctors who responded (92.3%) took some leave following the birth of their most recent child; over three-quarters (77.4%) took 2 weeks, 13.3% (n = 48) took less than 2 weeks and a small number (2.2%, n = 8) took more than 2 weeks. Table 1 compares the different patterns of paternity leave taken, categorised by the legal availability of OPL and APL. After the formal introduction of OPL in 2003, substantially more doctors took some leave following the birth of a child (95.6%, n = 323/338, an increase from 50%, n = 13/26).
Table 1.
Amount of leave taken by doctors categorised by legal entitlement for ordinary and/or additional paternity leave.
Uptake and feasibility of additional paternity leave
Of respondents who had children after April 2011, only 3% (n = 4) took APL. One of these commented that he had taken leave in addition to OPL, but had not formally applied for APL. Of respondents who had children before April 2011, 50% stated they would have considered APL were it available. All groups were asked to comment on reasons why APL might not be feasible: 31.5% (n = 114) reported that their partner did not return to full-time employment, 35.1% (n = 127) reported that their partner was breastfeeding and/or was the intended primary carer, 20.7% (n = 75) cited financial reasons, 23.2% (n = 84) reported concerns regarding how their training would be affected, and 21.5% (n = 78) cited concerns that the decision to take extended leave would be perceived negatively by colleagues.
Awareness of additional paternity leave
Over one-third (38.1%, n = 51) of respondents who became fathers after April 2011 were not aware of the APL policy. Only 9.7% (n = 13) were explicitly made aware of the policy by their employer.
Attitudes experienced when taking OPL and working hours on return
Almost three-quarters (74.9%, n = 271) of all respondents felt supported by their employer with regard to choice of dates and the duration of OPL. Men who had their most recent child after the introduction of OPL (April 2003 onwards) clearly perceived an increased level of support. Of those who had their most recent child before April 2003, only 44% (n = 11) felt supported. Of those who had their most recent child between April 2003 and April 2011, 80.7% (n = 168) felt supported. Of those who had their most recent child after April 2011, 72.4% (n = 97) felt supported. Very few respondents (2.22%, n = 8) returned to work on a less than full-time basis.
Limitations of study design
Recruitment bias may have influenced the results of this study. Ideally, we would have liked to include the paternity leave patterns of all doctors who have taken paternity leave in recent years while working for the London Deanery. Unfortunately this information was not available because of data protection laws. The study does not ascertain the amount of annual leave taken by fathers following the birth of a child, either in addition to or instead of OPL.
Discussion
The high uptake of OPL among recent fathers is encouraging. Paternity leave has been linked to increased paternal involvement later in life5 and increased rates of breastfeeding.6 However, less than 3% of doctors who responded have made use of the APL entitlement since its introduction. This proportion is roughly half of government predictions of likely uptake. By contrast, 50% of doctors who became fathers before April 2011 reported that they would have taken APL were it available.
A number of factors are likely to contribute to this discrepancy. First, the introduction of APL has not been well publicised. In our study, 38.1% of men who became fathers after April 2011 were unaware of the policy and less than 10% were told about APL by their employer. Second, our results also demonstrate practical deterrents: 31.5% of fathers surveyed stated that their partners did not return to full-time employment and a similar proportion (35.1%) replied that their partners remained the primary carer and/or were breastfeeding. Financial reasons were a concern for 20.7%, 23.2% reported concerns regarding how APL would impact their training and 21.5% anticipated negative perceptions from colleagues.
Lack of flexibility as to when the leave must be taken (from 20 weeks after the birth) was also noted. One father commented ‘2 weeks is clearly too short, but the new proposal is additionally nonsensical. Ideally, a father would want to take paternity leave in the first few weeks to support mum . . . my wife had a C-section with each of our three so she needed me there early…this ideally required a 4–6 week support period at least’.
Early paternal support is particularly important in the UK where it is relatively rare for new parents to live within extended family units.7 Fathers may also opt to take annual leave to extend their early availability; at present, the National Office of Statistics does not have information regarding how prevalent this practice is. Even the well-established parental leave policies of Nordic countries are generally designed such that the majority of leave is taken with one parent remaining at work. It is recognised, however, that Scandinavian parents often opt to take annual leave or, when available, sabbatical while the other parent is on parental leave.8
Several fathers cited the financial implications of APL as a deterrent. Fathers are known to struggle with the financial implications of even OPL when they are offered only statutory pay, with some choosing to take annual leave instead.9,10 Hence it is unsurprising that largely unpaid APL is often not an option.
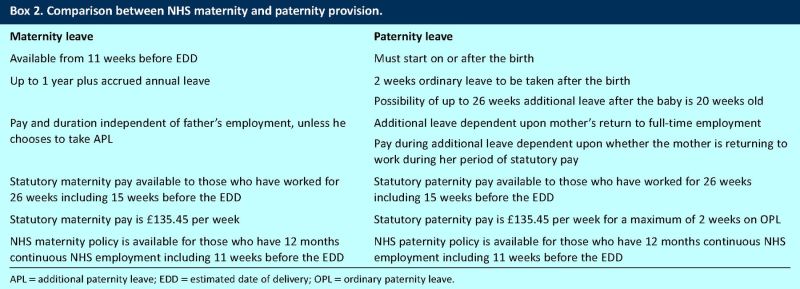
The NHS is currently one of the UK's largest equal opportunities employers; perceptions (correct or otherwise) that it is unfeasible to take legally entitled leave are worrying. One medical consultant commented ‘busy department, not possible’ when asked about additional leave and several others specifically mentioned staffing shortages. Female consultants in equally busy departments, however, routinely take substantially more than 2 weeks maternity leave. NHS maternity policy allows up to 12 months leave (and annual leave accrued).11–13 In contrast to APL, maternity leave is not dependent on the father's return to full-time employment (Box 2). Adequate maternity leave is now expected, regardless of economic or workplace needs.
Box 2. Comparison between NHS maternity and paternity provision.
It is difficult to ascertain whether the perceived negative career implications of APL highlighted by this survey are justified. Women who historically are responsible for the bulk of child rearing are indeed less likely to achieve top positions in the majority of industries, including hospital consultant posts.14 Many women take career breaks for several years, however, with a substantial proportion never returning to the same post, so it is hard to draw a parallel. Most of the data regarding extended paternity leave are from Nordic populations. One study of Norwegian fathers cited perceived negativity as a reason as to why leave was not taken in full.15 In practice, only 10% of the study population did, in fact, experience negative comments about their chosen leave. One American study suggested that fathers who were offered paternity leave were in fact more loyal to the company thereafter; however this involved substantially shorter periods of leave.16 Little is known regarding the long-term impact of extended paternity leave on career progression.
It is known that paternity leave patterns are influenced by the wishes of mothers,17 and so the opinion of mothers regarding APL, and indeed their awareness of the policy, are likely to influence uptake. Within this study group, less than 10% fathers were made aware of APL by their employer; it is not routinely mentioned in trust maternity policies and it is possible many female employees have not considered APL. Studies also suggest that the majority of new mothers, when possible, prefer to return to work part time, which renders the current model of APL unavailable.18
The experiences of doctors who took OPL were generally positive, particularly in recent years. Several respondents commended the NHS for paying most fathers full pay. A number of doctors had been particularly well supported following difficult personal circumstances. One foundation year trainee was ‘encouraged [to take] time off although [he] hadn't been working long enough to qualify officially’.
Sadly, positive experiences were not unanimous and a minority of doctors were either pressured to forgo paternity leave or made to feel a nuisance for taking it. One in eight felt their employers were unsupportive of their paternity plans, some reporting sarcastic and unhelpful comments from seniors. Although such experiences were not common, when they occurred they caused bad feeling. One psychiatry trainee whose partner gave birth in 2011 reported that ‘despite 6 months’ notice [I was] placed on nights, eventually had to get BMA involved and faith in current employer is very low, shambolic to treat employees in this manner!’
The issue of provision of cover during OPL was also raised. Several respondents specifically commented that they were expected to cover on-call commitments, including weekends, that fell within paternity leave. One anaesthetic StR (most recent child born in 2009) said he ‘only got 2 weeks off by working a week locum cover at employer's hospital for free!’ Some doctors reported inadequate cover during their absence; one foundation trainee said of his post: ‘Very busy. No locum provided so felt guilty leaving rest of team to cope’.
We addressed the issue of whether doctors were expected to cover on-call commitments during paternity leave with the BMA. They confirmed that the employer was responsible for providing cover and that there was no obligation to make up the shifts at a later date.
The issue of timing the onset of leave with the birth was also problematic. ‘I was responsible for the last minute swaps required when the birth was predictably unpredictable!’ said one surgical StR, whose most recent baby was born in 2011. Another father remarked that the birth occurred during the last day of his paternity leave. Again, we looked to the BMA who responded that there was no legal obligation for a father to begin OPL before birth. In fact, the BMA website specifies that paternity leave cannot start before the birth of the child.
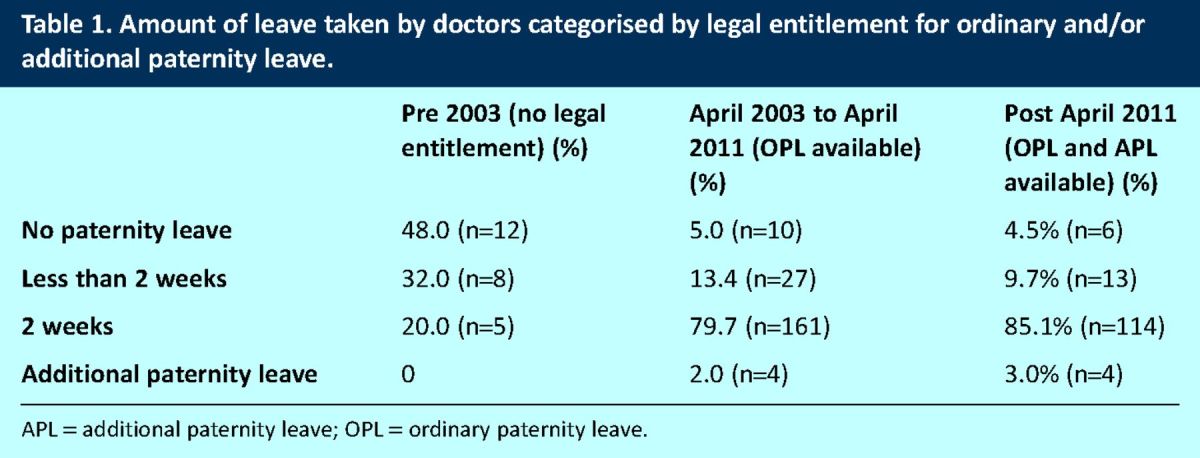
The eligibility for and calculation of paternity pay (both ordinary and additional) for NHS doctors is complex, especially for doctors within training posts. Doctors who have more than 12 months continuous NHS employment at the estimated date of delivery are entitled to NHS paternity pay, which is 2 weeks of full pay during OPL (Box 3). This is regardless of when they most recently changed trust. Doctors who have not worked the full year but have worked more than 26 weeks within the same trust, including 15 weeks before the estimated delivery date (EDD), qualify for statutory paternity pay (£135.45 per week).13 APL is available for those who have either had 12 months continuous NHS employment at the EDD or worked for 26 weeks with the same employer at 14 weeks before the EDD, in addition to the eligibility criteria discussed earlier. Statutory paternity pay within APL is only available if the leave is taken within the time period that the mother would still receive statutory maternity pay were she to have remained on leave (prior to 39 weeks post birth) and the father has been within the same trust 26 weeks at 14 weeks prior to the EDD.
Box 3. Current guidance on ordinary paternity leave in the NHS.
Taking more than 3 months of either maternity leave or APL increases duration of training, with Certificates of Completion of Training (CCT) dates to be changed according to the duration of leave taken.13 In addition, while parents who take more than 2 weeks maternity or paternity leave can expect to return to a training position, they cannot be guaranteed the same rotation.
A study of female doctors who qualified in the 1970s and 1980s suggests that the support of maternity leave is itself recent. New mothers in this period were often unable to take maternity leave because of short contracts and sometimes were obliged to resign or pay for their own locum cover.19 Paternity leave of any form has only been a legal requirement since April 2003. The change from no leave to the potential for up to 6 months has occurred within less than a decade; perhaps it will take another decade, or more, for paternity leave to be seen with acceptance of maternity leave and for changes in childcare provision between the sexes to be equalised. It is likely that the biological necessity of a new mother taking at least some time off paves the way for her to be the main carer in most families. It is important, however, that NHS employees feel supported however they chose to divide legally entitled leave. Indeed, uptake of APL might prove beneficial for the NHS which has an increasingly female-dominated work force. The publication of an NHS-wide parental leave policy including advice on dealing with common queries highlighted by this survey would be a useful guide for doctors and their employers.
References
- 1.UK Government. Paternity Leave and Pay , 2012. www.direct.gov.uk/en/Parents/Moneyandworkentitlements/WorkAndFamilies/Paternityrightsintheworkplace/DG_190788 [Accessed 6 June 2013]. [Google Scholar]
- 2.Churcher J. Paternity leave rights to be extended. The Independent 15 September 2009. www.independent.co.uk/news/uk/politics/paternity-leave-rights-to-be-extended-1787733.html [Accessed 6 June 2013]. [Google Scholar]
- 3.Department for Business Innovation and Skills. Final impact assessment: additional paternity leave and pay. London: BIS, 2010. www.bis.gov.uk/files/file54236.pdf [Accessed 6 June 2013]. [Google Scholar]
- 4.Smile S. Q&A: paternity leave, The Guardian 5 October 2006. www.guardian.co.uk/business/2006/oct/05/workingparents.familyfinance [Accessed 6 June 2013]. [Google Scholar]
- 5.Nepomnysaschy L, Waldfogal J. Paternity leave and fathers’ involvement with their young children: evidence from the American ECLS-B. Community Work Fam 2007;10:427–53. 10.1080/13668800701575077 [DOI] [Google Scholar]
- 6.Flacking R, Dykes F, Ewald U. The influence of fathers’ socioeconomic status and paternity leave on breastfeeding duration: a population-based cohort study. Scand J Public Health 2010;38:337–43. 10.1177/1403494810362002 [DOI] [PubMed] [Google Scholar]
- 7.Office for National Statistics , Dunstan S. (ed). General lifestyle survey overview: a report on the 2009 general lifestyle survey. London: ONS, 2011. www.ons.gov.uk/ons/rel/ghs/general-lifestyle-survey/2009-report/overview-report-2009.pdf [Accessed 6 June 2012]. [Google Scholar]
- 8.Rostgaard T. Setting time aside for the father – father's leave in Scandinavia. Community Work Fam 2002;5:343–64. 10.1080/1366880022000041810 [DOI] [Google Scholar]
- 9.Himmelweit S. The right to request flexible working: a very British approach to gender (in)equality. Aust Bull Labour 2007;33:246–63. [Google Scholar]
- 10.Kelly J. The politics of paternity leave. BBC News, 2012. www.bbc.co.uk/news/magazine-11086630 [Accessed 17 November 2012]. [Google Scholar]
- 11.British Medical Association Junior Doctors Committee Junior Doctor's Handbook, 2012. bma.org.uk/practical-support-at-work/contracts/juniors-contracts/juniors-handbook [Accessed 14 June 2012]. [Google Scholar]
- 12.British Medical Association Maternity leave (for NHS medical staff), 2011. bma.org.uk/-/media/Files/PDFs/Practical%20advice%20at%20work/Working%20parents/maternity%20leave%20guidance%202011.pdf [Accessed 5 June 2013]. [Google Scholar]
- 13.NHS Employers Maternity issues for doctors in training, 2010. www.nhsemployers.org/Aboutus/Publications/Pages/MaternityIssuesForDoctorsInTraining.aspx [Accessed 5 June 2013]. [Google Scholar]
- 14.Bloor K, Freemantle N, Maynard A. Gender and variation in activity rates of hospital consultants. J R Soc Med;101:27–33. 10.1258/jrsm.2007.070424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lami-Taskula J. Nordic men on parental leave: can the welfare state change gender relations? In: Ellingsater LA, Leira A. (eds) Politicising parenthood in Scandinavia. Bristol: The Policy Press, 2006:79–100. [Google Scholar]
- 16.Grover S, Crooker K. Who appreciates family-responsive human resource politics: the impact of family-friendly policies on the organizational attachment of parents and non-parent. Pers Psychol 1995;48:271–88. 10.1111/j.1744-6570.1995.tb01757.x [DOI] [Google Scholar]
- 17.McKay L, Doucet A. ‘Without taking away her leave’: a Canadian case study of couples’ decisions on fathers’ use of paid parental leave. Fathering 2010;8:300–20. 10.3149/fth.0803.300 [DOI] [Google Scholar]
- 18.Morris L. The experiences of women returning to work after maternity leave within the UK: a summary of survey results, 2008. www.nct.org.uk/sites/default/files/related_documents/ReturningToWork-Survey.pdf [Accessed 10 December 2012]. [Google Scholar]
- 19.Warren VJ, Wakeford RE. ‘We’d like to have a family’ – young women doctors’ opinions of maternity leave and part-time training. J R Soc Med 1989;82:528–31. [DOI] [PMC free article] [PubMed] [Google Scholar]