Abstract
Mobile telemedicine involves the use of mobile device (e.g., cell phones, tablets) technology to exchange information to assist in the provision of patient care. Throughout the world, mobile telemedicine initiatives are increasing in number and in scale, but literature on their impact on patient outcomes in low-resource areas is limited. This study explores the potential impact of a mobile oral telemedicine system on the oral health specialty referral system in Botswana. Analysis of 26 eligible cases from June 2012 to July 2013 reveals high diagnosis concordance between dental officers and oral health specialists at 91.3% (21/23) but significant management plan discordance at 64.0% (16/25), over two-thirds of which involved the specialists disagreeing with the referring clinicians about the need for a visit to a specialist. These findings suggest mobile telemedicine can optimize the use of insights and skills of specialists remotely in regions where they are scarce.
Keywords: telemedicine, mobile Health (mHealth), oral medicine, disease management, health impact assessment
BACKGROUND
According to the World Health Organization’s Global Health Workforce Alliance, there is the challenge of both the sheer number of providers and their distribution, with almost half of the world’s population living in rural areas where about 40% of nurses and under 25% of doctors work.1 One tool for addressing the barriers of health care provision is mobile, or cellular phone based, technology. The use of such technology to assist specifically to facilitate the management of patients is known as mobile telemedicine.
As the coverage of mobile telecommunication networks has increased globally so have initiatives attempting to leverage them for telemedicine and for improving health more broadly under the umbrella of mobile health or mHealth.2 Despite this increase, a recent literature review on the impact of mHealth in Africa found the quality of data available to be poor and not addressing important questions about impact, access, scalability, and sustainability.3 A separate review of mobile health projects for non-communicable diseases in sub-Saharan Africa offered a thorough framework of optimizing work and research in the field which identified six health system challenges, the sixth being coordination of care, including consultation and referral systems.4
Botswana is estimated to have only three physicians per 10 000 individuals, only a small fraction of whom are specialists.5 Provided patients overcome obstacles to accessing the specialists, which include but are not limited to acquiring child care and travel arrangements, their medical care at the tertiary facility is frequently suboptimal. Patients may be asked to obtain diagnostic testing which could have been acquired closer to their home, and they may also face lengthy wait times for procedures that could have been scheduled in advance to optimize their visit. In addition some patients present to specialists for conditions that could have been managed by nonspecialists with appropriate guidance.
In 2007, the Botswana-UPenn Partnership (BUP) collaborated with the Botswana Ministry of Health (MoH) to implement some of the country’s pioneering mobile telemedicine systems to assist with the specialist referral systems in the fields of dermatology, oral medicine, and radiology. To contribute to the limited studies on the impact of mobile telemedicine focused on specialty referrals on patient outcomes, BUP undertook the study presented here of its mobile oral telemedicine system that allows clinicians in areas remote from oral maxillofacial surgeons and oral medicine specialists to refer patients with complicated oral lesions for virtual specialist consultation. The primary study objective was to assess the system’s impact on the patients’ diagnoses and management plans.
METHODS
Approval for our observational study was received from the Botswana MoH’s Human Research and Development Committee and University of Pennsylvania’s Institutional Review Board.
Mobile oral telemedicine system
An overview of the flow of the mobile oral telemedicine system is provided in Table 1. In brief, select dental officers practicing remote from oral medicine specialists and oral maxillofacial surgeons within Botswana were provided with HTC myTouch smart phones (HTC, New Taipei City, Taiwan) preloaded with an Open Data Kit (University of Washington, Seattle, WA, USA) mobile telemedicine application customized by Positive Innovation for the Next Generation (Gaborone, Botswana) for the BUP mobile oral telemedicine system (Figure 1). The dental officers submitted referrals through the application for patients with complicated oral lesions for whom they would like specialist input. They were able to include clinical data about the patients, including pictures, and their clinical assessment of the patient.
Table 1:
Overview of mobile oral telemedicine system in Botswana
| Step 1 | Dental officer evaluates a patient with a complicated oral problem for which the dental officer decides to open a mobile oral telemedicine case. |
| Step 2 | Dental officer records patient identifiable information in a ledger with a corresponding mobile oral telemedicine case identifier (e.g., 0001) |
| Step 3 | Dental officer logs into the customized mobile oral telemedicine system application using a supplied clinic smart phone. |
| Step 4 | Dental officer opens up a new case and inputs relevant patient information, including history of present condition, past medical history, photographs of the oral problem of concern and/or imaging that are taken using the smart phone camera, and his/her proposed diagnosis and management plan. |
| Step 5 | Dental officer submits the new case information to the mobile oral telemedicine database using the mobile network or Wi-Fi connection. |
| Step 6 | Dental officer establishes a plan to admit the patient or follow up with him/her in clinic while awaiting the specialist feedback. |
| Step 7 | Mobile oral telemedicine system sends a text message and e-mail to the specialist that a case is available for review. |
| Step 8 | Specialist logs into online portal for the mobile oral telemedicine system using a supplied tablet. |
| Step 9 | Specialist reviews submitted case information on the online portal. |
| Step 10 | Specialist opens a response template and inputs his proposed diagnosis and management plan. |
| Step 11 | Specialist submits the response to the mobile oral telemedicine database using the mobile network or Wi-Fi connection. |
| Step 12 | Mobile oral telemedicine system sends a text message and e-mail to the referring dental officer that a response from the specialist is available. |
| Step 13 | Dental officer logs into online portal via the mobile network or Wi-Fi network using the supplied clinic smart phone. |
| Step 14 | Dental officer reviews the submitted specialist response on the online portal. |
| Step 15 | Dental officer manages the patient based on input from the specialist. |
| Step 16 | Dental officer submits information the management and outcome of the patient through a follow up form available on the customized mobile oral telemedicine system application via the supplied clinic smart phone using the mobile network or Wi-Fi connection. |
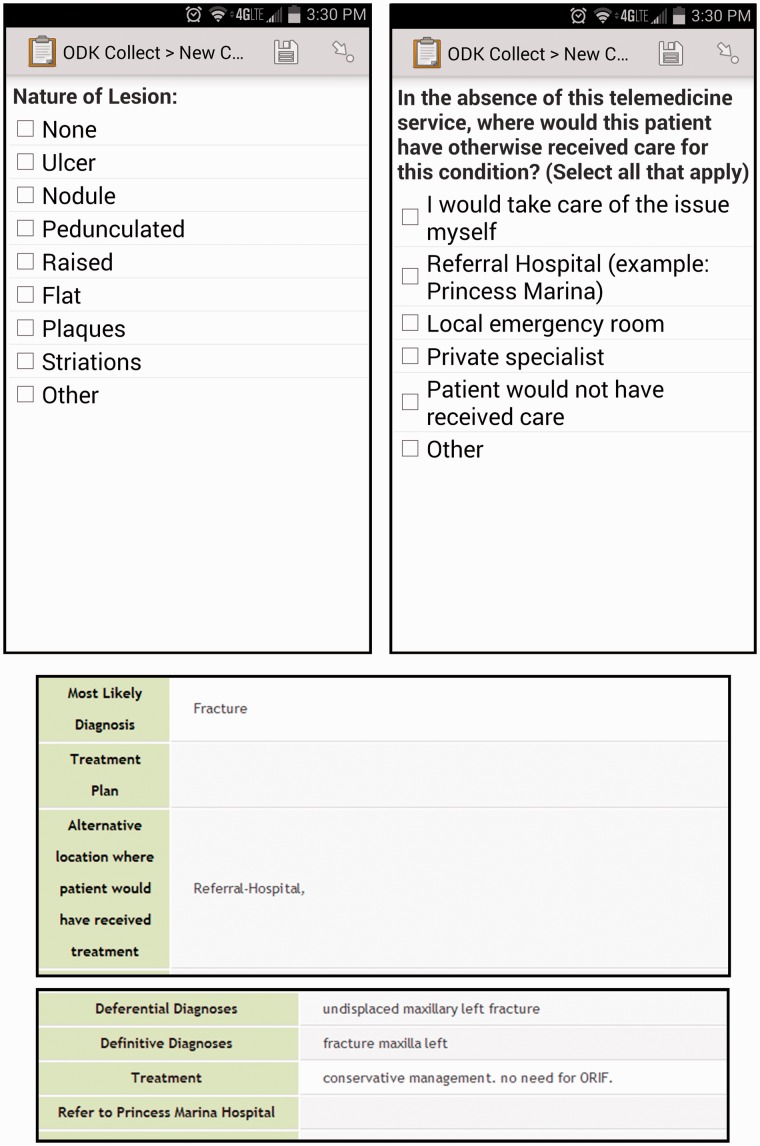
Figure 1:
Screenshots of the Mobile Oral Telemedicine System Application First row, left: A question that had existed on the mobile phone application used by referring providers since its development. First row, right: A question added to the mobile phone application used by referring providers as part of the study. Second row: Sample of the view of a case submitted by a referring provider as seen from the web-based portal. Third row: Sample of the view of the response submitted by a specialist to the case submitted in the row above as seen from the web-based portal.
Specialists in distant locations, including Gaborone and less often the United States, accessed an online portal on a ZTE Lite mobile tablet (ZTE Corporation, Shenzhen, China) through which they reviewed submitted cases and provided their input. The referring dental officers also received access to the online portal to view the specialists’ responses via their supplied mobile phones. After receiving the specialists’ responses, dental officers were to follow up with the relevant patients and submit information on the patients’ course of illness and treatment through the mobile telemedicine application.
Inclusion and exclusion criteria
Data was collected both retrospectively and prospectively as detailed here. Records for adult patients receiving care via the mobile oral telemedicine system in Botswana June–October 2012 were included for analysis and informed consent was waived. After approval of the study in October 2012, verbal informed consent had to be obtained for patients by the dental officers. Exclusion criteria for analysis were age <18 years, incomplete mobile telemedicine consultation, and failure to obtain consent for patients seen after October 2012.
Data collection and analysis
Data was retrieved directly from the mobile oral telemedicine system’s Open Data Kit database. For each case, the referring dental officer’s provisional diagnosis, differential diagnoses, proposed treatment plan, and level of care proposed in absence of telemedicine service were analyzed. The corresponding specialist’s provisional diagnosis, differential diagnosis, proposed treatment, and decision about patient’s need to be seen by the specialist were analyzed.
The diagnoses and management plans proposed by the dental officers referring cases were assessed for concordance with those put forward by the specialists. The inferred resource utilization of the two management plans was also assessed for concordance. Concordance was assessed as a categorical variable with values of Concordant, Discordant, and Unable to Determine.
Data was cleaned in Microsoft Excel (Microsoft, Redmond, WA, USA) and analyzed in Stata 12.1 for Windows (StataCorp LP, College Station, TX, USA). The data analysis plan was to utilize descriptive statistics (i.e., frequencies, means), comparative statistics (i.e., Chi-square), and sub-group analysis of patient outcomes.
RESULTS
Study population
Twenty-six eligible cases were submitted from June 2012 to July 2013. The average age of the patients was 45.5 years (SD 17.2 years). Table 2 shares the demographic and clinical breakdown of the patients as well as subgroup analysis by gender, HIV status, and provisional diagnosis at the time of the case submission from the referring dental officer. Provisional diagnoses were categorized into: cancer (e.g., Kaposi’s sarcoma, squamous cell carcinoma), infection (e.g., oral candidiasis, viral warts), fracture, benign mass (e.g., osteoma, silolith), dermatologic conditions (pemphigus, laceration), and other (e.g., “osteoradionecrosis”).
Table 2:
Study results with subanalysis by demographic and clinical data
| Number of cases | Proportion with diagnostic concordancea | Proportion with treatment concordancea | Proportion of potential referrals that would be divertedb | |
|---|---|---|---|---|
| Total | 26 | 21/23 | 9/25 | 11/21 |
| 91.3% | 36.0% | 52.4% | ||
| Gender | ||||
| Female | 14 | 11/12 | 7/14 | 3/11 |
| 91.7% | 50.0% | 27.3% | ||
| Male | 12 | 10/11 | 2/11 | 8/10 |
| 90.9% | 18.2% | 80.0% | ||
| P-values | .95 | .10 | .02 | |
| HIV Status | ||||
| Negative | 20 | 17/19 | 4/19 | 11/19 |
| 89.5% | 21.1% | 57.9% | ||
| Positive | 6 | 4/4 | 5/6 | 0/2 |
| 100% | 83.3% | 0.0% | ||
| P-values | .50 | .01 | .12 | |
| Referring Dental Officer’s Provisional Diagnosis | ||||
| Cancer | 7 | 6/6 | 1/6 | 3/5 |
| 100% | 16.7% | 60% | ||
| Infection | 2 | 1/2 | 0/2 | 1/2 |
| 50% | 0.0% | 50% | ||
| Fracture | 4 | 3/475% | 1/425% | 2/450% |
| Benign mass | 4 | 4/4100% | 2/450% | 2/450% |
| Dermatologic condition (noninfectious) | 3 | 3/3100% | 1/333.3% | 2/2100% |
| Other | 2 | 2/2100% | 1/250% | 0/20.0% |
| P-values | .76 | .76 | .53 | |
The table below presents descriptive proportions of cases submitted through the mobile oral telemedicine system in categories of diagnostic concordance, treatment concordance and potential referrals that would be diverted based on responses from specialists. Subgroup analysis by gender, HIV status and the provisional diagnosis at the time of the case submission by the referring dental officer is included. Pearson Chi-square analysis of differences with subgroups noted and relationship bolded for P < 0.05.
aThe denominators are the cases for which the relevant data for both the referring dental officer and the answering specialist was available.
bThe denominators are the cases in which the referring dental officer indicated he/she would have sent the patient to the referral hospital in the absence of telemedicine services whereas the numerators are the cases in which the responding specialist indicated the patient did not need to be seen in the referral hospital.
Diagnostic and management concordance
Diagnoses from both the referring dental officer and the responding specialist were available for 23 of the cases and concordant in 21 of them (91.3%). Management plans were available from both providers in 25 of the cases and was concordant in 9 (36.0%).
With regard to discordance in management plans for 16 cases, in 11 cases (68.8%) the referring dental officer indicated he/she would have referred the patient to the specialist in the absence of the telemedicine system whereas the specialist indicated not to do so. Review of these cases revealed the specialist recommended biopsy alone in four cases, biopsy and oral medications in one case, biopsy and blood work in one case, procedure by the local provider in three cases, conservative management in one case, and referral to another specialist, specifically a radiation oncologist, in one case. In review of the other five cases in which there was management discordance was not related to which provider was deemed appropriate for the patients’ next visit, in one case both the referring dental officer and the specialist agreed the former could manage it but the specialist recommended a medication the referring dental officer did not consider. In the other four cases both parties agreed a referral to a specialist was prudent, but in three cases the specialist asked for imaging beforehand, in two cases for certain laboratory studies, and in one case a biopsy rather than imaging as volunteered by the referring dental officer.
DISCUSSION
Optimization of scarce resources is a priority for the provision of health care in resource-limited settings. Our study in Botswana indicates the utilization of mobile technology to afford clinicians input from specialists can avoid unnecessary referrals while still allowing for clinicians to work up and treat the patients in an informed manner distinct from what they would have done otherwise. While subanalysis by gender and HIV status did show a statistically significant difference, more work needs to be done to determine clinical relevance.
Our finding that 52.4% of submitted cases could potentially be managed without the patient needing an in-person specialist visit that would have otherwise been sought is in line with a comparable study of over 400 cases using a computer-based specialist referral system involving a variety of specialties in Canada which found based on physician recall 43% of cases avoided in-person specialist referral.6 Though different populations, settings, and system modalities, the resemblance of the outcomes of both our studies strongly suggests there is a substantial proportion of cases for which providers need specialist guidance but do not necessitate an in-person consultation. Being able to more effectively manage this subgroup with mobile telemedicine therefore could have a large impact on optimizing resource utilization around specialty care.
Limitations
A significant limitation of our study is the small number of cases. This was due in part to the challenge of consenting patients given the requirement for study recruiters to have human subjects research training, which none of the referring dental officers had prior to the study’s initiation. Another reason for few cases was the decision to transition from the pilot mobile oral telemedicine system to a forthcoming mobile telemedicine system to be used across multiple specialties under the direction of the MoH. Delays with the development of the latter system led to the former being discontinued without anything available to take its place and therefore an inability to send cases towards the end of the study period.
Another notable limitation of the study is while suggestive of the potential for more informed care of patients with complex oral lesions, data on what actually happened to the patients is necessary to determine if that potential was in fact realized. Though the mobile oral telemedicine system had a component that involved the referring dental officers submitting information on what ultimately happened to the patients for whom cases were submitted, including treatments they underwent and the clinical progression of their ailments, such data was not sent in the vast majority of the cases (24/26, 92.3%).
CONCLUSION
The preliminary results of this study on the potential diversion of unnecessary referrals and optimization of patient care at primary and secondary care facilities were shared with the MoH and helped motivate its efforts to scale this approach throughout the country. The hope is for the country-wide system to overcome challenges of being able to access patient outcomes through more optimal integration of the system into the workflow of relevant providers and patients’ medical health records. Investigation of these outcomes will be crucial in more accurately capturing the system’s impact and subsequently enhancing it. The expansion of mobile oral telemedicine services in Botswana will likely make such future research in the country more robust, and those working in other resource-limited settings with adequate mobile network infrastructure will be able to learn from its efforts accordingly.
FUNDING
This work has been supported by a Doris Duke Charitable Foundation Clinical Research Fellowship Grant to author M.T.
COMPETING INTERESTS
The authors have no competing interests to declare.
CONTRIBUTORS
Each of the authors has given final approval of the submitted manuscript. The authors qualify for authorship based on their substantial contributions to the intellectual content as indicated below:
-Conception and design: M.T., R.L.-Q., C.A., D.M., M.P., B.T., C.K.
-Acquisition of data: M.T., D.M., M.P., B.T., N.M.-D.
-Analysis and interpretation of data: M.T., C.K.
-Drafting of the manuscript: M.T.
-Critical revision of the manuscript for important intellectual content: M.T., R.L.-Q., C.A., D.M., M.P., B.T., N.M.-D., C.K.
ACKNOWLEDGEMENTS
We would like to recognize the support of all the medical officers, health care providers, and patients in Botswana that made the study and this innovative form of care possible.
REFERENCES
- 1.World Health Organization. Health workers: a global profile. In: The World Health Report 2006- Working together for health. Geneva, Switzerland: World Health Organization; 2006: 1–17. [Google Scholar]
- 2.Betjeman TJ, Soghoian SE, Foran MP. mHealth in Sub-Saharan Africa. Int J Telemed Appl Appl. 2013. doi:10.1155/2013/482324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health. 2014;14:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bloomfield GS, Vedanthan R, Vasudevan L, et al. Mobile health for non-communicable diseases in Sub-Saharan Africa: a systematic review of the literature and strategic framework for research. Globalization and Health. 2014;10:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Bank. Data: Physicians (per 1,000 people). http://data.worldbank.org/indicator/SH.MED.PHYS.ZS Accessed 11 July 2014. [Google Scholar]
- 6.Keely E, Liddy C, Afkham A. Utilization, Benefits, and Impact of an e-Consultation Service Across Diverse Specialties and Primary Care Providers. Telemed J E Health. 2013;19(10):733–738. [DOI] [PMC free article] [PubMed] [Google Scholar]