Abstract
The Royal College of Physicians report Acute medical care: the right person, in the right setting–first time advocates the introduction of a standardised NHS Early Warning Score (NEWS).1 Recommendations for the optimum scoring system have been released by NHS Quality Improvement Scotland (NHS QIS) and the National Institute for Health and Clinical Excellence (NICE). This study reviewed clinical practice in London and Scotland against national guidelines. All hospitals responsible for acute medical admissions completed a telephone survey (n=25 London; n=23 Scotland). All used an early warning system at point of entry to care. Eleven different systems were used in London and five in Scotland. Forty per cent of London hospitals and 70% of Scottish hospitals incorporated the minimum data set recommended by NICE. Overall, Scotland was closer to achieving standardisation. If NEWS is implemented, consideration of the NHS QIS approach may support a more consistent response.
Key Words: acute medicine, early warning scores, national guidelines
Introduction
Early warning systems (EWS) are bedside tools used to assess basic physiological parameters to identify patients with potential or established critical illness.2 Evidence suggests that they may predict risk of intensive care admission, death and length of hospital stay.3,4 They are alternatively described as physiological track and trigger systems (TTS).
Currently, there are several hundred unique yet similar TTS in use worldwide.5 These can be broadly classified into single parameter, multiple parameter, aggregate-weighted and combination systems.2 Single parameter systems are based upon periodic observation of vital signs, measured against predefined thresholds of acceptability, which prompt a response when any threshold is crossed. Multiple parameter systems require more than one threshold to be crossed (ie an abnormality in two or more physiological parameters) to prompt a response. Aggregate-weighted scoring systems (AWSS) assign scores to physiological values which are summed and compared to thresholds for response. Combination systems link single or multiple parameter systems with AWSS.
Many hospitals in the UK have developed their own TTS, which vary in reliability, validity and utility.6 These systems incorporate diverse physiological variables and thresholds of acceptability often based on clinical intuition rather than rigorous derivation and validation methodologies.7 There is concern that UK hospitals rely on subjective preferences and rarely look beyond their own institutions for the creation of scoring tools.8 Standardisation of TTS across the NHS has been highlighted as a focus for improvement, to ensure that patients receive prompt, appropriate care for the severity of their illness and to facilitate staff training.
In Scotland, the 2004 report of the NHS Quality Improvement Scotland (NHS QIS) Emergency Medical Admissions Scoping Group proposed the introduction of a Scottish Early Warning System (SEWS) and produced standardised documentation for use in pre-hospital and hospital care, staff training and audit. Their specific recommendations were for an AWSS with a colour-coded chart and a defined response algorithm.9 Their recommended scoring parameters were heart rate, respiratory rate, systolic blood pressure, level of consciousness, oxygen saturation, temperature and urine output.
Subsequently, in 2007, the Acute Medicine Task Force of the Royal College of Physicians (RCP) made recommendations for the development of an NHS Early Warning Score (NEWS) to be used at all stages in the acute medicine pathway, with the recording of a minimum clinical data set.1 The National Institute for Health and Clinical Excellence (NICE) recommend that the minimum clinical data set should comprise the SEWS parameters excluding urine output, incorporated into a multiple parameter or aggregate weighted scoring system, linked to a graded response strategy.10
Before NEWS can be launched across the UK, further work is required to develop a specific TTS, validated for diagnostic accuracy, reproducibility, ease of use and acceptability to users. It appears sensible that NEWS will reference systems already in clinical practice. The Department of Health and the RCP have evaluated TTS use across the UK.2,11 The results suggest that TTS uptake is widespread, however, the data are of limited use due to the time which has passed since its acquisition2 and the relatively small sample sizes.11
There is a requirement for up-to-date, detailed information about the individual scoring systems in current usage and how far the NHS is from adopting a unified approach. Such information will facilitate delivery of a more consistent approach to NEWS, based on evidence of existing and best practice.
Aims
This study was undertaken to review the use of TTS in all hospitals admitting acute medical patients in London and Scotland, and to compare current practice with national guidelines. London was selected as a model for England since its population size and number of hospitals is comparable to Scotland. This study forms part of a wider review by the Society of Acute Medicine of the use of TTS within UK hospitals.
Methods
All hospitals in London and Scotland with acute medical units (AMUs) were identified from www.nhs.uk. London was defined by the boundaries of the Greater London boroughs. The research team conducted a telephone survey of senior nursing staff on each AMU to ascertain their routine recording and charting of patient physiological parameters at admission. Telephone surveys were performed for London between 13 and 20 July 2010 and for Scotland between 1 and 8 September 2010. A set of audit standards was derived from recommendations produced by the NHS QIS, NICE and the RCP1,9,10 against which the survey responses were compared. Telephone responses were verified with faxed copies of admission observation and early warning charts. Where telephone answers differed from the faxed charts, information from the latter was used. Compliance with the audit standards was compared between London and Scotland using the phi coefficient for 2×2 contingency tables. Cohen's guidelines for the description of effect size as small (phi=0.1), moderate (phi=0.3) or large (phi=0.5) were adopted.12
Results
All hospitals with AMUs were identified and participated in this study; 25 in London and 23 in Scotland (ie 100% response rate). All hospitals use a variant of TTS. Adherence to the audit standards for TTS is documented for both regions in Table 1.
Table 1.
Audit standards and compliance.
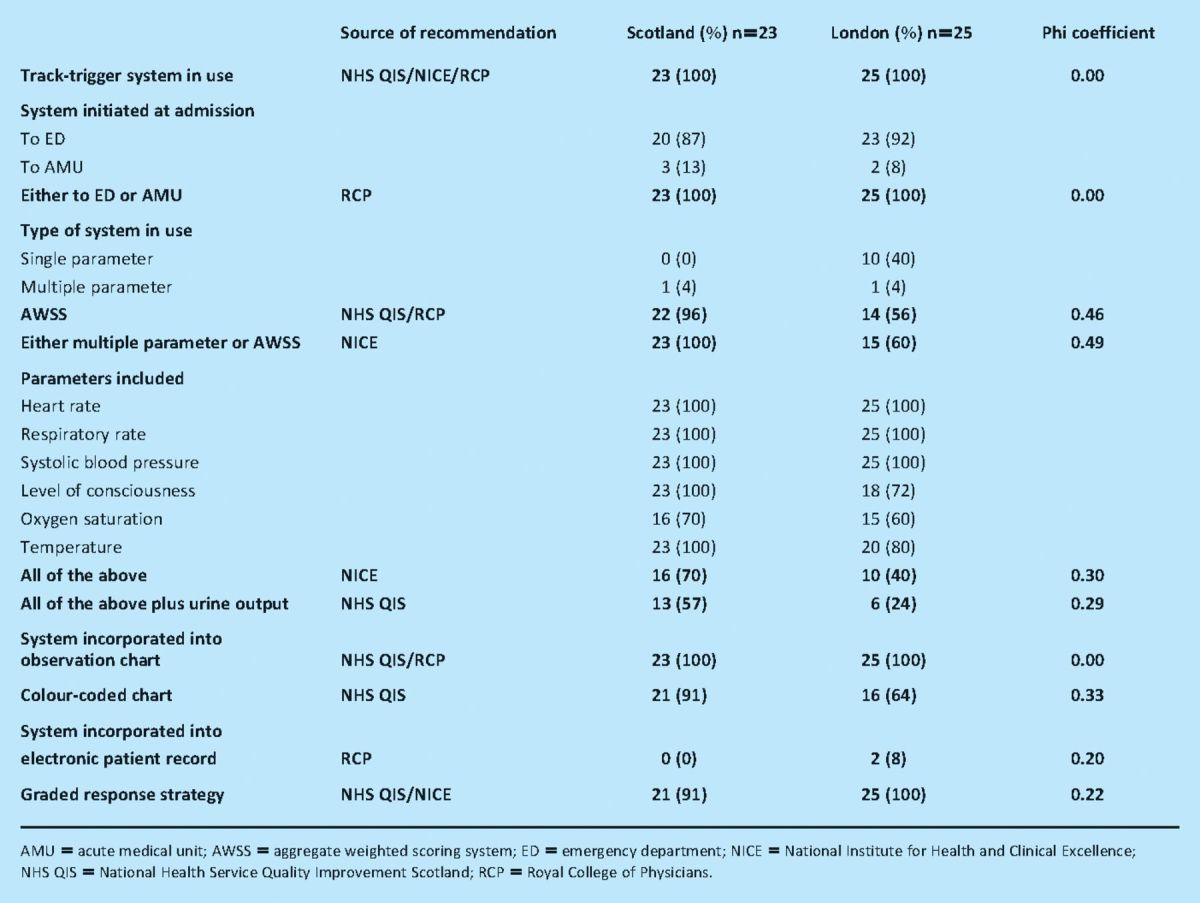
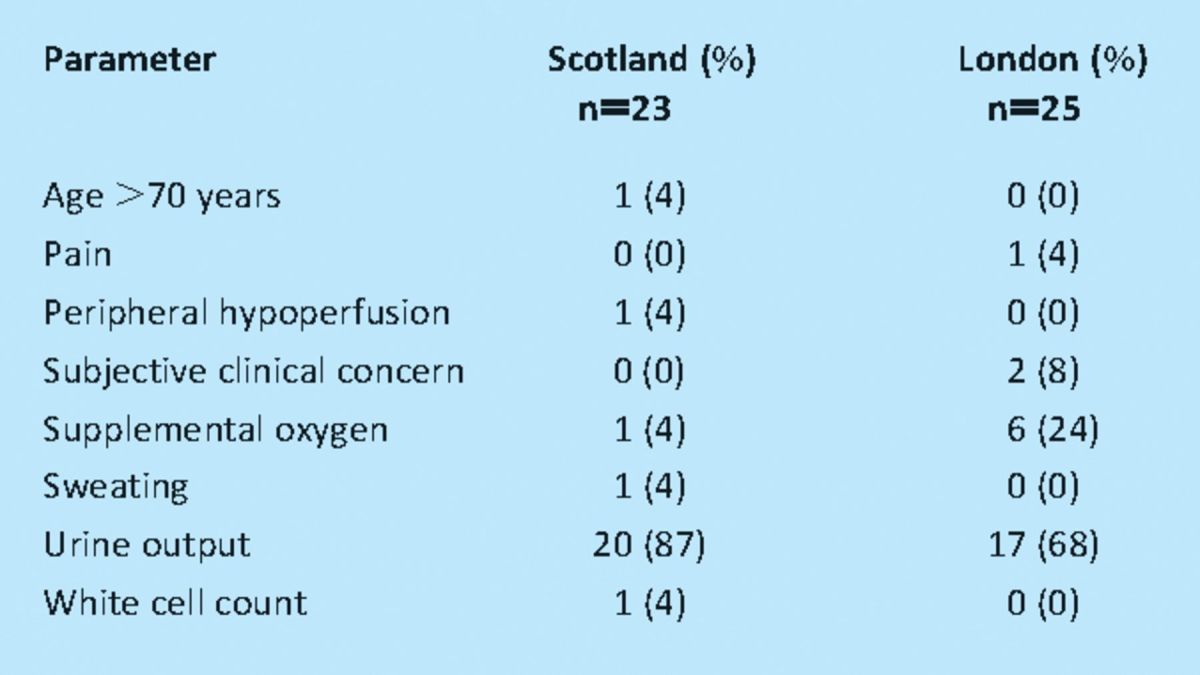
Eleven different systems (measured by the number of different combinations of trigger parameters) are in use in London, compared with five in Scotland. Scottish hospitals are more likely to utilise the minimum data sets specified by NICE and the NHS QIS than London hospitals (Table 1). The phi coefficient for the two regions is 0.30 for adherence to NICE guidance and 0.29 for adherence to NHS QIS guidance, indicating moderate differences between London and Scotland, with Scottish hospitals performing better. Twenty one (91%) of the hospitals in Scotland and 17 (68%) in London use triggers additional to those recommended by NICE (Table 2).
Table 2.
Physiological parameters used as triggers in addition to minimum National Institute for Health and Clinical Excellence recommendations.
Adherence to the optimum scoring system (defined as: initiated at admission, either multiple parameter or AWSS; including NICE specified parameters as a minimum data set; within a colour-coded chart; resulting in a graded response strategy) is demonstrated in 14 (61%) hospitals in Scotland and six (24%) in London. The phi coefficient for the two regions is 0.37 indicating a moderate difference in adherence between London and Scotland, with Scottish hospitals achieving greater adherence to the optimum scoring system.
Discussion
The RCP has proposed the introduction of a standardised TTS (NEWS), highlighting the benefits as a means of ‘ensuring full documentation of clinical details, quality of care, safe transfer of care, audit and medico-legal reviews’ and as an aid to training acute healthcare providers through familiarity and consistency of documentation.1
The results of this study confirm that TTS are widely used in the assessment of acute medical admissions, initiated at point of care. Nevertheless, there is marked variation in their nature. There is greater concordance between hospitals and with national guidance in Scotland than in London.1,9,10 Scottish hospitals are closer to the perceived ideal situation of standardised TTS and shared documentation.
In both London and Scotland the majority of TTS in current use are multiple parameter or AWSS. While the evidence supporting one type of TTS over another is inconclusive,6 NICE recommend multiple parameter and AWSS over single parameter systems since these allow for a graded response strategy.10 NICE recognise that AWSS may be optimised to achieve high levels of sensitivity and specificity, thus the higher proportion of AWSS noted in Scotland is advantageous.
A greater range of trigger parameters are used in London than Scotland and fewer London hospitals incorporate the minimum parameters recommended by NICE and the NHS QIS. All hospitals studied include heart rate, respiratory rate and systolic blood pressure. The majority of hospitals include level of consciousness, oxygen saturation, temperature and urine output. A minority of hospitals, predominantly in London, include additional parameters such as requirement for supplemental oxygen and subjective clinical concern.
Of the parameters recommended by NICE and NHS QIS, oxygen saturation (SpO2) is the least utilised in both regions, although uptake is higher in Scotland. SpO2 was not included in the first published early warning score13 and may be omitted from TTS based on this model; SpO2 was included in SEWS.9 Omission of SpO2 may also result from difficulties in determining normal values, which vary according to the presence of chronic disease such as chronic obstructive pulmonary disease and with supplemental oxygen therapy.
All hospitals incorporate TTS into a standard observation chart or computer-based observation record. Although the majority of these charts are colour coded in Scotland and London, the proportion is greater in Scotland. Colour-coded charts provide users with visual cues to support established numerical values for parameters within TTS. They are believed to assist in the recognition of patient deterioration,14 particularly if they are in spectral colour palates.15
Computer-based systems are used in around one in 12 London hospitals but have yet to be introduced to acute trusts in Scotland. The merits of computer-based systems are in the speed and accuracy of recording patient observations16 and in the collation of data to validate and optimise the performance of TTS.17 As part of the NHS IT programme ‘Connecting for health’, it is envisaged that the use of electronic patient records will become more widespread.18
Differences between London and Scotland in concordance with audit standards may reflect several factors; firstly, the timings of national recommendations for TTS promulgated in the two areas. The NHS QIS released guidance in 2004,9 while the RCP and NICE released their guidance three years later effectively giving Scottish hospitals a ‘head start’ to implement change.1,10
Secondly, the NHS QIS released guidance for a specific TTS (SEWS) with standardised documentation, while the RCP and NICE released more general guidance without example documentation. This may have facilitated prompt local uptake of SEWS while individual London hospitals were developing and implementing local versions of TTS.
Thirdly, the Scottish Patient Safety Programme (SPSP), supported by the Scottish Government and coordinated by NHS QIS, promoted the use of SEWS across Scotland. This national programme for standardising care and improving patient outcomes has encouraged collaborative working between trusts and health boards which does not yet occur between London hospitals. Lack of knowledge sharing and organisational learning may have contributed to the greater disparity of London TTS.
The RCP is due to release specific guidance, detailing their NEWS AWSS, validated against a clinical signs database. Their guidance will cover the scoring and weighting applied to the physiological parameters and the clinical responses to the triggers, defining the urgency of response and the clinical competencies required for responders.
The results of this study infer widespread adoption of NEWS and may be enhanced by the provision of a single structured scoring system with associated documentation and a strategy for training, audit and review, as demonstrated by the NHS QIS with SEWS. Engagement with all levels of the NHS through a centralised programme, such as the SPSP, may also support a more consistent response. This study will serve as a benchmark against which progress can be judged.
Limitations
The primary limitation of this study was the restriction to two discrete areas of the UK, meaning generalisation of the results should be made with caution. Furthermore, the data collected represented a snapshot at the time of survey, and many hospitals reported ongoing revision to both their early warning systems and documentation.
Conclusion
At present there is disparity between hospitals in the NHS in the recording and interpretation of basic physiological parameters. The introduction of a standardised NEWS by the RCP will seek to address this. Uptake is likely to be improved when a single score is promulgated with an associated observation chart and appropriate infrastructure is established for staff training and regular review. In Scotland, where such a score has been in existence since 2004, concordance between hospitals and with recommended practice is greater than in London, where more general guidance has been employed.
References
- 1.Royal College of Physicians. Acute medical care. The right person, in the right setting–first time 2007. London: RCP [Google Scholar]
- 2.Department of Health and Modernisation Agency. The National Outreach Report 2003. London: DH [Google Scholar]
- 3.Groarke JD, Gallagher J, Stack J, et al. Use of an admission early warning score to predict patient morbidity and mortality and treatment success. Emerg Med J 2008; 25: 803–6 [DOI] [PubMed] [Google Scholar]
- 4.Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified early warning score in medical admissions. QJM 2001; 94: 521–6 10.1093/qjmed/94.10.521 [DOI] [PubMed] [Google Scholar]
- 5.Jansen JO, Cuthbertson BH. Detecting critical illness outside the ICU: the role of track and trigger systems. Curr Opin Crit Care 2010; 16: 184–90 10.1097/MCC.0b013e328338844e [DOI] [PubMed] [Google Scholar]
- 6.Gao H, McDonnell A, Harrison DA, et al. Systematic review and evaluation of physiological track and trigger warning systems for identifying at-risk patients on the ward. Intensive Care Med 2007; 33: 667–79 10.1007/s00134-007-0532-3 [DOI] [PubMed] [Google Scholar]
- 7.Cuthbertson BH, Smith GB. A warning on early-warning scores!. Br J Anaesth 2007; 98: 704–6 10.1093/bja/aem121 [DOI] [PubMed] [Google Scholar]
- 8.Subbe CP. Better ViEWS ahead? It is high time to improve patient safety by standardizing early warning scores. Resuscitation 2010; 81: 923–4 [DOI] [PubMed] [Google Scholar]
- 9.National Health Service Quality Improvement Scotland. Emergency Medical Admissions Scoping Group final report 2004. Edinburgh: NHSQIS [Google Scholar]
- 10.National Institute for Health and Clinical Excellence. Acutely ill patients in hospital: recognition of and response to acute illness in adults in hospital 2007. London: NICE; [PubMed] [Google Scholar]
- 11.Ward D, Potter J, Ingham J, Percival F, Bell D. Acute medical care. The right person, in the right setting–first time: how does practice match the report recommendations? Clin Med 2009; 9: 553–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen J. Statistical power analysis for the behavioural sciences 1977. New York: Academic Press, 223–5 [Google Scholar]
- 13.Morgan RJM WF, Wright MM. An early warning scoring system for detecting developing critical illness. Clin Intens Care 1997; 8: 100 [Google Scholar]
- 14.Australian Commission on Safety and Quality in Healthcare. Recognising and responding to clinical deterioration: use of observation charts to identify clinical deterioration 2009 [Google Scholar]
- 15.Ratwani RM, Trafton JG, Boehm-Davis DA. Thinking graphically: connecting vision and cognition during graph comprehension. J Exp Psychol Appl 2008; 14: 36–49 10.1037/1076-898X.14.1.36 [DOI] [PubMed] [Google Scholar]
- 16.Prytherch DR, Smith GB, Schmidt P, et al. Calculating early warning scores–a classroom comparison of pen and paper and hand-held computer methods. Resuscitation 2006; 70: 173–8 [DOI] [PubMed] [Google Scholar]
- 17.Prytherch DR, Smith GB, Schmidt PE, Featherstone PI. ViEWS–Towards a national early warning score for detecting adult inpatient deterioration. Resuscitation 2010; 81: 932–7 [DOI] [PubMed] [Google Scholar]
- 18.House of Commons Public Accounts Committee. The National programme for IT in the NHS: progress since 2006 2009. London: Stationery Office [Google Scholar]


