Abstract
Background:
Capitellar osteochondritis dissecans (OCD) is commonly managed surgically in symptomatic adolesent throwers and gymnasts. Little is known about the impact that surgical technique has on return to sport.
Purpose:
To evaluate the clinical outcomes and return-to-sport rates after operative management of OCD lesions in adolescent athletes.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
The PubMed, CINAHL, EMBASE, SPORTDiscus (EBSCO), and Cochrane Central Register of Controlled Trials databases were queried for studies evaluating outcomes and return to sport after surgical management of OCD of the capitellum. Two independent reviewers conducted a systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Studies reporting patient outcomes with return-to-sport data and minimum 6-month follow-up were included in the review.
Results:
After review, 24 studies reporting outcomes in 492 patients (mean age ± SD, 14.3 ± 0.9 years) were analyzed. The overall return-to-sport rate was 86% at a mean 5.6 months. Return to the highest preoperative level of sport was most common after osteochondral autograft procedures (94%) compared with debridement and marrow stimulation procedures (71%) or OCD fixation surgery (64%). Elbow range of motion improved by 15.9° after surgery. The Timmerman-Andrews subjective and objective scores significantly improved after surgery. Complications were low (<5%), with 2 cases of donor site morbidity after osteoarticular autograft transfer (OAT) autograft harvest. The most common indications for reoperation were repeat debridement/loose body removal.
Conclusion:
A high rate of return to sport was observed after operative management of capitellar OCD. Patients were more likely to return to their highest level of preoperative sport after OAT autograft compared with debridement or fixation. Significant improvements in elbow range of motion and patient outcomes are seen with low complication rates after OCD surgery.
Keywords: osteochondritis dissecans, elbow, gymnast, thrower, OATs, return to sport
Osteochondritis dissecans (OCD) of the capitellum is a well-defined condition in adolescent athletes, most commonly seen in throwers and gymnasts. The radiocapitellar joint carries the majority of the force across the elbow during valgus loading, a motion that is repetitive in these sports and thought to underlie the pathologic process of OCD development.5 Microtrauma from compressive and shear forces sustained at the radiocapitellar joint during these activities may lead to microvascular injury in the capitellum, and eventually to OCD.
Patients with early and stable lesions who also have open capitellar physes occasionally heal spontaneously with nonoperative management.17 The healing potential of advanced lesions is poor with nonoperative treatment measures.17,27 When left untreated, the majority of cases result in elbow pain with daily activity at long-term follow-up.27 Operative management is typically offered for unstable lesions and those who ultimately fail nonoperative management; these lesions have been classically treated with debridement and/or marrow-stimulating procedures.16,25 Proposed alternatives to this mode of treatment have been fragment fixation6,7,23,31 or resection and replacement with osteoarticular autograft transfer (OAT).15,30,34
Previous series have demonstrated infrequent return to sport with nonoperative management17 or debridement and marrow-stimulation procedures.24,25 Perhaps in response to these reports, OAT procedures have gained popularity in recent literature.14,15,22 Current OAT surgical literature is limited to small, single-institution retrospective case series. Comparative studies evaluating differences in return-to-sport rates and outcomes as a function of type of operation are limited. The purpose of this study was to evaluate the clinical outcomes and return-to-sport rates after operative management of OCD lesions in adolescent athletes. We hypothesized that return to sport and clinical outcomes would be highest after OAT autograft procedures.
Methods
Search Strategy
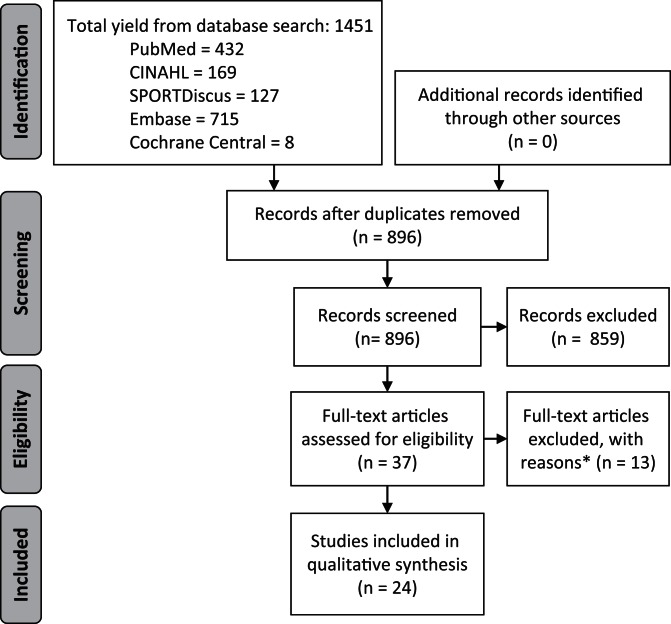
Search strategies were developed with the assistance of a health sciences librarian with expertise in systematic review processes. A review was then conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.20,21 Comprehensive search strategies including both index and keyword methods were devised for the following databases: PubMed, CINAHL (EBSCO), Embase (Elsevier), SPORTDiscus (EBSCO), and Cochrane Central Register of Controlled Trials (Wiley). No database filters were utilized in an effort to maximize sensitivity. Searches were conducted in September 2015, and results for each database can be found in the flow diagram (Figure 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart demonstrating the search strategy. After initial review, 37 full-length articles met the criteria for review. Reasons for exclusion at this stage (*) were failure to report return-to-sport data (n = 3), nonoperative management only (n = 2), failure to report outcomes as a function of procedure when multiple procedures were performed in a manuscript (n = 4), average age >20 years (n = 1), and irrelevant topic (n = 3).
Exclusion Criteria
A total of 1451 references were identified using the aforementioned search strategy. After removal of duplicate references and the addition of references identified through bibliographic review, a total of 896 potential records were identified for screening. References were included during the screening process if they were original articles that described surgical management of OCD lesions of the elbow. Articles were excluded for the following criteria: (1) abstracts, comments, editorials or letters only; (2) non–English language publications; (3) animal studies; (4) technique papers; (5) imaging or anatomic papers; (6) review articles; (7) articles with average age >20 years; (8) articles with <6-month follow-up; (9) articles failing to quantitatively report return to sport; (10) nonoperative management; and (11) mixed treatments with failure to stratify outcomes by operation type. Due to paucity of literature in this area, small case series were included in the screening process. After completion of the screening process, a total of 37 full-text articles were available for in-depth review.
Article Review
Two reviewers (B.K. and K.J.H.) independently evaluated the 37 articles that made it past the search and screening process, identifying articles that met inclusion criteria. In total, 24 studies met inclusion criteria. There was no disagreement between reviewers over included articles; however, a third reviewer (R.W.W.) was available if no consensus was reached on inclusion. Additionally, the bibliographies of each of the 24 selected articles were reviewed for potential articles not identified in the original search strategy, and further articles were found.
Data Assessment
Data from the selected 24 original articles were analyzed by identifying the following information: treatment modality, number of subjects, age of subjects, follow-up period, type of sport, complication, patient outcomes, and return to sport (see the Appendix). In several articles, multiple surgical treatment options were presented, and thus, treatments were subdivided and analyzed independently. The quality of included studies in the present work was assessed according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE)1 working group by 2 independent reviewers (K.J.H. and R.W.W.).
Data Analysis
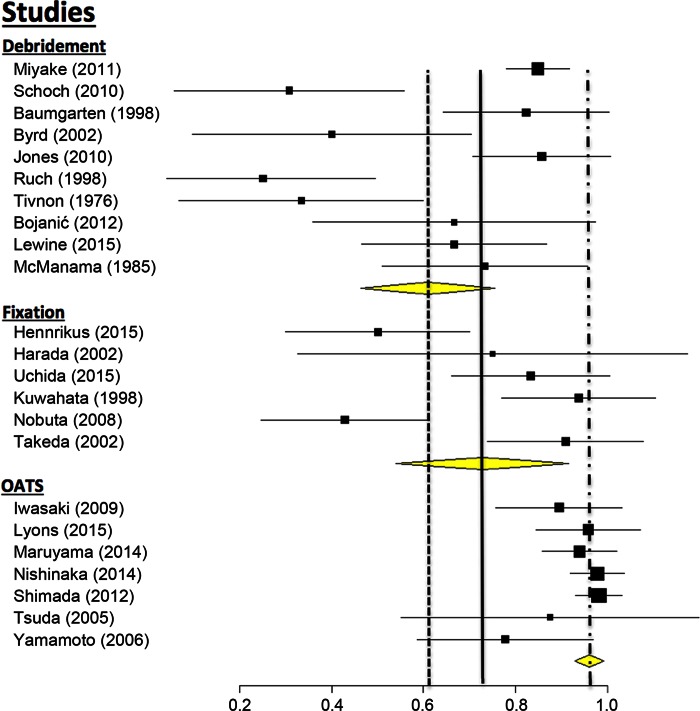
Descriptive statistics, including frequencies for categorical variables and mean ± SD for continuous variables, were conducted using Microsoft Excel (Microsoft Corp). The primary outcome, proportion of participants with return to high/previous level of sport, was calculated for each study and transformed using the Freeman-Tukey double arcsine method. A random-effects model, which accounts for heterogeneity of study design, patient groups, methods, and outcomes of included studies, was used to determine and compare weighted group averages for each operation type using the inverse-variance method. After these analyses, weighted group averages and 95% CIs were backtransformed.18 Analyses were conducted using R version 3.1.1 (“Metafor” Meta-Analysis Package for R; R Foundation for Statistical Computing).32 OpenMetaAnalyst (Brown University)33 was used to display return to sport with 95% CIs for each study. The overall random-effects pooled estimate for each operation type was also displayed (Figure 2).
Figure 2.
Forest plot analysis demonstrating differences in return to the previous level of sport across 3 techniques. The mean return to previous level of sport rate for osteoarticular allograft transfers (OATs) is 0.95 (95% CI, 0.89-0.99; far right dotted line) and was found to be significantly higher than that for debridement (0.62; 95% CI, 0.46-0.77; solid line) or fixation (0.72; 95% CI, 0.51-0.89; far left dotted line).
Results
We found 24 studies‡ that met inclusion criteria. Outcome data were available on 492 patients with a mean age of 14.3 ± 0.9 years. Primary sport type was reported for 94.3% (464/492) of patients; most commonly reported primary sport of participation was baseball (371/464) followed by gymnastics (35/464).
Return to Sport
Our study identified 492 athletes treated for OCD of the capitellum. At a mean follow-up of 39.8 ± 17.3 months, 424 patients (86%) were able to return to sport. Mean return to sport after surgery was 5.6 ± 2.1 months in the 11 studies that included this information.
Microfracture and Debridement
There were 10 studies2–4,9,13,16,19,24,25,29 that reported return-to-sport data after debridement and microfracture procedures. The mean age of patients in this group was 14.5 ± 1.0 years. The mean follow-up was 39.6 months. Of the 236 patients with OCD lesions treated with debridement and/or microfracture, 168 (71%) returned to their previous level of sport, and 205 (87%) were able to return to any level of sport. The mean time to return to sport was 4.2 ± 1.5 months after microfracture/debridement operations.
Fixation
We identified 6 studies6,7,12,23,28,31 that evaluated return-to-sport data after fixation of capitellar OCD lesions. Several methods of fixation were used, including hydroxyapatite pins, K-wires, and Herbert screws. The mean age of patients in this group was 14.2 ± 0.3 years. The mean follow-up was 40.4 months. Of the 92 patients with OCD lesions treated with fixation, 59 (64%) returned to their previous level of sport, and 63 (68%) were able to return to any level of sport. There were 4 studies6,12,23,28 that reported an average time of 5.9 ± 1.1 months from surgery to return to sport.
Osteochondral Autograft
There were 8 studies8,10,14,15,22,26,30,34 identified that reported return-to-sport data after osteochondral autograft for treatment of capitellar OCD. One study did not report return to previous level/highest level of sport.10 Both rib and knee autografts were included. The mean age of patients in this group was 14.1 ± 0.9 years. The mean follow-up was 35.0 months. Of the 164 patients with OCD lesions treated with OAT autograft, 124/132 (94%) returned to their previous level of sport, and 156 (95%) were able to return to any level of sport. There were 5 studies14,15,22,26,30 reporting an average time of 5.9 ± 0.9 months from surgery to return to sport.
Statistical Analysis
Of studies that met inclusion criteria, 23 of 24 provided data regarding return to previous level of sport (not simply return to any sport). The mean pooled proportion of return to previous level of sport for OAT was 0.95 (95% CI, 0.89-0.99). This was found to be higher than the mean proportion for debridement procedures (0.62; 95% CI, 0.46-0.77; P < .001) or fixation procedures (0.72; 95% CI, 0.51-0.89; P = .01) (Figure 2).
Range of Motion
Nineteen of 24 studies reported pre- and postoperative elbow range of motion. The mean preoperative elbow flexion was 127.14° ± 5.08°. The mean elbow extension was 11.56° ± 9.47° short of full extension (flexion arc, 115.58°). The mean postoperative elbow range of motion was 134.29° ± 3.93° of flexion and 2.76° ± 5.47° short of full extension (flexion arc, 131.53°). The mean improvement in elbow total range of motion was 15.95° ± 4.15°. There was no difference in final elbow range of motion between techniques.
Patient-Reported Outcomes
Pre- and postoperative Timmerman-Andrews (TA) scores were recorded in 9 of 24 studies.§ The mean TA scores preoperatively were 62.57 ± 6.65 for the subjective component and 77.0 ± 4.34 for the objective component. The mean TA scores postoperatively were 93.0 ± 4.44 for the subjective component and 89.33 ± 6.04 for the objective component. Two studies8,15 reported Lysholm knee scores after OAT autograft treatment; the mean reported Lysholm score was 99.7. Patient-reported outcomes did not differ between techniques.
Lesion Size
Only 8 studies7,8,16,23,25,26,30,31 reported a diameter for size of the OCD lesion undergoing treatment. Sizes of lesions were similar between the debridement group (13.35 mm), the fixation group (11.93 mm), and the OAT group (13.87 mm).
Complications
Assessment of donor site complications were reported in 58,10,14,26,34 of the OAT autograft studies. There were 2 reported cases of donor site morbidity: 1 case of donor site–related anterior knee pain8 and 1 pneumothorax from rib OAT harvesting.26 Revision surgery occurred in 22 of 492 patients. The majority of revision surgeries were for debridement/loose body removal (10/22) or implant removal (8/22). Loose body removal was most common after drilling or microfracture procedures occurring in 9 of 236 (3.81%) cases. Other reasons for revision surgery included conversion of fixation to OAT autograft,7 fragment revision fixation,7 and radial head resection for elbow stiffness.24 There was only 1 reported postoperative infection.14 There were 8 implant failures7,23 and 1 postoperative radial nerve palsy requiring exploration.7
Quality Appraisal
The quality of included studies as assessed according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE)1 working group was found to be low to very low (see the Appendix). Studies generally consisted of level 4 evidence, were retrospective in nature, and performed as single-institution case series. No studies were randomized or used control groups. Validated outcome measures were rarely used.
Discussion
Good outcomes can generally be expected after surgical management of capitellar OCD lesions in young athletes. Overall, about 86% of patients were able to return to any sport at around 6 months postoperatively. It appears that a greater percentage (95%) of athletes may be able to return to high-level athletics after OAT autograft compared with either fixation or debridement procedures. Surgical management leads to significant improvements in elbow range of motion and patient-reported outcomes. Complications after surgery are rare, and reoperation was required in less than 5% of patients. Overall, surgeons should expect high levels of return to sport and good clinical outcomes after surgical management of OCD lesions in the capitellum.
Not all cases of capitellar OCD require surgical management. Takahara et al27 evaluated the outcomes of 24 patients who underwent nonoperative management of capitellar OCD lesions. Nonoperative management was activity restriction for 6 months. At a mean follow-up of 5.2 years, they determined that only 17% of patients were pain free, and 54% had pain with everyday activities. Of 15 cases with follow-up radiographs, 3 cases had healed: all were early-stage OCD lesions. In the same study there were 5 early and stable lesions that failed to heal and were associated with worse outcomes. This suggests initial imaging demonstrating stable lesions should not be an absolute indication for nonoperative management. Rather, patients should be followed clinically, and those who fail to heal, continue to be symptomatic, or progress radiographically should be offered surgery.
OCD of the elbow is a disease of both articular cartilage and subchondral bone.11 Marrow stimulation and debridement was the mainstay of surgical management in prior decades and continues to have a role today. In fact, many medical insurance programs only cover debridement/microfracture treatments for elbow cartilage disorders such as OCD. The goals of this technique are to remove diseased tissue and blocks to motion and stimulate fibrocartilage in-growth at the capitellar defect. Diseased subchondral bone or cancellous bone loss are not addressed or restored by this technique. This is evidenced in the work by Baumgarten et al,2 who observed capitellar flattening on plain films in 50% of patients after abrasion arthroplasty. Return to high-level sports likely requires lateral column stability in addition to a treated cartilage defect. Marrow stimulation and debridement techniques may produce fibrocartilage over the prior defect without addressing the void of subchondral diseased bone required for lateral support. If the architecture of the capitellum is not restored, the elbow may suboptimally handle valgus loads during high-level competition. A procedure that addresses both the subchondral bone and the articular cartilage may more accurately restore architecture and provide a more favorable rate of return to high-level athletics.
Osteoarticular autograft transfer procedures14,15,22,26 have the ability to address friable cartilage and diseased subchondral bone while restoring architectural loss associated with OCD.11 Restoration of structural support to the lateral elbow while concurrently addressing unstable cartilage lesions is a possible explanation for higher rates of return to high-level sports (94%) associated with OAT. To restore the native architecture, however, OAT borrows tissue from other areas of the body, and morbidity from the donor site must be included in the overall assessment of this operation's efficacy. The 2 studies that performed outcome scores on knees after graft harvest in our study reported excellent outcomes, with Lysholm knee scores averaging over 99.5.8,15 The only 2 complications after harvest noted in the present study were chronic mild anterior knee pain with stair climbing8 and a pneumothorax from rib osteochondral harvest.26 This represents a donor site morbidity rate of 1.2% (2/164). Because of low donor site morbidity and the ability to restore capitellar architecture, some surgeons advocate OAT as a first consideration when operatively treating unstable OCDs in athletes with the goal of returning to sport. Unfortunately, despite a growing body of evidence of utility of OAT, many medical insurance carriers deem OAT to be investigational and will not cover this type of surgery in the elbow.
Unstable OCD lesions treated with fixation appeared to be least likely to return to sport in the present study. Only 64% of patients in the present study were able to return to their previous level of sport after fixation compared with 71% after debridement/stimulation and 94% after OAT autografting. This finding is biologically intuitive when one considers that the disease process affects both articular cartilage and subchondral bone11 and fragment fixation retains at least some of this diseased tissue. In contrast, debridement procedures and OAT autografting allow for the potential of complete excision of diseased tissue and joint restoration with fibrocartilage or hyaline cartilage, respectively.
The present study has some important limitations worth mentioning. On review of available evidence that met our inclusion and exclusion criteria, study quality as assessed by GRADE1 was determined to be low or very low. There were a few level 2 and 3 studies found on initial review that had to be excluded as the results were pooled and not stratified by operation type. No study had standardized treatment algorithms with a comparison of outcomes or randomization, leaving all reports open to surgeon selection bias. Validated patient-reported outcomes were not used. Additionally, a short requirement for follow-up (minimum, 6 months) was necessary to make the study of substantial size, and therefore, athletes who return to sport after 6 months may have been missed. This could potentially have caused an underestimation of the true return-to-sport rate. Finally, postoperative rehabilitation protocols may have potentially influenced return to sport and could not be analyzed given limited reporting in the available articles. Further studies with adequate follow-up, conducted in a prospective manner with either comparison groups or randomization, are warranted to detect differences in outcomes according to technique.
Conclusion
Overall, 86% of athletes treated surgically for OCD of the capitellum are able to return to some level of sport. Operative management of capitellar OCD lesions generally results in improvements in elbow range of motion and patient-reported outcomes, and complication rates are low. Significant differences in return to the previous or highest level of sport are seen depending on which operation is chosen, with OAT autograft outperforming debridement or fixation treatments.
Acknowledgment
The authors acknowledge Jennifer DeBerg, MLS, Librarian, Hardin Library for Health Sciences, University of Iowa, for assistance in database query and management during the systematic review process.
Appendix
Quality Appraisal of Studies Revieweda
| Lead Author (Year) | Journal | Level of Evidence | No. of Patients | Mean Follow-up (1 = yes, 0 = no) | Control Group (1 = yes, 0 = no) | Randomization (1 = yes, 0 = no) | Standardization (1 = yes, 0 = no) | Selection Bias (1 = yes, 0 = no) | Baseline Characteristics (Function) (1 = yes, 0 = no) | Follow up >12 mo (1 = yes, 0 = no) | Loss to Follow-up >15% | Primary Outcome Excellent/Good | Summary |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baumgarten2 (1998) | Am J Sports Med | 4 | 17 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | N/A (retrospective) | No formal outcome assessment used; 4 of 17 reported any pain | Low to very low |
| Bojanić3 (2012) | Croat Med J | 4 | 9 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | N/A (retrospective) | 9 | Low to very low |
| Byrd4 (2002) | Am J Sports Med | 4 | 10 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | N/A (retrospective) | 10 | Low to very low |
| Harada6 (2002) | J Shoulder Elbow Surg | 4 | 4 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | N/A (retrospective) | No formal outcome assessment used; no pain reported by any with activities of daily living | Low to very low |
| Hennrikus7 (2015) | J Pediatr Orthop | 4 | 24 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | N/A (retrospective) | 24.00 | Low to very low |
| Iwasaki8 (2009) | J Bone Joint Surg Am | 4 | 19 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 18 | Low to very low |
| Kosaka10 (2013) | J Pediatr Orthop | 4 | 32 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 29 | Low to very low |
| Kuwahata12 (1998) | Orthopaedics | 4 | 7 patients, 8 elbows | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | No formal outcome assessment used | Low to very low |
| Lewine13 (2015) | J Pediatr Orthop | 4 | 21 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | N/A (retrospective) | Average postop Timmerman-Andrews score = 184.3; breakdown by patient not given | Low to very low |
| Lyons14 (2015) | J Shoulder Elbow Surg | 4 | 11 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | N/A (retrospective) | Average overall DASH score = 1.4; breakdown by patient not given | Low to very low |
| Maruyama15 (2014) | Am J Sports Med | 4 | 33 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 29 | Low to very low |
| McManama16 (1985) | Am J Sports Med | 4 | 15 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | N/A (retrospective) | 13 | Low to very low |
| Mihara17 (2009) | J Shoulder Elbow Surg | 4 | 27 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | N/A (retrospective) | 11 | Low to very low |
| Miyake19 (2011) | J Hand Surg Am | 4 | 106 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | N/A (retrospective) | No formal outcome assessment used | Low to very low |
| Nishinaka22 (2014) | J Shoulder Elbow Surg | 4 | 22 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | Average postop Timmerman-Andrews score = 169; individual patient breakdown not given | Low to very low |
| Nobuta23 (2008) | Upsala J Med Sci | 4 | 28 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | N/A (retrospective) | 24 | Low to very low |
| Ruch24 (1998) | Arthroscopy | 4 | 12 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | N/A (retrospective) | Nonspecified questionnaire used at follow up; no good/excellent scales defined | Low to very low |
| Schoch25 (2010) | Arthroscopy | 4 | 13 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | N/A (retrospective) | Mean postop DASH score = 8.6 (range, 0-22.41); no breakdown of excellent/good results given | Low to very low |
| Shimada26 (2012) | J Bone Joint Surg Am | 4 | 26 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | N/A (retrospective) | 22 | Low to very low |
| Takeda28 (2002) | Am J Sports Med | 4 | 11 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | N/A (retrospective) | 10 | Low to very low |
| Tivnon29 (1976) | Am J Sports Med | 4 | 12 patients, 15 surgeries | 0 | 0 | 0 | 0 | 0 | 0 | 1 | N/A (retrospective) | 4 (based off of return to sport only) | Low to very low |
| Tsuda30 (2005) | Arthroscopy | 4 | 3 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 30/33 lost to follow-up | 3 | Low to very low |
| Uchida31 (2015) | Am J Sports Med | 4 | 18 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 17 | Low to very low |
| Yamamoto34 (2006) | Am J Sports Med | 4 | 18 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | Only mean Timmerman-Andrews scores given; individual breakdown not provided | Low to very low |
aDASH, Disabilities of the Arm, Shoulder and Hand; N/A, not applicable; postop, postoperative.
Footnotes
Declaration of Conflicting Interests: The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baumgarten TE, Andrews JR, Satterwhite YE. The arthroscopic classification and treatment of osteochondritis dissecans of the capitellum. Am J Sports Med. 1998;26:520–523. [DOI] [PubMed] [Google Scholar]
- 3. Bojanić I, Smoljanović T, Dokuzović S. Osteochondritis dissecans of the elbow: excellent mid-term follow-up results in teenage athletes treated by arthroscopic debridement and microfracture. Croat Med J. 2012;53:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Byrd JT, Jones KS. Arthroscopic surgery for isolated capitellar osteochondritis dissecans in adolescent baseball players: minimum three-year follow-up. Am J Sports Med. 2002;30:474–478. [DOI] [PubMed] [Google Scholar]
- 5. Cain EL, Dugas JR, Wolf RS, Andrews JR. Elbow Injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31:621–635. [DOI] [PubMed] [Google Scholar]
- 6. Harada M, Ogino T, Takahara M, Ishigaki D, Kashiwa H, Kanauchi Y. Fragment fixation with a bone graft and dynamic staples for osteochondritis dissecans of the humeral capitellum. J Shoulder Elbow Surg. 2002;11:368–372. [DOI] [PubMed] [Google Scholar]
- 7. Hennrikus WP, Miller PE, Micheli LJ, Waters PM, Bae DS. Internal fixation of unstable in situ osteochondritis dissecans lesions of the capitellum. J Pediatr Orthop. 2015;35:467–473. [DOI] [PubMed] [Google Scholar]
- 8. Iwasaki N, Kato H, Ishikawa J, Masuko T, Funakoshi T, Minami A. Autologous osteochondral mosaicplasty for osteochondritis dissecans of the elbow in teenage athletes. J Bone Joint Surg Am. 2009;91:2359–2366. [DOI] [PubMed] [Google Scholar]
- 9. Jones KJ, Wiesel BB, Sankar WN, Ganley TJ. Arthroscopic management of osteochondritis dissecans of the capitellum: mid-term results in adolescent athletes. J Pediatr Orthop. 2010;30:8–13. [DOI] [PubMed] [Google Scholar]
- 10. Kosaka M, Nakase J, Takahashi R, et al. Outcomes and failure factors in surgical treatment for osteochondritis dissecans of the capitellum. J Pediatr Orthop. 2013;33:719–724. [DOI] [PubMed] [Google Scholar]
- 11. Kusumi T, Ishibashi Y, Tsuda E, et al. Osteochondritis dissecans of the elbow: histopathological assessment of the articular cartilage and subchondral bone with emphasis on their damage and repair. Pathol Int. 2006;56:604–612. [DOI] [PubMed] [Google Scholar]
- 12. Kuwahata Y, Inoue G. Osteochondritis dissecans of the elbow managed by Herbert screw fixation. Orthopedics. 1998;21:449. [DOI] [PubMed] [Google Scholar]
- 13. Lewine EB, Miller PE, Micheli LJ, Waters PM, Bae DS. Early results of drilling and/or microfracture for grade IV osteochondritis dissecans of the capitellum [published online June 17, 2015]. J Pediatr Orthop. doi:10.1097/BPO.0000000000000575. [DOI] [PubMed] [Google Scholar]
- 14. Lyons ML, Werner BC, Gluck JS, et al. Osteochondral autograft plug transfer for treatment of osteochondritis dissecans of the capitellum in adolescent athletes. J Shoulder Elbow Surg. 2015;24:1098–1105. [DOI] [PubMed] [Google Scholar]
- 15. Maruyama M, Takahara M, Harada M, Satake H, Takagi M. Outcomes of an open autologous osteochondral plug graft for capitellar osteochondritis dissecans: time to return to sports. Am J Sports Med. 2014;42:2122–2127. [DOI] [PubMed] [Google Scholar]
- 16. McManama GB, Jr, Micheli LJ, Berry MV, Sohn RS. The surgical treatment of osteochondritis of the capitellum. Am J Sports Med. 1985;13:11–21. [DOI] [PubMed] [Google Scholar]
- 17. Mihara K, Tsutsui H, Nishinaka N, Yamaguchi K. Nonoperative treatment for osteochondritis dissecans of the capitellum. Am J Sports Med. 2009;37:298–304. [DOI] [PubMed] [Google Scholar]
- 18. Miller JJ. The inverse of the Freeman-Tukey double arcsine transformation. Am Statistician. 1978;32:138. [Google Scholar]
- 19. Miyake J, Masatomi T. Arthroscopic debridement of the humeral capitellum for osteochondritis dissecans: radiographic and clinical outcomes. J Hand Surg Am. 2011;36:1333–1338. [DOI] [PubMed] [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J, Altman D, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statements. BMJ. 2009;339:5. [PMC free article] [PubMed] [Google Scholar]
- 21. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nishinaka N, Tsutsui H, Yamaguchi K, Uehara T, Nagai S, Atsumi T. Costal osteochondral autograft for reconstruction of advanced-stage osteochondritis dissecans of the capitellum. J Shoulder Elbow Surg. 2014;23:1888–1897. [DOI] [PubMed] [Google Scholar]
- 23. Nobuta S, Ogawa K, Sato K, Nakagawa T, Hatori M, Itoi E. Clinical outcome of fragment fixation for osteochondritis dissecans of the elbow. Ups J Med Sci. 2008;113:201–208. [DOI] [PubMed] [Google Scholar]
- 24. Ruch DS. The arthroscopic management of osteochondritis dissecans of the adolescent elbow. Arthroscopy. 1998;14:797–803. [DOI] [PubMed] [Google Scholar]
- 25. Schoch B, Wolf BR. Osteochondritis dissecans of the capitellum: minimum 1-year follow-up after arthroscopic debridement. Arthroscopy. 2010;26:1469–1473. [DOI] [PubMed] [Google Scholar]
- 26. Shimada K, Tanaka H, Matsumoto T, et al. Cylindrical costal osteochondral autograft for reconstruction of large defects of the capitellum due to osteochondritis dissecans. J Bone Joint Surg Am. 2012;94:992–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Takahara M, Ogino T, Fukushima S, Tsuchida H, Kaneda K. Nonoperative treatment of osteochondritis dissecans of the humeral capitellum. Am J Sports Med. 1999;27:728–732. [DOI] [PubMed] [Google Scholar]
- 28. Takeda H, Watarai K, Matsushita T, Saito T, Terashima Y. A surgical treatment for unstable osteochondritis dissecans lesions of the humeral capitellum in adolescent baseball players. Am J Sports Med. 2002;30:713–717. [DOI] [PubMed] [Google Scholar]
- 29. Tivnon MC, Anzel SH, Waugh TR. Surgical management of osteochondritis dissecans of the capitellum. Am J Sports Med. 1976;4:121–128. [DOI] [PubMed] [Google Scholar]
- 30. Tsuda E, Ishibashi Y, Sato H, Yamamoto Y, Toh S. Osteochondral autograft transplantation for osteochondritis dissecans of the capitellum in nonthrowing athletes. Arthroscopy. 2005;21:1270. [DOI] [PubMed] [Google Scholar]
- 31. Uchida S, Utsunomiya H, Taketa T, et al. Arthroscopic fragment fixation using hydroxyapatite/poly-l-lactate acid thread pins for treating elbow osteochondritis dissecans. Am J Sports Med. 2015;43:1057–1065. [DOI] [PubMed] [Google Scholar]
- 32. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1–48. [Google Scholar]
- 33. Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw. 2012;49(5):1–15. [Google Scholar]
- 34. Yamamoto Y, Ishibashi Y, Tsuda E, Sato H, Toh S. Osteochondral autograft transplantation for osteochondritis dissecans of the elbow in juvenile baseball players: minimum 2-year follow-up. Am J Sports Med. 2006;34:714–720. [DOI] [PubMed] [Google Scholar]