Key points
Acute watery diarrhoea may include cholera which can be a life-threatening emergency due to severe losses of water and electrolytes
Many cases of watery diarrhoea are due to toxin-secreting organisms; the mucosa is intact so oral rehydration is highly effective, especially when combined with zinc therapy
Most cases of acute watery diarrhoea can be managed with oral rehydration therapy, but intravenous fluids may be required in severe cases; hypokalaemia needs specific treatment
Acute bloody diarrhoea (dysentery) is commonly due to amoebiasis or shigellosis; urgent serology is helpful in diagnosing amoebiasis which requires specific therapy
Clostridium difficile can cause diarrhoea in the immunocompromised or following antibiotic therapy; treatment with antibiotics is usually successful but probiotics do not work
Epidemiology
Diarrhoea is a disorder which all humans experience at one time or another, and which in most instances is mild and self-limiting. It is however one of the largest contributors to mortality in childhood, probably second only to respiratory infection, and can be very severe in the immunocompromised and the elderly. Diarrhoea can pose major problems for travellers, though it is rarely life-threatening. Diarrhoeal disease can also erupt in major epidemics related to water or food contamination.
Several excellent reviews are available on the complex epidemiology and clinical effects of enteric pathogens, endemic and epidemic,1,2 options for treatment,2,3 prevention and vaccination.4 This article will focus on the relationship between pathophysiology, clinical features and management, with an emphasis on cholera.
Clinical syndromes
Fundamentally, it is useful to recognise three major and fairly distinct syndromes:
acute watery diarrhoea
acute bloody diarrhoea
persistent diarrhoea.
The distinction between acute and persistent illnesses is set at 14 days. This is somewhat arbitrary (all persistent illnesses must begin as acute illnesses) but the aetiology differs in significant ways (Table 1). Other useful syndromes to recognise (not discussed in this article) are:
diarrhoea in the immunocompromised
antibiotic-related diarrhoea
travellers' diarrhoea
specific food-poisoning syndromes.5
Table 1.
Major pathogens in relation to clinical syndromes.
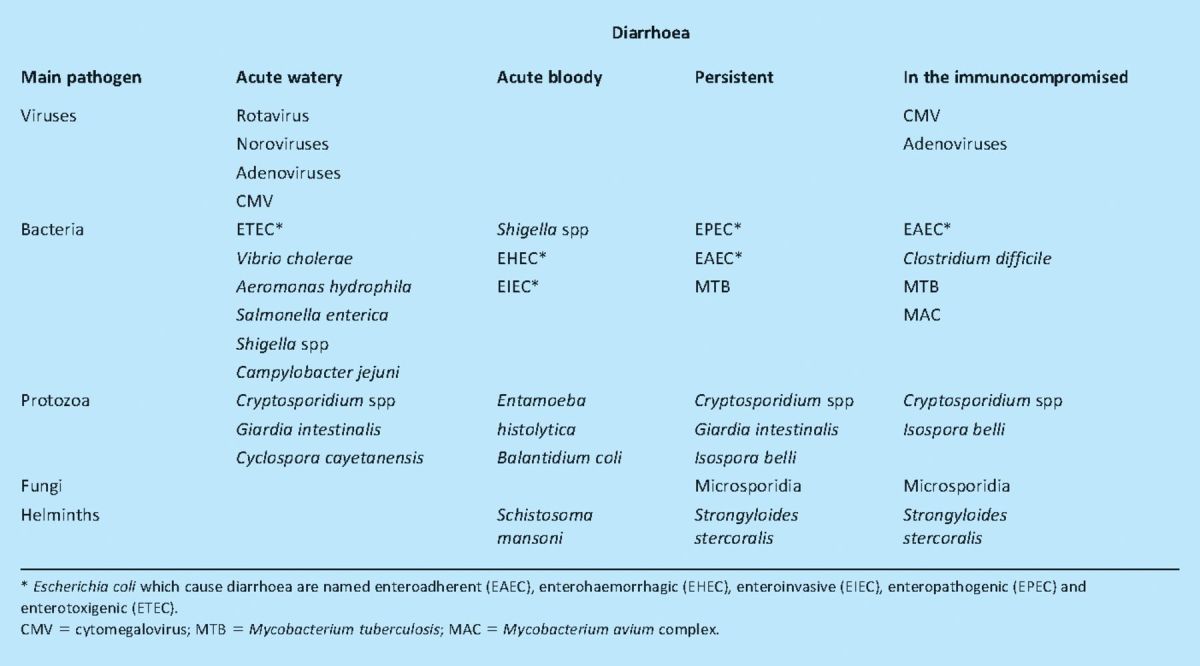
Acute watery diarrhoea
The prototypical infection leading to acute watery diarrhoea is cholera. In terms of global health, cholera causes only a tiny fraction of diarrhoeal disease and is quantitatively dwarfed by all the other pathogens under this heading in Table 1. In terms of diarrhoea morbidity and mortality in children under five years of age, diarrhoeagenic Escherichia coli (especially enterotoxigenic E. coli (ETEC)6) is far more important. However, it is worth considering cholera separately as an understanding of some elements of pathogenesis leads to a direct understanding of several principles of management of any pathogen in this group.
Cholera
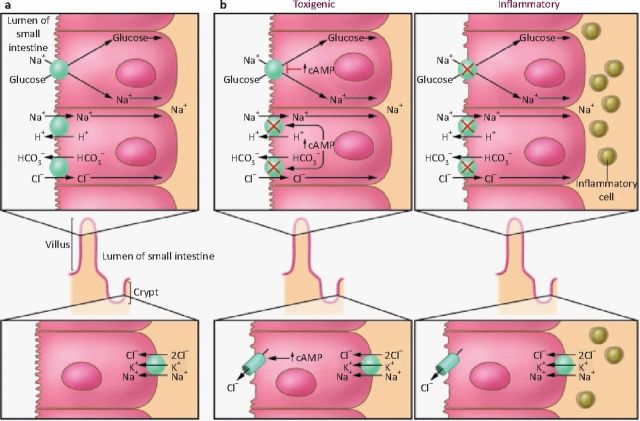
The history of cholera is fascinating in that it demonstrates how a simple Gram-negative bacillus from the estuarine waters of the Ganges delta acquired a cassette of virulence genes on one or more plasmids and evolved into a major human pathogen which has unleashed seven pandemics and spread to all continents.7,8 Its power to kill spectacularly in a matter of hours has inspired considerable fear, and even novels! The pathophysiology is still not completely understood (in particular, the interaction between toxins and the enteric nervous system), but several points can be made (Fig 1 illustrates the physiology of cholera):
-
1
The mucosal architecture of the small intestine, in particular the epithelium, remains intact.
-
2
Large numbers of bacteria are required to induce disease. Each bacterium liberates a finite quantity of cholera toxin which induces irreversible changes in a number of epithelial cells. The consequence is that the infectious dose is high–about 109 bacteria are required to produce clinical cholera in a healthy person.9
-
3
The greater the amount of toxin synthesised in the gut, the greater the severity of clinical illness. The toxin induces cyclic adenosine monophosphate synthesis in the cell, leading to changes in the balance of water and salt transport so that the small intestine becomes a net secretor of water and electrolytes. This overwhelms the reserve absorptive capacity of the colon and unabsorbed water reaches the rectum.
-
4
When a cell is exposed to cholera toxin, although it is morphologically normal, its chloride secretion is irreversibly turned on. This does not prevent the cell from absorbing sodium (Na) through the Na-glucose co-transporter. By providing extra substrate for the Na-glucose co-transporter, the re-uptake of Na (then water) becomes possible.
-
5
The faecal losses of electrolytes are relatively constant, so cholera leads fairly predictably to a hypokalaemic metabolic acidosis in addition to severe volume depletion.
-
6
Once the toxin is removed, normal epithelial regeneration replaces the population of cells which have been physiologically reprogrammed with a new population of enterocytes which secrete water and electrolytes normally.
Fig 1.
Movement of sodium ions (Na+) and chloride ions (Cl−) in the small intestine during health and diarrhoea. (a) Normal subjects. Na+ is absorbed by two different mechanisms in absorptive cells from villi: glucose-stimulated absorption and electroneutral absorption (which represents the coupling of Na/H and Cl/bicarbonate (HCO3) exchanges). (b) During diarrhoea caused by a toxin and inflammation. In toxigenic diarrhoea (eg caused by the enterotoxin produced by Vibrio cholerae), increased mucosal levels of cyclic adenosine monophosphate (cAMP) inhibit electroneutral sodium chloride (NaCl) absorption but have no effect on glucose-stimulated Na+ absorption. In inflammatory diarrhoea (eg following infection with Shigella spp or Salmonella spp) there is extensive histological damage, resulting in altered cell morphology and reduced glucose-stimulated Na+ and electroneutral NaCl absorption. The role of one or more cytokines in this inflammatory response is critical. In secretory cells from crypts, Cl− secretion is minimal in normal subjects and activated by cAMP in toxigenic and inflammatory diarrhoea. Reproduced from reference 1.
Management
The management of cholera exploits these principles:
-
1
Oral rehydration solution (ORS) is used to stimulate Na-glucose co-transport and increase uptake of water and electrolytes into the small intestine. The ORS must contain potassium, and ideally bicarbonate or citrate to help compensate for the loss of bicarbonate in stool.
-
2
Antibiotics are useful to reduce both the amount of toxin being generated and stool losses, and to allow the repopulation of the epithelial compartment with normal cells, thus shortening the clinical illness.
The International Centre for Diarrhoeal Disease Research in Bangladesh has extensive experience of managing cholera. Using the guiding principles listed above, it has managed to reduce the mortality of cholera to well below 1%. The addition of zinc has allowed a further reduction in duration of illness.3,10,11 Oral rehydration therapy is the mainstay of treatment, with intravenous (iv) fluid therapy reserved for the most severe cases where there is shock or impairment of consciousness.
Enterotoxigenic Escherichia coli diarrhoea
As with cholera, other pathogens which synthesise similar toxins, such as ETEC, require similar management. The heat labile toxin of ETEC is structurally and functionally very similar to cholera toxin, though the heat stable toxin is very different and alters cyclic guanosine monophosphate synthesis, inducing secretion by a different mechanism.6
The principal difference in management between cholera and ETEC diarrhoea is that there is a consensus that non-cholera diarrhoea, being less severe than cholera, does not justify the use of antibiotics. There are rapid tests to distinguish cholera from other acute watery diarrhoeal illnesses, and urgent laboratory advice should be sought if there is clinical suspicion that a patient may have cholera.
Acute bloody diarrhoea (dysentery)
Dysentery is the name given to acute bloody diarrhoea, with or without fever. The two dominant causes are bacillary (Shigella spp) or amoebic (Entamoeba histolytica), but Campylobacter spp can also cause a similar illness. Travellers from the Philippines, Borneo and other parts of South-East Asia may rarely have Balantidium coli infection. Invasive amoebiasis is best diagnosed by serology.
Management
Treatment is with metronidazole 800 mg eight-hourly, orally or iv depending on clinical condition, for 10 days, followed by diloxanide furoate 500 mg eight-hourly for 10 days.12 Most strains of Shigella and enteroinvasive E. coli remain susceptible to ciprofloxacin.13
The unresolved question is how to treat bloody diarrhoea due to enterohaemorrhagic E. coli (EHEC). There are significant grounds for thinking that treatment of EHEC with antibiotics leads to the release of verocytotoxin which precipitates haemolytic uraemic syndrome (HUS). This causes severe morbidity and even mortality, so it might be better not to treat dysentery with antibiotics until stool culture confirms that EHEC is not responsible. In severe cases, it would be wise to get microbiological advice, collect the right samples and treat on a probabilistic basis. Interestingly, EHEC appears to cause long-term renal damage and hypertension.14
Persistent diarrhoea
This is a large subject, for which space does not allow full discussion. Common causes are shown in Table 1. Protozoal infections are a major cause of persistent diarrhoea in the tropics,12,15 but in many places, including India, non-infectious causes such as inflammatory bowel disease are becoming more common and should not be forgotten. One helminth, Strongyloides stercoralis, causes diarrhoea; diagnosis is serological and treatment often difficult.
When to use antibiotics during diarrhoeal disease
A key clinical question, about which there is limited consensus, is when to use antibiotics in diarrhoeal disease. Cholera always requires antibiotics (eg ciprofloxacin or tetracycline), as does amoebic dysentery. However, not all dysentery illnesses require antibiotics (in view of the concern that treatment of EHEC will lead to HUS), but it will be difficult not to intervene in severe cases. When a protozoan infection is detected in a patient with persistent diarrhoea, it should always be treated. Toxin-secreting Clostridium difficile should always be treated when there is diarrhoea in the immunocompromised and following antibiotics. Recent evidence confirms that probiotics do not treat C. difficile infection,16 but are useful in reducing the duration of acute watery diarrhoea.17 Travellers' diarrhoea responds to antibiotics (ciprofloxacin 500 mg as a single dose or, preferably, rifaximin 200 mg tid for three days18), but symptomatic treatment with loperamide and oral fluids is usually all that is required.
References
- 1.Petri WA, Jr, Miller M, Binder HJ, et al. Enteric infections, diarrhoea, and their impact on function and development. J Clin Invest 2008; 118: 1277–90 10.1172/JCI34005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Casburn-Jones A, Farthing MJ. Management of infectious diarrhoea. Gut 2004; 53: 296–305 10.1136/gut.2003.022103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Santosham M, Chandran A, Fitzwater S, et al. Progress and barriers for the control of diarrhoeal disease. Lancet 2010; 376: 63–7 10.1016/S0140-6736(10)60356-X [DOI] [PubMed] [Google Scholar]
- 4.Serazin AC, Shackelton LA, Wilson C, Bhan BK. Improving the performance of enteric vaccines in the developing world. Nat Immunol 2010; 11: 769–73 10.1038/ni0910-769 [DOI] [PubMed] [Google Scholar]
- 5.Brett MM. Food poisoning associated with biotoxins in fish and shellfish. Curr Opinion Infect Dis 2003; 16: 461–5 10.1097/00001432-200310000-00013 [DOI] [PubMed] [Google Scholar]
- 6.Qadri F, Svennerholm AM, Faruque AS, Sack RB. Enterotoxigenic Escherichia coli in developing countries: epidemiology, microbiology, clinical features, treatment, and prevention. Clin Microbiol Rev 2005; 18: 465–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wachsmuth IK, Blake PA, Olsvik O. Vibrio cholerae and cholera: molecular to global perspectives 1994. Washington: ASM Press [Google Scholar]
- 8.Faruque SM, Nair B. Vibrio cholerae: genomics and molecular biology 2008. Norfolk: Caister Academic Press [Google Scholar]
- 9.Cash RA, Music SI, Libonati JP, et al. Response of man to infection with Vibrio cholerae. I. Clinical serologic, and bacteriologic responses to a known inoculum. J Infect Dis 1974; 129: 45–52 10.1093/infdis/129.1.45 [DOI] [PubMed] [Google Scholar]
- 10.Roy SK, Hossain MJ, Khatun W, et al. Zinc supplementation in children with cholera in Bangladesh: randomised controlled trial. BMJ 2008; 336: 266–8 10.1136/bmj.39416.646250.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazzerini M, Ronfani L. Oral zinc for treating diarrhoea in children. Cochrane Database Syst Rev 2008; 3: CD005436. [DOI] [PubMed] [Google Scholar]
- 12.Farthing MJ, Cevallos AM, Kelly P. Cook G, Zumla A. Intestinal protozoa. Manson's tropical diseases 2008. 22nd edn. London: Saunders, 1375–406 10.1038/ncpgasthep0557 [DOI] [Google Scholar]
- 13.Traa BS, Walker CL, Munos M, Black RE. Antibiotics for the treatment of dysentery in children. Int J Epidemiol 2010; 39(Suppl 1) i70–4 10.1093/ije/dyq024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clark WF, Sontrop JM, Macnab JJ, et al. Long term risk for hypertension, renal impairment, and cardiovascular disease after gastroenteritis from drinking water contaminated with Escherichia coli O157:H7: a prospective cohort study. BMJ 2010; 341: c6020. 10.1136/bmj.282.6262.481-a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kenny JM, Kelly P. Protozoal gastrointestinal infections. Medicine 2009; 37: 599–602 10.1016/j.mpmed.2009.08.001 [DOI] [Google Scholar]
- 16.Miller M. The fascination with probiotics for Clostridium difficile infection: lack of evidence for prophylactic or therapeutic efficacy. Anaerobe 2009; 15: 281–4 [DOI] [PubMed] [Google Scholar]
- 17.Allen SJ, Martinez EG, Gregorio GV, Dans LF. Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst Rev 2010; 11: CD003048. 10.1002/14651858.CD003048.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Layer P, Andresen V. Review article: rifaximin, a minimally absorbed oral antibacterial, for the treatment of travellers' diarrhoea. Aliment Pharmacol Therap 2010; 31: 1155–64 [DOI] [PubMed] [Google Scholar]