ABSTRACT
Asthma is a heterogeneous condition with multiple phenotypes that respond to treatments in different ways. Allergic asthma is an important phenotype and although currently available treatments are effective, about 5% of affected patients have severe, treatment-refractory disease. Despite advances in our understanding of the disease, there remains an unmet need in this group of patients. The most recent and significant advance in treatment has been anti-immunoglobulin E (IgE) therapy, which improves symptoms and quality of life in patients with severe allergic asthma. Clinical trials are ongoing with novel biologic agents that demonstrate potential efficacy; determining the subsets of patients for which they are suitable will be crucial to ensure cost effectiveness. Personalised medicine and targeted therapies may hold the key to long-term control in this group of patients.
KEY WORDS: Allergic asthma, phenotype, Th2, treatment
Background
More than 300 million people have asthma globally, and this figure is expected to increase by a further 100 million by 2025.1 More than 5 million people in the UK are receiving medication for asthma, with total costs to the National Health Service (NHS) of about £1 billion per year, which equates to about 1% of the total NHS budget.2 Although most cases of asthma have the potential to be well controlled using inhaled corticosteroids (ICS) and long-acting β2 agonists (LABAs), about 5% of patients have severe, refractory disease.3 Patients in this group are often difficult to treat, require significant attention and utilise 50% of the available NHS resources for asthma. Despite significant advances in therapy in recent years, almost 80,000 hospital admissions and 1,200 deaths each year in the UK are directly attributable to asthma.2
What is allergic asthma?
Asthma represents a spectrum of disorders produced by a variety of overlapping clinical phenotypes and characterised by variable airways obstruction and inflammation. The main features include hyper-responsiveness of the airways to a wide variety of exogenous and endogenous stimuli and a specific pattern of mucosal inflammation involving activated mast cells, eosinophils and T lymphocytes. This is associated with altered responses of structural cells in the airway, including epithelial cells.4
Asthma can be divided into intrinsic asthma (non-atopic), extrinsic asthma (atopic or allergic) and occupational asthma. Allergic asthma is the most common form, is associated with atopy and usually develops in childhood or early adulthood. Atopy is defined as a genetic predisposition to produce immunoglobulin E (IgE) against common environmental aeroallergens such as dust mites, moulds, pollens and animal dander. About 80% of patients with asthma are atopic compared with 30% of the general population.5
Individuals with allergic asthma are initially sensitised to allergens and subsequently develop symptoms on re-exposure.6 Immunoglobulin E binds to the surface of mast cells and basophils and is cross-linked by allergens, which leads to the release of mediators such as histamine, prostaglandins, leukotrienes, chemokines and cytokines.7 These mediators are responsible for many of the features associated with asthma, including bronchoconstriction. Continued expression of these mediators leads to an inflammatory response, which manifests as persistent symptoms, airway hyper-responsiveness and bronchospasm.
Current treatment for allergic asthma
The treatment pathway for asthma is set out in the joint guidelines of the British Thoracic Society (BTS) and Scottish Intercollegiate Guidelines Network (SIGN).8 Current therapeutic options initially focus on bronchodilators and anti-inflammatory inhaled corticosteroids (ICS). If symptoms persist, a trial of other therapies such as a leukotriene receptor antagonist (LTRA) or oral theophylline may be beneficial alongside increasing doses of ICS. At this stage, some patients with asthma may require maintenance systemic corticosteroids to control or partially control their symptoms. These patients experience decreased quality of life, miss a substantial number of days from work or school and are at risk from the many and potentially serious side effects of long-term corticosteroid therapy. In patients with severe allergic asthma, the current options include anti-IgE therapy, steroid-sparing immunosuppressive drugs (eg methotrexate, ciclosporin, mycophenolate mofetil and azathioprine) or participating in trials with novel biological agents.
Inhaled corticosteroids, long-acting β2 agonists and muscarinic receptor antagonists
Inhalers combining ICS and LABA and ‘as-required’ use of an additional short-acting β2 agonist (SABA) are commonly prescribed to achieve asthma control. Previous studies have noted increased mortality when LABAs are used in isolation,9 but the addition of LABAs to lower doses of ICS is associated with greater anti-inflammatory activity and improved asthma control.9,10
Recently, the Single inhaler Maintenance And Reliever Therapy (SMART) approach has been introduced for patients at step 3 of the BTS/SIGN guideline.8 Patients are able to use the budesonide–formoterol combination according to symptoms, potentially resulting in a reduction in the risk of exacerbations and lower overall exposure to ICS.11
Muscarinic receptor antagonists are widely used in patients with chronic obstructive pulmonary disease (COPD) but have been less popular in patients with asthma, largely due to their slower onset of action as a reliever medication compared with inhaled β2 agonists. Recent trials in patients with poorly controlled asthma receiving ICS/LABA found that the addition of tiotropium, a long-acting muscarinic receptor antagonist (LAMA), was associated with modest improvements in forced expiratory volume in one second (FEV1) and significantly increased time to a first exacerbation, with an overall 21% reduction in the risk of a severe exacerbation.12
Success with SMART therapy and muscarinic receptor antagonists requires careful selection of suitable patients and monitored trials of therapy to assess response. A number of different inhaler combinations in development may benefit patients with allergic asthma, including LABA/LAMA and once-daily ICS/LABA combinations. However, the exact place for these new inhalers in the current stepwise approach is unclear at present.
Anti-IgE therapy
Omalizumab is a recombinant humanised monoclonal anti-IgE antibody that was licensed as an add-on therapy to improve asthma control in patients with severe allergic asthma. It binds to free IgE in the serum, forming small biologically inert IgE–anti-IgE complexes.13 Omalizumab cannot interact with IgE already bound to cells, which prevents the development of anaphylaxis. Following administration of omalizumab, total serum IgE levels increase but levels of free IgE in serum decrease rapidly to <5% of baseline. However, clinical efficacy takes longer to emerge as the IgE bound to mast cells and basophils takes several weeks to be downregulated.
The efficacy and safety of omalizumab as add-on therapy for patients with severe allergic asthma has been extensively evaluated. The INvestigatioN of Omalizumab in seVere Asthma TrEatment (INNOVATE) randomised, double-blind, multicentre study enrolled 419 patients aged 12–75 years with severe allergic asthma.14 The patients were randomised to receive omalizumab or placebo for 28 weeks. Patients treated with omalizumab had significantly reduced rates of severe exacerbations (0.24 vs 0.48, p = 0.002) and emergency visits (0.24 vs 0.43, p = 0.038). In addition, patients receiving omalizumab demonstrated improved asthma-related quality of life, morning peak expiratory flow and asthma symptom scores. Both groups had a similar incidence of adverse events.
The PERSIST study was a prospective, open label, observational, open-centre study in 158 patients with severe persistent allergic asthma. The effectiveness of omalizumab as add-on therapy was evaluated after 16 and 52 weeks of treatment and compared to the year prior to starting therapy. Patients had better physician-rated effectiveness, greater improvements in quality of life, greater reductions in exacerbation rates and greater reductions in healthcare utilisation than previously reported in efficacy studies.15
The potential benefits of omalizumab thus include improved asthma control, with the possibility of a reduction in the use of oral corticosteroids, fewer presentations to emergency care, reduced exacerbations and improved quality of life.
Between 1,500 and 1,600 patients are currently being treated with omalizumab in the UK and more than 155,000 patients have been treated worldwide since its launch. The drug is administered subcutaneously on a 2–4 weekly basis, with the dose based on total IgE levels and weight. However, patients must fulfil certain criteria to be eligible and cost, dosing criteria and the absence of allergic factors in about 40% of patients with severe asthma16 limit its use.
Th2 response
T cells are the main source of cytokines, including interleukins, and play an important role in driving the inflammatory changes in asthma. T helper (Th) 1 (Th1) and Th2 cells are subsets of cells that develop from the same precursor cells and produce specific cytokines. Th1 cells mediate macrophage activation and phagocytic-dependent inflammation through the production of interferon gamma (IFN-γ). In contrast to normal airways, which are Th1 predominant, the airways in allergic asthma have an increased number of Th2 cells.17 Th2-cell differentiation is stimulated by interleukin (IL) 4 and results in the production of interleukins such as IL-4, IL-5, IL-9 and IL-13 (Fig 1), which are linked to airway inflammation and hyper-responsiveness (AHR).18 Gene-expression profiling of bronchial biopsies taken from patients with asthma has led to the formation of a ‘Th2 signature’ and dichotomisation into Th2-high and Th2-low sub-phenotypes. These sub-phenotypes display patterns in airway remodelling and mucus composition and exhibit important differences in terms of their response to treatment with ICS, with improved lung function in Th2-high patients.19 This supports previous in vitro studies that have shown an association between Th1/Th2 cytokine imbalance and steroid insensitivity.20,21
Fig 1.
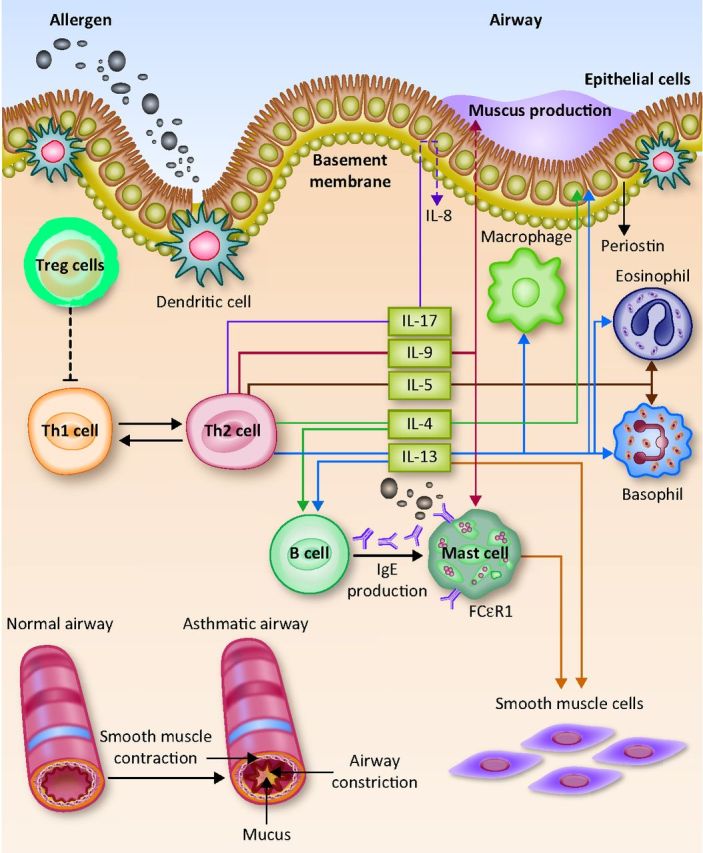
Inflammatory pathways of interleukins currently involved in asthma clinical trials. Inhaled allergens (such as pollen, dust mites and animal dander) can activate mast cells and basophils. This can trigger an acute inflammatory response in sensitive individuals, resulting in airway inflammation and airways hyper-responsiveness. Allergens are recognised and processed by dendritic cells, which drive T helper (Th) 2 differentiation and secretion of multiple cytokines, including interleukin 4 (IL-4), IL-5, IL-9, IL-13 and IL-17. IL-4 and IL-13 induce B cells to produce immunoglobulin E (IgE), IL-13 induces epithelial cells to secrete periostin (a biomarker of airway eosinophilia) and IL-5 promotes the proliferation, differentiation, recruitment and survival of eosinophils. FcϵR = Fc receptors for immunoglobulin E; IG = immunoglobulin; IL = interleukin; Treg cell = regulatory T cell. Reproduced with permission from Gibeon and Menzies-Gow (2012).18
Overall, evidence suggests that specific patterns of cytokine expression can identify patients who may respond better to targeted therapies and that their modulation may result in fewer exacerbations, an enhanced response to treatment with ICS and improved asthma control.
Potential Th2 targets in allergic asthma
Interleukin 5 promotes the proliferation, differentiation, recruitment and survival of eosinophils22 and is a key inflammatory cell mediator in the pathogenesis of asthma. High eosinophil counts in sputum are associated with poor asthma control, can predict future exacerbations and can help direct medication changes,23,24 which make IL-5 an attractive target in allergic asthma.
Early studies using mepolizumab and reslizumab, monoclonal antibodies directed against IL-5, failed to show efficacy, but recent trials have been promising. Mepolizumab has been associated with a significant decrease in asthma exacerbations in patients with severe eosinophilic asthma25 and reslizumab has demonstrated improvements in airway function and a trend towards greater asthma control.25 Benralizumab, a monoclonal antibody that targets the α chain of the IL-5 receptor, has shown promise in phase 2 trials.27
Interleukin 4 and IL-13 are functionally and structurally related. Both induce B cells to produce IgE, highlighting their role in allergic asthma and the potential to augment their expression. Lebrikizumab is an IL-13 monoclonal antibody that has been associated with improvements in lung function.28 Particular benefits were noted in subjects with high levels of serum periostin – a protein first identified in osteoblasts and produced by bronchial epithelial cells. Periostin seems to be a systemic biomarker of Th2-high asthma and airway eosinophilia and correlates with a better response to treatment with ICS.29 This suggests that lebrikizumab may be useful for a specific group of patients with allergic asthma, and results from phase 3 trials are awaited.
Immunotherapy
Allergen-specific immunotherapy (hyposensitisation therapy) involves the gradual administration of a specific allergen at increasing amounts, with the aim of inducing systemic tolerance. The mechanism of action remains incompletely understood, but it may relate to skewing of the Th2 immunity seen in allergic asthma towards a Th1 response. It is the only treatment of allergic asthma that targets one of the underlying mechanisms.30 Although immunotherapy has been used for more than 100 years, there have been recent advances and increasing interest in new allergen preparations, including allergen-antibody complexes and new delivery modalities.
Subcutaneous injection immunotherapy (SCIT) and sublingual immunotherapy (SLIT) have both been used. Early trials produced mixed results, and treatment was associated with a risk of severe and occasionally fatal anaphylaxis. A Cochrane review of 88 randomised controlled trials using SCIT for asthma noted a significant overall reduction in symptoms of asthma and use of medications, with improvements in bronchial hyper-reactivity following immunotherapy. However, one in 16 patients would be expected to develop a local adverse reaction and one in nine a systemic reaction.31 Sublingual immunotherapy was introduced in the 1990s, has a better safety profile than SCIT and is suitable for regular self-administration of allergen extract. A meta-analysis of 25 studies with 1,706 patients using SLIT found a small beneficial effect.32 Despite being well tolerated, SLIT is associated with local side effects, including mild lip swelling and itching, in 40–85% of patients.30
Immunotherapy can potentially provide lasting relief in allergic asthma, and both SCIT and SLIT have trial data for supporting their use. However, other studies have failed to find a benefit and its role in treating allergic asthma remains unclear.33
Conclusion
Significant advances have been made in our understanding of severe allergic asthma in recent years and greater comprehension of the underlying immunology has led to the identification of attractive targets for drug development. However, the only targeted medication that has made it to clinical practice is anti-IgE therapy (omalizumab). This limited success is due to a combination of factors. These include the selection of the wrong patient group for trials, cytokine interactions in what is essentially a complex and convoluted system with built-in immunological redundancy, difficulty translating animal models of asthma to humans, individual patient responses to therapy and side effects to novel biologic agents (Table 1).18
Table 1.
Targets and drugs in allergic asthma.
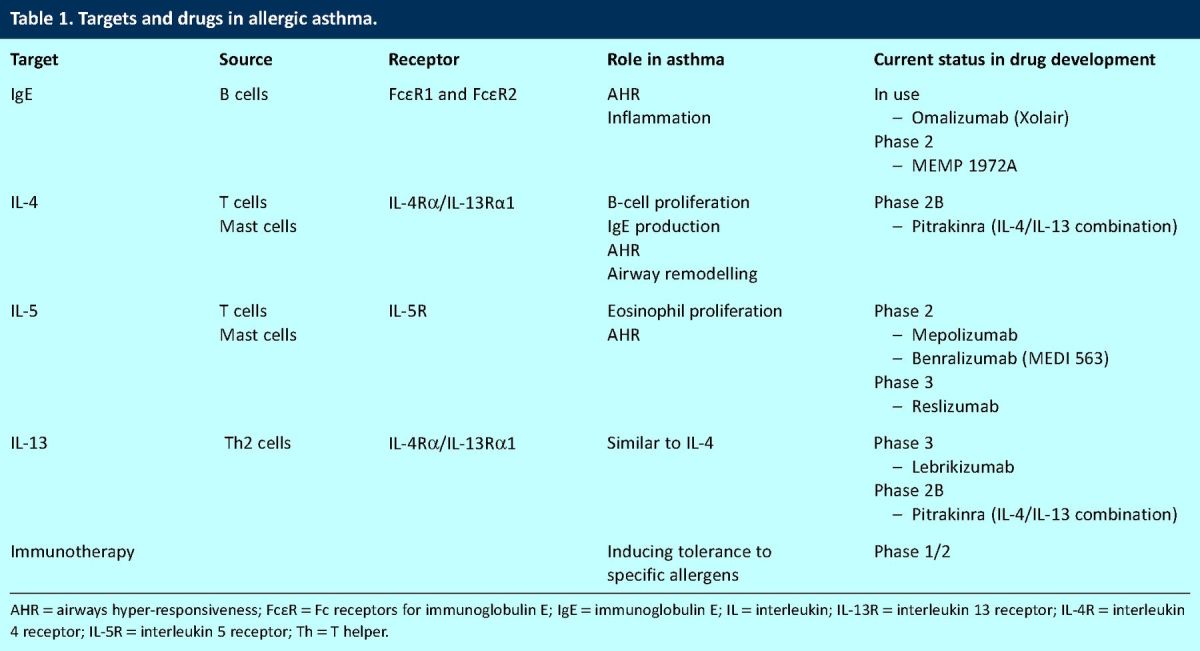
Many patients with allergic asthma continue to experience symptoms despite maximal appropriate therapy and there remains an unmet need in this group. At present, active phase 2/3 trials are investigating the effectiveness of modulating IL-5, IL-4 and IL-13, but the drugs under investigation are still several years away from potential clinical use. Future treatment will focus on personalised medicine to determine the exact phenotype underlying an individual's allergic asthma, allowing the correct targeted therapy to be used at their first presentation.
Competing interests
David Gibeon has no competing interests. Andrew Menzies-Gow has participated on advisory boards for Novartis, Genentech, Roche, GlaxoSmithKline and Napp Pharmaceuticals, has received travel and accommodation to attend international conferences from GlaxoSmithKline, Novartis AG and Boehringer Ingelheim, has received lecture fees from GlaxoSmithKline, Novartis and Chiesi and has received payments for his institution for participating in clinical trials with GlaxoSmithKline and Novartis.
References
- 1.Masoli M, Fabian D, Holt S, Beasley R. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 2004;59:469–78. 10.1111/j.1398-9995.2004.00526.x [DOI] [PubMed] [Google Scholar]
- 2.Asthma UK. Asthma facts and FAQs. www.asthma.org.uk/asthma-facts-and-statistics [Accessed 16 September 2013]. [Google Scholar]
- 3.American Thoracic Society Proceedings of the ATS workshop on refractory asthma: current understanding, recommendations, and unanswered questions. Am J Respir Crit Care Med 2000;162:2341–51. 10.1164/ajrccm.162.6.ats9-00 [DOI] [PubMed] [Google Scholar]
- 4.Gibson J, Geddes D, Costabel U. et al. Respiratory medicine, 3rd ed. London: Saunders, 2003. [Google Scholar]
- 5.Moore WC, Bleecker ER, Curran-Everett D, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute's Severe Asthma Research Program. J Allergy Clin Immunol 2007;119:405–13. 10.1016/j.jaci.2006.11.639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Strunk RC, Bloomberg GR. Omalizumab for asthma. N Engl J Med 2006;354:2689–95. 10.1056/NEJMct055184 [DOI] [PubMed] [Google Scholar]
- 7.Busse WW, Lemanske RF., Jr Asthma. N Engl J Med 2001;344:350–62. 10.1056/NEJM200102013440507 [DOI] [PubMed] [Google Scholar]
- 8.British Thoracic Society and Scottish Intercollegiate Guideline Network British guideline on the management of asthma. Thorax 2008;63:iv1–121. 10.1136/thx.2008.101691 [DOI] [Google Scholar]
- 9.Sears MR. The FDA-mandated trial of safety of long-acting beta-agonists in asthma: finality or futility? Thorax 2013;68:195–8. 10.1136/thoraxjnl-2012-202414 [DOI] [PubMed] [Google Scholar]
- 10.Bateman ED, Boushey HA, Bousquet J, et al. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med 2004;170:836–44. 10.1164/rccm.200401-033OC [DOI] [PubMed] [Google Scholar]
- 11.Thomas M, Pavord I. Single inhaler maintenance and reliever therapy (SMART) in general practice asthma management: where are we? Prim Care Respir J 2012;21:8–10. 10.4104/pcrj.2012.00022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kerstjens HA, Engel M, Dahl R, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Eng J Med 2012;367:1198–207. 10.1056/NEJMoa1208606 [DOI] [PubMed] [Google Scholar]
- 13.Schulman ES. Development of a monoclonal anti-immunoglobulin E antibody (omalizumab) for the treatment of allergic respiratory disorders. Am J Respir Crit Care Med 2001;164:S6–11. 10.1164/ajrccm.164.supplement_1.2103025 [DOI] [PubMed] [Google Scholar]
- 14.Humbert M, Beasley R, Ayres J, et al. Benefits of omalizumab as add-on therapy in patients with severe persistent asthma who are inadequately controlled despite best available therapy (GINA 2002 step 4 treatment): INNOVATE. Allergy 2005;60:309–16. 10.1111/j.1398-9995.2004.00772.x [DOI] [PubMed] [Google Scholar]
- 15.Brusselle G, Michils A, Louis R, et al. ‘Real-life’ effectiveness of omalizumab in patients with severe persistent allergic asthma: the PERSIST study. Respir Med 2009;103:1633–42. 10.1016/j.rmed.2009.06.014 [DOI] [PubMed] [Google Scholar]
- 16.Heaney LG, Brightling CE, Menzies-Gow A, et al. Refractory asthma in the UK: cross-sectional findings from a UK multicentre registry. Thorax 2010;65:787–94. 10.1136/thx.2010.137414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meyer EH, DeKruyff RH, Umetsu DT. T cells and NKT cells in the pathogenesis of asthma. Annu Rev Med 2008;59:281–92. 10.1146/annurev.med.59.061506.154139 [DOI] [PubMed] [Google Scholar]
- 18.Gibeon D, Menzies-Gow AN. Targeting interleukins to treat severe asthma. Expert Rev Respir Med 2012;6:423–39. 10.1586/ers.12.38 [DOI] [PubMed] [Google Scholar]
- 19.Choy DF, Modrek B, Abbas AR, et al. Gene expression patterns of Th2 inflammation and intercellular communication in asthmatic airways. J Immunol 2011;186:1861–9. 10.4049/jimmunol.1002568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leung DY, Martin RJ, Szefler SJ, et al. Dysregulation of interleukin 4, interleukin 5, and interferon gamma gene expression in steroid-resistant asthma. J Exp Med 1995;181:33–40. 10.1084/jem.181.1.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bentley AM, Hamid Q, Robinson DS, et al. Prednisolone treatment in asthma. Reduction in the numbers of eosinophils, T cells, tryptase-only positive mast cells, and modulation of IL-4, IL-5, and interferon-gamma cytokine gene expression within the bronchial mucosa. Am J Respir Crit Care Med 1996;153:551–6. 10.1164/ajrccm.153.2.8564096 [DOI] [PubMed] [Google Scholar]
- 22.Lopez AF, Sanderson CJ, Gamble JR, et al. Recombinant human interleukin 5 is a selective activator of human eosinophil function. J Exp Med 1988;167:219–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Romagnoli M, Vachier I, Tarodo de la Fuente P, et al. Eosinophilic inflammation in sputum of poorly controlled asthmatics. Eur Respir J 2002;20:1370–7. [DOI] [PubMed] [Google Scholar]
- 24.Green RH, Brightling CE, McKenna S, et al. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet 2002;360:1715–21. 10.1016/S0140-6736(02)11679-5 [DOI] [PubMed] [Google Scholar]
- 25.Pavord ID, Korn S, Howarth P, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet 2012;380:651–9. 10.1016/S0140-6736(12)60988-X [DOI] [PubMed] [Google Scholar]
- 26.Castro M, Mathur S, Hargreave F, et al. Reslizumab for poorly controlled, eosinophilic asthma: a randomized, placebo-controlled study. Am J Respir Crit Care Med 2011;184:1125–32. 10.1164/rccm.201103-0396OC [DOI] [PubMed] [Google Scholar]
- 27.Gossage D, Geba G, Gillen A. et al. A multiple ascending subcutaneous dose study of MEDI-563, a humanized anti-IL-5RA monoclonal antibody, in adult asthmatics. Poster presented at the Annual Congress of the European Respiratory Society. Barcelona, Spain, 18–22 September 2010. (Poster P1177). [Google Scholar]
- 28.Corren J, Lemanske RF, Hanania NA, et al. Lebrikizumab treatment in adults with asthma. N Engl J Med 2011;365:1088–98. 10.1056/NEJMoa1106469 [DOI] [PubMed] [Google Scholar]
- 29.Jia G, Erickson RW, Choy DF, et al. Periostin is a systemic biomarker of eosinophilic airway inflammation in asthmatic patients. J Allergy Clin Immunol 2012;130:647–54. 10.1016/j.jaci.2012.06.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cappella A, Durham SR. Allergen immunotherapy for allergic respiratory diseases. Hum Vaccin Immunother 2012;8:1488–512. 10.4161/hv.21629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abramson MJ, Puy RM, Weiner JM. Injection allergen immunotherapy for asthma. Cochrane Database Syst Rev 2010;(8):CD001186. [DOI] [PubMed] [Google Scholar]
- 32.Calamita Z, Saconato H, Pela AB, Atallah AN. Efficacy of sublingual immunotherapy in asthma: systematic review of randomized-clinical trials using the Cochrane Collaboration method. Allergy 2006;61:1162–72. 10.1111/j.1398-9995.2006.01205.x [DOI] [PubMed] [Google Scholar]
- 33.Incorvaia C, Riario-Sforza GG, Incorvaia S, Frati F. Sublingual immunotherapy in allergic asthma: Current evidence and needs to meet. Ann Thorac Med 2010;5:128–32. 10.4103/1817-1737.65038 [DOI] [PMC free article] [PubMed] [Google Scholar]


