Summary
The retrosternal region (RSS) can be involved by diverse lesions. The RSS is the region behind the sternum and anterior to the ascending aorta. It normally is less than 3 cm deep. Chest X-ray is usually the first imaging modality to raise a suspicion of RSS pathology; however computed tomography is the mainstay to delineate and characterize lesions in this location. Lesions in this location include thyroid, thymic and lymph node lesions; germ cell tumors and vascular lesions. Lesions arising from the sternum, lungs as well as the pleura can also involve this space. The pictorial review depicts the diverse spectrum of lesions in this location.
MeSH Keywords: Sternum; Thorax; Tomography, Emission-Computed
Background
The retrosternal space (RSS) has been described as one of the two clear spaces seen on a lateral chest radiograph where the lungs meet behind the sternum (the first clear space); the second clear space being the retrocardiac space where the lungs meet behind the heart (Figure 1). Anterior clear space is its synonymous counterpart due to its inherent increased translucency formed by the meeting zone of two lungs behind the sternum. The RSS is normally less than 3 cm deep. For simple understanding, the region should be seen as a part of the anterior mediastinum just behind the sternum between the lungs in the centre of the thorax from the thoracic inlet to the central tendon of the diaphragm [1].
Figure 1.

Lateral chest radiograph shows retrosternal space (RSS), which is the region posterior to the sternum and anterior to the ascending aorta.
Loss of translucency of this region on lateral X-ray indicates local pathology with a diverse group of differential diagnoses, ranging from benign infective/non-infective origin to vascular and neoplastic etiology. On the other hand, widening of this region indicates emphysema. While lateral radiographs show indirect signs of retrosternal pathology, computed tomography (CT) delineates well the nature and extent of retrosternal lesions
This pictorial review presents a comprehensive imaging spectrum of various RSS pathologies followed by a brief description of image-guided retrosternal lesion biopsy/cytology.
Thyroid masses
Less than 5% of enlarged thyroid glands have mediastinal extension producing a commonly used however non-specific term known as ‘retrosternal goiter’. Most of them represent downward extension of non-toxic multinodular colloid goiter or, occasionally an adenoma or carcinoma.
On chest radiograph, the thyroid mass appears as a well-defined round or oval soft tissue mass with or without calcific foci in the superior part of the anterior or middle mediastinum fading into the neck (Figure 2). Thyroid masses are usually anterior and lateral to the trachea which may cause lateral displacement and compression of the trachea. The tracheal displacement depends on the location of the mass. Posteriorly placed masses (approximately 25% of the goiter) often separate the trachea and the esophagus, and such separation by a localized mass rising into the neck is virtually diagnostic of a thyroid mass.
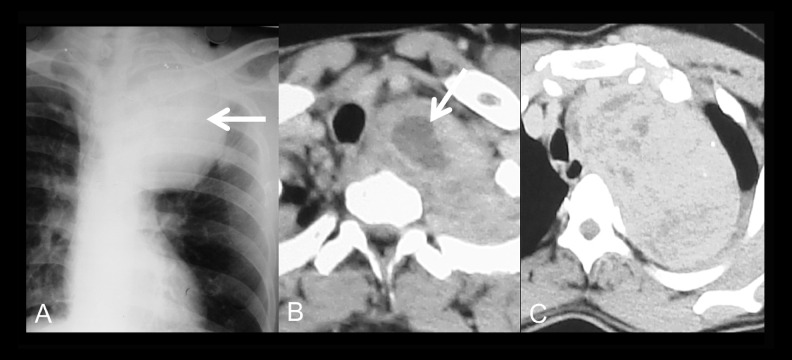
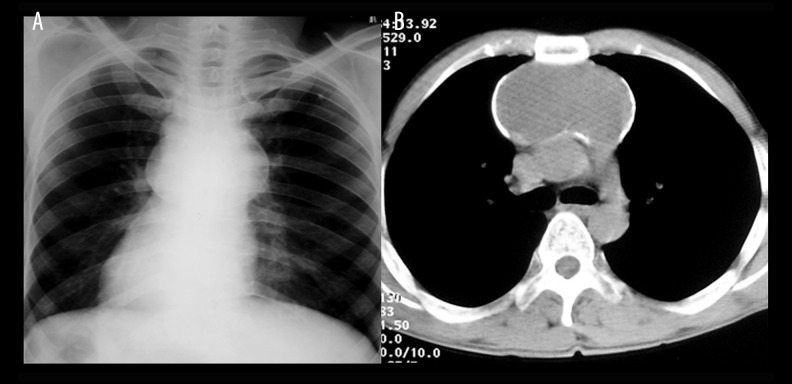
Figure 2.
(A) Biopsy-proven thyroid cancer with retrosternal extension. Chest radiograph postero-anterior view shows a large anterior mediastinal mass with tracheal deviation (arrow). (B, C) Axial CT sections show a large thyroid mass with areas of necrosis ( white arrow, B) extending into RSS.
CT is often used for determination of lesion extent and for its characterization following a neck ultrasound. A high-attenuation paratracheal mass showing continuity with the thyroid gland invariably suggests a thyroid origin. Distinguishing benign from malignant masses is not possible on CT or MRI [1].
Thymic masses
A normal thymus gland is the commonest cause of an RSS abnormality in infants. Pathological enlargement of the thymus gland can be due to a number of causes. Thymoma is the most common cause in adults [1].
Thymoma
Thymoma is usually seen as focal well-defined RSS asymmetric swelling with homogenous density and uniform contrast enhancement. Calcification or cystic changes may be seen. Diagnosing thymoma before the age of 30 is relatively difficult because the normal gland is variable in size. Pleural invasion and remote pleural metastases are signs of invasive thymoma [1].
Thymic carcinoma
These are typically large, heterogeneous masses containing areas of necrosis and calcification demonstrating evidence of invasion of adjacent structures (Figure 3) [2].
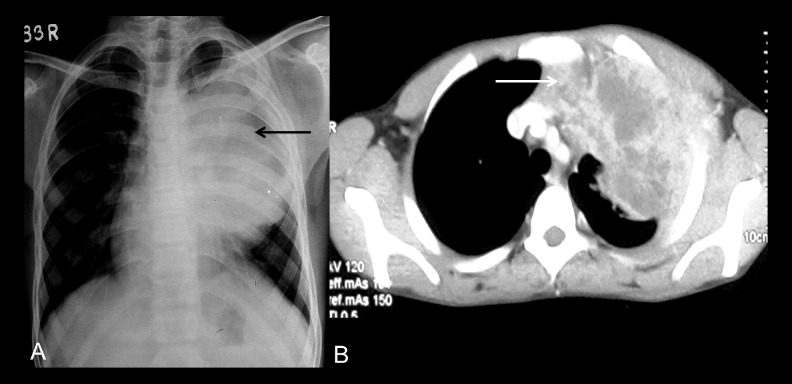
Figure 3.
(A) Thymic carcinoma: Chest radiograph posteroanterior view shows well-defined mediastinal mass. (B) Axial CT section shows a thymic mass with necrosis located in the retrosternal location (white arrow), which proved to be a thymic carcinoma.
Thymic lymphoma
It is usually a part of a generalized disease, most commonly associated with Hodgkin’s lymphoma compared to non-Hodgkin’s lymphoma. The imaging features are the same as those of thymoma and in an advanced bulky disease thymic involvement cannot be differentiated from confluent lymph node enlargement (Figure 4).
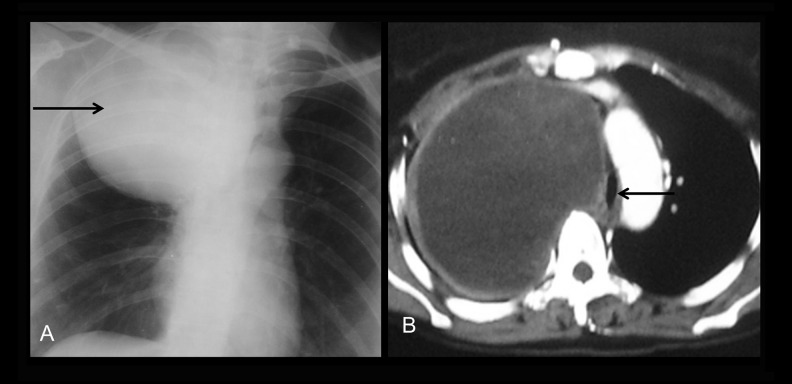
Figure 4.
(A) Thymic lymphoma: Lateral chest radiograph shows a mass in RSS obliterating retrosternal lucency (arrow). (B) Thymic lymphoma: Axial CT section shows a homogenously-attenuating lymph node mass in RSS encasing the aortic arch (arrow) and superior vena cava (curved arrow).
Thymic carcinoid
Although histologically distinct from thymoma, radiologically it is indistinguishable from thymoma unless it is associated with ectopic hormone production (Figure 5) [2].
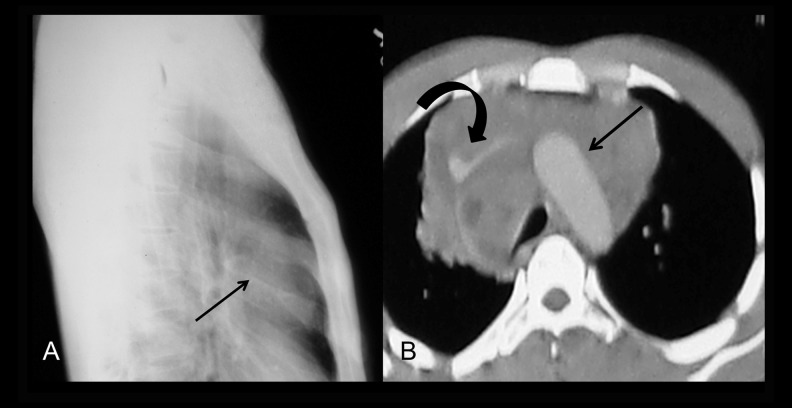
Figure 5.
(A) Thymic carcinoid: Chest radiograph posteroanterior view shows a large anterior mediastinal mass (arrow). (B) Axial CT section revealed a large thymic mass with calcific focus within (arrow), which proved to be thymic carcinoid on biopsy.
Thymolipoma
It is a rare tumor with age range 3–60 years. It can grow to a very large size and mould itself to the mediastinum mimicking cardiomegaly or lobar collapse on X-ray. CT/MRI shows fatty nature of the mass with islands of the thymus and fibrous septa running through the lesion (Figure 6) [3].
Figure 6.
Thymolipoma: Axial CT section shows a large, insinuating retrosternal mass with areas of fat (arrow) suggesting thymolipoma.
Thymic cyst
It is classified as congenital (most common), degenerative/inflammatory, and neoplastic. Congenital thymic cysts are unilocular with homogenous water attenuation. Multilocular cysts are postulated to be inflammatory in nature. Degenerative cystic change in thymic neoplasm occasionally simulates a congenital cyst and requires histological confirmation (Figure 7) [4].
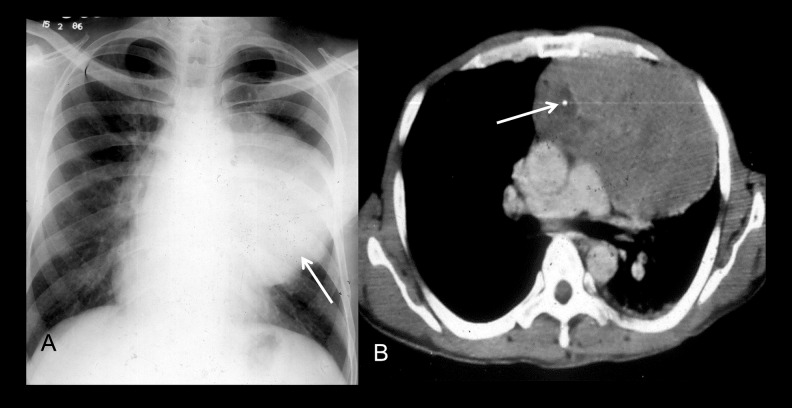
Figure 7.
(A) Thymic cyst: Chest radiograph posteroanterior view shows a well-defined calcified anterior mediastinal mass. (B) Thymic cyst: Axial CT section revealed a cystic thymic lesion (arrow) with calcified wall.
Thymic hyperplasia
Myasthenia gravis and thyrotoxicosis are the two common clinical diagnoses associated with thymic hyperplasia apart from rebound thymic hyperplasia which occurs on recovery from stress/sepsis or cessation of steroid/chemotherapy. Usually both lobes are uniformly enlarged, although occasionally it may mimic a thymic mass (Figure 8). Ultrasound can show the ‘starry sky pattern” of the normal thymus while MRI can show signal drop on opposed-phase images to confirm thymic hyperplasia.
Figure 8.
Thymic hyperplasia: Axial CT section reveals a symmetrically enlarged thymus (arrow) following cessation of steroid therapy consistent with thymic hyperplasia.
Germ Cell tumor (GCT)
GCT is usually seen in second to fourth decades. They arise within or in intimate contact with the thymus. GCT includes mature teratoma, a benign and the most common mediastinal GCT, and a number of malignant forms, the most common type being seminoma (Figure 9). Mature teratomas are sharply circumscribed lesions with presence of fat and/or calcification. Cystic component may predominate (Figure 10).
Figure 9.

Seminoma: Axial CT section shows a well-defined homogenously-enhancing mass which was a biopsy-proven seminoma
Figure 10.

Axial CT section shows a large RSS mass with fatty areas within (arrow) which proved to be teratoma.
Malignant GCTs are large poorly circumscribed masses. Fat and calcification are usually not seen. Elevation of serum markers like beta-human chorionic gonadotropin (β-hcg) and alpha fetoprotein help in distinguishing them from thymoma and lymphoma. Almost 60% of seminomas present with lung or extrathoracic metastases [5].
Bronchogenic cyst
Bronchogenic cysts are the most common type of foregut cysts. They are most commonly located in right paratracheal/carinal location and a retrosternal location is an uncommon site. On CT it appears as a thin-walled fluid-attenuating lesion with or without wall calcification. Sometimes it may be hyperdense due to protein contents or milk of calcium (Figure 11) [6].
Figure 11.
(A) Bronchogenic cyst: Chest radiograph postero-anterior view shows a large mediastinal mass. (B) Axial CT section shows a large cystic lesion in RSS closely abutting the trachea (arrow). This was a bronchogenic cyst on histopathology.
Lymphangioma
RSS lymphangioma is an exceedingly rare entity in adults. They are frequently discovered incidentally on imaging. CT scan shows unilocular/multilocular cystic attenuation lesion and can tell about the vascular relation and exact anatomical extension of the cysts. Complete removal of the cyst is the treatment of choice. However, owing to the infiltrative nature of the lesion, there is a high possibility of post-operative recurrence [7].
Retrosternal abscess
It is usually seen as walled-off discrete fluid or air – fluid collection. Retrosternal fluid collection and foci of air are normal in the first 20 days in sternotomy cases. So de novo appearance or progressive increase of air collection in absence of other explanation is required for diagnosis.
Mediastinal hematoma
In patients with blunt chest trauma, early diagnosis of rerosternal hematoma (ill-marginated high-attenuation soft tissue) is important, because it could be associated with thoracic vessel injury. Subacute or chronic hematoma may be of low attenuation and can appear cystic with fluid-fluid level sometimes.
Examples of other retrosternal cystic lesions are pericardial cyst and parathyroid cyst. Cystic degeneration of anterior mediastinal neoplasms, post-radiotherapy residual thymic cyst of mediastinal lymphoma, and predominant cystic change in the retrosternal goiter may also mimic a pure cystic lesion. Although rare, hydatid cyst should be considered in the differential diagnosis of mediastinal cystic lesions especially in endemic regions.
Mesenchymal tumor
More than half of mediastinal mesenchymal tumors are malignant and include lipoma, liopsarcoma and fibrosarcoma. Liopmas are characterized by the presence of fat with or without thin septa. Enhancing soft tissue along with mass effect and invasion of adjacent structures help differentiating liposarcoma from its benign counterpart (Figure 12) [8].
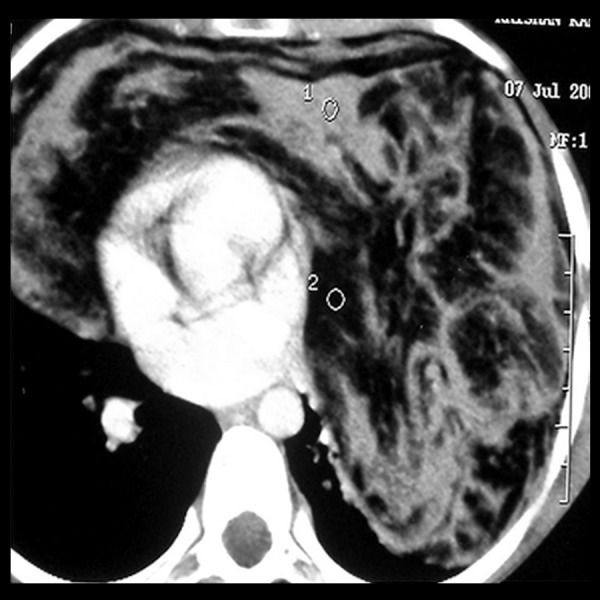
Figure 12.
Liposarcoma: Axial CT section shows a large, heterogeneously-enhancing, necrotic mass occupying RSS and most of the left hemithorax (arrow). This was a biopsy-proven case of proven liposarcoma.
Vascular lesion
Aortic and subclavian artery and ventricular aneurysms, right ventricular enlargement and cardiac/pericardial masses may also obliterate the retrosternal space (Figure 13).
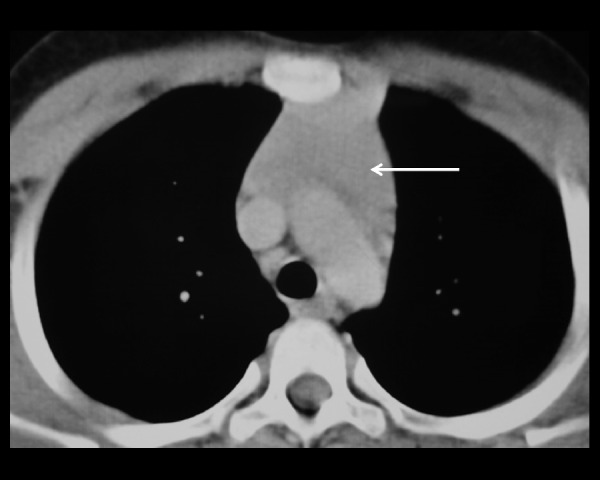
Figure 13.
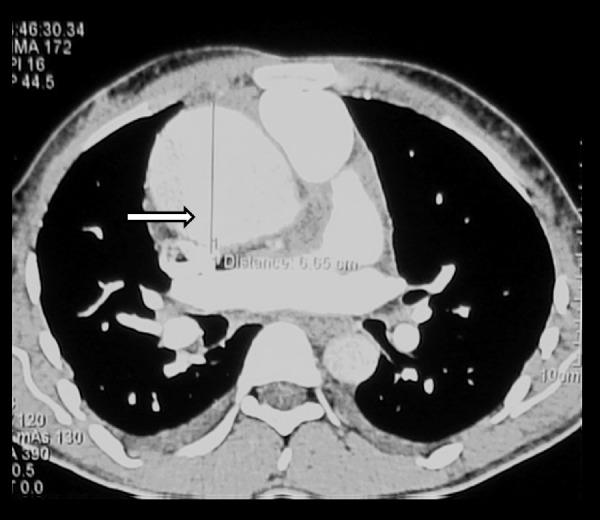
Ascending aortic aneurysm: CT axial section shows a dilated ascending aorta (6 cm in diameter). This can cause obliteration of RSS on chest radiograph and present as an RSS mass.
Lymphadenopathy
Lymphadenopathy of inflammatory/infective origin such as tuberculosis and sarcoidosis (Figure 14) or non-inflammatory/neoplastic nodal lesions (lymphoma or metastatic) may present as predominant retrosternal lesion.
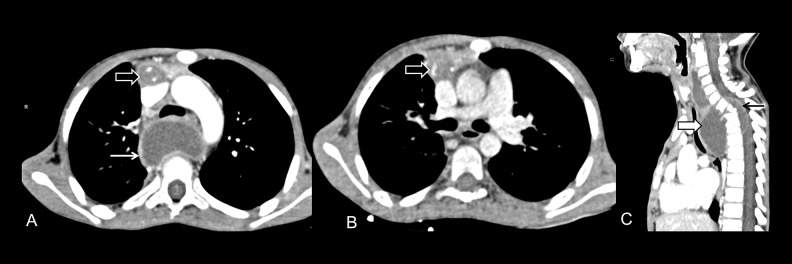
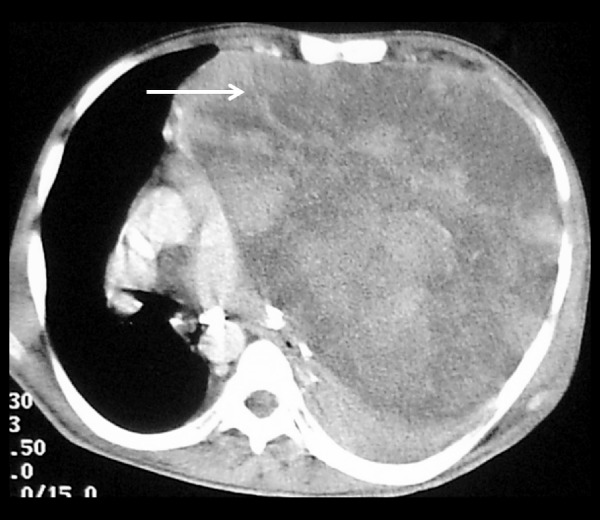
Figure 14.
(A, B) Tuberculosis: Axial CT sections show necrotic conglomerate nodes with abscess formation in the retrosternal region (black block arrow) along with a paravertebral abscess (white arrow). (C) Sagittal reformatted image shows Pott’s spine with paravertebral abscess (white block arrow) with epidural extension (black arrow).
Miscellaneous
Bony lesions
Most sternal tumors represent metastases from the breast, lung, kidney, or thyroid. Primary sternal tumors are uncommon. Chondrosarcoma is the most common primary malignant sternal tumor while osteosarcoma is rare. Other sternal tumors include plasmacytoma, multiple myeloma, lymphoma (Figure 15) [9].
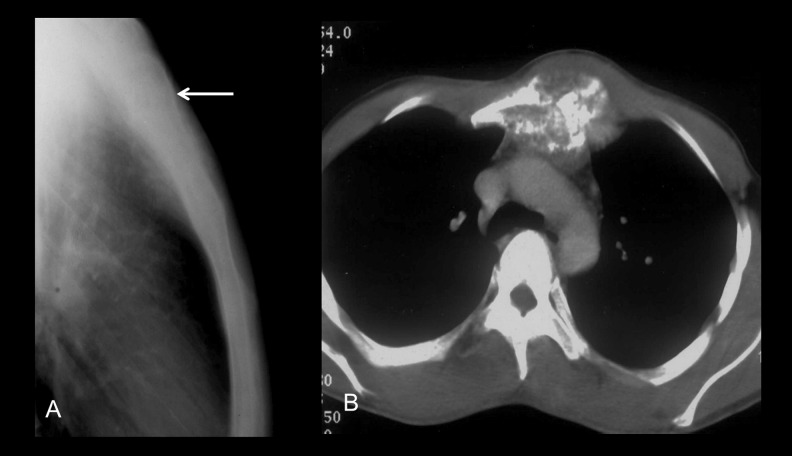
Figure 15.
(A) Chondrosarcoma of the sternum: Lateral view of the sternum showing a lytic bony lesion involving the upper sternum (arrow). (B) Chondrosarcoma of the sternum: Axial CT scan reveals a lytic expansile sternal bony lesion with calcification, extending into RSS (arrow).
Pleural tumors
Masses arising from the mediastinal pleura may project into RSS and may mimic an RSS mass. Although diffuse malignant pleural mesothelioma is the most common primary pleural tumor, involvement of the pleura with metastatic disease is more frequent [10].
Lung mass mimicking retrosternal lesion
Sometimes, a lung mass located in the anterior segment of the right upper lobe, medial segment of the right middle lobe or lingula may mimic a retrosternal mass
Conclusions
Majority of anterior mediastinal lesions are located in the retrosternal space which can be diagnosed with substantial accuracy by computed tomography excluding unlikely diagnoses to a great extent.
References
- 1.Mac Donald SLS, Padley S. The mediastinum, including the pericardium. In: Adam A, Dixon AK, Grainger RG, Allison, editors. Diagnostic Radiology. China: Elsevier; 2007. pp. 243–68. [Google Scholar]
- 2.Do YS, Im JG, Lee BH, et al. CT findings in malignant tumors of thymic epithelium. J Comput Assist Tomogr. 1995;19:192–97. doi: 10.1097/00004728-199503000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Chew FS, Weissleder R. Mediastinal thymolipoma. Am J Roentgenol. 1991;157:468. doi: 10.2214/ajr.157.3.1872228. [DOI] [PubMed] [Google Scholar]
- 4.Garin AH, Sagel SS. Mediastinum. In: Lee JKT, Sagel SS, Stanley RJ, Heiken JP, editors. Computed Body Tomography with MRI correlation. Philadelphia: Lippincott Williams and Wilkins; 2006. pp. 311–419. [Google Scholar]
- 5.Nichols CR. Mediastinal germ cell tumor: Clinical features and biologic correlates. Chest. 1991;99:472–79. doi: 10.1378/chest.99.2.472. [DOI] [PubMed] [Google Scholar]
- 6.McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, et al. Bronchogenic cyst: imaging features with clinical and histopathological correlation. Radiology. 2000;217:441–46. doi: 10.1148/radiology.217.2.r00nv19441. [DOI] [PubMed] [Google Scholar]
- 7.Glazer HS, Siegel MJ, Sagel SS. Low attenuation mediastinal masses on CT. Am J Roentgenol. 1989;152:1173–77. doi: 10.2214/ajr.152.6.1173. [DOI] [PubMed] [Google Scholar]
- 8.Boiselle PM, Rosad-de-christenson ML. Fat attenuation lesions of mediastinum. J Comput Assist Tomogr. 2001;25:881–89. doi: 10.1097/00004728-200111000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Restrepo CS, Martinez S, Lemos DF, et al. Imaging appearances of the sternum and sternoclavicular joints. Radiographics. 2009;29:839–59. doi: 10.1148/rg.293055136. [DOI] [PubMed] [Google Scholar]
- 10.Hussein-Jelen T, Bankier AA, Eisenberg RL. Solid pleural lesions. Am J Roentgenol. 2012;198:512–20. doi: 10.2214/AJR.11.7626. [DOI] [PubMed] [Google Scholar]