Abstract
Objective To develop and prospectively evaluate a web-based tool that forecasts the daily bed need for admissions from the cardiac catheterization laboratory using routinely available clinical data within electronic medical records (EMRs).
Methods The forecast model was derived using a 13-month retrospective cohort of 6384 catheterization patients. Predictor variables such as demographics, scheduled procedures, and clinical indicators mined from free-text notes were input to a multivariable logistic regression model that predicted the probability of inpatient admission. The model was embedded into a web-based application connected to the local EMR system and used to support bed management decisions. After implementation, the tool was prospectively evaluated for accuracy on a 13-month test cohort of 7029 catheterization patients.
Results The forecast model predicted admission with an area under the receiver operating characteristic curve of 0.722. Daily aggregate forecasts were accurate to within one bed for 70.3% of days and within three beds for 97.5% of days during the prospective evaluation period. The web-based application housing the forecast model was used by cardiology providers in practice to estimate daily admissions from the catheterization laboratory.
Discussion The forecast model identified older age, male gender, invasive procedures, coronary artery bypass grafts, and a history of congestive heart failure as qualities indicating a patient was at increased risk for admission. Diagnostic procedures and less acute clinical indicators decreased patients’ risk of admission. Despite the site-specific limitations of the model, these findings were supported by the literature.
Conclusion Data-driven predictive analytics may be used to accurately forecast daily demand for inpatient beds for cardiac catheterization patients. Connecting these analytics to EMR data sources has the potential to provide advanced operational decision support.
Keywords: cardiac catheterization, hospital, forecasting, patient admission, cardiac care unit
BACKGROUND AND SIGNIFICANCE
The number of cardiac catheterizations performed in the United States has risen sharply over the last 30 years. Catheterization laboratory infrastructure has increased, and, in 2007, an estimated 85% of all United States hospitals provided cardiac catheterization services.1 Although the volume of catheterization laboratories has decreased in recent years, the variety of catheterization procedures has expanded to include both diagnostic and therapeutic procedures.1,2 A diverse mix of procedure types and increasingly complex patients make it difficult to predict patients’ post-procedure care needs. For example, low-risk diagnostic procedures may reveal adverse conditions or trigger an immediate therapeutic intervention that necessitates extended recovery (ie, an inpatient overnight stay).3,4 Thus, prior to catheterization, it is often unknown whether a patient’s post-procedure condition will require an inpatient overnight stay.5,6
Uncertainty regarding hospital admissions from catheterization laboratories challenges efficient inpatient bed management.6 Cardiology hospital units contain specialized monitoring equipment (eg, telemetry beds) designed for recovering catheterization patients, in addition to cardiac patients admitted from the emergency department (ED) and external locations (ie, direct admissions). To proficiently manage patient flow, providers must project the number of admissions from each of these sources daily. ED patients are unscheduled, but the patterns of daily ED admissions are predictable (ie, there is low day-to-day variation).6–8 Direct admissions typically follow similar patterns. The catheterization laboratory is a large source of cardiac inpatient admissions, and, because of the high uncertainty of admission numbers from the catheterization laboratory, daily admission projections often focus on this source.6
In many hospitals, providers predict the demand for beds (ie, the number of admissions) for any given day after reviewing the catheterization schedule the evening before or the morning of the same day. These predictions are based on provider experience and intuition.9 Overestimating admissions from the catheterization laboratory places unnecessary holds on beds that may be used to admit patients from competing admission sources.10 This can lead to bottlenecks in patient flow from the ED, which result in long waits to gain inpatient access (ie, ED boarding time). A study of ED boarding for cardiac patients demonstrated that daily catheterization volume was the strongest driver of ED boarding time, regardless of patients’ clinical conditions.6,11 Boarding may be unsafe – boarding time for cardiac patients has been associated with poor adherence to American College of Cardiology therapy guidelines and a higher risk of recurrent myocardial infarction.12 Underestimating catheterization admissions has negative consequences as well. Cardiology bed shortages force catheterization patients to recover in sub-optimal care areas (eg, held within the catheterization laboratory, off-service inpatient beds, or post-anesthesia care units) or can lead to a cancellation of the catheterization procedure.13–15 Catheterization admission prediction is a critical component of hospital bed management that could be supported by informatics-based solutions.
Patient flow is a crude indicator of hospital service quality, access, and cost.16,17 As a result, the US Institute of Medicine, the National Academy of Engineering, and the President’s Council of Advisors on Science and Technology recommend that engineers and informaticists apply their skills to the task of improving patient flow.17,18 Although general patient flow modeling applications are expansive, there are a limited number of studies that target the prediction of hospital admissions. Many of these studies were conducted retrospectively, with little demonstration of the real-time forecasting capability required for decision support.
HOSPITAL OPERATIONAL FORECAST MODELS
The most relevant studies we identified developed models to predict unplanned hospital admissions for outpatient surgeries. Their objective was to determine individual patient factors (ie, predictors) associated with unplanned admissions.19–23 However, these studies were not intended to support bed management. Applicable models must be operable in real-time and aggregate individual predictions (ie, probabilities) to forecast the total amount of beds that a hospital needs over time. We found a few examples of such models in our literature search, including studies forecasting admissions from the ED, based on information available at initial patient triage.24–26 These models were developed from naïve Bayes, linear, and logistic regression analyses. One study of pediatric intensive care units forecasted patients’ future length of stay by deploying a discrete-time logistic regression (ie, survival) model. Individual patient probabilities of discharge were continuously updated and aggregated to forecast bed availability over time.9 Another study created separate logistic regression-based admission (inflow) and discharge (outflow) predictions for individual patients in a small community hospital. Probabilities were summed over time to produce running forecasts of hospital occupancy.27 Although these models were developed for real-time bed management, none of them demonstrated evidence of integration into information technology-based decision support or were prospectively validated.
OBJECTIVE
The objective of this study was to develop and prospectively validate a decision support application to predict cardiology admissions for adults from a catheterization laboratory. The automated tool forecasts daily cardiology bed needs from routinely available clinical data extracted from the catheterization scheduling system. Predictor information such as demographics, scheduled procedures, and clinical indicators mined from free-text notes were input to a multivariable logistic regression model. The regression model predicts the probability of inpatient admission prior to the procedure, and probabilities are aggregated to predict daily bed needs. The forecast model is embedded within a web-based application that is available for providers to interact with and review the information it contains to support bed management decisions.
MATERIALS AND METHODS
Setting, Design, and Measurements
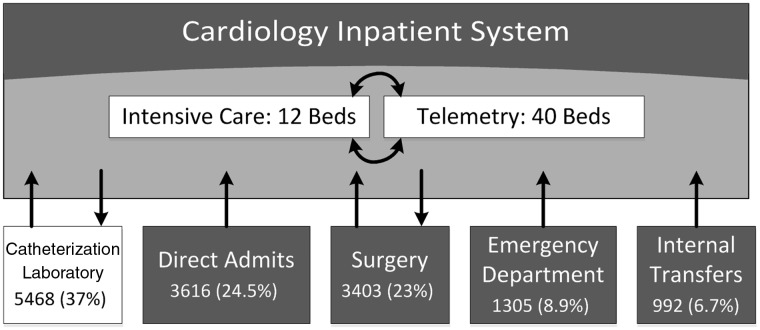
The study was performed at an urban 1059-bed tertiary care hospital. A diagram depicting patient flow to the cardiology department (inpatient admissions) may be seen in Figure 1. The cardiology department manages 52 inpatient beds at this hospital, which are fully equipped with telemetry and bedside monitoring devices. Twelve of these beds are designated to treat intensive care patients. The adjacent catheterization laboratory contains nine procedural rooms, a 12-bed preparatory area, and a separate 12-bed recovery area. Catheterization patients account for the highest proportion (37%) of the total admissions to the cardiology department’s beds. The admission forecast model was derived using a cohort of 6384 catheterization patients over a 13-month period between June 1, 2012 and July 1, 2013 (ie, the training set). Prior to the implementation of the tool, the cardiology staff assessed each day’s catheterization schedule (at 17:00), surveying patient procedures, basic demographics, and source locations (eg, arriving from home vs already an inpatient). Then, based on this information, nurse providers would huddle and use their experience and intuition to estimate the number of open beds needed the next day to accommodate new patient admissions as well as who those admitted patients may be. Recognizing opportunities for error and known variability in daily estimates across providers, the nursing leadership of the hospital requested that the forecast application be developed to support more consistent and accurate predictions. The web application was developed, went live, and the model was evaluated on an out-of-sample cohort of 7029 patients over the next 13-months, between July 2013 and August 2014 (ie, the test set). Although the forecast model underwent a 10-fold cross-validation prior to implementation, the model used in current practice (reported in the Results section of this article) was developed from the entire training cohort. All forecast evaluation measures were applied to the out-of-sample (ie, prospective) test cohort. However, the forecast tool has evolved somewhat since its implementation, in response to additional clinician feedback, improved data cleaning procedures, and changes in information technology infrastructure, which temporarily disrupted data connections. The final model reported herein represents the most recent and clean version of the model and its results during the evaluation period.
Figure 1:
Cardiology inpatient admission sources for the entire 26-month study period.
The predicted outcome was inpatient admission. This includes admission to any level of care (ie, floor or intensive care unit) in the cardiology department. A small portion of patients were admitted to off-service units, when the cardiology department was full or for specific clinical conditions. These patients were also considered to have the outcome of inpatient admission. Predictor variables included patients’ age, gender, admission source, procedure, and clinical indicators hypothesized to influence admission. These variables were selected by a focus group of cardiology providers (ie, nurses and physicians) and were readily available in the catheterization information system. The clinical indicators were mined from free-text notes available in the patients’ records prior to their catheterization. A simple, rule-based natural language processing algorithm was developed to map keyword(s) and exclusions, as seen in Table 1. The semantic map was derived through an iterative process of searching for inclusion and exclusion strings, in cooperation with our cardiology provider focus group. Clinical indicators were mapped as either present or absent. When exclusion keywords (Table 1) were detected (ie, negation data) the indicator was labeled “absent” for that patient. Clinical indicators were not mutually exclusive; multiple indicators were mapped to individual patients. There were no missing predictor data within the training and test cohorts. However, 1.3% of cases did not have an admission or discharge outcome. Listwise deletion was used to omit these data from the training and test datasets.
Table 1:
Clinical Indicators Mined from Cardiologist Free-Text Notes
| Clinical indicators | Keyword(s) | Exclusion criteria |
|---|---|---|
| Abnormal stress test |
|
|
| Angina |
|
|
| Coronary artery bypass graft |
|
|
| Coronary artery disease |
|
|
| Cardiomyopathy |
|
“-cmp” |
| Chest pain |
|
|
| Congestive heart failure |
|
|
| Diabetes |
|
|
| Elevated calcium score |
|
"negative calcium score" and "neg calcium score" |
| Hyperlipidemia |
|
|
| Hypertension |
|
|
| Obese |
|
|
| Percutaneous coronary intervention |
|
|
| Positive cardiac enzymes |
|
|
| Previous myocardial infarction |
|
Forecast Algorithm
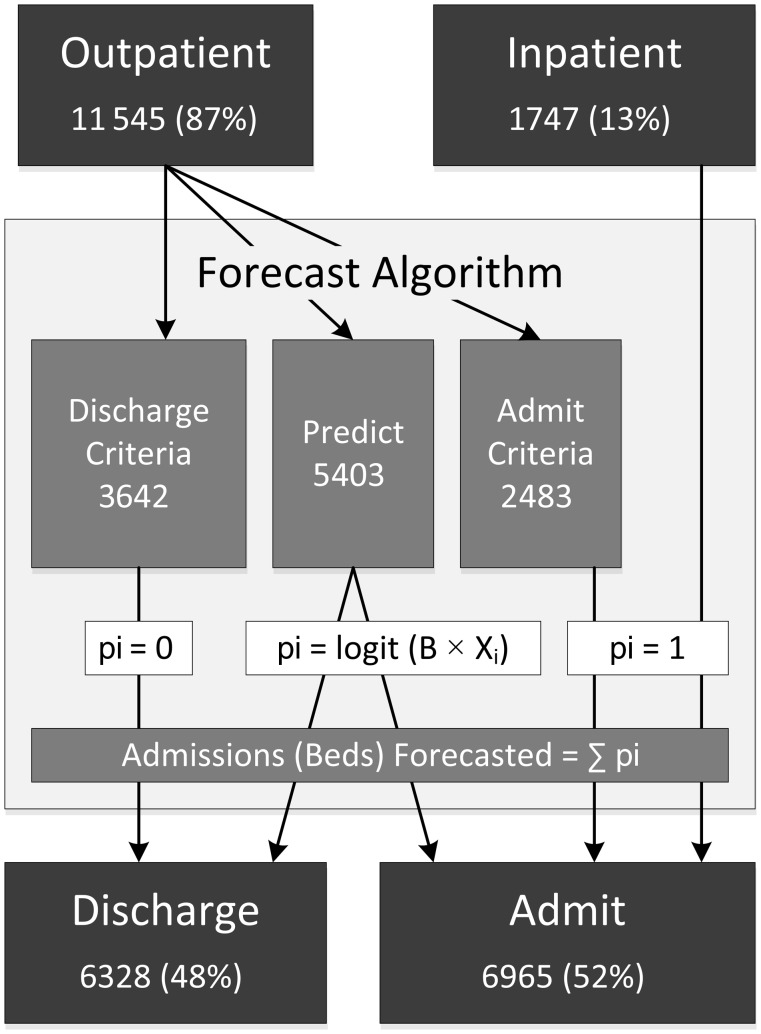
The forecast algorithm combines individual predictions from a multivariable logistic regression model with a set of rules that identify patients meeting criteria for admission or discharge. Figure 2 diagrams the algorithm, in which individual patients’ probability of admission (pi) are summed to predict the total number of daily admissions (beds required). Most catheterization patients originate as outpatients (86.9%); they arrive at the hospital the same day as their procedure. The remaining patients were admitted (ie, became inpatients) before their procedure and destined to return to their same inpatient bed. These patients are identified by our web application as current inpatients prior to catheterization and are assigned a bed (pi = 1), as seen in Figure 2. In addition, specific outpatients that undergo catheterization procedures that meet definitive criteria for inpatient admission (14 procedures) or discharge (13 procedures) are also assigned to those categories. If a patient undergoes any of the procedures that meet admission criteria, the patient is predicted to need a bed (pi = 1). Alternatively, a patient is predicted to be discharged (pi = 0) only if their procedure meets discharge criteria and they did not undergo a concurrent procedure.
Figure 2:
Catheterization forecast algorithm flow diagram for the entire 26-month cohort. “Outpatient” and “inpatient” designations describe the catheterization laboratory admission sources. “Discharge” and “admit” designations describe the binary outcome predicted.
The predicted probability of hospital admission was generated for 46.8% of outpatient catheterization patients by multivariable logistic regression. Patients meeting automatic admission or discharge criteria (Figure 2) were excluded from this model derivation cohort. Predictor information included patients’ age, gender, scheduled procedure(s), and clinical indicators. It is important to note that procedural variables were structured such that an individual patient may have one or many scheduled procedures during their catheterization.
A purposeful variable selection method described by Hosmer and Lemeshow was used to create our final model.28–30 This method included univariate analyses to select predictors with a significant (Wald Test P < 0.25) relationship to the admission outcome. Significant predictors from univariate analyses comprised the initial multivariable model. Variables that were non-significant in the multivariable model (P < 0.1) were systematically dropped to examine confounding. If the dropped variable changed other predictor coefficients by >25% (signifying confounding), the variable was retained. Once this iterative process was complete, the variables originally filtered in univariate analyses were re-introduced to the multivariable model and were retained if they were significant or confounding. This process was conducted to achieve the most parsimonious and stable model to deploy in the web application. The discriminatory power of the final model was measured by the area under the receiver operator curve for our test cohort.
Daily forecasts of inpatient bed needs were produced by summing individual patient admission probabilities (Figure 2) for catheterization patients each day. One bed was added to this forecast each day as a safety adjustment, to avoid underestimation, which is perceived to be a more costly type of inaccuracy. Lastly, observed numbers of filled inpatient beds used were compared to the bed needs forecasted (residual analyses) for our prospective test cohort. All forecast algorithm construction, logistic regression modeling, and evaluation was performed using the MATLAB technical computing environment (Mathworks, Natick, MA).
Web Application
The forecast algorithm was integrated into clinical practice via a web-based decision support tool. The application uses Microsoft Structured Query Language (SQL) Server 2012 to compute and store admission forecasts that are updated with a daily job configured in SQL Server Agent. Each day at 16:45, the SQL server receives an extract of the scheduled catheterization procedures for the following day from the catheterization information system. At 17:00, a job executes to process the data extract and store predictors within the application database. This includes an SQL-stored procedure that processes free-text notes to map clinical indicators to patients. The probability of admission is then computed for each patient (Figure 2), summed, rounded to the nearest integer, and adjusted up by 1 to report the total number of admissions forecasted, which translates to the amount of patient beds needed. The application design choice to render predictions at 17:00 the day prior was done based on feedback from nurses, in accordance with their workflow and daily planning huddle. This is when scheduling information was most valuable – when there was enough lead time to take action. However, it was possible that patients were added to the following day’s catheterization schedule after 17:00 the previous day. These additional patients were accounted for in our training set, but were unknown to the forecast application at the time predictions were rendered. However, we were able to capture this entire test cohort retrospectively; the forecast model and prediction results for the entire test cohort are reported. The web application was constructed with Microsoft ASP.NET, Microsoft Entity Framework, and jQuery, to display daily forecasts, patients’ admission probabilities, and their corresponding predictor variable data. This information is also communicated to cardiology providers in a daily email that includes the web application link and is triggered by the SQL Server Agent job after all the previous steps are complete.
RESULTS
Forecast Algorithm
A total of 13 292 adult patients received catheterization procedures at the hospital over the 26-month study period. 6965 (52.4%) of these patients were admitted post-catheterization procedure, and 6328 (47.6%) were discharged to home after their catheterization procedure. Prior to their procedure, 86.9% of these patients arrived at the catheterization laboratory from external locations (ie, as outpatients) and the remaining originated from in-hospital (ie, as inpatients), as diagrammed in Figure 2. For outpatients eligible for admission prediction, logistic regression predicted 46.8% would be admitted, and the remaining outpatients met criteria for either projected admission (21.5%) or discharge (31.7%).
The results of the logistic regression model are displayed in Table 2. Advancing age and male gender were associated with an increased probability of admission. The purposeful selection process yielded nine catheterization procedures and eight clinical indicators that were predictive of admission. Procedures were classified in reference to the most common procedure, “left heart catheterization, possible percutaneous coronary intervention,” performed on 54% of the patients in the total cohort. Compared to this reference procedure, different procedures demonstrated a large range of effects on the likelihood of patient admission. Less invasive procedures associated with low rates of patient admission (odds ratios < 0.1) included electrophysiology studies, catheter ablation, patent foramen ovule closures, and heart catheterizations without possible follow-up percutaneous coronary interventions (Table 2). Clinical indicators of congestive heart failure, positive cardiac enzymes, and coronary artery bypass grafts increased patients’ likelihood of admission. Less severe indicators, such as hypertension, hyperlipidemia, angina, and smoking, decreased patients’ risk for admission.
Table 2:
Catheterization Inpatient Forecast Model for Predicted Outpatient Admissions
| Variable | N (%) | Odds ratio (95% CI) | P-value |
|---|---|---|---|
| Age (reference: <35 years) | 246 (5) | -- | -- |
| 35–50 | 567 (10) | 2.18 (1.34–3.55) | 0.0026 |
| 50–59 | 1141 (21) | 2.11 (1.33–3.34) | 0.001 |
| 60–69 | 1698 (31) | 2.24 (1.43–3.51) | <0.001 |
| 70–79 | 1098 (20) | 2.51 (1.57–4.01) | 0.001 |
| ≥80 | 653 (12) | 4.64 (2.8–7.69) | <0.001 |
| Gender (reference: Female) | 1950 (36) | -- | -- |
| Male | 3453 (64) | 1.27 (1.06–1.52) | 0.01 |
| Procedures (reference: Left heart cath, possible PCI) | 2919 (54) | -- | -- |
| Left heart catheterization | 542 (10) | 0.25 (0.18–0.34) | <0.001 |
| Electrophysiology ablation, ventricular tachycardia | 253 (5) | 0.55 (0.36–0.84) | 0.006 |
| Right and left heart catheterization | 249 (5) | 0.32 (0.2–0.49) | <0.001 |
| Electrophysiology ablation, atrial flutter | 219 (4) | 0.2 (0.14–0.3) | <0.001 |
| Right and left heart catheterization, possible percutaneous cardiac intervention | 129 (2) | 0.47 (0.25–0.87) | 0.0178 |
| Electrophysiology study (with additional procedure) | 54 (1) | 0.21 (0.09–0.5) | <0.001 |
| Patent foramen ovale closure | 45 (1) | 0.14 (0.04–0.5) | 0.002 |
| Electrophysiology study (without additional procedure) | 39 (1) | 0.26 (0.1–0.72) | 0.01 |
| Electrophysiology ablation, atrial tachycardia | 33 (1) | 0.35 (0.11–1.07) | 0.064 |
| Other procedure | 921 (17) | 1.01 (0.77–1.32) | 0.951 |
| Clinical indicators (reference: None) | -- | -- | -- |
| Hypertension | 1961 (43) | 0.43 (0.34–0.56) | <0.001 |
| Hyperlipidemia | 1749 (38) | 0.59 (0.46–0.76) | <0.001 |
| Angina | 1000 (22) | 0.7 (0.55–0.9) | 0.017 |
| Coronary artery bypass graft | 443 (10) | 1.95 (1.42–2.67) | <0.001 |
| Cardiomyopathy | 402 (9) | 0.65 (0.47–0.91) | 0.036 |
| Smoker | 390 (8) | 0.45 (0.32–0.65) | <0.001 |
| Congestive heart failure | 277 (6) | 1.9 (1.22–2.95) | 0.001 |
| Positive cardiac enzymes | 37 (1) | 4.95 (1.01–24.33) | 0.049 |
Cath, catheterization; CI, confidence interval; PCI, percutaneous coronary intervention.
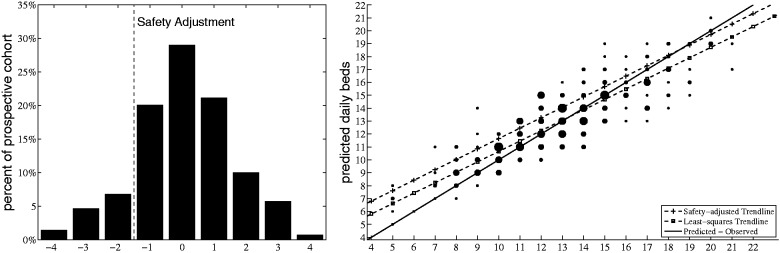
Performance Evaluation
Predictions generated from the forecast model derived from our training set were evaluated prospectively (ie, the test set). The area under the receiver operating characteristic curve was 0.722 for patients eligible for admission prediction. These regression-based patient probability estimates were mixed with rule-based estimates (Figure 2) to forecast total catheterization patient admissions. For our prospective cohort, there was an average of 24.8 (standard deviation [STD] 6.4) patients undergoing a procedure each weekday. An average of 12.8 (STD 3.6) of these patients were admitted each day. During the prospective evaluation, the number of forecasted admissions (ie, the predicted amount of beds needed) were compared to observed admissions (ie, the amount of beds used). The results of the residual analyses are displayed in Figure 3. The forecasted number admissions was correct were within one bed on 70.3% of the days evaluated and within three beds on 97.5% of the days evaluated (Figure 3, Left). Applying the one-bed safety adjustment to avoid underestimation resulted in 87.1% of forecasts being equal to or greater than the number of daily admissions observed. A scatter plot (Figure 3, Right) demonstrates the algorithm’s stability and predictive accuracy in relation to the volume of catheterization patients admitted to the hospital. The least squares trend line demonstrates how forecasts revert to the mean, ranging from over-predictive (forecasts > observed), when the number of observed admissions was relatively low (<11), to under-predictive, when the number of observed admissions was relatively high (>16). Evaluating this same least squares trend for the safety adjustment demonstrated that the observed demand for beds must exceed 21 admissions (which only occurred on 1 day during the study period; 0.36%) for the adjusted prediction to be likely to under-predict the amount of beds needed.
Figure 3:
Residual analyses – Left panel: Percentage of each daily residual (predicted beds needed - number of beds used) in prospective cohort. Right panel: forecasted admissions (beds predicted) vs observed admissions (number of beds used) in prospective cohort.
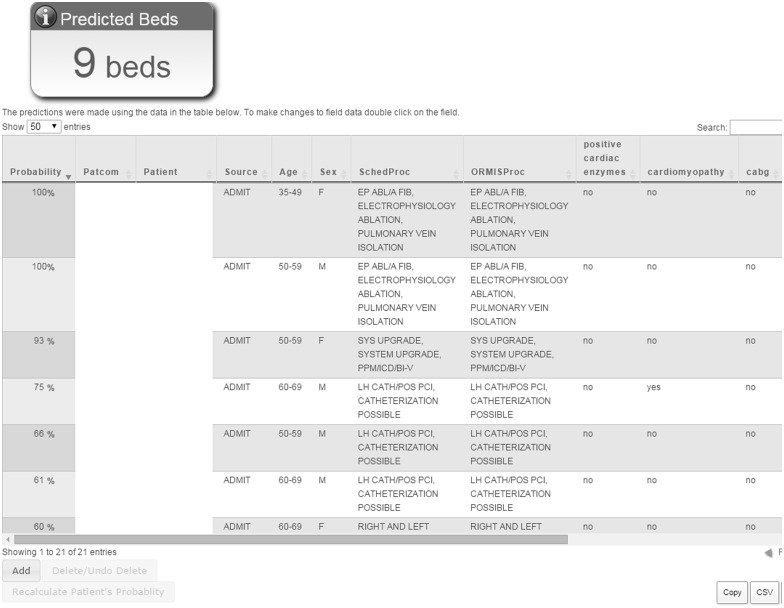
Web Application
The web application was used over the course of the prospective evaluation period. The user interface, with the safety-adjusted forecast, is displayed in Figure 4. The web application is interactive; end-users may edit any predictor variable values or add/remove patients from the daily list via the interface, to account for discrepancies. Any editing immediately triggers the application to recalculate admission probabilities and update the total forecasted number of beds needed. User interaction was frequent during the pilot (training) period and was valuable for allowing developers to recognize misclassified patients and identify rule-based procedures. However, after this period of refinement was complete, user interaction no longer occurred, even though the interactive features of the application remained. Every day, current users receive emails of the number of forecasted admissions (the number of beds needed), generated by the application, and view the web interface when more in-depth information on specific patients is of interest to them.
Figure 4:
Catheterization laboratory inpatient forecast tool web interface.
DISCUSSION
This study demonstrates the development and prospective evaluation of a web-based cardiac catheterization laboratory inpatient forecast tool. The tool is designed to predict daily admissions to facilitate more proactive management of patient flow. Improving patient flow in acute care hospitals has generally been recognized as a high-priority area that can contribute toward more efficient and accessible healthcare in the United States.16 The expansion of electronic medical records (EMRs) has led to an increased capability to track patients and create bed board displays, which are used in most hospitals.31 These systems have simultaneously produced the data required for large-scale patient flow modeling and analytics.5,9,19–25,32 Despite the spread of EMRs and advances in analytics, evidence of integration of the two is lacking. Demonstrations of patient flow analytics, especially predictive analytics, that interoperate with EMRs to provide real-time decision support are sparse. This study is novel, in that it addresses this gap by exhibiting the development and prospective evaluation of a patient flow forecast model actively being used in clinical practice.
Several retrospective studies that modeled predictors of unplanned inpatient admissions from outpatient services were consistent with our results,19–23,32 although our objective of providing decision support was different from these studies’ objectives. None of these other studies focused on catheterization laboratories; however, some studies did describe characteristics of cardiac catheterization patients and utilization patterns that were relevant to the present work.4,5,33 Despite fundamental differences between our research and related research, there were some consistent findings between the two. For example, it has previously been noted that aging (elderly) and male patients are at an increased risk of unplanned hospital admission after a catheterization procedure.5,33 Counterintuitive results related to smoking (a clinical indicator) decreasing the risk of catheterization patients’ hospital admission (Table 2) have also been reported previously.19–23 It has been theorized that smoking’s suppression of nausea and vomiting – a common cause of post-catheterization inpatient admission – puts smokers at a decreased risk for admission.19,20,22,23 This pattern also applied to all clinical indicators that may be categorized as less acute (eg, hypertension, hyperlipidemia, and angina).
Our model is likely to predict inpatient bed demand within one bed, unless the magnitude of that demand is extremely high or low. With the safety adjustment, under-predictions that fall short by more than one bed are virtually eliminated. At the same time, the safety adjustment significantly increases over-predictions exceeding one bed. Hence, in settings in which catheterization cancellations and boarding are less desirable than cardiac ED patient boarding, the safety adjustment may be appropriate. In contrast, if catheterization patients can safely be boarded post-procedure while they wait for a cardiac inpatient bed, it may be preferable to omit the safety adjustment from the model. At our institution, it was more important to avoid catheterization cancellations and boarding, so the safety adjustment was applied in the model.
Limitations
This study must be evaluated in the context of several limitations. First, the study was conducted at a single site for a specific patient population. Although the objective and the modeling strategy may be generalized, the forecast model’s results and accuracy may be highly dependent upon the patient population and the mechanisms used for data entry and collection. Similarly, the forecast algorithm operates quickly, on EMR data, some of which is keyed in manually (eg, clinical indicators). These data are subject to errors and variation in entry. For example, some patients may have hyperlipidemia, but that information may have either not been entered into or mislabeled in the catheterization scheduling system. The election of clinical indicators and the iterative development of data extraction processes (eg, natural language processing) was designed to minimize the potential for these errors. Further, the predictive component of the forecast model was performed using logistic regression. Although not explicitly a limitation, other machine learning-type algorithms may have produced marginally improved forecasts, and were initially considered for this study. However, logistic regression methods result in simple calculations that were easily executed within SQL-stored procedures. This was advantageous because the centralized hospital information technology infrastructure did not support the use of the additional software required to implement more advanced machine learning algorithms. In addition, the interactive capability of users to edit individual patients’ data ensured that corrections can be made on the fly. Despite this capability, the development of the application was focused on creating a passive application such that no additional data entry (ie, work) would be required by clinician users in order to use it. Lastly, another limitation of this study is that only the forecast tool’s accuracy was evaluated prospectively. In the future, we plan to evaluate the forecast tool’s operational impact on bed management decision-making and patient flow.
CONCLUSION
This study describes the development and prospective evaluation of a forecast tool that predicts hospital admissions from the catheterization laboratory. The web-based tool is interoperable with local EMRs and is used to support daily patient flow decisions in practice. This study represents the integration of predictive analytics into a local EMR system that aims to improve the management of healthcare resources (inpatient beds). Although increasing emphasis has been placed on using data-driven analytics to increase organizational efficiency, a gap still largely exists in integrating these methods into health information technology, especially for real-time decision-making.
CONTRIBUTORS
M.T., E.F., J.A., E.K., and S.L. made significant contributions to the conception and design of the work. M.T., J.A., and S.L. made significant contributions to the acquisition and processing of the data used for the analysis. M.T. and S.L. made significant contributions to the analysis and interpretation of the data for the work. All authors have contributed to either drafting or revising the article, have approved the version to be published, and agree to be accountable for all aspects of the work.
FUNDING
This work was supported by the Johns Hopkins Health System Department of Operations Integration.
COMPETING INTERESTS
None.
ACKNOWLEDGEMENTS
The authors wish to acknowledge Eric Schmitt and Kirby Smith for their assistance in the design and development of the web application.
REFERENCES
- 1.Bashore TM, Balter S, Barac A, et al. 2012. American College of Cardiology Foundation/Society for Cardiovascular Angiography and Interventions Expert Consensus Document on cardiac catheterization laboratory standards update: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents developed in collaboration with the Society of Thoracic Surgeons and Society for Vascular Medicine. J Am Coll Cardiol. 2012;59:2221–2305. [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics – 2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bashore TM, Bates ER, Berger PB, et al. American College of Cardiology/Society for Cardiac Angiography and Interventions Clinical Expert Consensus Document on cardiac catheterization laboratory standards. A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001;37:2170–2214. [DOI] [PubMed] [Google Scholar]
- 4.Dehmer GJ, Weaver D, Roe MT, et al. A contemporary view of diagnostic cardiac catheterization and percutaneous coronary intervention in the United States: A report from the CathPCI Registry of the National Cardiovascular Data Registry, 2010 through June 2011. J Am Coll Cardiol. 2012;60:2017–2031. [DOI] [PubMed] [Google Scholar]
- 5.Clark VL, Dolce J. Unplanned admissions after outpatient cardiac catheterization. Clin Cardiol. 1993;16:823–826. [DOI] [PubMed] [Google Scholar]
- 6.Levin SR, Dittus R, Aronsky D, et al. Optimizing cardiology capacity to reduce emergency department boarding: A systems engineering approach. Am Heart J. 2008;156:1202–1209. [DOI] [PubMed] [Google Scholar]
- 7.Litvak E. Optimizing patient flow by managing its variability. In: Berman S, ed. Front Office to Front Line: Essential Issues for Health Care Leaders. Oakbrook Terrace, IL: Joint Commission Resources; 2005:91. [Google Scholar]
- 8.Litvak E, Long MC. Cost and quality under managed care: irreconcilable differences? Am J Manag Care. 2000;6:305–312. [PubMed] [Google Scholar]
- 9.Levin SR, Harley ET, Fackler JC, et al. Real-time forecasting of pediatric intensive care unit length of stay using computerized provider orders. Crit Care Med. 2012;40:3058–3064. [DOI] [PubMed] [Google Scholar]
- 10.Levin S, Han J, Aronsky D, et al. 2007. IEEE international conference on industrial engineering and engineering management; stranded on emergency isle: Modeling competition for cardiac services using survival analysis. 2007;1772–1776. [Google Scholar]
- 11.Levin S, Dittus R, Aronsky D, et al. Evaluating the effects of increasing surgical volume on emergency department patient access. BMJ Qual Saf. 2011;20:146–152. [DOI] [PubMed] [Google Scholar]
- 12.Diercks DB, Roe MT, Chen AY, et al. Prolonged emergency department stays of non-ST-segment-elevation myocardial infarction patients are associated with worse adherence to the American College of Cardiology/American Heart Association guidelines for management and increased adverse events. Ann Emerg Med. 2007;50:489–496. [DOI] [PubMed] [Google Scholar]
- 13.Smith CD, Spackman T, Brommer K, et al. Re-engineering the operating room using variability methodology to improve health care value. J Am Coll Surg. 2013;216:559–568; discussion 568–570. [DOI] [PubMed] [Google Scholar]
- 14.O'Brien P, O'Connell C, Fenwick S, et al. Improved bed use with creation of a short-stay unit in a cardiac catheterization recovery room. Heart Lung. 2011;40:56–62. [DOI] [PubMed] [Google Scholar]
- 15.Dolkart O, Amar E, Weisman D, et al. Patient dissatisfaction following prolonged stay in the post-anesthesia care unit due to unavailable ward bed in a tertiary hospital. Harefuah. 2013;152:446–450, 500. [PubMed] [Google Scholar]
- 16.Institute for Healthcare Improvement. “Optimizing Patient Flow: Moving Patients Smoothly Through Acute Care Settings.” (Online information; retrieved 11/17/2014). 2003. http://www.ihi.org/IHI/Results/Whitepapers. [Google Scholar]
- 17.Institute of Medicine of the National Academies, Board on Health Care, Committee on the Future of Emergency Care in the United States Health System Services. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2007:397.
- 18.President's Council of Advisors on Science and Technology (U.S.). Report to the President, Better Health Care and Lower Costs: Accelerating Improvement Through Systems Engineering. [Washington, District of Columbia]: Executive Office of the President, President's Council of Advisors on Science and Technology, 2014.
- 19.Whippey A, Kostandoff G, Paul J, et al. Predictors of unanticipated admission following ambulatory surgery: a retrospective case-control study. Can J Anaesth. 2013;60:675–683. [DOI] [PubMed] [Google Scholar]
- 20.Gold BS, Kitz DS, Lecky JH, et al. Unanticipated admission to the hospital following ambulatory surgery. JAMA. 1989;262:3008–3010. [PubMed] [Google Scholar]
- 21.Mingus ML, Bodian CA, Bradford CN, et al. Prolonged surgery increases the likelihood of admission of scheduled ambulatory surgery patients. J Clin Anesth. 1997;9:446–450. [DOI] [PubMed] [Google Scholar]
- 22.Fleisher LA, Pasternak LR, Lyles A. A novel index of elevated risk of inpatient hospital admission immediately following outpatient surgery. Arch Surg. 2007;142:263–268. [DOI] [PubMed] [Google Scholar]
- 23.Chung F, Mezei G. Factors contributing to a prolonged stay after ambulatory surgery. Anesth Analg. 1999;89:1352–1359. [DOI] [PubMed] [Google Scholar]
- 24.Peck JS, Benneyan JC, Nightingale DJ, et al. Predicting emergency department inpatient admissions to improve same-day patient flow. Acad Emerg Med. 2012;19:E1045–E1054. [DOI] [PubMed] [Google Scholar]
- 25.Sun Y, Heng BH, Tay SY, et al. Predicting hospital admissions at emergency department triage using routine administrative data. Acad Emerg Med. 2011;18:844–850. [DOI] [PubMed] [Google Scholar]
- 26.Peck JS, Gaehde SA, Nightingale DJ, et al. Generalizability of a simple approach for predicting hospital admission from an emergency department. Acad Emerg Med. 2013;20:1156–1163. [DOI] [PubMed] [Google Scholar]
- 27.Littig SJ, Isken MW. Short term hospital occupancy prediction. Health Care Manag Sci. 2007;10:47–66. [DOI] [PubMed] [Google Scholar]
- 28.Hosmer D, Lemeshow S. Applied Survival Analysis: Regression Modeling of Time to Event Data. New York: Wiley; 1999. [Google Scholar]
- 29.Bursac Z, Gauss CH, Williams DK, et al. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17–0473–3–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hosmer D, Lemeshow S, Sturdivant R. Applied Logistic Regression. New York: Wiley; 2000. [Google Scholar]
- 31.Drazen E, Rhoads J. Using tracking tools to improve patient flow in hospitals. Issue Brief. California Healthcare Foundation; 2011. [Google Scholar]
- 32.Fortier J, Chung F, Su J. Unanticipated admission after ambulatory surgery – a prospective study. Can J Anaesth. 1998;45:612–619. [DOI] [PubMed] [Google Scholar]
- 33.Chambers CE, Dehmer GJ, Cox DA, et al. Defining the length of stay following percutaneous coronary intervention: an expert consensus document from the society for cardiovascular angiography and interventions. Endorsed by the American College of Cardiology Foundation. Catheter Cardiovasc Interv. 2009;73:847–858. [DOI] [PubMed] [Google Scholar]