Abstract
This study aimed to quantify and compare the prevalence of simple prescribing errors made by clinicians in the first 24 hours of a general medical patient's hospital admission. Four public or private acute care hospitals across Australia and New Zealand each audited 200 patients' drug charts. Patient demographics, pharmacist review and pre-defined prescribing errors were recorded. At least one simple error was present on the medication charts of 672/715 patients, with a linear relationship between the number of medications prescribed and the number of errors (r=0.571, p<0.001). The four sites differed significantly in the prevalence of different types of simple prescribing errors. Pharmacists were more likely to review patients aged >75 years (39.9% vs 26.0%; p<0.001) and those with more than 10 drug prescriptions (39.4% vs 25.7%; p<0.001). Patients reviewed by a pharmacist were less likely to have inadequate documentation of allergies (13.5% vs 29.4%, p<0.001). Simple prescribing errors are common, although their nature differs from site to site. Clinical pharmacists target patients with the most complex health situations, and their involvement leads to improved documentation.
Key Words: clinical pharmacist, medication chart, prescription error
Introduction
Medication safety is the outcome of a complex process involving doctors, pharmacists, nurses and patients. A recent review suggests that about 2–3% of Australian hospital admissions are related to medications and that medication incidents are the second most common type of incident reported in Australian hospitals.1 A range of factors that contribute to hospital medication incidents have been identified, including errors and omissions in prescribing, administration and dispensing.1 Prescribing errors can be considered as one category of error that can lead to medication-related harm. Not all prescribing errors will lead to harm and not all adverse drug effects are due to prescribing errors. Previous authors have sought to define prescribing errors in order to allow comparison between different systems, but a broad range of scenarios fit within this definition.2 ‘Potential for harm’ is key to the definition of a clinically meaningful prescribing error. This can range from the risk of harm from receiving a drug that is contraindicated or in an excessive dose to the risk of harm from not receiving a drug because the order is incompletely documented and therefore invalid. Simple prescribing errors may be better appreciated as breaches in documentation (failing to sign a prescription or writing the drug illegibly are examples) but can still lead to harm and would therefore satisfy the definition of a prescribing error.
A patient's admission to hospital is a time when prescribing errors commonly occur,3 and these can then be perpetuated throughout a patient's stay in hospital and even after hospital discharge, increasing the potential for harm.4 With the current redesign of acute medical services to provide measurable quality of care in Australia and New Zealand,5 there is both an opportunity and an imperative to minimise the prevalence of prescribing errors and improve patient safety.
The primary aim of this multicentre audit was to quantify and compare the prevalence of simple prescribing errors made by clinicians in the first 24 hours after medical patients' admissions on four sites across Australia and New Zealand. Secondary aims of the study were to identify those patients whose charts were reviewed by a pharmacist, the characteristics of these particular patients and the frequency with which patient weight was recorded on medication charts.
Methods
Three sites in Australia (Joondalup Health Campus, Western Australia (WA); Royal Perth Hospital, WA, and Royal Adelaide Hospital, South Australia) and one in New Zealand (Auckland Hospital) collaborated in this study. Each hospital obtained local and reciprocal ethical approval for the study. In a prospective fashion, each hospital aimed to audit the medication charts of 200 consecutive adult medical patients admitted to its department of medicine from 19 April 2010, including patients admitted at weekends or overnight. All of the hospitals used paper prescription charts and did not routinely use computerised prescribing or decision-making tools. All prescribers were medical officers (mostly junior medical officers). All Australian sites used the Australian national inpatient medication chart (NIMC). All medical departments had limited clinical pharmacy support.
The patient drug chart was photocopied within 24 hours of patient admission (defined as within 24 hours of first presentation at hospital according to the time recorded by the emergency department or hospital unit triage). The date and time of admission were recorded, together with the patient's age, sex and list of drugs prescribed in the community, as clerked by the admitting medical officer. We defined working hours as 8.00am to 5.00pm on a weekday, excluding public holidays. Simple prescribing errors made on the chart by the prescribing clinician were recorded by medical officers of advanced physician trainee level (equivalent to at least four years of postgraduate training or specialty training 3 in the UK) or higher. The definitions of all recorded simple prescribing errors were agreed by reviewers at all sites as:
-
1
drug not prescribed by generic name (this is a requirement of prescriptions on the NIMC)
-
2
drug name illegible
-
3
prescription unsigned by prescriber
-
4
prescriber's name illegible or not provided
-
5
prescription undated
-
6
inadequate documentation of allergy (documentation of allergy was considered inadequate if a medication name but no reaction was documented or there was no documentation whatsoever concerning allergy on the medication chart).
Any annotation by a clinical pharmacist on the medication chart was recorded in our audit as evidence of clinical pharmacist review. Each site had a separate reviewer and any disputed classifications were adjudicated by the lead author (LB).
The following patients were excluded from the study:
patients younger than 16 years
those for whom no medications had been prescribed
surgical or obstetric admissions
those admitted but transferred immediately to another hospital.
Due to ethical agreements, data from individual sites were not identifiable as from a particular institution, which are therefore reported as hospitals 1–4 in the results, and no patient identifiers were recorded. SPSS software (version 19) was used for statistical analysis. Chi-squared analysis was used to test comparisons of performance between sites. Spearman's rank correlation coefficient was calculated for the linearity of associations, where relevant. A difference was considered significant when p<0.05.
Results
General description
After consideration of the above criteria, 715 patients were included in the analysis: 200 each from hospitals sites 1 and 2, 146 from hospital site 3 and 169 from hospital site 4. The mean patient age was 66.7 (range 16–98; standard deviation 19.7) years. The mean age on each site ranged from 64.1 years to 70.6 years. Overall, there were 363 (51%) female patients and 352 (49%) male patients (Table 1).
Table 1.
Patient characteristics across four hospital sites.
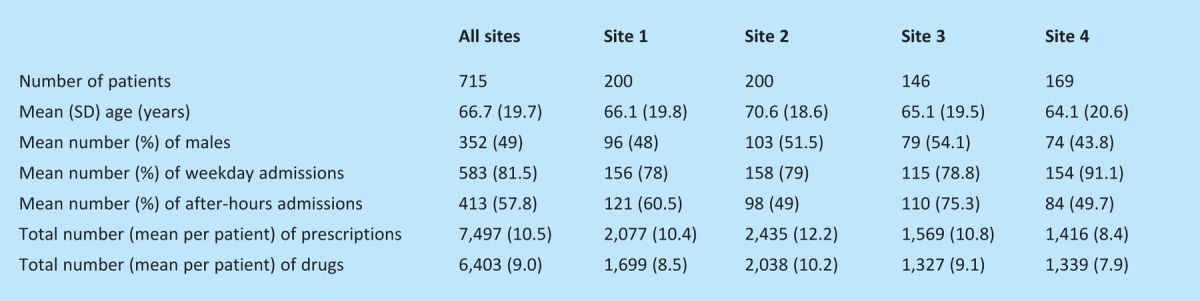
The majority of patients (81%) were admitted to hospital on a weekday and 46% were admitted overnight (5.00pm–8.00am). Just less than 60% of patients were admitted out of routine working hours during the period of the study (ie on weekends or public holidays and overnight). The 715 patients received 7,497 prescriptions in total, and 6,403 drugs were prescribed. The number of prescriptions was higher than the number of drugs prescribed, because some drugs need to be prescribed more than once on the chart (for example, if there is a different dose in the morning and the evening). This represented a mean of nine drugs and 10.5 prescriptions per patient (see Table 1).
Simple prescribing error prevalence
The medication charts for 672/715 patients contained at least one simple error. There was a linear relationship between the number of medications prescribed and the number of errors (r=0.571; p<0.001). At least one prescribing error was present on the charts of all patients prescribed more than 18 drugs. Patients' names were documented on all but one chart, and second patient identifiers were present on all but five patients' charts. Patients' weights were documented infrequently (on the drug charts of only 35 patients). The medication charts of 413 (57.8%) patients contained a drug prescribed by trade name, and drug names were illegible on the charts of 47 (6.6%) patients. Prescriptions were not signed on the charts of 148 (20.7%) patients, and prescriptions were not dated on the charts of 267 (37.3%) patients (Table 2). The four sites differed significantly in the prevalence of each of these types of simple error. There was no significant difference in the prevalence of errors for patients admitted inside usual working hours compared with those admitted on weekends or evenings, or overnight.
Table 2.
Comparison of simple prescribing errors across four hospital sites.
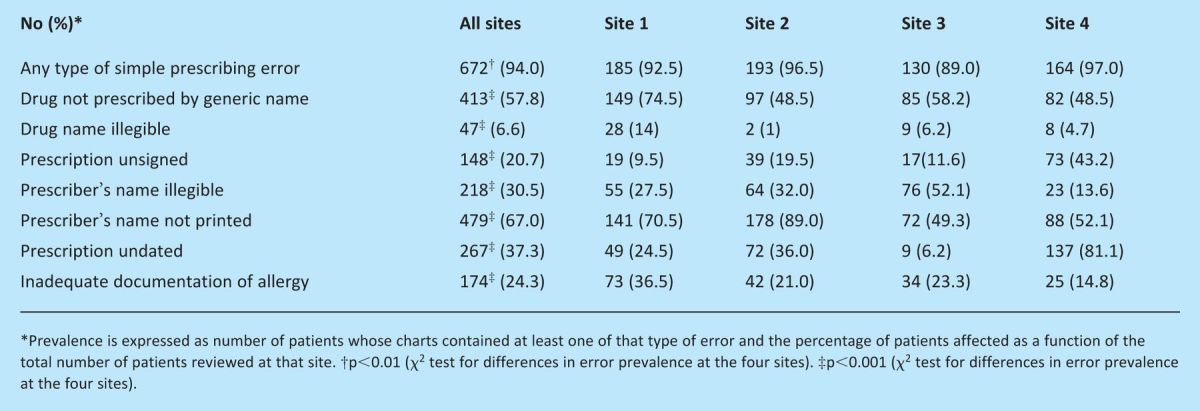
Allergies
Documentation of allergy was inadequate in 174 (24.3%) patients. Specifically, a medication name but no reaction was documented for 115 (16%) patients and for an additional 59 (8%) patients there was no documentation whatsoever on their chart concerning allergy. Adequate recording of no known drug allergy was present in 440 (62%) patients, and another 101 (14%) had at least one medication name and allergic reaction recorded. The percentage of patients with incomplete documentation of allergy varied significantly between the sites (p<0.001) (see Table 2).
Pharmacist review
At the time of sampling, a clinical pharmacist had reviewed 229 (32%) patients' drug charts within 24 hours of admission to hospital. Charts were less likely to have been reviewed by a pharmacist if the patient was admitted over a weekend compared with on a weekday (19% vs 35%; p<0.001). Patients admitted overnight were as likely as daytime admissions to see a pharmacist within 24 hours. Pharmacists were more likely to review those patients aged >75 years (39.9% vs 26.0%; p<0.001) and those with more than 10 drug prescriptions (39.4% vs 25.7%; p<0.001). Patients' charts reviewed by a pharmacist were less likely to have inadequate documentation of allergies (13.5% vs 29.4%; p<0.001).
Discussion
We have demonstrated a high incidence of simple prescribing errors in the charts of medical patients during the initial period of their hospital admission. Notably, the findings occur across a variety of sites, including both private and public hospitals in Australia and New Zealand. The frequency of error types differed across the four sites, but, in general, the findings are similar to previously published findings in comparable studies from the UK.3,6 Accurate comparisons of the prevalence of errors in the literature are difficult given the differences in study design and the heterogeneous nature of occurrences that can be classified as prescribing errors.7 Failure to document any information regarding drug allergy in 8% of our patients is also similar to the findings in other studies (13%).3
Limitations
We have measured only simple prescribing errors made by clinicians rather than more complex errors involving choice of drug, dose and route, or errors in transcribing, administering or dispensing. We have not noted whether patients' weights were recorded elsewhere in each patient's case notes. We have not measured any incidents of harm. However, the potential for harm is an accepted definition for a prescribing error. Previous studies have shown harm from simple prescribing errors:8,9 for example, the use of trade names is associated with greater prevalence of duplication of medications, presumably due to pre scribers' failure to recognise identical medications.3 Another obvious source of harm from simple errors is the inadequate documentation of allergy when omissions could result in the administration of a contraindicated drug.10
Intersite prevalence of simple prescribing errors
Although simple prescribing errors are widespread, there were differences between hospitals in the prevalence of specific types of errors. These differences may be due to design of local drug charts, differing cultures among clinicians, varied education practices or role modelling. For example, hospital 4 had markedly higher numbers of unsigned and undated prescriptions than hospital 1. This may be due to the (unacceptable) practice of only signing and dating the first prescription on a page. Our study did not examine the causes of such differences; however, considering the magnitude of these intersite differences, any interventions to reduce the prevalence of these errors should be site specific and should also take into account local variations in practice.
The role of clinical pharmacists
The linear relationship between the number of medications prescribed and the number of errors denotes that polypharmacy is a risk factor for simple prescription errors.11,12 Clinical pharmacists are appropriately targeting older patients and those taking larger numbers of medications as a priority for early review. Efficacy of clinical pharmacists' involvement was evident in the higher prevalence of adequate allergy documentation among patients who had been reviewed by a clinical pharmacist in this study. It is not clear from our study exactly how pharmacists were able to influence documentation, although their usual practice is to speak with junior medical staff about any issues they find on chart review. They are not legally able to alter prescriptions but are able to document allergy on the chart. The benefit of pharmacist review has been seen in other studies, with improved accuracy and documentation.13,14 However, the timeliness of pharmacist review is paramount in improving safety, particularly with regard to allergy documentation. This presents a challenge for admissions after hours.
Intervention design
Prescribing errors can be caused by inattention and lack of knowledge.15 These are more likely to occur if tasks are carried out after hours by busy and distracted staff.16 Academic detailing has been shown to reduce hospital prescribing errors.17 However, a recent review concluded that published evidence regarding the impact of educational strategies on improving prescribing errors is limited. Published studies, in general, were of brief interventions with short follow-up periods and lacked testing in ‘real-life’ situations.7 The local preponderance of error types should guide local interventions to reduce the prevalence of errors. Any common errors (eg absence of weight documentation on charts) should guide generic education policy. The NIMC was introduced in Australia in 2006;18 this has allowed repetitive audit on a national level to track the frequency of prescribing errors, which has demonstrated a reduced rate of such errors.19 However, local collection of data and feedback may encourage ownership of this problem by prescribers and could be more effective at inducing behavioural change.9,20 Our data suggest that simple prescribing errors were common at all hospital sites but the types of errors differed across the four sites. An online training module for prescribers on the use of the NIMC has been developed by the National Prescribing Service (and is currently in a pilot testing phase) and could be another useful tool for education.21 Whether a generic or locally flavoured intervention is more effective at improving error prevalence is unknown, and future national collaboration by clinicians is welcomed.
Conclusion
Safe and appropriate prescribing is a complex process. In this study, we addressed only limited elements of this process and have demonstrated that simple errors and poor documentation of allergy are common but can be improved with the involvement of clinical pharmacists. Future focus on interventions should include multidisciplinary collaboration, eg academic detailing of prescribers by clinical pharmacists, review of medication charts by nursing staff and clinical pharmacists, and discussion of any medication chart shortcomings with prescribers. In addition, a competency-based curriculum for medical students and postgraduate trainees would ensure appropriate expertise in prescribing.
The National Prescribing Service in Australia has developed an online prescribing curriculum that seeks to address the issue of prescribing competencies in new graduates and is now widely used in teaching during the final medical undergraduate year. Further collaboration between licensing bodies, specialty colleges and universities would help ensure that a competency-based approach is universally enforced.
References
- 1.Roughead EE, Semple SJ. Medication safety in acute care in Australia: where are we now? Part 1: a review of the extent and causes of medication problems 2002–2008. Aust New Zealand Health Policy 2009;6:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dean B, Barber N, Schacter M, Barber N. What is prescribing error? Qual Health Care 2000;9:232–7 10.1136/qhc.9.4.232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gray E, Ullah S, Lwin A, et al. Prescription errors in patients on an acute medical assessment unit. J R Coll Physicians Edinb 2007;37:305–8 [Google Scholar]
- 4.Pippins JR, Gandhi TK, Hamann C, et al. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med 2008;23:1414–22 10.1007/s11606-008-0687-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scott I, Vaughan L, Bell D. Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care 2009;21:397–407 10.1093/intqhc/mzp045 [DOI] [PubMed] [Google Scholar]
- 6.General Medical Council. An in depth investigation into causes of pre scribing errors by foundation trainees in relation to their medical education – EQUIP study. London: GMC; 2009. www.gmc-uk.org/about/research/research_commissioned_4.asp [Accessed 22 January 2012] [Google Scholar]
- 7.Ross S, Bond C, Rothnie H, et al. What is the scale of prescribing errors committed by junior doctors? A systematic review. Br J Clin Pharmacol 2009;67:629–40 10.1111/j.1365-2125.2008.03330.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhasale AL, Miller GC, Reid SE, Britt HC. Analysing potential harm in Australian general practice: an incident-monitoring study. Med J Aust 1998;169:73–6 [DOI] [PubMed] [Google Scholar]
- 9.Thomas AN, Panchagnula U. Medication-related patient safety incidents in critical care: a review of reports to the UK National Patient Safety Agency. Anaesthesia 2008;63:726–33 10.1111/j.1365-2044.2008.05485.x [DOI] [PubMed] [Google Scholar]
- 10.Benkhaial A, Kaltschmidt J, Weisshaar E, et al. Prescribing errors in patients with documented drug allergies: comparison of ICD-10 coding and written patient notes. Pharm World Sci 2009;31:464–72 10.1007/s11096-009-9300-5 [DOI] [PubMed] [Google Scholar]
- 11.Goldberg RM, Mabee J, Chan L, Wong S. Drug-drug and drug-disease interactions in the ED: analysis of a high-risk population. Am J Emerg Med 1996;14:447–50 10.1016/S0735-6757(96)90147-3 [DOI] [PubMed] [Google Scholar]
- 12.Scott I, Jayathissa S. Quality of drug prescribing in older patients: is there a problem and can we improve it? Int Med J 2010;40:7–18 10.1111/j.1445-5994.2009.02040.x [DOI] [PubMed] [Google Scholar]
- 13.Campbell F, Karnon J, Czoski-Murray C, Jones R. A systematic review of the effectiveness and cost effectiveness of interventions aimed at preventing medication error (medicines reconciliation) at hospital admission. London: NICE; 2008. www.nice.org.uk/nicemedia/pdf/PatientSafetyMedsSystematicReview.pdf [Accessed 22 January 2012] [DOI] [PubMed] [Google Scholar]
- 14.Carter MK, Allin DM, Scott LA, Grauer D. Pharmacist-acquired medication histories in a university hospital emergency department. Am J Health Syst Pharm 2006;63:2500–3 10.2146/ajhp060028 [DOI] [PubMed] [Google Scholar]
- 15.Dean B, Schachter M, Vincent C, Barber N. Causes of prescribing errors in hospital inpatients: a prospective study. Lancet 2002;359:1373–9 10.1016/S0140-6736(02)08350-2 [DOI] [PubMed] [Google Scholar]
- 16.Nichols P, Copeland TS, Craib IA, et al. Learning from error: identifying contributory causes of medication errors in an Australian hospital. Med J Aust 2008;188:276–9 [DOI] [PubMed] [Google Scholar]
- 17.Shaw J, Harris P, Keogh G, et al. Error reduction: academic detailing as a method to reduce incorrect prescriptions. Eur J Clin Pharmacol 2003;59:697–9 10.1007/s00228-003-0683-2 [DOI] [PubMed] [Google Scholar]
- 18.Australian Commission on Safety and Quality in Health Care. National inpatient medication chart. Darlinghurst, New South Wales: ACSQHC; 2009. www.health.gov.au/internet/safety/publishing.nsf/Content/national-inpatient-medication-chart [Accessed 26 January 2012] [Google Scholar]
- 19.Coombes I, Reid C, McDougall D, et al. Pilot of a national Inpatient Medication Chart in Australia: improving prescribing safety and enabling prescribing training. Br J Clin Pharmacol 2011;72:338–49 10.1111/j.1365-2125.2011.03967.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lagerlov P, Loeb M, Andrew M, Hjortdahl P. Improving doctors' prescribing behaviour through reflection on guidelines and prescription feedback: a randomised controlled study. Qual Health Care 2000;9:159–65 10.1136/qhc.9.3.159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ross S, Loke YK. Do educational interventions improve prescribing by medical students and junior doctors? A systematic review. Br J Clin Pharmacol 2009;67:662–70 10.1111/j.1365-2125.2009.03395.x [DOI] [PMC free article] [PubMed] [Google Scholar]


