Abstract
Consultant-delivered care has been shown to improve outcomes for acute medical patients. However, the ideal composition of a medical team to support consultant-delivered care is not clear and little is known about the effect of continuing consultant-delivered care until the patient is discharged. Between December 2011 and April 2012, 260 general medical patients requiring inpatient care were managed by a consultant-delivered multidisciplinary team (CD-MDT) and 150 patients by a standard consultant-led team of trainee doctors. The length of hospital stay was significantly lower for patients managed by a CD-MDT than for those managed by a standard team (4–5 days vs 7 days, p<0.001). No difference between the groups was seen for readmission rates, patient safety or mortality. In conclusion, a CD-MDT is a safe and effective model of inpatient medical care and is associated with a shorter length of hospital stay.
KEY WORDS: Consultant-delivered care, general internal medicine, multidisciplinary team
Introduction
Patient care delivered directly by a consultant or fully trained doctor is associated with better outcomes for patients. The recent report from the Academy of Royal Medical Colleges highlighted the benefits of consultant-delivered care, including effective clinical decision making, efficient use of resources and better outcomes for patients.1 However, the move to a consultant-delivered service has implications for resources and requires changes to the current model of service, including consultants’ working practices.
Although the benefit of consultant-delivered care has been recognised, most data arise from observational studies of consultant input within the first 24 hours of acute admission to hospital.2–6 What remains unclear is the benefit of extending consultant-delivered care beyond the acute phase until the patient is discharged from hospital. Although some evidence to support this comes from the US ‘hospitalist’ model of inpatient care, this may not be directly applicable to other healthcare systems.7–9
Many hospitals in the UK have introduced acute medical units and acute physicians to deliver acute medical care, which is followed by triage to a medical specialty for ongoing care until discharge. Although this has improved the acute care of patients,3,10 this model may not benefit certain subgroups of patients.5 One particular group who may fail to achieve the improved outcomes of this model of care are general medical patients. These patients, whose acute illness fails to align with a medical specialty or who fall below the age criteria for elderly care medicine, are of particular concern, as they often have significant comorbidity and complex multisystem diseases. Furthermore, general medical patients are often allocated to non-specialist and non-medical wards due to pressure on bed resources and so may not benefit from the medical and multidisciplinary expertise they require.
The purpose of this study was to address the clinical needs of these patients by developing a novel team consisting of a consultant combined with a multidisciplinary team (MDT) to deliver inpatient care up to the point of discharge. The primary aim was to study the impact of this model of medical care on patient outcomes, including length of hospital stay.
Methods
Design and setting
The study was part of a project funded by the NHS Strategic Health Authority to develop and evaluate an innovative model of consultant-delivered inpatient care while providing additional medical capacity to deal with increased medical admissions during the winter months. The patient population studied involved unselected general medical patients admitted to the University Hospital of Southampton during the winter period of December 2011–April 2012. The impact on patient care was measured in standard patient outcomes, including length of stay, patient safety, adverse events and mortality.
Development of consultant-delivered multidisciplinary teams
Two consultant-delivered, multidisciplinary teams (CD-MDTs) were developed to deliver inpatient medical care to general medical patients (CD-MDT-1 and CD-MDT-2). Each team consisted of a full-time consultant physician, a medical nurse (Band 6) and a pharmacist. Both consultant physicians had completed specialist training in general (internal) medicine within the past five years, with the consultant for CD-MDT-1 dual accredited in nephrology and the consultant for CD-MDT-2 dual accredited in intensive care medicine. In addition, a single medical assistant, whose background experience included completion of a foundation degree in applied medical technology and two years’ clinical experience as a medical assistant, was allocated to both teams. The overall composition of the teams contrasts with the standard medical team in the UK, which typically consists of a consultant-led team of trainee doctors.
Role of the CD-MDT and team members
The primary role of the consultant was delivery of patient care from the point at which patients were transferred from the acute medical unit to the ward until discharge. The consultant was directly responsible for daily patient ward rounds, managing investigations, coordinating administration and discharge planning, and managing any clinical emergencies.
The MDT was developed to support the consultant with efficient delivery of all aspects of medical care. The principal role of the pharmacist was medicines management, including drug repatriation, medicines advice and managing discharge medicines. In addition, the pharmacist in CD-MDT-1 was an accredited independent prescriber, which enabled greater scope and flexibility for managing medicines. In practice, independent pharmacist prescribing was limited to management of antibiotic and anticoagulants, as most prescribing was done on the MDT's daily ward round in conjunction with the consultant.
The medical nurse acted as a case manager, which included coordinating the patient caseload; managing investigations; discharge planning; and liasing with other clinical teams, patients and families. The medical assistant provided clinical support (eg phlebotomy, venous cannulation and electrocardiography) and administrative support (eg requesting investigations and collating results).
Work pattern
Each CD-MDT had a separate caseload of general medical patients and delivered inpatient care from the time the patient was transferred from the acute medical unit to the ward until discharge. Patients were reviewed daily by the consultant and MDT during the working week (Monday–Friday). Outside working hours and at the weekend, medical care was provided by on-call medical staff. To study the effect of six-day consultant-delivered care on patient length of stay and weekend discharges, patients managed by CD-MDT-2 were also reviewed by a consultant and medical nurse on an additional day over the weekend.
Patient characteristics and selection
General medical patients were defined as those aged <80 years admitted with an acute medical illness that did not align with specialist medical care. Patients admitted to the acute medical unit were managed by an acute medical physician for the first 24–72 hours. Those requiring ongoing inpatient care were then allocated by an acute physician to either a specialist team (cardiology, respiratory, gastroenterology, hepatology, nephrology or stroke medicine) or general medical care depending on the acute diagnosis. General medical patients were then allocated by a bed manager to a medical or non-medical ward.
Clinical care from the point patients arrived at the receiving ward was continued by a CD-MDT or a control team. CD-MDT-1 managed general medical patients from three medical wards: a 22-bed female ward, a 12-bed male ward and a 10-bed short-stay ward; the latter two wards were opened to increase bed capacity during the winter. CD-MDT-2 managed general medical patients transferred to three non-medical surgical and orthopaedic wards. Patients were transferred to these wards because of pressure on medical ward capacity during the winter months.
Control medical team
A control medical team delivered inpatient care according to the standard model of a consultant-led team in the UK, which comprises trainee doctors (one specialty trainee (ST4), one core medical trainee (CT1 or CT2) and one foundation year trainee (FY1 or FY2) with cross-cover). Patients were reviewed daily by trainees, with a consultant conducting a formal ward round twice a week on a Monday and Wednesday. Weekend and out-of-hours care was delivered by the medical on-call team only to those patients identified as needing medical review. The on-call team consisted of a specialist trainee and core trainee led by a consultant. The control medical team received general medical patients from two 22-bed medical wards.
Study size, duration, data collection and analysis
The study ran from December 2011 to April 2012; CD-MDT-1 was operational for 16 weeks and CD-MDT-2 for only 10 weeks due to a delay recruiting members for the MDT. The study size was constrained by the number of patients admitted over the limited study period.
Patient data were collected prospectively for each medical team. Data on demographics, diagnosis at discharge according to the international and statistical classification of diseases and health-related problems, tenth edition (ICD-10), and outcome measures were collected from the patient administration system (Enterprise CaMIS; Ascribe, Bolton, UK) and doctors’ work list (University Hospital Southampton database). Data on complaints and critical incidents were collated from the hospital's risk and patient safety unit.
Data were managed and analysed using a spreadsheet (Excel; Microsoft) and statistical software (SigmaPlot). The Kruksall–Wallis test was used to compare three or more non-parametric datasets.
Ethical approval
Ethical approval was not obtained for the project, as the initial design was to develop and study innovative team models to deliver medical care rather than to study the direct impact on patient care.
Results
Patient demographics
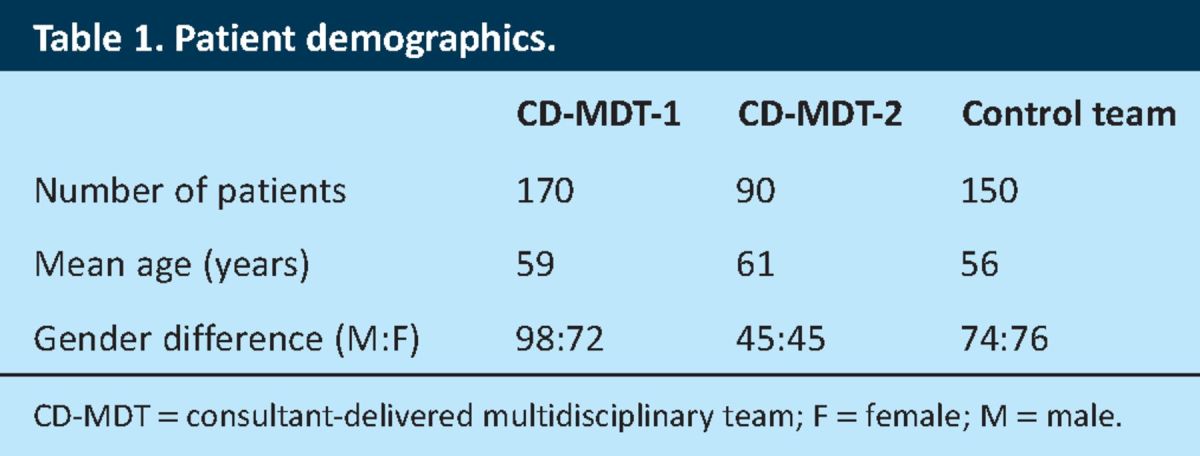
Over the 16-week study period, CD-MDT-1 delivered inpatient care to 170 general medical patients, CD-MDT-2 to 90 patients (over 10 weeks) and the control team to 150 patients. The fact that CD-MDT-2 became operational six weeks after the start of the study is reflected in the small number of patients managed overall compared with the other teams. Age and gender distribution did not differ between the teams (Table 1).
Table 1.
Patient demographics.
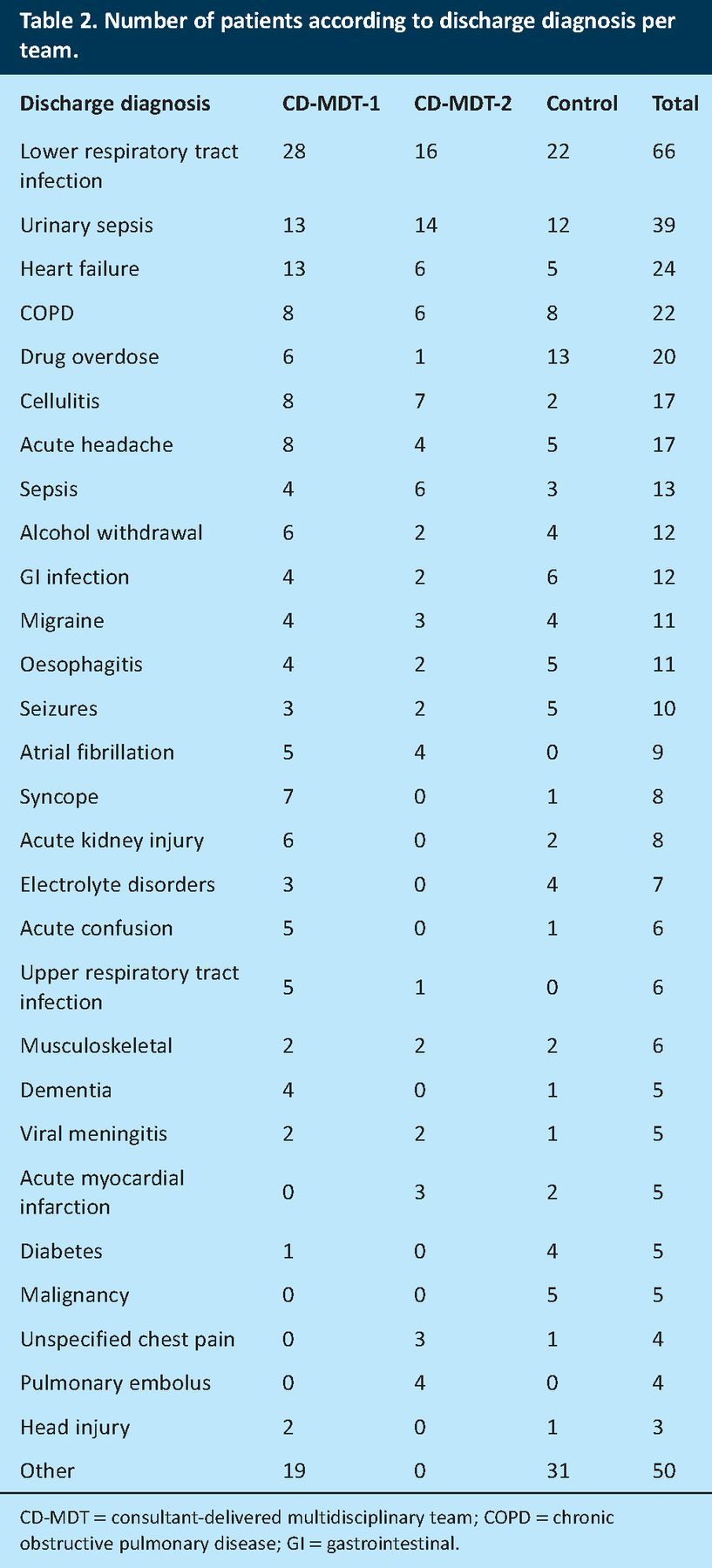
Patient diagnosis and casemix
A wide range of discharge diagnoses were recorded for each team, reflecting the casemix of general medical patients. Discharge diagnoses were comparable between teams, with the most common being lower respiratory tract infections, urinary tract infections, heart failure and exacerbation of chronic obstructive pulmonary disease (Table 2). Some discharge diagnoses (such as pulmonary emboli and myocardial infarction) may seem to have been more suitable for a specialist team rather than general medicine; this may be because the diagnosis was unclear at the time of admission or developed during the patient's hospital admission.
Table 2.
Number of patients according to discharge diagnosis per team.
Workload and activity for the CD-MDTs
No difference between the teams was seen in terms of daily caseload or work activity. Although the total number of patients managed by each team differed over the study period, no difference in the daily caseload between teams was seen: median (range) daily caseload of 13 (5–17) patients for CD-MDT-1, 9 (3–17) in CD-MDT-2 and 14 (5–22) for the control team. Similarly, no difference was seen in the number of patients allocated to each team per week, although there was a wide range of patient numbers (10 (range 1–16) for CD-MDT-1, 9 (1–17) for CD-MDT-2 and 8 (2–24) for the control team).
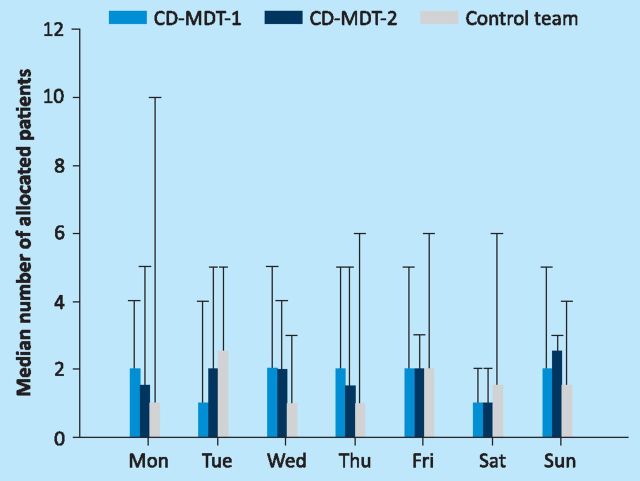
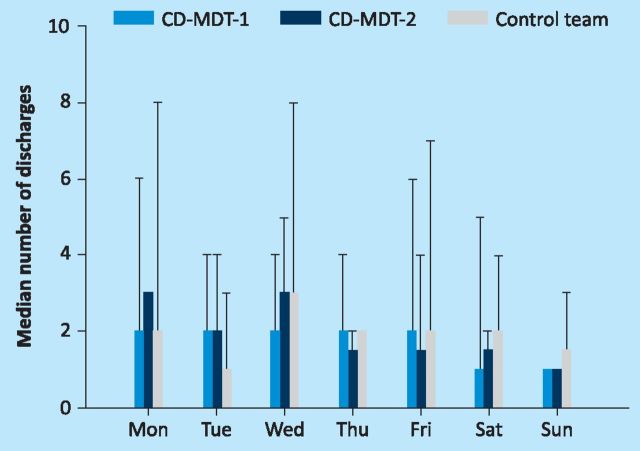
Previous hospital data had highlighted peaks in admissions and discharges on Mondays and Fridays, which was attributed to 5-day working. Analysis of patient allocations and discharges according to the day of the week showed a trend towards fewer allocations and discharges at the weekend compared to weekdays (Fig 1 and (Fig 2). Although Mondays and Fridays were associated with peak allocation and discharge activity for CD-MDT-1 and the control team, no difference in median activity was seen between different days of the week for each team (Fig 1 and (Fig 2).
Fig 1.
Number of patients allocated per day. Data expressed as median number of patients; bars are maximum number of allocated patients per day.
Fig 2.
Number of patients discharged per day. Data expressed as median number of patients; bars are maximum number of discharged patients per day.
Length of patient stay
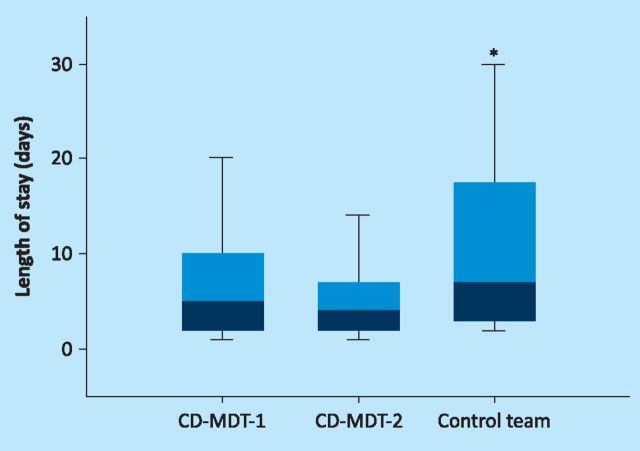
Patients managed by both CD-MDTs had significantly shorter lengths of stay compared to those managed by the control team. Median length of stay was 5 (range 1–54) days for patients managed by CD-MDT-1, 4 (1–37) for CD-MDT-2 and 7 (1–80) for the control team (p<0.001, Fig Fig 3).
Fig 3.
Length of stay by team. Box plot showing length of stay in days for each team. *p<0.001 versus other teams.
Readmissions
No difference between teams was seen in the number of readmissions within 30 days of discharge: 28 (16%) patients for CD-MDT-1, 16 (20%) for CD-MDT-2 and 26 (14%) for the control team. Although a trend to greater readmissions in the CD-MDTs was seen compared to the control team, this was not statistically significant (χ2 1.24, p = 0.2). For comparison, the annual readmission rate for all acute medicine patients in the trust was 9.6%.
In-hospital patient mortality
In-hospital mortality was not statistically different between the teams: five (3%) deaths for CD-MDT-1, two (2%) for CD-MDT-2 and 12 (6%) for the control team. In addition, no difference was seen in 30-day mortality after discharge: one (1%) death for CD-MDT-1, one (1%) for CD-MDT-2 and four (3%) for the control team.
Patient safety
No critical incidences were reported for any patients managed by the study and control teams. However, one complaint relating to a factual error in a discharge summary was documented for a patient managed by CD-MDT-1.
Discussion
Our study investigated the impact on patient care of a novel medical team. The primary aim was to establish whether a consultant could deliver inpatient care with the support of a MDT rather than a team of trainee doctors. The patient outcome data support the clinical effectiveness of this model of care and highlight a reduction in length of stay for patients. In addition, this model of care did not adversely affect patient safety or outcomes when compared with the standard model of inpatient medical care in the UK.
The process of delivering inpatient care is complex, with many factors affecting patient outcome and length of stay, including severity of patient illness, quality of medical and nursing care, and systems supporting discharge planning and social care for patients. There are several possible reasons for the observed difference in patient length of stay between the study and control teams. Firstly, direct involvement of a consultant in the delivery of patient care has been shown to improve patient outcomes and efficiency of care in the context of acute and emergency medicine.2,4-6 Intuitive reasons for the ‘consultant effect’ on patient care include more experienced and appropriate decision making and improved resource management.1 Similarly, there may be a benefit of extending consultant-delivered care beyond the acute phase until discharge.
Evidence from the hospitalist model of care in the USA, in which inpatient services are delivered from admission to discharge by generalists, is associated with improved patient outcomes and reduced length of stay.8,9 However, this model is not directly comparable with the UK due to differences in training, experience of staff and healthcare systems. Our study demonstrates the benefit of extending consultant-delivered care beyond the first 24–48 hours to the point of discharge within the context of the system in the UK.
The specific impact of the MDT supporting consultant-delivered care is difficult to quantify. Subjective advantages identified by the teams included more effective communication and decision making, with better knowledge of hospital systems and resources available. Combining a consultant, pharmacist and senior nurse in the MDT enabled integration of medical and medicines management with social care and discharge planning. Interestingly, the value of a pharmacist prescriber above that of a general pharmacist was not as expected, as most prescribing was undertaken on the MDT's daily ward round. Although one similar study in the USA demonstrated the benefit of a medical nurse and physician working in conjunction with an MDT,11 the evidence comes from care provided in addition to the medical team rather than as a substitute for doctors.12,13 Other advantages include better continuity of medical care than the control team, as study team members did not have additional clinical roles such as outpatient or on-call commitments.
Other explanations for differences between consultant-delivered care and the control team could include patient casemix, work intensity and study bias. Although patient demographics and diagnosis were comparable between teams, patient allocation to each team was not randomised, so patients with greater severity of acute illness may have been allocated preferentially to particular medical teams and wards. However, no differences in work intensity and caseload were detected between the teams.
Value for general medical patients
The spectra of discharge diagnoses and variations in patient length of stay highlight the diversity and complexity of this cohort of general medical patients. Although most patients had a single overarching diagnosis, a significant proportion were admitted with a non-specific presentation such as sepsis, headache or confusion. The addition of multiple comorbidities, chronic illness and drug and alcohol abuse makes this group of patients vulnerable and particularly challenging to manage. These patients are often managed on non-specialist or surgical wards and accurate diagnosis and ongoing management may be delayed. This may adversely affect the quality of medical care and timely access to specialist medical and multidisciplinary services. An experienced consultant-delivered MDT model of care may mean that these patients receive better quality medical care and timely access to specialist hospital services.
Implications of this study
This study provides further evidence for the benefit of consultant-delivered care and highlights that general medical patients are an ‘overlooked’ group. A CD-MDT may be a more effective model of care for this potentially vulnerable group of patients. This study shows not only that consultant-delivered care is safe and effective but also that it may be more effective than a standard medical team model for certain patients. With increasing interest in the value of consultant-delivered care, this study highlights the importance of hospitals taking the opportunity to reevaluate and redesign the delivery of medical care from the perspective and needs of the patient, as well those of the medical staff.
Funding
This work was supported by the South Central Strategic Health Authority, NHS South of England.
References
- 1.Academy of Medical Royal Colleges The benefits of consultant-delivered care. London: AMRC, 2012. http://aomrc.org.uk/publications/statements/doc_download/9450-the-benefits-of-consultantdelivered-care.html [Accessed 7 June 2013]. [Google Scholar]
- 2.Robinson G, McCann K, Freeman P, et al. The New Zealand national junior doctors’ strike: implications for the provision of acute hospital medical services. Clin Med 2008;8:272–5. 10.7861/clinmedicine.8-3-272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Byrne D, Silke B. Acute m edical units: review of evidence. Eur J Intern Med 2011;22:344–7. 10.1016/j.ejim.2011.05.016 [DOI] [PubMed] [Google Scholar]
- 4.Armitage M, Raza T. A consultant physician in acute medicine: the Bournemouth Model for managing increasing numbers of medical emergency admissions. Clin Med 2002;2:331–3. 10.7861/clinmedicine.2-4-331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moore S, Gemmell I, Almond S, et al. Impact of specialist care on clinical outcomes for medical emergencies. Clin Med 2006;6:286–93. 10.7861/clinmedicine.6-3-286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.White AL, Armstrong PAR, Thakore S. Impact of senior clinical review on patient disposition from the emergency department. Emerg Med J 2010;27:262–5. [DOI] [PubMed] [Google Scholar]
- 7.Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc 2009;84:248–54. 10.4065/84.3.248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care 2004;10:561–8. [PubMed] [Google Scholar]
- 9.Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med 2002;137:866–74. 10.7326/0003-4819-137-11-200212030-00007 [DOI] [PubMed] [Google Scholar]
- 10.Scott I, Vaughan L, Bell D. Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care 2009;21:397–407. 10.1093/intqhc/mzp045 [DOI] [PubMed] [Google Scholar]
- 11.Cowan MJ, Shapiro M, Hays RD, et al. The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs. J Nurs Admin 2006;36:79–85. 10.1097/00005110-200602000-00006 [DOI] [PubMed] [Google Scholar]
- 12.O’Mahony S, Mazur E, Charney P, et al. Use of multidisciplinary rounds to simultaneously improve quality outcomes, enhance resident education, and shorten length of stay. J Gen Intern Med 2007:1073–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaboli PJ, Hoth AB, McClimon BJ, et al. Clinical pharmacists and inpatient medical care: a systematic review. Arch Intern Med 2006;166:955–64. 10.1001/archinte.166.9.955 [DOI] [PubMed] [Google Scholar]