Venous thromboembolism (VTE), encompassing deep vein thrombosis (DVT) and pulmonary embolism (PE), is a major public health issue, with an incidence of 1/1,000 and thousands of VTE-related deaths each year in the UK. The estimated cost of VTE and its complications to the NHS is in excess of £600 million.1 PE is the most common cause of inpatient mortality, and is the leading cause of death in pregnant women. Common risk factors include hospitalisation, surgery, cancer and immobilisation; and in women, combined oral contraceptive use, hormone replacement therapy and pregnancy. Approximately a quarter of VTE episodes are unprovoked, that is without an identifiable precipitant.2
Clinical features of DVT include swelling and pain, pitting oedema, increased warmth and superficial venous dilation of the lower limb. PE may present with or without symptoms of a DVT in addition to chest pain, breathlessness, haemoptysis, syncope, hypotension, tachycardia and hypoxia. Without prompt recognition and treatment, PE can lead to death in up to 30%. Clinical diagnosis of VTE can be challenging and, furthermore, clinically silent episodes are not uncommon.
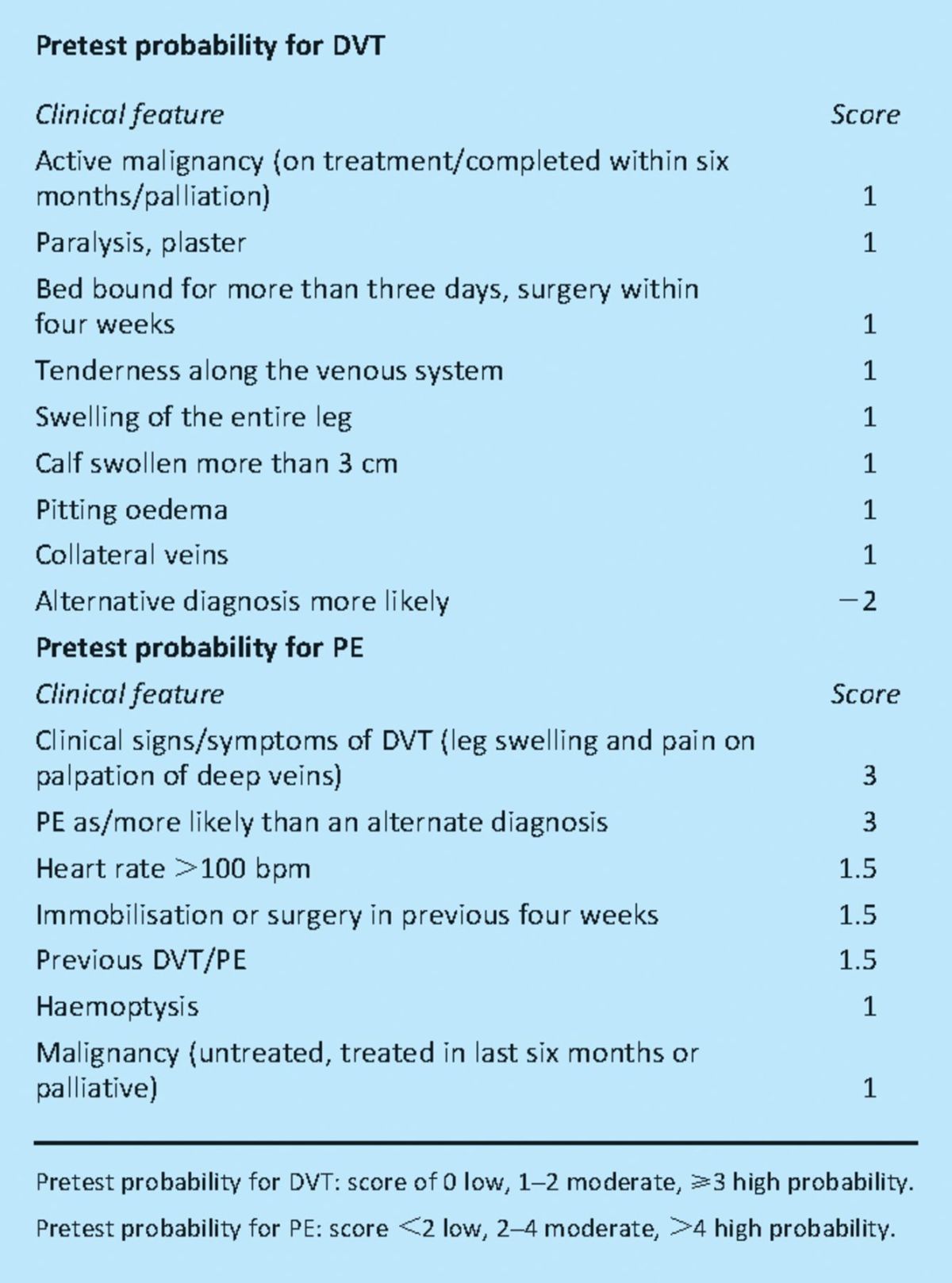
Integrated diagnostic strategies have been demonstrated to be safe, efficacious and cost effective.3 These strategies employ the use of a clinical pretest probability score (Table 1) in combination with D-dimer to inform the need for further diagnostic imaging. Patients at low risk of DVT/PE with a negative D-dimer result (using a high sensitivity assay) require no further investigation. However, those identified as moderate or high probability, or with a raised D-dimer require definitive imaging to confirm or exclude the diagnosis.
Table 1.
Clinical features to determine pretest probability for deep vein thrombosis (DVT) and pulmonary embolism (PE). Adapted with permission from John Wiley & Sons.3
Non-invasive compression ultrasonography is increasingly used first line for investigation of DVT, with advantages over venography including superior safety and portability. Sensitivity can be adversely affected by operator experience and poor views may be obtained in the presence of severe obesity, gross oedema or a plaster cast. However, its sensitivity for symptomatic proximal DVT remains up to 97%.4 Computed tomography (CT) pulmonary angiography is currently accepted as the investigation of choice for PE diagnosis5; its increased resolution allows detection of PE to subsegmental levels, in addition to detection of alternate diagnoses, such as, infection or cancer.
Treatment for VTE is primarily aimed at prevention of clot extension, embolisation and symptom relief, with additional long-term aims of minimising recurrence and preventing post-thrombotic syndrome.6 Anticoagulation is the mainstay of treatment and should be initiated at confirmation of diagnosis or when first suspected if there is a delay in diagnostic imaging. Thrombolysis or surgical thrombectomy/embolectomy should be reserved for selected patients with haemodynamic instability due to massive PE or critical limb ischaemia secondary to DVT.
Low molecular weight heparins (LMWHs) are the preferred agents for initiation of anticoagulation due to improved efficacy, safety and ease of administration with once daily subcutaneous injection.6 Monitoring of the anticoagulant effect is not required routinely with LMWH and rates of early mortality, recurrence and major bleeding are reduced compared to unfractionated heparin, as is the risk of heparin-induced thrombocytopenia. Warfarin should be initiated once the diagnosis of VTE is confirmed, in the absence of contraindications, with a target international normalised ratio (INR) of 2.5. LMWH should continue for at least five days and until the INR has been therapeutic for 24 hours. There are a number of emerging oral anticoagulants which do not require monitoring for anticoagulant effect. Dabigatran, a direct thrombin inhibitor and rivaroxaban, a direct Xa inhibitor are currently in advanced stages of investigation in the setting of VTE treatment and hold promise.7
Anticoagulation should be continued for at least three months to prevent early recurrent thrombosis.6 Extension of therapy beyond this period should be based on the presence or absence of precipitating factors at VTE diagnosis. The risk of recurrence is low if VTE was provoked by major surgery, approximately 10% at two years if provoked by a transient risk factor and up to 25% at two years in the absence of recognised risk factor8 and/or in the presence of active cancer. Individualised assessment should be undertaken to consider the benefit of continuing anticoagulation to prevent recurrence, while taking into account risk factors for bleeding, patient preference and compliance. Patients should be counselled at completion of anticoagulation regarding their individual risk of recurrence and risk reduction strategies. All patients should be counselled regarding maintenance of a healthy lifestyle with weight reduction and smoking cessation advice as appropriate. Thromboprophylaxis should be provided in future periods of risk particularly during hospitalisation and the postoperative period.
Post-thrombotic syndrome (PTS) is a common complication following DVT, manifesting in 20–50% of patients. Compression stockings have been demonstrated to halve this risk. Below knee graduated compression stockings, with an ankle pressure of 30–40 mmHg, are recommended for daily wear from as soon as symptoms allow after a confirmed DVT for a duration of at least two years.6
VTE complicating hospitalisation has gained increased recognition in recent years and VTE prevention has been identified as a key patient safety priority. The National VTE Prevention Programme advocates a systematic approach to reducing hospital-associated thrombosis (HAT). It is now national policy that all adult patients are assessed for risk of VTE on admission backed up by a national VTE goal linked to a financial incentive and national mandatory VTE risk assessment data collection.9 The National Institute for Health and Clinical Excellence has published clinical guidelines for reducing risk in all hospitalised patients accompanied by a VTE prevention standard.10 Widespread adoption of universal VTE risk assessment on admission to hospital and appropriate provision of thromboprophylaxis should lead to a significant reduction of preventable episodes of HAT.
References
- 1.Arya R. Venous thromboembolism prevention: a patient safety priority 2010. London: King's Thrombosis Centre; www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_101398 [Google Scholar]
- 2.Heit JA, Silverstein MD, Mohr DN, et al. The epidemiology of venous thromboembolism in the community. Thromb Haemost 2001; 86: 452–63 10.1161/ATVBAHA.108.162545 [DOI] [PubMed] [Google Scholar]
- 3.Wells PS. Integrated diagnostic strategies for diagnosis of venous thromboembolism. J Thromb Haemost 2007; 5: S41–50 10.1111/j.1538-7836.2007.02493.x [DOI] [PubMed] [Google Scholar]
- 4.Kearon C, Julian JA, Math M, Newman TE, Ginsberg JS. Noninvasive diagnosis of deep vein thrombosis. Ann Int Med 1998; 128: 663–77 10.1055/s-2001-12842 [DOI] [PubMed] [Google Scholar]
- 5.Agnelli G, Becattini C. Acute pulmonary embolism. NEJM 2010; 363: 266–74 10.1056/NEJMra0907731 [DOI] [PubMed] [Google Scholar]
- 6.Kearon C, Kahn SR, Agnelli G, et al. Antithrombotic therapy for venous thromboembolic diseases: American College of Chest Physicians evidence-based clinical practice guidelines (8th edn). Chest 2008; 133: 454–545 [DOI] [PubMed] [Google Scholar]
- 7.Roberts LN, Arya R. New anticoagulants for the prevention and treatment of venous thromboembolism. Curr Vasc Pharmacol 2010; 8: 373–82 [DOI] [PubMed] [Google Scholar]
- 8.Baglin T, Luddington R, Brown K, Baglin C. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: prospective cohort study. Lancet 2003; 362: 523–6 10.1016/S0140-6736(03)14111-6 [DOI] [PubMed] [Google Scholar]
- 9.Department of Health. The operating framework for 2010/11 for the NHS in England 2009. London: Department of Health/NHS Finance, Performance and Operations; www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/@sta/@perf/documents/digitalasset/dh_110159.pdf [Google Scholar]
- 10.National Collaborating Centre for Acute Care. Venous thromboembolism: reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in hospitalised patients 2009. London: National Clinical Guideline Centre–Acute and Chronic Conditions [Google Scholar]


