ABSTRACT
Thoracic ultrasound training has become part of the respiratory medicine curriculum. Data on training, access to teaching and achievement of competency in thoracic ultrasound by respiratory specialty trainees are scarce. Using the web-based kwiksurveys, we surveyed current respiratory specialty trainees (STs) in the UK. 177 responses were recorded. Nearly three-quarters of trainees had access to bedside ultrasound but only 15.3% had regular ultrasound training. Overall, 28.8% had achieved level 1 competency but only 44.4% of trainees at ST6 and above were level 1 competent. The majority of respiratory trainees have access to thoracic ultrasound but structured training is limited, with only a small proportion of trainees attaining level 1. More structured training and mentoring is needed to enable trainees to achieve the required competencies.
KEY WORDS: Ultrasound, thoracic, competency, training, curriculum
Introduction
Pleural disorders remain a common medical problem accounting for approximately one-quarter of consultations in respiratory clinics.1 In recent years, thoracic ultrasound has become an important tool for the investigation and management of pleural diseases2 as it is relatively inexpensive and allows a real-time assessment of the pleural space.3 Current British Thoracic Society (BTS) guidelines for the management of pleural diseases strongly recommend thoracic ultrasound for the investigation and management of patients with pleural effusions.2
Thoracic ultrasound has been shown to improve the success rate of thoracocentesis, as it is more sensitive in detecting pleural fluid than plain radiography, reduces the risk of complications of pleural procedures4–7 and is now more widely used by respiratory specialists.8 The Joint Royal College of Physicians Training Board (JRCPTB) for respiratory medicine now requires trainees to achieve Royal College of Radiology thoracic ultrasound level 1 competency by the completion of specialist training.9
To the best of our knowledge, this is the first nationwide survey of current respiratory specialty trainees (STs) to investigate the level of training and competency in thoracic ultrasound. The primary aim was to assess whether respiratory trainees have access to training to the level required by the current respiratory medicine curriculum. The secondary aims were to assess whether training differs between teaching and district general hospitals and to assess the extent to which respiratory trainees are involved in the provision of ultrasound services for non-respiratory specialties.
Methods
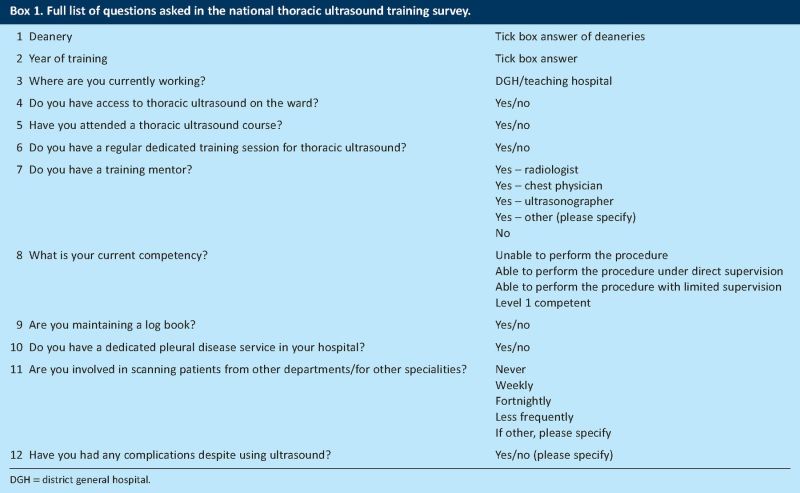
We designed a 12-question survey using the web-based tool kwiksurveys10 (for a full list of questions see Box 1). The direct link for the survey was e-mailed to each regional training programme director in respiratory medicine in each of the 16 deaneries in the UK, asking them to distribute the link among all the trainees within their region.
Data on the trainee's deanery, year of training and whether the current placement was in a teaching or district hospital were collected, together with information on the availability of thoracic ultrasound on wards, the provision of dedicated ultrasound training sessions in the trainee's current hospital and whether the respiratory ST had a training mentor, specifying who that mentor was. Questions also ascertained the current level of competency (as defined by the criteria for completion of the Directly Observed Procedural Skills),9 whether a log book was maintained and the frequency of ultrasound scanning requests by other departments or specialties.
Data were analysed using the Pearson's Chi-squared (χ2) test to compare differences between teaching and district hospitals. Statistical analyses were performed in PASW Statistics 18.0 (SPSS Inc, Chicago, Illinois).
Results
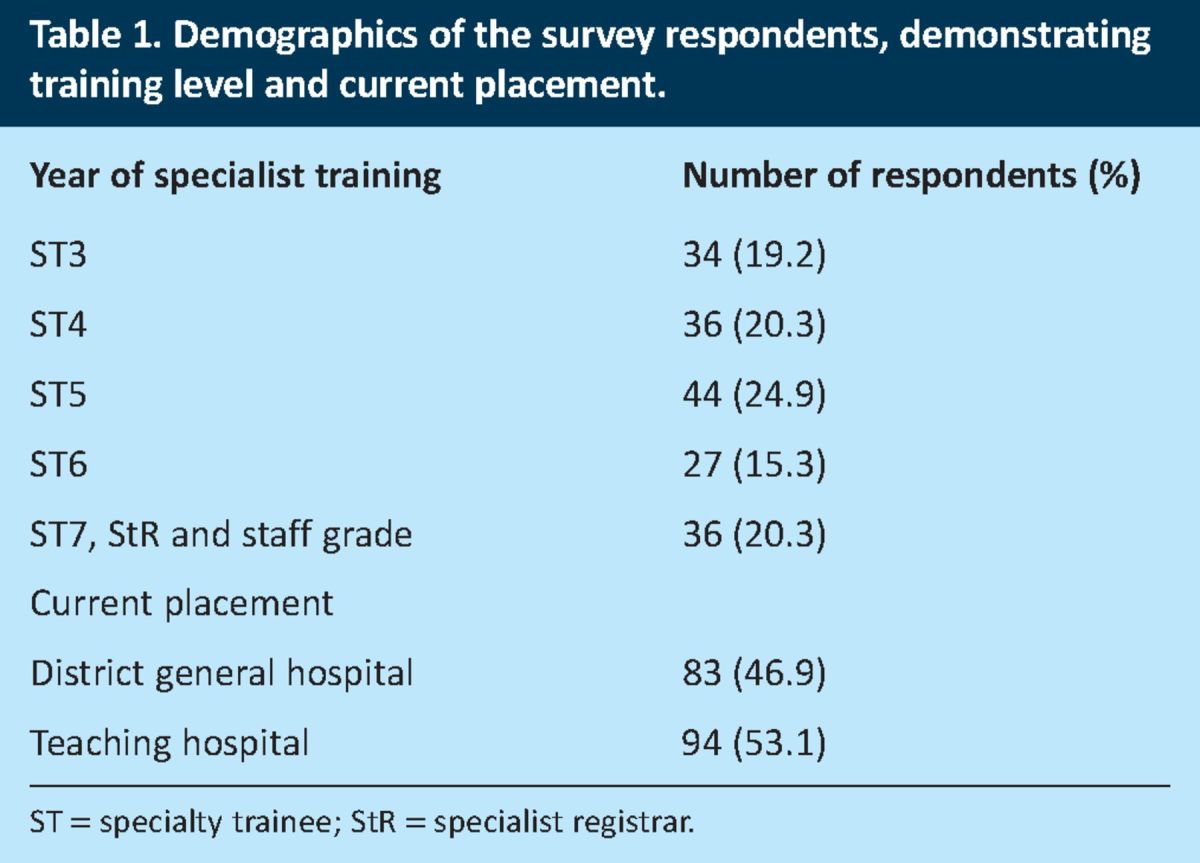
The survey was conducted over a 4-week period in the summer of 2011. 177 responses were recorded from UK postgraduate deaneries, with most from the Yorkshire and the Humber Deanery (20.3%), Scotland (13.6%) and the London Deanery (11.3%). When specialty trainee level 7 (ST7), specialist registrar (StR) and staff grades were added together, there was an even distribution of training level with approximately one-fifth of responses in each training grade (Table 1). Around 53% of responders were in teaching hospitals. Fewer than 23% of trainees were in hospitals with a dedicated pleural disease service (25.0% in district general hospitals (DGHs), 19.1% in teaching hospitals).
Table 1. .
Demographics of the survey respondents, demonstrating training level and current placement.
Ultrasound training
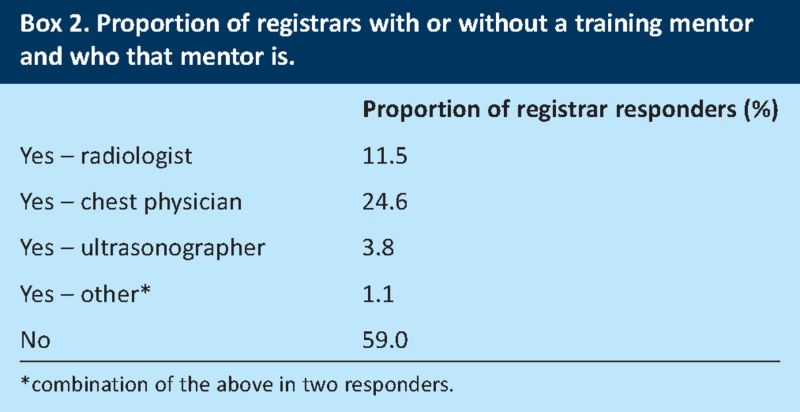
Only 15.3% of responders had a regular dedicated training session, with those in teaching hospitals (20.2%) more likely to have such a session than those in than DGHs (9.6%) (χ2 = 3.81, p = 0.05) (Table 2). Approximately 40% of trainees had a training mentor, in the majority of cases a chest physician (Box 2). Trainees whose current placement was in a teaching hospital were no more or less likely to have a mentor than those in DGHs.
Table 2. .
Access to regular ultrasound sessions, ultrasound training mentor and to ultrasound on the ward, characterised by current placement.
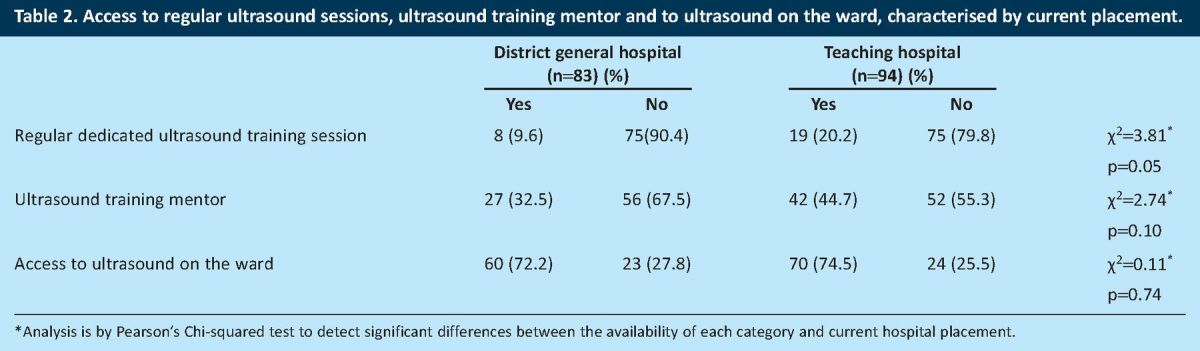
Most trainees had access to ultrasound on the ward (73.5%), and again there was no difference when analysed by current placement (Table 2). Nearly three-quarters of trainees had attended a thoracic ultrasound training course.
Current competency and log book
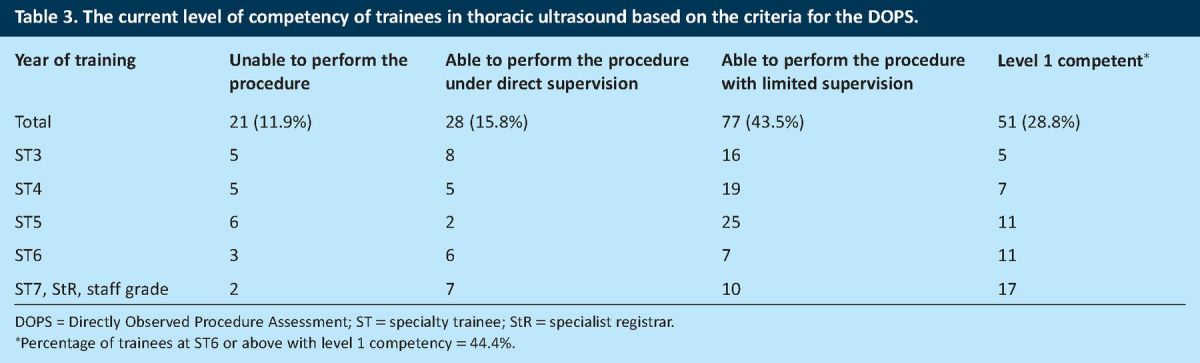
Of the trainees who responded, 28.8% had achieved level 1 competency and 43.5% were able to perform the procedure with limited supervision (Table 3). Of those who were ST6 or above, 44.4% had achieved level 1 competency. Fewer than 10% recorded a complication using ultrasound monitored procedures, mainly pneumothoraces. Only 63% of trainees are currently recording a log book.
Table 3. .
The current level of competency of trainees in thoracic ultrasound based on the criteria for the DOPS.
Frequency of ultrasound scanning for other departments or specialties
Nearly one-quarter of trainees were asked on a weekly basis to perform an ultrasound for another department, with some being asked daily; one-third of trainees had never been requested to do this.
Discussion
This is the first nationwide survey to investigate the level of training and competency in thoracic ultrasound among respiratory medicine trainees in the UK. It assesses the acquisition of relevant knowledge, practice and training as well as competency and skill maintenance. There are a number of encouraging findings from this survey but also areas of concern.
The curriculum for respiratory medicine and the current medical literature recommend that trainees should gain knowledge of the cross-sectional ultrasound anatomy of the thorax and upper abdomen.9,11–13 This can be achieved through attendance at thoracic ultrasound training courses, which allow trainees to gain theoretical knowledge regarding the technique of ultrasound and provide some experience in recognising common pathologies. There are a number of such courses nationally and so it is not surprising that a large number of trainees reported that they have attended one. A further encouraging finding was that over 70% of trainees reported access to a thoracic ultrasound machine. This supports the results of the BTS national pleural procedures audit which revealed that 77% of respiratory departments had access to at least one ultrasound machine.14 Moreover, our survey showed that there was no significant difference in the availability of thoracic ultrasound between teaching and DGHs, which is reassuring given that trainees who are dual accredited spend over half of their specialty training outside the teaching hospital environment.
Our findings also highlighted some important deficiencies in thoracic ultrasound training. Current respiratory trainees are required to obtain level 1 thoracic ultrasound competency as a mandatory skill to be achieved by specialty training level 5 (ST5) and to provide evidence of continuing competency by maintaining a log book. This is driven by the requirement to improve the safety of pleural procedures.15,16 Our data show that fewer than one-third of responders have achieved level 1 ultrasound competency; indeed only 44.4% of trainees at grade ST6 or above have achieved this level of competency. Furthermore, only one-quarter of trainees reported access to thoracic ultrasound training sessions, with 20.2% and 9.6% of trainees reporting the availability of regular dedicated training sessions in teaching hospitals and DGHs, respectively. Given that a significant proportion of respiratory trainees have not obtained level 1 thoracic ultrasound competency by ST5, our findings raise concerns as to whether this curriculum requirement can currently be achieved.
While access to thoracic ultrasound training should be a priority issue, it is also important that trainees have a mentor to help them achieve competency. It was disappointing to find that 60% of respiratory trainees do not have a mentor, but there are potential explanations for this. Training should be supervised by a practitioner with level 2 competency or by a practitioner with level 1 competency with at least 2 years experience of level 1 practice.17 Currently, less than half of respiratory departments have at least one consultant with level 1 thoracic ultrasound competency and even fewer have someone with the level of competency required for supervision.14 Hopefully with time, more respiratory consultants will reach the appropriate level of competency needed to provide mentoring and training in thoracic ultrasound.
There are a number of other strategies for the improvement of thoracic ultrasound training. As respiratory trainees are performing thoracic ultrasound not only for their own patients but also for patients under other specialists, radiology department activity is being spared, potentially allowing scope to negotiate for the provision of training sessions by an experienced ultrasonographer. Funding might also be gained through appropriate coding for pleural procedures supported by thoracic ultrasound, as currently there are no fixed tariffs for thoracic ultrasound performed by a respiratory specialist.18 Furthermore, improved training in thoracic ultrasound can be delivered through specialist pleural services, as these provide access for trainees to a respiratory physician who is experienced in thoracic ultrasound or a radiologist with pleural interest,19 although currently those types of services are available only in a minority of hospitals. Finally, each region should endeavour to co-ordinate thoracic ultrasound training to allow trainees to gain an appropriate level of competence. For example, in the Yorkshire and the Humber Deanery, a regional pulmonary procedures committee has been established to supervise and co-ordinate training in pleural procedures including thoracic ultrasound.
There are some limitations to this study. As with any survey, the results are dependent on those who respond and how well the survey is distributed. Nonetheless, it is reassuring that a broadly even distribution of doctors of different grades responded and that the responders were distributed evenly between district and teaching hospitals. The survey had a reasonable overall response with responders representing all but one deanery. Finally, the criteria for competency that are currently used have little in the way of validation against clinical results, so these data can only be a ‘snap-shot’ of current practice that can be used to help drive awareness and improve exposure to this important emerging skill.
Conclusions
In conclusion, thoracic ultrasonography is an important skill that has become an integral part of the curriculum in respiratory medicine. Our findings will hopefully highlight the need for more structured training and mentoring. We suggest that an easy method of monitoring training levels would be to incorporate some of our questions into the BTS national pleural procedures audit.
Box 1. Full list of questions asked in the national thoracic ultrasound training survey.
Box 2. Proportion of registrars with or without a training mentor and who that mentor is.
References
- 1.Hooper C, Lee YCG, Maskell NA. Investigation of a unilateral pleural effusion in adults: British Thoracic Society pleural disease guideline 2010. Thorax 2010;65:ii4-17. 10.1136/thx.2010.136978 [DOI] [PubMed] [Google Scholar]
- 2.Havelock T, Teoh R, Laws D, Glesson F, BTS Pleural Disease Guideline Group. Pleural procedures and thoracic ultrasound: British Thoracic Society pleural disease guidelines 2010. Thorax 2010;65:ii61-76. 10.1136/thx.2010.137026 [DOI] [PubMed] [Google Scholar]
- 3.Koenig SJ, Narasimhan M, Mayo PH. Thoracic ultrasonography for the pulmonary specialist. Chest 2011;140:133-41. 10.1378/chest.11-0348 [DOI] [PubMed] [Google Scholar]
- 4.Weingardt JP, Guico RR, Nemcek, Jr AA, et al. Ultrasound findings following failed, clinically directed thoracocentesis. J Clin Ultrasound 1994;22:419-26. 10.1002/jcu.1870220702 [DOI] [PubMed] [Google Scholar]
- 5.Feller-Kopman D. Therapeutic thoracocentesis: the role of ultrasound and pleural manometry. Curr Opin Pulm Med 2007;3:312-8. 10.1097/MCP.0b013e3281214492 [DOI] [PubMed] [Google Scholar]
- 6.Mayo PH, Goltz HR, Tafreshi M, Doelken P. Safety of ultrasound-guided thoracentesis in patients receiving mechanical ventilation. Chest 2004;125:1059-62. 10.1378/chest.125.3.1059 [DOI] [PubMed] [Google Scholar]
- 7.Gordon CE, Feller-Kopman D, Balk EM, Smetana GW. Pneumothorax following thoracentesis: a systematic review and meta-analysis. Arch Intern Med 2010;170:332-9. 10.1001/archinternmed.2009.548 [DOI] [PubMed] [Google Scholar]
- 8.Kastelik JA, Alhajji M, Faruqi S, et al. Thoracic ultrasound: an important skill for respiratory physicians. Thorax 2009;64:825-6. 10.1136/thx.2009.115378 [DOI] [PubMed] [Google Scholar]
- 9.Competence Based Curricula and Assessment — StRs. www.jrcptb.org.uk/trainingandcert/ST3-SpR/Pages/Respiratory-Medicine.aspx#Curriculum-Assessment [Accessed 5 June 2013] [Google Scholar]
- 10.Kwiksurveys www.kwiksurveys.com. [Accessed 5 June 2013] [Google Scholar]
- 11.Wrightson JM, Maskell NA. Thoracic ultrasound for beginners: utility and training issues for clinicians. Br J Hosp Med 2011;72:325-30. [DOI] [PubMed] [Google Scholar]
- 12.Wrightson JM, Fysh E, Maskell NA, Lee YC. Risk reduction in pleural procedures: sonography, simulation and supervision. Curr Opin Pulm Med 2010;16:340-50. 10.1097/MCP.0b013e32833a233b [DOI] [PubMed] [Google Scholar]
- 13.Mayo PH, Beaulieu Y, Doelken P, et al. American College of Chest Physicians/La Société de Réanimation de Langue Française Statement on competence in critical care ultrasonography. Chest 2009;135:1050-60. 10.1378/chest.08-2305 [DOI] [PubMed] [Google Scholar]
- 14.Hooper C, Maskell NA. British Thoracic Society national pleural procedures audit 2010. Thorax 2011;66:636-7. 10.1136/thoraxjnl-2011-200077 [DOI] [PubMed] [Google Scholar]
- 15.Harris A, O’Driscoll BR, Turkington PM. Survey of major complications of intercostal chest drain insertion in the UK. Postgrad Med J 2010;86:68-72. 10.1136/pgmj.2009.087759 [DOI] [PubMed] [Google Scholar]
- 16.NHS National Patient Safety Agency. Chest drains: risks associated with the insertion of chest drains. London: NHS National Patient Safety Agency, 2008. www.nrls.npsa.nhs.uk/resources/?entryid45 = 59887&q = 0%c2%acchest+drains%c2%ac [Accessed 5 June 2013]. [Google Scholar]
- 17.The Royal College of Radiologists. Ultrasound training recommendations for medical and surgical specialties. London: RCR, 2012. www.rcr.ac.uk/docs/radiology/pdf/BFCR(12)17_ultrasound_training.pdf [Accessed 5 June 2013]. [Google Scholar]
- 18.British Thoracic Society A guide to coding of respiratory care. London: BTS, 2012. www.brit-thoracic.org.uk/delivery-of-respiratory-care/a-guide-to-coding-of-respiratory-care.aspx. [Accessed 5 June 2012]. [Google Scholar]
- 19.Hooper C, Lee YCG, Maskell NA. Setting up a specialist pleural disease service. Respirology 2010;15:1028-36. 10.1111/j.1440-1843.2010.01832.x [DOI] [PubMed] [Google Scholar]