Sodium (Na+) is the main electrolyte in the extracellular compartment (ECC) and its level represents the relative content of sodium in relation to water. Sodium loss in excess of water loss or water gain will result in hyponatraemia, while water loss in excess of sodium or sodium excess will result in hypernatraemia. The body regulates serum Na+ through:
aldosterone, by exchanging potassium for Na+ at the distal tubule
vasopressin by water reabsorption in the collecting ducts
angiotensin II by Na+ reabsorption in the proximal tubule, and
atrial natriuretic peptide by suppressing the renin-angiotensin-aldosterone system and Na+ excretion from the collecting duct.
Hyponatraemia
Although hyponatraemia is a relative decrease of Na+ to water, in practice it is almost always dilutional with a low plasma osmolality, indicating that water intake has exceeded water excretion.1 It is the most common disorder of electrolytes encountered in clinical practice, occurring in up to 15–30% of hospitalised patients.2
Clinical features
Although an arbitrary division, hyponatraemia is considered acute if it develops within 48 hours or chronic if it takes longer.1 The former results in brain oedema, causing nausea and malaise when the Na+ is 125–130 mmol/l. Headache, obtundation, convulsion, coma and death may ensue when serum Na+ is below 110–115 mmol/l. Although chronic hyponatraemia is considered asymptomatic above this level, subtle symptoms may be present at a higher Na+ concentration (.120 mmol/l) (eg lethargy and dizziness) and an even higher risk of falls presumably due to unsteadiness.3
Brain adaptation
The brain adapts to hyponatraemia after 48 hours by shifting solutes to the ECC, thereby protecting itself from cell oedema. This adaptive mechanism takes days to develop fully. Correcting hyponatraemia rapidly (.10–12 mmol/l/day) causes fluid to shift from the intracellular compartment (ICC) to the ECC. Consequently, the brain limits cell shrinkage by the reuptake of solutes to prevent water escape. This reuptake is slower than the initial loss and the brain cells shrink as a result of a net fluid loss, resulting in osmotic demyelination in different parts of the brain, notably the pons. Risk factors for osmotic demyelination are alcoholic cirrhosis and hypoxia, while premenopausal women and endurance athletes are at high risk of brain damage or death from hyponatraemia.4,5
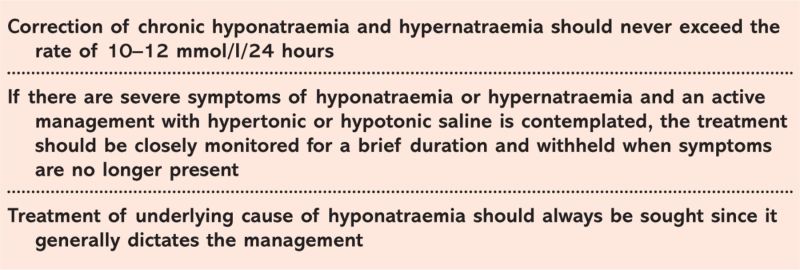
Key Points.
Classification
Solutes that are impermeable to the cell membrane are osmotically active. Na+ and its accompanying electrolytes account for 86% of plasma osmolality.6 Therefore, hyponatraemia is synonymous with hypotonicity, but in two circumstances the hyponatraemia and osmolality are discordant: first, pseudohyponatraemia in hyperlipidaemia which artificially lowers Na+ while the directly measured osmolality is unchanged. The second is isotonic or hypertonic hyponatraemia, for example hypertonic hyponatraemia due to hyperglycaemia where it is preferable to measure plasma osmolality either using direct measurement or correcting the measured sodium for the glucose elevation (2.4 mmol/l decrease in Na+ for each 5.6 mmol/l increase in glucose).7,8 Other solutes unaccounted for by the calculated osmolality (osmolality52[Na+]1 glucose1urea) could also elevate the plasma osmolality when measured directly, giving rise to an osmolar gap (eg mannitol, methanol and ethylene glycol). This should prompt a careful history and toxicology screen.
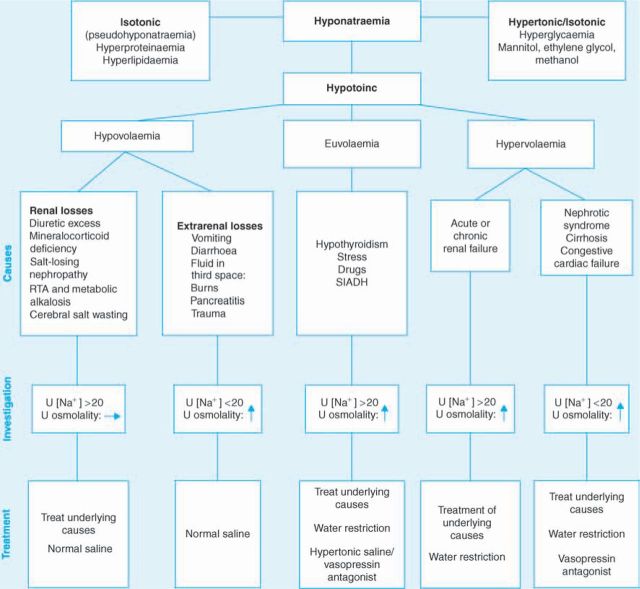
Based on the volume status, hypotonic hyponatraemia is separated into euvolaemic, hypovolaemic and hypervolaemic hyponatraemia (Fig 1).
Fig 1.
Flowchart for the management of hyponatraemia. RTA = renal tubular acidosis; SIADH = syndrome of inappropriate secretion of antidiuretic hormone; U = urine.
Treatment
Hyponatraemia can be corrected by fluid restriction, salt replacement, vasopressin antagonist or a combination of the three. In hypovolaemia, correcting fluid depletion with saline is the mainstay of therapy and will correct the relative water excess. Hypervolaemia requires treatment of the underlying disorder and fluid restriction alone or with a vasopressin antagonist, while water restriction with or without salt replacement is indicated when euvolaemia is present.
Correction rate
Treatment of hyponatraemia is not without its complications so there needs to be careful consideration of the risks and benefits of aggressive versus slower correction. The general principle with hyponatraemia is that the rate of correction should be closely linked to the rate of development. However, in the practical setting, it is difficult to distinguish between acute and chronic onset and a more appropriate approach is to decide on the rate of correction on the basis of presence and severity of symptoms.
Severe symptoms. For those with severe symptoms of any cause (eg convulsion), aggressive treatment with 1.8–3% hypertonic saline is indicated (in some UK hospitals hypertonic saline is available as 1.8% only). The aim is to elevate the Na+ by 1.0 mmol/hour in the first 2–3 hours or until symptoms disappear, while keeping the target for the first 24 hours below 10 mmol/l to avoid osmotic demyelination. This can be achieved only with close monitoring to avoid exceeding these limits. The rate of infusion of 3% hypertonic saline per hour can be crudely calculated by multiplying the weight in kg by the rate of Na+ correction required per hour.8 For example, a 70 kg subject will require approximately 70 ml/hour of 3% hypertonic saline to elevate the Na+ by 1.0 mmol/l/hour – but this is no substitute for regular monitoring during therapy.
Mild symptoms. In chronic hyponatraemia with mild symptoms (Na+,110–115 mmol/l), a challenging clinical decision has to be made to pursue either active correction with intravenous (iv) infusion of saline or slower methods of correction (ie fluid restriction to 500 ml/day below the daily urine volume).8
In active intervention, a lower correction rate than for acute hyponatraemia is used: 1.8–3% hypertonic saline to increase Na+ by 0.5 mmol/hour in the first few hours, with total correction no more than 10 mmol/l/day to avoid osmotic demyelination.
It should be stressed that treatment should be halted if any of the following is achieved9:
cessation of symptoms
Na+ reaches 120 mmol/l, or
10 mmol/l increase in Na+ occurs within the first 24 hours.
Pragmatically, there needs to be a very good reason for actively infusing hypertonic saline rather than fluid restriction alone with biochemical reassessment after 12 and 24 hours.
Type of fluid
Severe symptomatic hyponatraemia of any cause: hypertonic saline, as outlined above. Hypertonic saline may be available in several strengths, so it is crucial to double check that the correct prescription is implemented.
Symptomatic hypovolaemic hyponatraemia: isotonic saline is sufficient in most cases.8
Chronic hypovolaemic hyponatraemia: discretion needs to be exercised as euvolaemia will suppress vasopressin, causing water diuresis and accelerated correction of Na+. Therefore, vasopressin use may be required to slow down Na+ rise. An alternative approach is to infuse hypertonic saline.
Symptomatic euvolaemic hyponatraemia (ie syndrome of inappropriate secretion of antidiuretic hormone): hypertonic saline infusion should be used (with the caveats noted above). Isotonic saline will result in further lowering of Na+ due to increased net sodium excretion because water, not sodium handling, is at fault in the kidneys.
The new vasopressin antagonist drugs can be used in hypervolaemic and euvolaemic hyponatraemia. They may have a role in causing aquaresis through blocking the vasopressin effect on V2 receptor in the collecting duct.10,11
Hypernatraemia
Hypernatraemia always denotes hypertonic hyperosmolality with ICC shrinkage.12 Even if there is salt-free water diuresis (eg nephrogenic or central diabetes insipidus), hypernatraemia does not ensue unless there is low free water intake (eg hypothalamic lesion of thirst centre or lack of access to water). It is thus common in the intubated, infirmed and infants with hypotonic diarrhoea.
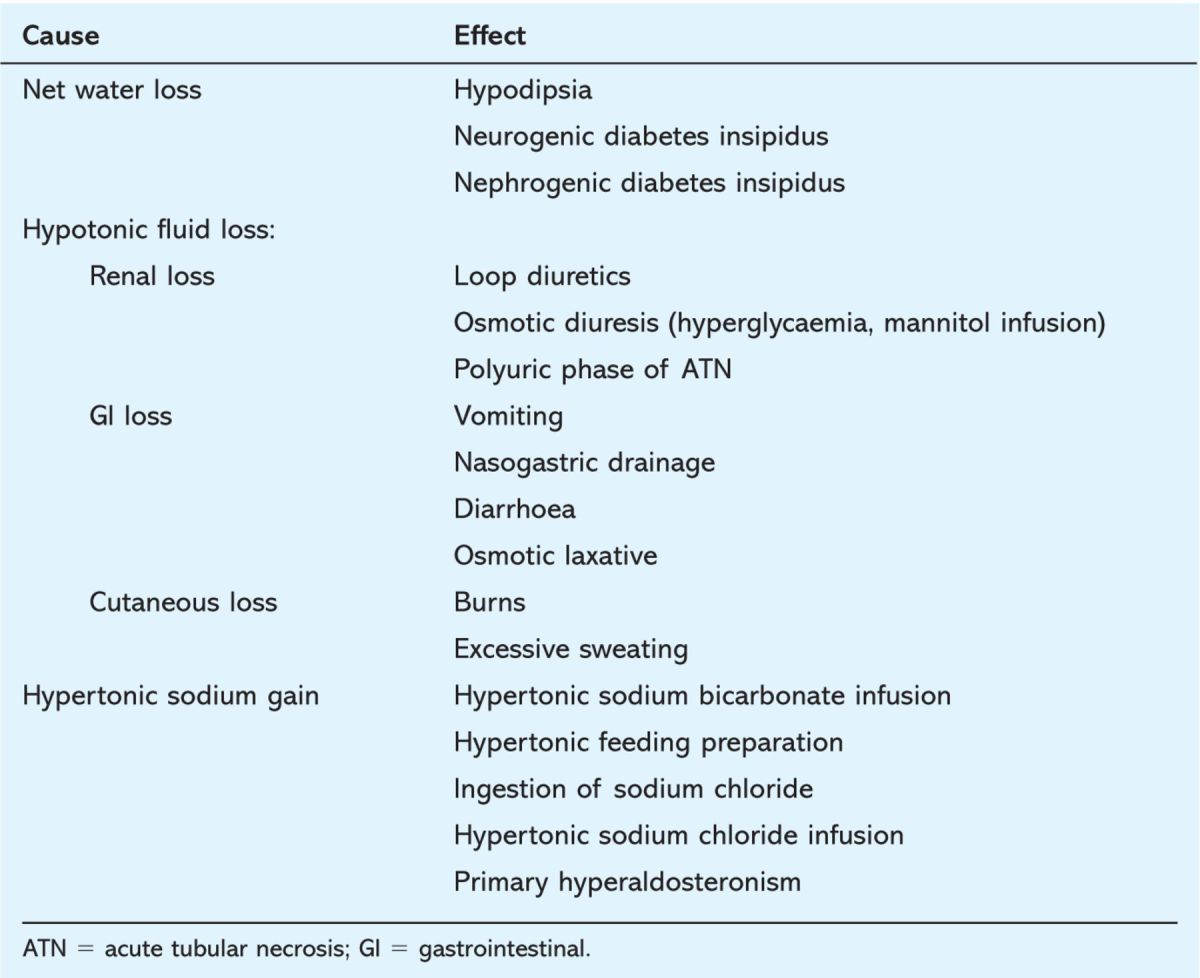
The brain reacts by solutes uptake to shift water from the ECC to the ICC, thereby preventing cell shrinkage, a consequence of severe (.160 mmol/l) or rapid onset (,12 hours) hypernatraemia which can lead to intracranial bleeding, convulsion and coma. Table 1 lists causes of hypernatraemia.
Table 1.
Causes of hypernatraemia.
Treatment
Treatment of hypernatraemia requires attendance to the underlying cause and reduction of serum Na+ by hypotonic fluid. It is safest to administer the fluid through the oral or enteral route. If iv administration is used, it should be hypotonic (0.45% hypotonic saline or 5% dextrose) unless isotonic fluid is required in haemodynamically compromised subjects.
Correction rate
The same general principle is followed when considering the rate of correction: rapid onset hypernatraemia can be safely reduced by a rate of 1 mmol/ l/hour with the aim of not exceeding more than 10–12 mmol/l/24 hours.1,12 In chronic hypernatraemic states, the target correction should be no more than 0.5 mmol/l/hour (12 mmol/l/24 hours) to avoid brain oedema and prevent potential osmotic demyelination.
To estimate the change in Na+ following the infusion of 1 litre of fluid, the following formula is used:
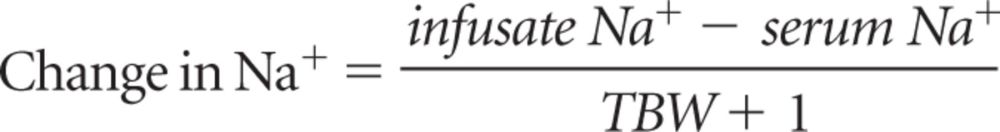 |
(infusate Na+ is concentration of sodium in the infused fluid in mmol/l; serum Na+ is concentration of sodium in serum in mmol/l; TBW 5 total body water, 0.5 and 0.613 of body weight in kg in women and men, respectively)
The Na+ correction required per unit time is then divided by the change in Na+ from the formula to obtain the fluid volume to effect that correction.12–14 Measured and insensible fluid loss allowance is added to make up the final volume to be infused over that time.
Conclusions
The cause of the hypo- and hypernatraemia will guide the correct treatment, but in both scenarios the correction needs care. If in doubt, slower rather than rapid correction is the best policy.
References
- 1.Capasso G, Robert U.Electrolytes and acid-base: common fluid and electrolyte disorders. Medicine 2007;35:368–76 [Google Scholar]
- 2.Hawkins RC.Age and gender as risk factors for hyponatremia and hypernatremia. Clin Chim Acta 2003;337:169–72 10.1016/j.cccn.2003.08.001 [DOI] [PubMed] [Google Scholar]
- 3.Renneboog B, Musch W, Vandemergel X, Manto MU, Decaux G.Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits. Am J Med 2006;119:71. 10.1016/j.amjmed.2005.09.026 [DOI] [PubMed] [Google Scholar]
- 4.Ayus JC, Wheeler JM, Arieff AI.Postoperative hyponatremic encephalopathy in menstruant women. Ann Intern Med 1992;117:891–7 [DOI] [PubMed] [Google Scholar]
- 5.Siegel AJ.Exercise-associated hyponatremia: role of cytokines. Am J Med 2006;119(Suppl 1)S74–8 10.1016/j.amjmed.2006.05.012 [DOI] [PubMed] [Google Scholar]
- 6.Weiss-Guillet EM, Takala J, Jakob SM.Diagnosis and management of electrolyte emergencies. Best Pract Res Clin Endocrinol Metab 2003;17:623–51 10.1016/S1521-690X(03)00056-3 [DOI] [PubMed] [Google Scholar]
- 7.Hillier TA, Abbott RD, Barrett EJ.Hyponatremia: evaluating the correction factor for hyperglycemia. Am J Med 1999;106:399–403 10.1016/S0002-9343(99)00055-8 [DOI] [PubMed] [Google Scholar]
- 8.Verbalis JG, Goldsmith SR, Greenberg A, Schrier RW, Sterns RH.Hyponatremia Treatment Guidelines 2007: Expert Panel Recommendations. Am J Med 2007;120(Suppl 1)S1–26 10.1016/j.amjmed.2007.09.001 [DOI] [PubMed] [Google Scholar]
- 9.Verbalis JG.Disorders of body water homeostasis. Best Pract Res Clin Endocrinol Metab 2003;17:471–503 10.1016/S1521-690X(03)00049-6 [DOI] [PubMed] [Google Scholar]
- 10.Greenberg A, Verbalis JG.Vasopressin receptor antagonists. Kidney Int 2006;69:2124–30 10.1038/sj.ki.5000432 [DOI] [PubMed] [Google Scholar]
- 11.Cawley MJ.Hyponatremia: current treatment strategies and the role of vasopressin antagonists. Ann Pharmacother 2007;41:840–50 10.1345/aph.1H502 [DOI] [PubMed] [Google Scholar]
- 12.Adrogue HJ, Madias NE.Hypernatremia. N Engl J Med 2000;342:1493–9 10.1056/NEJM200005183422006 [DOI] [PubMed] [Google Scholar]
- 13.Adrogue HJ, Madias NE.Aiding fluid prescription for the dysnatremias. Intensive Care Med 1997;23:309–16 10.1007/s001340050333 [DOI] [PubMed] [Google Scholar]
- 14.Kang SK, Kim W, Oh MS.Pathogenesis and treatment of hypernatremia. Nephron 2002;92(Suppl 1)14–7 10.1159/000065372 [DOI] [PubMed] [Google Scholar]