Key points
Dengue is the most widely distributed mosquito-borne viral infection of humans, affecting an estimated 100 million people worldwide each year, with 40% (2.5 billion) of the world's population estimated to be at risk for infection
Dengue should be considered in any patient with fever, particularly if there is a recent travel history to endemic regions
Dengue severity exists as a continuous spectrum of dengue fever through to severe dengue
The most important of the many clinical features associated with severe dengue, from the standpoint of threat to life and guiding clinical intervention, is increased vascular permeability leading to the dengue shock syndrome
During the critical phase of illness, regular review (every 15–30 minutes) of vital signs is essential (pulse rate, blood pressure, peripheral temperature and haematocrit)
The mainstay of treatment is prompt, vigorous, but judicious fluid resuscitation. If it is appropriate to institute volume resuscitation at an early stage, shock is usually reversible
Careful clinical judgement is required throughout the patient's stay in hospital to maintain an effective circulation whilst assiduously avoiding fluid overload
Dengue is the most rapidly spreading arboviral disease globally, occurring in over 100 countries. The burden of dengue has increased at least fourfold over the last three decades: it is estimated that there are 50 million dengue infections and 616,000 disability-adjusted life years annually. Approximately 500,000 severe dengue cases are reported annually, with 20,000 dengue related deaths in 2002. These figures are inevitably a gross underestimate as many countries do not report their data.
The clinical management and outcome of patients with dengue still varies widely from country to country. This is particularly true as dengue emerges in new areas of the world where the public health systems are not experienced in the prevention of the disease, or the surge capacity in clinics and hospitals is not available to deal with the sudden increase in the number of patients and the clinical experience is limited. In these settings, mortality and morbidity are often higher than in other regions where dengue has been endemic for decades.
Dengue cases have been seen more frequently outside endemic areas in recent decades. This is due to the enormous shift to urban living, increase in tourism, business related travel and global deployment of military and international non-governmental organisations. No vaccine or prophylaxis is available.
Epidemiology
Dengue is now classified by the World Health Organization (WHO) into dengue fever and severe dengue (Table 1). Full details of the 2009 WHO scheme can be found online (see key references).
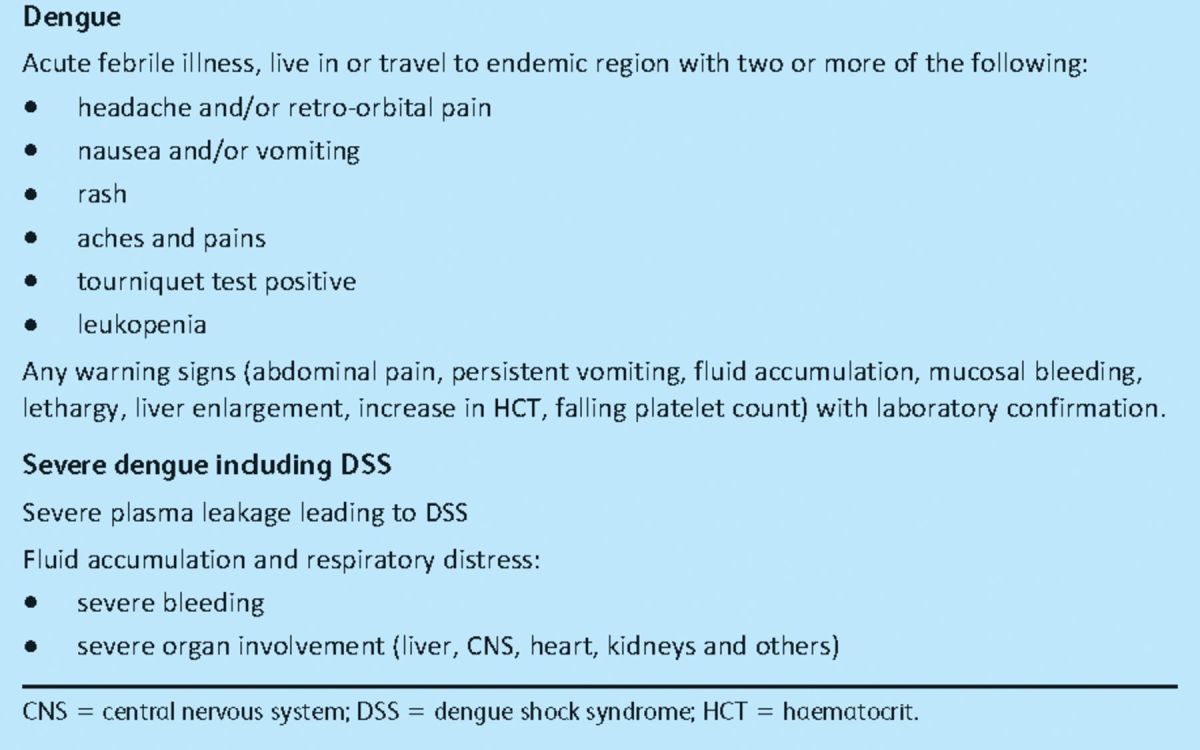
Table 1.
World Health Organization (WHO) case classification.
The most important feature of severe dengue is increased capillary permeability leading to dengue shock syndrome (DSS). When shock becomes established, mortality rates of >10% have been reported, although they can be less than 1% when patients are looked after by experienced clinical teams.
The dengue virus is a single stranded, positive-sense RNA virus approximately 11 kb in length. It is a member of the Flavivirus genus, which also includes yellow fever, Japanese encephalitis and West Nile virus. There is considerable genetic diversity in the dengue virus family with four serotypes (Den I, II, III and IV).
The major global vector is Aedes aegypti. The adult mosquito is strongly anthropophilic, prefers resting in sheltered dark areas inside houses, with a diurnal feeding pattern usually peaking mid-morning and late afternoon.
Pathophysiology
The most widely cited hypothesis to explain the features of severe dengue is increased viral replication due to enhanced infection of monocytes in the presence of pre-existing antidengue antibodies at subneutralising level (antibody-dependent immune enhancement).
This observation, which has strong epidemiologic and in vitro experimental evidence in support, argues that moderate viraemia is controlled in asymptomatic dengue infection. The host immune system develops long-lasting immunity to the serotype of the infecting strain and short-lived cross-protection against heterologous serotypes. The levels of cross-protective antibody directed against the heterologous serotypes fall below neutralising levels after a few months. From this stage onward, infection with a second heterologous strain may result in increased viral uptake via FcÁ receptors into monocytes and enhanced viral replication. Severe disease has been reported during primary infections, however, and not all secondary infections lead to severe disease, so other theories (viral and host genetic factors) have been suggested to try to explain the complex epidemiologic and immunopathogenetic features.
Clinical features
Dengue fever is a mild, self-limited febrile episode, commonly associated with a rash. It usually begins with fever, respiratory symptoms, anorexia, nausea, vomiting and headache. Back pain, myalgias, arthralgias and conjunctivitis may also occur. The initial fever usually resolves within one week, and a few days later a generalised morbilliform or maculopapular rash may develop. Fever may return with the rash (Figs 1 and 2).
Fig 1.

Acute skin manifestations of dengue: (a) characteristic minor bleeding near injection sites; (b) severe bleeding caused by pressure from blood pressure cuff; (c) rash in established dengue shock syndrome.
Fig 2.
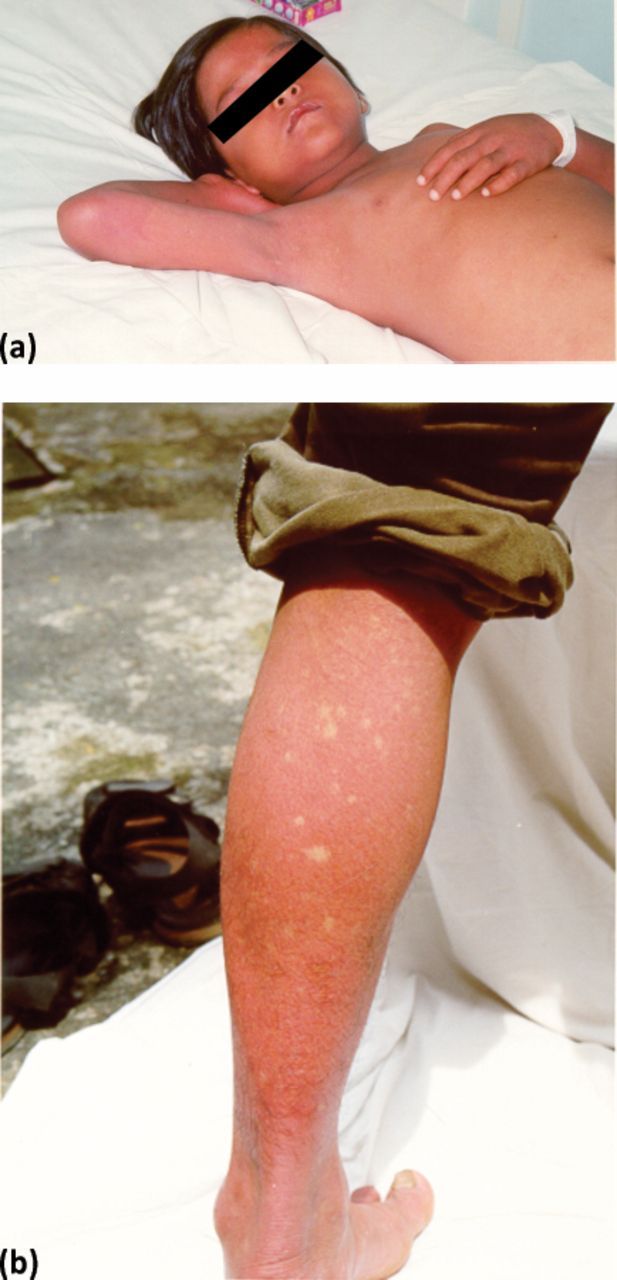
Characteristic skin manifestations in convalescent dengue: (a) early convalescent macular diffuse rash occurring in the first week after recovery; (b) typical convalescent rash with ‘islands of white in a sea of red’.
The two groups of dengue (dengue fever and severe dengue) form part of a continuous spectrum of severity. The most important clinical features of severe dengue are capillary permeability leading to DSS. Other complications include severe mucosal bleeding (and, less commonly, intracerebral and pulmonary haemorrhage), pleural effusions, encephalopathy, pneumonia and liver dysfunction.
Thrombocytopenia is a very common feature in dengue and there is abnormal platelet function. Mild prolongation of prothrombin and partial thromboplastin times with reduced fibrinogen levels is common, but fibrin degradation products have not been found to be elevated to a degree consistent with classic disseminated intravascular coagulation (DIC). Patients with DSS have significant abnormalities in all the major pathways of the coagulation cascade.
Diagnosis
Classic dengue illness can be an easy diagnosis to make in endemic regions with experienced clinical staff and a high prior probability that a febrile illness with rash and thrombocytopenia is caused by dengue. However, most symptoms and signs accompanying dengue infection are common to many febrile illnesses, with few features that reliably discriminate dengue especially early on. Proof of a dengue infection depends on confirmatory reverse transcriptase-polymerase chain reaction (RT-PCR), dengue serology, specific dengue NS1 antigen detection or viral isolation, if available. Serologic confirmation of acute dengue infection relies on the demonstration of specific immunoglobulin (Ig) M and IgG antibodies against dengue in patients' serum.
The differential diagnosis is extensive and varies depending on where the patient is seen, but would include malaria, typhoid, leptospirosis, scrub and murine typhus, septicaemia, other viral haemorrhagic fevers (eg Ebola, Lassa fever), chikungunya, and Rift Valley fever (usually without a rash). A pulse pressure of less than 20 mmHg is one of the early manifestations of shock, usually occurring before the onset of systolic hypotension.
Management
The mainstay of treatment is prompt, but careful, fluid resuscitation. If appropriate volume resuscitation is instituted at an early stage, shock is usually reversible. In some severe cases, and in patients inappropriately resuscitated, patients may progress to irreversible shock and death. Careful clinical judgement is required throughout the patient's stay in hospital to maintain an effective circulation whilst assiduously avoiding fluid overload.
Close attention and regular review (every 15–30 minutes during episodes of shock) of haematocrit (HCT), pulse pressure and peripheral perfusion are essential. For patients with DSS, WHO recommends immediate volume replacement with isotonic crystalloid solutions, followed by the use of plasma or colloid solutions, specifically dextrans, for profound or continuing shock.
Although there are currently no specific drugs for dengue, there is effective treatment based primarily on careful fluid management. Judicious restoration of circulating plasma volume is the cornerstone of therapy for patients with DSS. For uncomplicated dengue fever, less aggressive oral or parenteral fluid therapy is frequently indicated.
Severe dengue and dengue shock syndrome
This section focuses on the management of DSS. Management of unusual complications, such as dengue encephalopathy or fulminant hepatitis is not addressed as it is similar to the standard management.
Patients admitted with established DSS should be cared for in an intensive care or high dependency unit. Extreme care is needed to balance the requirement for intravenous (iv) fluid to maintain plasma volume against the risk of leakage of administered fluid into the interstitial space. The leaked fluid may contribute to the development of pleural effusions, ascites, respiratory compromise and the potential downward spiral towards multi-organ failure, DIC and death. As is often the case in looking after the critically ill, patients with the severest capillary leak syndrome and most at risk of these complications are also those in the greatest need of the most aggressive circulatory support. Getting this balance of fluid resuscitation and ongoing capillary leak right is the most difficult issue in managing patients with DSS.
Assessment
Rapid clinical assessment of pulse, blood pressure (BP), peripheral perfusion, urine output and mental state determines initial management. The results of basic laboratory investigations including HCT (preferably available on the ward) and platelet count are useful, but initiation of treatment must not be delayed pending their availability. Detailed examination should be carried out once resuscitation is in progress.
Features of severe disease
The following features are commonly associated with severe disease and a complicated clinical course:
poor peripheral perfusion
narrow pulse pressure (<10 mmHg) with poor peripheral perfusion
compromised cerebral perfusion (lethargy, irritability, drowsiness or restlessness)
presentation with shock early in the course of the disease (before day 4 of fever)
marked elevation of (or rapidly rising) HCT
pleural effusions or ascites at the time of presentation with shock. Large volumes of fluid must be present to be clinically detectable, implying either recent onset of catastrophic leak or a steady loss of fluid over a longer time before the development of haemodynamic compromise.
Young patients
Severe dengue occurs infrequently in infants, but special care must be taken with the fluid management in this age group. Fluid accounts for a greater proportion of body weight in infants and minimal daily requirements are correspondingly greater. Cardiovascular and renal function are still developing and there is less reserve to cope with disturbance. Finally, capillary beds are intrinsically more permeable than those of older children or adults. All infants must be treated as high risk patients and warrant early intervention with very careful resuscitation and intensive monitoring.
Resuscitation and management
Resuscitation with parenteral fluids should be started immediately after the initial rapid assessment. Reliable iv access must be secured as soon as possible. Rarely, in patients with profound shock, a venous cutdown or insertion of an intra-osseous line may be necessary. All patients with shock or respiratory compromise should receive oxygen by face mask or nasal cannula. A regular schedule of clinical observations (pulse, BP) at least every 30–60 minutes should be instituted, with a detailed record of all fluid intake and output. The HCT should be measured every two hours for the first six hours and thereafter every 4–6 hours until the patient is stable.
For most patients with DSS, resuscitation should be started with an isotonic crystalloid solution (physiologic saline, Ringer's lactate or Ringer's acetate) at a rate of 10–15 ml/kg over one hour. If the patient's clinical condition has stabilised after this time (wider pulse pressure, stable pulse rate, warm peripheries, stable HCT), the rate of fluid administration may be reduced to 10 ml/kg/hr for two hours, then gradually reduced to maintenance levels over the next 6–8 hours. A suitable schedule might be as follows:
10 ml/kg/hr for two hours
7.5 ml/kg/hr for two hours
5 ml/kg/hr for four hours, then
2–3 ml/kg/hr for 24–36 hours.
For most patients, iv therapy can then be stopped, provided that the clinical condition has been stable for 24 hours.
If there is evidence of ongoing cardiovascular compromise after the first hour of treatment (no improvement in pulse pressure or pulse rate, persisting peripheral shutdown, a rising HCT), a colloid solution (6% dextran 70 or 6% starch solution) should be substituted for the crystalloid solution at an initial rate of 10–20 ml/kg/hr. Hyperoncotic preparations such as 10% dextran have been implicated in the development of renal failure when used in hypovolaemic patients and should be avoided. If large volumes of colloid are infused, regular assessment of the coagulation profile is required.
Frequent observation of vital signs, mental state, urine output and serial HCT measurements are used to assess the response to treatment. After initial resuscitation, most patients can be managed successfully with the reducing schedule of isotonic crystalloid fluid until the reabsorptive phase of the illness begins around day 6–7. If there are further episodes of cardiovascular decompensation after the initial episode, supplementary treatment with small infusions of 5–10 ml/kg of colloid may be required.
Patients with no recordable pulse or BP must be managed more vigorously. Profoundly shocked patients require colloid therapy (6% dextran 70 or 6% starch solution) immediately. Despite initial severity, most patients improve with aggressive volume replacement and can be managed subsequently as outlined above. Central venous pressure (CVP) monitoring provides useful information to direct fluid therapy, but insertion of lines should be carried out only by experienced personnel and with careful attention to the coagulation state. Inotropic support may be required in addition to volume support. Significant pleural effusions and respiratory compromise are likely to develop; pleural and ascitic drainage and artificial ventilation may all prove to be necessary. Metabolic and electrolyte derangements are common in these critically ill patients and should be actively sought and treated.
Blood transfusion
Blood transfusion is indicated only for patients with major bleeding and should be undertaken with extreme care because of the problem of fluid overload. Major bleeding in DSS is almost always associated with severe or prolonged shock, usually from the gastrointestinal tract or vagina. Underlying causes include profound thrombocytopenia in combination with gastritis or stress ulceration. Internal bleeding may not become apparent for many hours until the first melaena stool is passed. Blood transfusion should be considered in all patients who fail to improve clinically after appropriate fluid resuscitation, particularly if the HCT unexpectedly fall. Platelet concentrates and fresh frozen plasma can also be helpful, but are effective for only a few hours. Routine platelet transfusions are not indicated. Steroids are not recommended in the management of severe dengue.
Fluid overload
Clinically significant fluid overload develops in several situations:
Most commonly, it follows either administration of iv fluid in excessive amounts or too rapidly in patients with moderate capillary leak, or continued parenteral fluid therapy when leak has resolved and the reabsorptive phase of the disease has begun.
Rarely, it may be seen in patients with catastrophic leak, for whom support of the circulation is not possible without administration of large volumes of fluid.
Fluid overload may occur in patients with underlying chronic disease, particularly cardiac or renal disorders.
Careful attention to treatment guidelines and frequent reassessment of the patient by experienced personnel should help to limit the occurrence of iatrogenic fluid overload. Early identification of rare patients with catastrophic leak or severe underlying disease may allow pre-emptive intervention before there is significant respiratory compromise.
Early respiratory signs of severe fluid overload include tachypnoea and recession, and evidence of ascites and pleural effusions. Pulmonary oedema, cyanosis and respiratory failure are late manifestations. In addition, severe fluid overload may compromise cardiac function, resulting in hypotension and circulatory failure. Measurement of CVP is helpful in differentiating between haemodynamic instability resulting from severe overload and instability caused by inadequate treatment of the underlying hypovolaemia.
Current research
Vaccine
A vaccine against dengue would be a major advance in the control of the disease. In view of the theoretical risks of antibody-mediated enhancement, a successful vaccine would have to offer lasting protection against all four serotypes. The leading vaccine candidate at present is a chimeric vaccine–a recombinant clone based on yellow fever vaccine strain, with dengue virus membrane and envelope protein genes substituted into the construct. This chimeric vaccine has shown promise in phase II clinical trials and appears safe and immunogenic. It is anticipated that phase III trials will start in the near future in multiple countries in Asia and Latin America.
Diagnostic aids
Making a diagnosis early in the disease and the ability to predict which patients will progress to severe disease would significantly aid clinical management. Specific IgM against dengue can be used as a sensitive maker of dengue infection and commercially available diagnostic kits are available. The detection of the dengue protein NS1 also has proven use in diagnosis and is of particular use in the first few days of illness. Real time PCR is a highly sensitive diagnostic tool in dengue diagnosis, but the cost of molecular tests such as PCR makes it an impractical tool for use in many settings where dengue is prevalent.
A rapid sensitive test that combines detection of NS1, IgG and IgM, allowing diagnosis of infection throughout the illness course, would be a major advance in dengue diagnostics. The development of appropriate clinical algorithms for use in resource limited settings in parallel with the development of molecular diagnostic tools is necessary if the burden of dengue is to be adequately dealt with. Detection of plasma leakage through serial ultrasound and with echocardiography may be a useful adjunctive tool in the management of patients with dengue diagnosis, particularly identifying those patients at highest risk of developing severe disease.
Antidengue drugs
A greater understanding of dengue virus biology has meant that drug targets have been identified that could potentially be the site of a therapeutic agent. The staggering success in developing drugs against HIV is an example of how efficient and effective antivirals can be developed given appropriate funding.
Potential targets receiving research attention are the viral proteins NS3 and NS5, which play an integral role in genome replication. Their protease domains could be a target for protease inhibitors and through inhibition of viral entry. The challenge is to bridge the gap between findings in the laboratory and effectiveness in patients. However, given the progress in the understanding of dengue virus biology, the future of drug development is encouraging.
There are potential therapeutic developments for the treatment of other flaviviruses such as hepatitis C. In view of structural similarities between different flaviviruses, these developments could be used in the field of dengue treatment. As the severe manifestations of disease are in part due to the immune response, perhaps the development of an immunomodulatory agent would be the best therapeutic strategy. Currently, two double-blind, randomised clinical trials are being conducted, one to assess the potential of a specific antiviral and the other to evaluate steroids in dengue (see key references).
Conclusions
Over the past 40 years, the incidence of dengue infections, particularly the more severe forms including DSS, has increased dramatically. Dengue is now one of the most common reasons for hospital admission in Asia and the Americas during the rainy seasons. The mortality rate for patients admitted with established DSS is 1–5%, even with the best available care, although it can be much higher (>10%). The most important clinical feature of dengue is increased vascular permeability leading to DSS. Infants and younger people are particularly prone to the development of shock, and adults are at increased risk of bleeding. Prompt, but judicious fluid resuscitation of fluid balance in DSS is the most important therapeutic intervention. Over-zealous resuscitation in the presence of ongoing capillary leak must be avoided.
Key references
- 1.The 2009 World Health Organization scheme. http://whqlibdoc.who.int/publications/2009/9789241547871_eng.pdf
- 2. Details of two double-blind, randomised clinical trials to assess the potential of a specific antiviral and to evaluate steroids in dengue. www.controlled-trials.com.
- 3.Hales S, de Wet N, Maindonald J, Woodward A. Potential effect of population and climate changes on global distribution of dengue fever: an empirical model. Lancet 2002; 360: 830–4 10.1016/S0140-6736(02)09964-6 [DOI] [PubMed] [Google Scholar]
- 4.Gubler DJ. Cities spawn epidemic dengue viruses. Nat Med 2004; 10: 129–30 10.1038/nm0204-129 [DOI] [PubMed] [Google Scholar]
- 5.Halstead SB. Pathogenesis of dengue: challenges to molecular biology. Science 1988; 239: 476–81 10.1126/science.3277268 [DOI] [PubMed] [Google Scholar]
- 6.Cummings DA, Iamsirithaworn S, Lessler JT, et al. The impact of the demographic transition on dengue in Thailand: insights from a statistical analysis and mathematical modeling. PLoS Med 2009; 6: e1000139 Epub 2009 Sep 1 10.1371/journal.pmed.1000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wills BA, Nguyen MD, Ha TL, et al. Comparison of three fluid solutions for resuscitation in dengue shock syndrome. N Engl J Med 2005; 353: 877–89 10.1056/NEJMoa044057 [DOI] [PubMed] [Google Scholar]


