Abstract
This concise guidance, prepared for physicians, summarises the British Occupational Health Research Foundation guideline for the prevention, identification and management of occupational asthma. Approximately one in six people of working age who develop asthma have work-related asthma, where work has either caused or aggravated their disease. Physicians who assess working adults with asthma need to ask the patient about their job and the materials they work with, and be aware of those that carry particular risks; they should also ask whether symptoms improve regularly on days away from work. A diagnosis of occupational asthma (ie asthma caused by work) should not be made on the basis of history alone, but be supported by immunological and physiological investigations of proven diagnostic benefit. Following a validated diagnosis of occupational asthma, physicians should recommend early avoidance of further exposure, because this offers the best chance of complete recovery. If appropriate and timely interventions are not taken, the prognosis of occupational asthma is poor, with only approximately one-third of workers achieving full symptomatic recovery.
Key Words: occupational asthma, work-related asthma, evidence-based guideline
Background
A recent meta-analysis indicates that occupational factors account for approximately one in six cases of asthma in adults of working age, including new onset or recurrent disease.1 The incidence of occupational asthma within a workforce depends on people's jobs and the innate hazards to which they are exposed. Incidence even varies within a single industry, because the effectiveness of management programmes and the control of exposure can vary among different employers.
Asthma is ‘work-related’ when there is an association between symptoms and work. The different types of work-related asthma should be distinguished, because the implications for the patient and their management differ. Work-related asthma includes two distinct categories:
Occupational asthma: that is, asthma induced by exposure in the working environment to airborne dusts, vapours or fumes, in workers with or without pre-existing asthma.2
Work-aggravated asthma: that is, pre-existing or coincidental new-onset adult asthma, which is made worse by non- specific factors in the workplace, such as cold, dry air, exertion, dust and fumes.
Occupational asthma can be subdivided into:
Sensitiser-induced occupational asthma, which is characterised by a latency period between first exposure to a respiratory sensitiser at work and the first presentation of immunologically mediated symptoms.
Irritant-induced occupational asthma, which starts typically within a few hours of a high-intensity exposure to an irritant gas, fume or vapour encountered at work.3
For some agents, both immunological and non-immunological mechanisms can be involved. This guidance focuses on sensitiser-induced disease, which accounts for approximately 90% of cases of occupational asthma.3
Scope and aims
This guidance summarises the 2010 update to the evidence-based guideline published by the British Occupational Health Research Foundation,3 with recommendations graded using the Scottish Intercollegiate Guidelines Network (SIGN) grading system.4 The first edition of the guideline was published in 2004 in support of the Health and Safety Executive (HSE) target to reduce the incidence of occupational asthma in the UK. The Appraisal of Guidelines and Research Evaluation (AGREE) instrument5 was used when developing the methodology. This guidance aims to:
inform physicians of the evidence base related to the identification, diagnosis, management and prevention of occupational asthma
help reduce the severity of individual cases of disease by earlier, accurate identification and better management
supplement other guidelines for the clinical management of asthma.6
Risk factors and prevention
The level of exposure to a causative agent at work is a major determinant of risk for the development of sensitiser-induced occupational asthma and so primary prevention should be focused on removing or reducing exposure at source. Other risk factors include the predisposing factors of atopy and genetic predisposition and, for some agents, the contributory factor of cigarette smoking. In the general population, rhinitis and asthma frequently co-occur; the same is true for occupational rhinitis and asthma. Occupational rhinitis can indicate that there is a risk of developing occupational asthma, the risk being highest in the year after the onset of rhinitis.
Recognition and diagnosis
The diagnosis of asthma is based on the recognition of a characteristic pattern of symptoms and signs and the absence of an alternative explanation for them. The key is to take a careful clinical history. The likelihood of an asthma diagnosis increases where: symptoms include at least two of wheeze, breathlessness, chest tightness and cough; auscultation reveals a widespread wheeze; and there is an otherwise unexplained low forced expiratory volume in 1 second (FEV1) or peak expiratory flow (PEF). Further details of diagnosis are contained in the British Guideline on the Management of Asthma.6
Early recognition and diagnosis of occupational asthma, with early avoidance of further exposure, offer the best chance of complete recovery. A potential occupational cause of asthma can be identified by asking working patients about their jobs and the materials with which they work, and by being aware of occupations and exposures that carry particular risks. A list of these is available from HSE.7 It is important to enquire whether symptoms improve regularly when away from the workplace, such as on days away from work or on holiday.
A diagnosis of occupational asthma should not be made on the basis of a positive history alone; the occupational and related consequences of an inaccurate diagnosis can be severe. Diagnostic tests of proven value include:
Properly conducted and analysed serial measurement of peak flow at and away from work. To obtain accurate readings and interpret them correctly in the occupational context, at least four readings per day are required, at and away from work, for a period of at least three weeks. Sample instructions and a record sheet are available.8 The completed measurements are most usefully plotted as daily minimum, mean and maximum values, with an index of daily variability calculated as the difference between the highest and lowest PEF expressed as a percentage of either the mean or highest value. The upper limit of normal for intraday variability in PEF measurements is approximately 20% using four or more PEF readings per day.6 A serial record of PEF is suggestive of work-related asthma where there is a consistent fall in values and/or increase in variability on days at work, with recovery on days away from work. The interpretation of records in the assessment of an occupational relationship requires some skill; computer-based analyses can be helpful.3 Serial peak flow measurement is only useful when a patient is still working in a job with exposure to the suspect agent. Relocation of a patient during the process of diagnosis is only necessary if symptoms are severe.
Specific immunoglobulin E (IgE) assay or skin-prick testing for causative agents with a clear immunological mechanism. For high-molecular-weight (protein) agents, these tests have high sensitivity.3
Specific inhalation testing, the gold standard, is available in a few specialist centres only and the diagnosis of occupational asthma can usually be made without this test.6
Advice on any, or all, of the above and on the management of patients with work-related asthma is available from physicians with a special interest in occupational lung diseases. Where there is uncertainty over a diagnosis or management, specialist referral is recommended.9
Management and prognosis
An early and accurate diagnosis of occupational asthma offers the unusual prospect of a ‘cure’ for the disease. Conversely, inaccurate diagnoses can either hamper symptom control and risk a poor prognosis (ie false negative diagnosis) or lead to unnecessary economic hardship and a failure to improve (ie false positive diagnosis).
Effective management involves timely intervention and taking appropriate actions to protect patients with occupational asthma from further exposure to its causes in the workplace. Given that there might be significant consequences for the patient's employment, informed consent should be written when communicating with a patient's employer. Employers can protect the patient by several means, ranging from engineering controls (which will protect other workers) to redeployment to a job free from exposure. Once sensitised, a patient's symptoms might be incited by exposure to extremely low concentrations of a respiratory sensitiser. Hence, respiratory protective equipment (RPE), such as air-fed helmets, might improve or prevent symptoms in some, but not all, patients who continue to be exposed to the causative agent. RPE offers protection only insofar as the correct type is selected, it is worn when appropriate, there is a good fit on the face and proper procedures are followed for its removal, storage and maintenance. Generally, occupational asthma has a poor prognosis, with approximately two-thirds of workers never achieving full symptomatic recovery and approximately three-quarters having persistent non-specific bronchial hyper-responsiveness. Approximately one-third of workers with occupational asthma are unemployed up to six years after diagnosis. Specialist hospital and, where available, specialist occupational health care might improve these outcomes.
Occupational asthma is a prescribed disease for the purpose of Industrial Injuries Disablement Benefit. Patients can access information about this benefit at www.direct.gov.uk/en/disabledpeople/financialsupport/otherbenefitsandsupport/dg_10016183 [Accessed 25 January 2012]. If the employer failed to take adequate precautions to prevent harm, the patient might be entitled to make a civil claim for compensation for personal injury. Occupational asthma is reportable under the Reporting of Injuries, Diseases and Dangerous Occurrences Regulations (RIDDOR), whereby employers have a statutory duty to report cases to the HSE.
Limitations of the guidance
The guidance includes few grade A recommendations. Criteria for grading evidence commonly regard randomised controlled trials (RCTs) as the highest level (A) of evidence, but these are not always the most appropriate study design for many areas of occupational medicine; for example, susceptibility to disease or the sensitivity and specificity of screening and diagnostic procedures. Lower grade recommendations do not necessarily mean that the topic is debatable or unimportant.
The proper application of evidence-based medicine requires that physicians exercise judgement, knowledge and expertise when deciding whether it is appropriate to apply guidance, taking into account individual circumstances and the patient's wishes.
Barriers to implementation
These include unnecessarily long delays in patients who might have occupational asthma accessing specialist assessment following the onset of their disease; lack of awareness of occupational factors during clinical assessments and of measures to control exposure to causative workplace agents; lack of access to occupational health services; and social and/or economic factors. Delayed management is detrimental because early diagnosis and early avoidance of further exposure provide the best chance of complete recovery. Half of the UK workforce is employed by small- and medium-sized enterprises, which are less likely to provide access to occupational health care. Communication is more likely to be between physicians and a manager or a worker responsible for safety than with another health professional. Obtaining the patient's consent might be a barrier because patients might wish to conceal their disease from their employer because of the fear of losing their job.
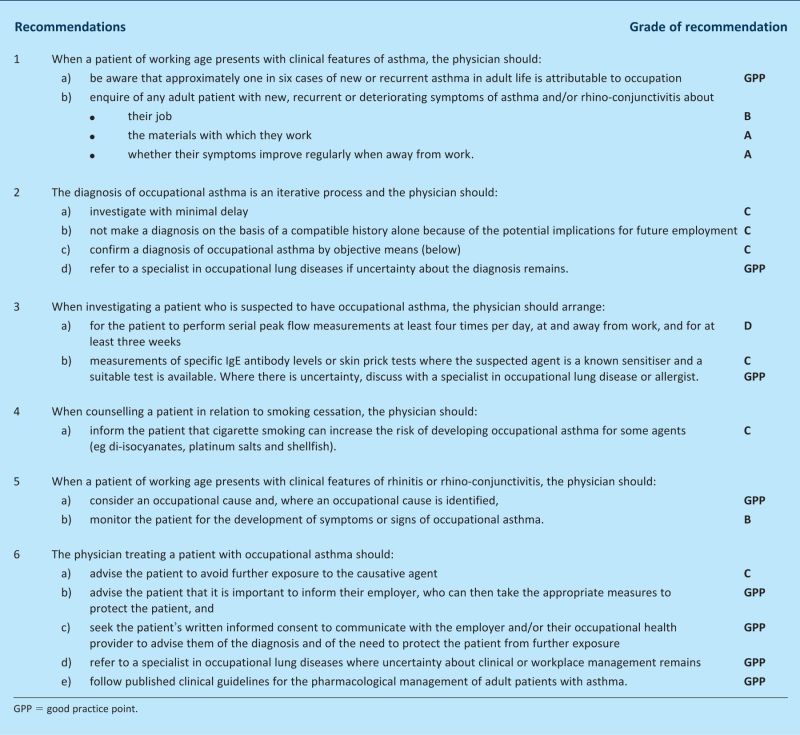
Box 1. The Guidelines.
References
- 1.Toren K, Blanc P. Asthma caused by occupational exposures is common: a systematic analysis of estimates of the population-attributable fraction. BMC Pulm Med 2009;9:7. 10.1186/1471-2466-9-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Francis HC, Prys-Picard CO, Fishwick D, et al. Defining and investigating occupational asthma: a consensus approach. Occup Environ Med 2007;64:361–5 10.1136/oem.2006.028902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicholson PJ, Cullinan P, Burge PS, Boyle C. Occupational asthma: prevention, identification & management: systematic review & recommendations. London: British Occupational Health Research Foundation; 2010. [Google Scholar]
- 4.Scottish Intercollegiate Guidelines Network. SIGN 50: a guideline developer's handbook. Edinburgh: SIGN; 2000. [Google Scholar]
- 5.The AGREE Collaboration. Appraisal of Guidelines for Research and Evaluation (AGREE) Instrument. London: The AGREE Collaboration; 2001. www.agreecollaboration.org [Accessed 25 January 2012] [Google Scholar]
- 6.British Thoracic Society & Scottish Intercollegiate Guidelines Network. Guideline 101. British guideline on the management of asthma. A national clinical guideline. London: BTS; Edinburgh: SIGN; 2011. www.sign.ac.uk/guidelines/fulltext/101/index.html [Accessed 25 January 2012] [Google Scholar]
- 7.Health & Safety Executive. List of substances that can cause occupational asthma. London: HSE; www.hse.gov.uk/asthma/substances.htm [Accessed 25 January 2012] [Google Scholar]
- 8.Oasys Research Group Asking a patient for a serial peak flow record. www.occupationalasthma.com/occupational_asthma_pageview.aspx?id=4562 [Accessed 25 January 2012]
- 9.Fishwick D, Barber CM, Bradshaw LM, et al. British Thoracic Society Standards of Care Subcommittee Guidelines on Occupational Asthma. Thorax 2008;63:240–50 [DOI] [PubMed] [Google Scholar]