ABSTRACT
Research to identify whether dizziness is a geriatric syndrome has largely overlooked often treatable vestibular causes. To ascertain the degree to which vestibular and other causes of dizziness interact in older people, an eight-month retrospective case-note review was undertaken in patients aged ≥65 years referred with dizziness or imbalance to an audiovestibular medicine clinic. Of 41 patients aged 65–93 years old, 15 (37%) had multiple symptom triggers, 23 (56%) had recent dizziness-related falls, 24 (59%) and 10 (24%) had peripheral and central vestibular causes for dizziness respectively, whereas 6 (15%) had both. Sixteen (39%) had benign paroxysmal positional vertigo, of which 13 (32%) had an additional peripheral vestibular impairment. Twenty-six (63%) had other (general medical/cardiac) causes; of these 13 (50%) also had vestibular causes. Polypharmacy, orthostatic hypotension, psychotropic drug use and anxiety were common contributory factors. Vestibular causes of dizziness contribute to a multifactorial geriatric syndrome. All patients with dizziness and falls should have a vestibular assessment (especially peripheral) to improve quality of life and reduce falls.
KEYWORDS : dizziness, geriatric syndrome, vestibular impairment, older people
Introduction
It is recognised that causes of dizziness (which encompass vertigo, disequilibrium, presyncope and more non-specific symptoms) are multiple and often highly complex. Dizziness is reported in over 30% of those aged ≥65 years,1 with a high incidence of benign paroxysmal positional vertigo (BPPV) and peripheral vestibular impairment (PVI) in elderly people.2,3 Both can result in non-specific dizziness and, significantly, dizziness is a strong risk factor for falls.4,5 As the population continues to age,6 the prevalence of these problems is rising. There is low recognition by clinicians that many peripheral vestibular symptoms are treatable,7 despite evidence that treating BPPV reduces falls8 and customised vestibular physiotherapy improves quality of life9 in elderly people.
Traditionally a syndrome is defined as a collection of signs or symptoms associated with a single diagnosis or condition, which typically has a known aetiology and pathophysiology. In contrast, geriatric syndromes describe a single manifestation (eg falls, incontinence or delirium) in an older person, with multiple aetiological factors and interacting pathophysiological pathways.10 It is important to recognise which clinical conditions may represent geriatric syndromes, so that clinical assessments and systems allow the thorough, multi-system, meticulous approach required to manage them. This will often involve management with a multidisciplinary team rather than a lone physician.
Previous research11,12 suggests that dizziness is a multifactorial (geriatric) syndrome but does not include specific assessments for peripheral and central vestibular causes of dizziness. Kao et al11 retrospectively evaluated 262 consecutive patients aged ≥60 years attending a geriatric assessment centre. They identified seven independent factors for dizziness (depressive symptoms, cataracts, abnormal balance or gait, postural hypotension, diabetes, past myocardial infarction, and the use of three or more medications). They found that the incidence of dizziness rose greatly in patients with higher numbers of risk factors. Gassmann and Rupprecht12 recruited 620 community-dwelling people aged 65 years and demonstrated multiple predictors for dizziness, noting that these were similar for falls; 59.7% had dizziness provoked by multiple positions or activities.
The aims of our study were to ascertain:
if dizziness in the older person could be categorised as a ‘geriatric syndrome’
to what extent peripheral and central vestibular causes of dizziness coexist with each other and with other known causes of dizziness in an older population referred for specialist assessment.
Although a detailed guide for assessing vestibular disorders in the older dizzy patient is beyond the scope of this paper, a basic structure for assessment of peripheral vestibular disorders is included because these are less commonly recognised by non-specialists.
Methods
This audiovestibular medicine (AVM) clinic was based in a district general hospital and predominantly included patients with complex balance problems. Referrals were accepted from secondary care and general practitioners (GPs). There was a close working relationship with the geriatrician-led falls clinic, neurology and ear, nose and throat (ENT) departments. Patients were seen by a single audiovestibular physician or the same AVM trainee, vestibular physiotherapist and audiology team attached to this clinic. They underwent a thorough evaluation as detailed below. The unit has a holistic approach to vestibular rehabilitation. This included, as necessary, customised exercises for peripheral vestibular impairment and exercises aimed at improving core stability, muscle strengthening, gait retraining and relaxation, as well as non-pharmacological measures for orthostatic hypotension and migraine.
An eight-month retrospective review was undertaken of all patients aged ≥65 years referred to this AVM clinic between 1 January and 31 August 2010 with vertigo, ‘dizziness’, disequilibrium or other balance disorder. All history, assessments, diagnoses, treatment and management plans were made or confirmed by the consultant audiovestibular physician. Some data, ie comorbidity and medication, were obtained from the referrer letter and hospital records. Additional data were taken from vestibular physiotherapist records.
A form was designed to include demographic details, detailed balance and systemic history including duration of dizziness, falls, medication, comorbidities, lying and standing blood pressure using recognised methods,13 bedside neuro-otological assessment and relevant neurological examination (Box 1). Not all assessments were possible on every patient for a variety of reasons ie musculoskeletal problems or poor functional status.
Box 1. Structure for a neuro-otological assessment.14,15
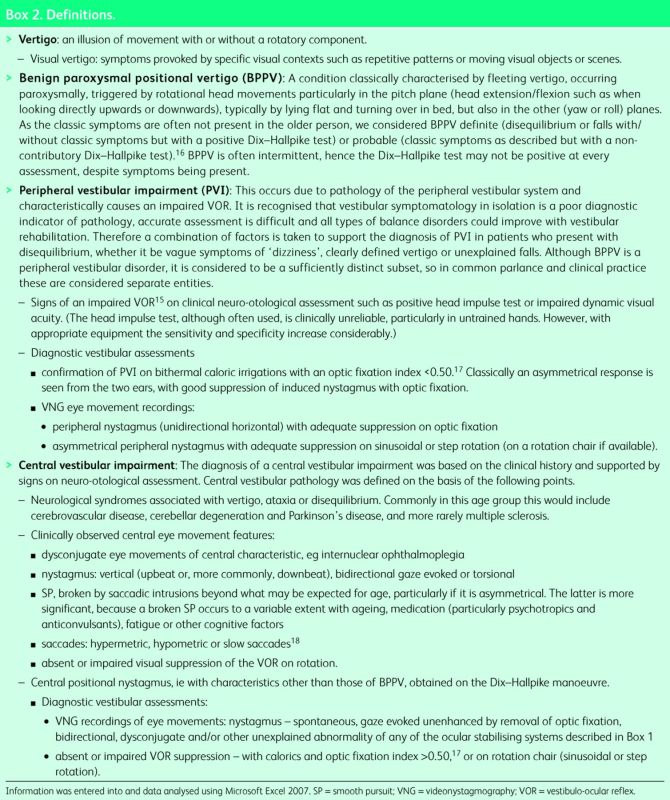
Data were also collected on specific audiovestibular tests (Box 1) and other laboratory or radiological assessments undertaken as required. Definitions are provided in Box 2.
Box 2. Definitions.
Results
Forty-one consecutive patients aged ≥65 years were included with no missing data. The age range was 65–93 years, with a median age of 76. Thirty patients (73%) were female. All patients were outpatients living in the community, with no care home residents assessed during this period.
Twenty-nine referrals (71%) were from secondary care. The largest source of referrals (18 patients, 44%) was from geriatricians (of whom 15 (83%) had attended the falls clinic). Other referrals were from the service's own vestibular physiotherapist (who received referrals independently from the community physiotherapy, neurorehabilitation and stroke teams, seven patients, 17%), neurology (two patients, 5%) and ENT (two patients, 5%). GPs referred 12 patients (29%).
There was considerable overlap of symptoms of imbalance. Vertigo was documented in 38 (93%), chronic imbalance in 40 (98%) and recent falls due to dizziness in 33 (81%). Symptoms had been present for a median of 24 months (range 3 months to 20 years).
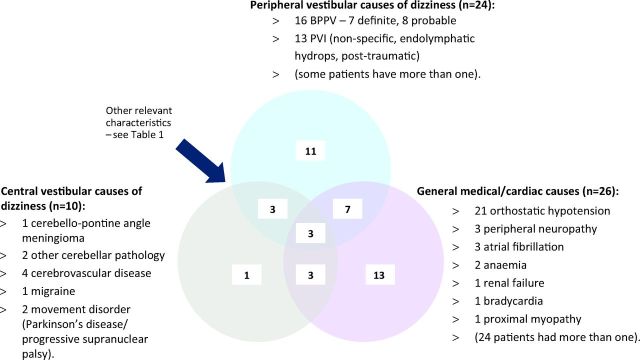
Twenty-six (63%) had general medical or cardiac causes for their symptoms. Two-fifths (16, 39%) had concomitant causes in two or all three of the different groups (central vestibular, peripheral vestibular and general medical/cardiac). Patients took a median of five medications per day (range 0–17). In addition, orthostatic hypotension (21/38, 55%), psychotropic medication (15, 37%), and anxiety (6, 15%) were common contributory factors (Table 1). Hearing loss of varying degrees, averaged across the five octave-interval frequencies from 250 Hz to 4 kHz (using recognised standards19), occurred in 29 (71%) patients, of whom 11 were mild, 14 moderate and 4 severe.
Table 1.
Relevant clinical characteristics of population sample.

Of 38 patients tested for orthostatic hypotension, 50% and 30% had a systolic drop of ≥20 mmHg immediately on standing and after 2–3 min, respectively; 63% and 12% had a diastolic drop of ≥10 mmHg immediately on standing and after 2–3 min, respectively.
Postural triggers of dizziness were the most common (31 patients, 76%), followed by visual triggers20 in 18 (44%), whereas 37% (15 patients) had more than one type of trigger.
Fig 1 shows the number diagnosed with peripheral vestibular, central vestibular and general medical/cardiac causes of dizziness. Overlap is shown where this exists.
Fig 1.
Venn diagram showing diagnosed peripheral and central vestibular, general medical and cardiac causes of dizziness. BPPV = benign paroxysmal positional vertigo; PVI = peripheral vestibular impairment.
Discussion
Through holistic assessment and analysis of peripheral and central vestibular causes of dizziness, vertigo and falls in this cohort, our findings indicate that vestibular impairment is a frequent cause of these symptoms in elderly people. Most often, however, patients use the vague term ‘dizziness’ to describe vertigo or symptoms that may precede non-accidental falls. Our findings extend and strengthen the literature on ‘dizziness’ as a geriatric syndrome that previously focused more on general medical comorbidity, polypharmacy and demographics.11,12 Although the definition of geriatric syndromes remains debatable, these are recognised as syndromes where multiple aetiological factors interact in a complex manner, resulting in a unified manifestation (in this case dizziness) that warrants specific multidisciplinary management and resources.10 The study also demonstrates the coexistence of peripheral and central vestibular causes of dizziness with each other and with other causes of dizziness in an older population. There are no criteria on how to unravel the multiple comorbidities in elderly patients with dizziness. However, it is very important to identify vestibular pathology because vestibular rehabilitation will aid compensation and therefore improve morbidity such as reducing symptoms and falls.
Notably, even before other well-established causes (polypharmacy, sensory impairment, psychological symptoms and co-morbid factors) of dizziness were taken into account, two-fifths (16/41, 39%) were diagnosed as having two or more causes for dizziness, including half (9/18, 50%) of those referred by geriatricians. If these well-established factors are included, these figures inevitably rise further, in keeping with previous work.11
High levels of prescription-drug usage were seen including high-risk medications (see Fig 1). Previous work has found a strong correlation between dizziness and four or more medications per day.12 Cognitive and visual impairment were not recorded routinely, making it difficult to comment on the contribution of these factors in this retrospective study.
Clearly those referred to a specialist AVM clinic are likely to have complex causes of dizziness and a high prevalence of peripheral vestibular disorders. However, notably in this study, a high proportion of those already seen by geriatricians, mostly via the falls service, had multifactorial causes. This emphasises the relevance of recognition of vestibular problems to falls specialists, especially in areas where an AVM service is not available.
The extent of awareness, diagnosis and management of patients with vestibular factors as a cause of their dizziness remains suboptimal. Vertigo has often been overdiagnosed as being due to causes such as cervical spondylosis, despite a lack of rigorous evidence that this condition in isolation is strongly linked to vertigo. All neck movements result in a concomitant head movement and any change in head position can make a vestibular disorder symptomatic. Furthermore, specific tests to confirm cervical vertigo are lacking. Therefore, it is much more useful to attempt to establish an alternative diagnosis that may be treatable, especially BPPV.14,21
Our findings help make the case for a robust multispeciality assessment of older patients with dizziness, falls and imbalance. Screening for peripheral and central vestibular causes of dizziness should be a routine component of assessing older people with balance disorders and falls;22 guidance and flow charts are available to aid clinicians.21,23 Many neuro-otological assessments (see Box 1) can be undertaken at the bedside or outpatient clinic without the need for assessments in a vestibular laboratory. However, training and practice are important in ensuring accuracy in ascertaining the relevant features.
We echo the call for ‘efficient, seamless movement’ between geriatrician-led falls clinics and balance/vertigo services, led by audiology teams, audiovestibular physicians or ENT specialists.24 In addition we argue that all local falls pathways should include guidance for referral for specialist assessment of those with suspected vestibular pathology.
Likewise, given the multifactorial nature of dizziness, there is considerable scope for geriatricians (as specialists in comprehensive geriatric assessment and general internal medicine) to contribute to management of patients seen in AVM or ENT clinics referred from different specialties, eg in none of the 41 patients was a bone health assessment made or new prescription of anti-osteoporotic agent initiated.
Conclusion
Our paper strengthens the literature by emphasising the role of often-treatable vestibular disorders in dizziness (as part of a geriatric syndrome), particularly as this aspect is largely unrecognised in the older population. Closer working between relevant professionals, education of health professionals and inclusion within curricula for specialist training for physicians are key to improving symptoms and costs by reducing falls and morbidity for older dizzy people. Additional research in this area, eg whether dizziness shares common risk factors with other geriatric syndromes,10 is important in consolidating this concept further.
Key points
Dizziness in older people is often multifactorial. It should be assessed and treated similarly to other geriatric syndromes with a thorough systematic approach.
Vestibular impairment is frequently a contributing factor to dizziness in older people.
All patients with dizziness and falls should be assessed for vestibular impairment as part of a systematic approach.
Acknowledgement
Thanks to Gillian Lomas (vestibular physiotherapist) at Bolton NHS Foundation Trust for assistance with provision of some missing data.
References
- 1.Whitney SL, Wrisley DM, Marchetti GF, Furman JM. The effect of age on vestibular rehabilitation outcomes. Laryngoscope 2002;112:1785–90. 10.1097/00005537-200210000-00015 [DOI] [PubMed] [Google Scholar]
- 2.Oghalai JS, Manolidis S, Barth JL, et al. Unrecognized benign -paroxysmal positional vertigo in elderly patients. Otolaryngol Head Neck Surg 2000;122:630–4. [DOI] [PubMed] [Google Scholar]
- 3.Von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry 2007;78:710–5. 10.1136/jnnp.2006.100420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tinetti ME, Williams CS, Gill TM. Health, functional, and -psychological outcomes among older persons with chronic -dizziness. J Am Geriatr Soc 2000;48:417–21. [DOI] [PubMed] [Google Scholar]
- 5.O’Loughlin JL, Robitaille Y, Boivin JF, et al. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 1993;137:342–54. [DOI] [PubMed] [Google Scholar]
- 6.Office for National Statistics Annual mid-year population estimates, 2010. London: Office of National Statistics, 2011. Available at: www.ons.gov.uk/ons/rel/pop-estimate/population-estimates-for-uk–england-and-wales–scotland-and-northern-ireland/mid-2010-population-estimates/annual-mid-year-population–estimates–2010.pdf [Accessed 16 March 2014]. [Google Scholar]
- 7.Baloh RW. Dizziness in older people. J Am Geriatr Soc 1992;40:713–21. [DOI] [PubMed] [Google Scholar]
- 8.Gananca FF, Gazzola JM, Gananca CF, et al. Elderly falls associated with benign paroxysmal positional vertigo. Braz J Otorhinolaryngol 2010;76:113–20. 10.1590/S1808-86942010000100019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung JY, Kim JS, Chung PS, Woo SH, Rhec CK. Effect of vestibular rehabilitation on dizziness in the elderly. Am J Otorhinolaryngol 2009;30:295–9. 10.1016/j.ijporl.2008.10.020 [DOI] [PubMed] [Google Scholar]
- 10.Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric -syndromes: clinical, research, and policy implications of a core -geriatric concept. J Am Geriatr Soc 2007;55:780–91. 10.1111/j.1532-5415.2007.01156.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kao AC, Nanda A, Williams CS, Tinetti ME. Validation of -dizziness as a possible geriatric syndrome. J Am Geriatr Soc 2001;49:72–5. 10.1046/j.1532-5415.2001.49012.x [DOI] [PubMed] [Google Scholar]
- 12.Gassmann KG, Rupprecht R. Dizziness in an older community dwelling population: a multifactorial syndrome. J Nutr Health Aging 2009;13:278–82. 10.1007/s12603-009-0073-2 [DOI] [PubMed] [Google Scholar]
- 13.The Consensus Committee of the American Autonomic Society and the American Academy of Neurology Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. Neurology 1996;46:1470. 10.1212/WNL.46.5.1470 [DOI] [PubMed] [Google Scholar]
- 14.Bronstein A, Lempert T. Dizziness. A practical approach to diagnosis and management. Cambridge: Cambridge University Press, 2007. [Google Scholar]
- 15.Davies R. Bedside neuro-otological examination and interpretation of commonly used investigations. J Neurol Neurosurg Psychiatry 2004;75suppl IViv32–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pollak L. The importance of repeated clinical examination in patients with suspected benign paroxysmal positional vertigo. Otol Neurotol 2009;30:356–8. 10.1097/MAO.0b013e3181967b9c [DOI] [PubMed] [Google Scholar]
- 17.British Society of Audiology Recommended procedure. The caloric test. London: British Society of Audiology, 2010. Available at: www.thebsa.org.uk/docs/RecPro/CTP.pdf [Accessed 31 October 2013]. [Google Scholar]
- 18.Hain TC. Interpretation and usefulness of oculomotor testing Jacobson GP, Newman CW, Kartush JM.Handbook of balance function testing. San Diego, CA: Singular Publishing, 1997101–22. [Google Scholar]
- 19.British Society of Audiology Recommended procedure. Pure tone air-conduction and bone-conduction threshold audiometry with and without masking. London: British Society of Audiology, 2011. Available at: www.thebsa.org.uk/docs/docsfromold/BSA_RP_PTA_FINAL_24Sept11_MinorAmend06Feb12.pdf [Accessed 31 October 2013]. [Google Scholar]
- 20.Guerraz M, Yardley L, Bertholon P, et al. Visual vertigo: symptom assessment, spatial orientation and postural control. Brain 2001;124:1646–56. 10.1093/brain/124.8.1646 [DOI] [PubMed] [Google Scholar]
- 21.Brandt T, Dieterich M, Strupp M. Vertigo and dizziness. Common complaints. London: Springer, 2009;113:128–9. [Google Scholar]
- 22.Umapathy D, West P. Dizziness and balance disorders in older people. CME Geriatr Med 2005;7:126–35. [Google Scholar]
- 23.Barraclough K, Bronstein A. Diagnosis in general practice. Vertigo. BMJ 2009;339:b3493. [DOI] [PubMed] [Google Scholar]
- 24.Lawson J, Johnson I, Bamiou DE, Newton J. Benign paroxysmal positional vertigo: clinical characteristics of dizzy patients referred to a Falls and Syncope Unit. Q J Med 2005;98:357–64. 10.1093/qjmed/hci057 [DOI] [PubMed] [Google Scholar]