The Dementia Commissioning for Quality and Innovation (Dementia CQUIN) document published by the UK Government Department of Health in 2012 sought to promote a proactive approach to dementia diagnosis by recommending that all individuals aged 75 years or over should be asked a single screening question: ‘Have you been more forgetful in the past 12 months to the extent that it has significantly affected your life?’1
The hope was that such screening would, if answered in the affirmative, initiate a ‘dementia risk assessment’ (exact nature unspecified) and thus help to close the gap between observed and expected numbers of dementia diagnoses.2 However, concerns have been voiced about the lack of evidence for such a screening policy,3 and the risk that it might promote overdiagnosis of dementia.4
Although the screening question may have face validity, its ability to identify patients with and without dementia is, to our knowledge, unknown. We sought to investigate this by asking the screening question to 100 consecutive patients attending a dedicated epilepsy outpatient clinic, on the grounds that subjective memory complaints are common in this patient population, related to underlying diagnosis, medication effects and comorbid affective disorder.
Nearly half of the patients questioned (48%) answered in the affirmative, although only one was aged greater than 75 years. No patient was adjudged to have dementia, although one 73-year-old man was thought to have mild cognitive impairment on the basis of repetitive questioning and getting lost if he went out alone.
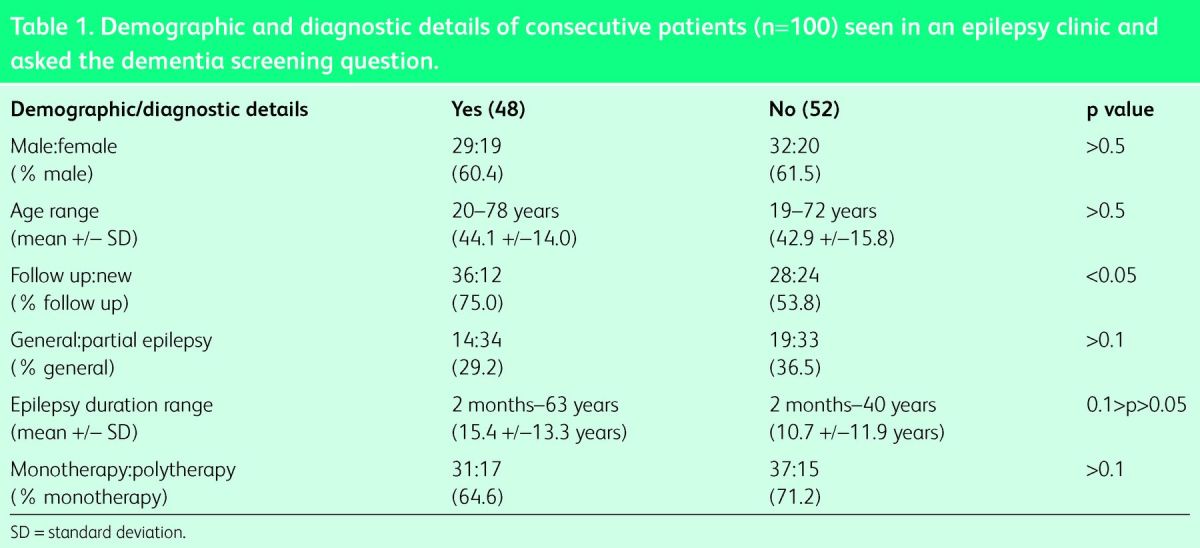
Comparing the groups answering yes and no (t tests for continuous variables, chi-squared tests for categorical variables; Table 1), no difference was found in sex ratio, age, seizure type or use of antiepileptic drugs (monotherapy vs polytherapy). Those answering in the affirmative were more likely to be follow-up than new patients. Although the difference in the duration of epilepsy in the two groups did not reach statistical significance, there was a trend to longer duration in the yes group. The limited sample size may have contributed to this result.
Table 1.
Demographic and diagnostic details of consecutive patients (n = 100) seen in an epilepsy clinic and asked the dementia screening question.
In those answering yes, examples of memory problems were sought. The most common were forgetting to attend appointments or to take medications, and forgetting to switch off appliances. These may be examples of memory lapses, common in everyday life and related to attentional rather than mnestic function, and not suggestive of an underlying neurodegenerative disorder.
These data suggest that the dementia screening question has very low specificity, and hence will identify many false positives, as previously suggested.4 It may be endorsed by individuals with purely subjective memory impairment.
There may be a parallel here with other centrally conceived health policies and directives, such as the guidelines for brain/CNS cancer identification (‘2-week referrals’) which generate large numbers of referrals, very few of whom have a tumour.5 If screening of this kind is to be implemented as a matter of public policy, then resources appropriate to deal with the anticipated increase in referrals will be required.
References
- 1.Department of Health Using the Commissioning for Quality and Innovation (CQUIN) payment framework. Guidance on the new national goals 2012–13. London: Department of Health, 2012. [Google Scholar]
- 2.Alzheimer's Society Mapping the Dementia Gap 2012. Progress on improving diagnosis of dementia 2011–2012. London: Alzheimer's Society, 2013. [Google Scholar]
- 3.Brunet MD, McCartney H, Heath I, et al. There is no evidence base for proposed dementia screening. BMJ 2012;345:e8588. 10.1136/bmj.e8588 [DOI] [PubMed] [Google Scholar]
- 4.Brunet M. Targets for dementia diagnoses will lead to overdiagnosis. BMJ 2014;348:g2224. 10.1136/bmj.g2224 [DOI] [PubMed] [Google Scholar]
- 5.Panicker J, Larner AJ. Two-week wait referrals for CNS cancer – are they working? J Neurol Neurosurg Psychiatry 2012;83(Suppl 2): A30–1. 10.1136/jnnp-2012-304200a.112 [DOI] [Google Scholar]


