Abstract
Adult spinal deformity (ASD) is one of the most challenging spinal disorders associated with broad range of clinical and radiological presentation. Correct selection of fusion levels in surgical planning for the management of adult spinal deformity is a complex task. Several classification systems and algorithms exist to assist surgeons in determining the appropriate levels to be instrumented. In this study, we describe our new simple decision making algorithm and selection of fusion level for ASD surgery in terms of adult idiopathic idiopathic scoliosis vs. degenerative scoliosis.
Keywords: Adult spinal deformity, Idiopathic scoliosis, Classification, Spinal fusion, Selective fusion, Algorithm
INTRODUCTION
Adult spinal deformity (ASD) is one of the most challenging spinal disorders associated with broad range of clinical and radiological presentations. Such deformities can involve any complex spectrum of spinal diseases that present in late adolescent and adulthood including adolescent and adult idiopathic scoliosis, degenerative scoliosis/kyphosis, sagittal and coronal imbalance, and postoperative deformity30). Decision making process is versatile among surgeons. In this study, we describe our new simple decision making algorithm and selection of fusion level for ASD surgery in terms of idiopathic, non-degenerative vs. degenerative deformity.
ADULT IDIOPATHIC SCOLIOSIS
Decision making algorithm for adult idiopathic scoliosis up to age of 50 is basically similar to adolescent idiopathic scoliosis. Hibbs9) introduced spinal fusion for the treatment of adolescent idiopathic scoliosis. He differentiated primary major curve from secondary minor curve. Primary major curve was always included in the fusion from end vertebra to end vertebra without rotation. Then the surgical treatment of adolescent idiopathic scoliosis (AIS) has made remarkable progress with the development of the Harrington8) rod in the late 1950s. Based on the experience on Harrington instrumentation, King et al.18) described their principle for selection of fusion level with their curve classification as follows : 1) Type I/S curve with true double major curve (thoracic and lumbar-thoracolumbar curve), fusion of both thoracic and lumbar (thoracolumbar) curves to the lower vertebra is needed, but no lower than the fourth lumbar vertebra (Stop at L3/L4); 2) Type II/S curve but false double major curve, selective fusion of the thoracic curve only is possible to the neutral vertebra (NV) and stable vertebra (SV) around thoracolumbar junction as the lowest instrumented vertebra (LIV). If the NV and SV are not same, the SV is the lowest instrumented vertebra (LIV); 3) Type III/Not S curve but overhanging curve. The LIV is the first vertebra that is most closely bisected by the center sacral vertical line (CSL) (=SV); 4) Type IV/Not S curve but overhanging curve down to L4, the LIV is the first vertebra that is bisected by the CSL (=SV); 5) Type V/Structural proximal thoracic curve, fusion of both proximal thoracic and main thoracic curves is needed. The first vertebra closely bisected by the CSL was selected as LIV around TL junction18). King et al. classification had several benefits : 1) The first treatment based classification, 2) Stable vertebra concept as the LIV, 3) Differentiated "selective thoracic fusion" of Type II curves (false double major curve) from thoracic and lumbar fusion of Type I (true double major curve) when appropriate, and 4) double thoracic curve identified (Type V : structural proximal thoracic and main thoracic curve). However, there were also several problems as follows : 1) fair to poor inter- and intra-observer reliability19), 2) Coronal plane only assessment without sagittal plane consideration, 3) Tough distinction between Type II & III curves29), 4) Exclusion of triple major curves (addition of type I and V) and isolated thoracolumbar/lumbar curves, and 5) Classification based on Harrington instrumentation outdated in era of segmental spinal instrumentation.
To overcome those limitations of King classification, Lenke et al.20) developed a new classification system to determine extent of spinal arthrodesis with three components : curve type (1 through 6), a lumbar spine modifier (A, B, or C), and a sagittal thoracic modifier (minus, normal, or plus). The six curve types have specific characteristics, on coronal and sagittal radiographs, that differentiate structural and nonstructural curves in the proximal thoracic, main thoracic, and thoracolumbar/lumbar (TL/L) regions. According to Lenke classification, major and structural minor curve should be fused. Advantages of Lenke classification are; 85–90% predictability, thoracolumbar/lumbar curves included, triple curve (Lenke type 4) defined, and 2-dimensional (coronal and sagittal plane) classification. However, several limitations have been recognized as follows : 12% rule breaker4), no selective fusion criteria included, poor inter-observer reliability in proximal thoracic curve, 2-dimensional (not 3-dimensional), no lowest or uppermost instrumented vertebra (UIV) criteria included. Using by Lenke classification, LIV is usually located in the middle of the curve for 3 or 4 curve A or B lumbar modifier.
Proposal of a new re-grouping of Lenke classification for AIS/young Adult IS
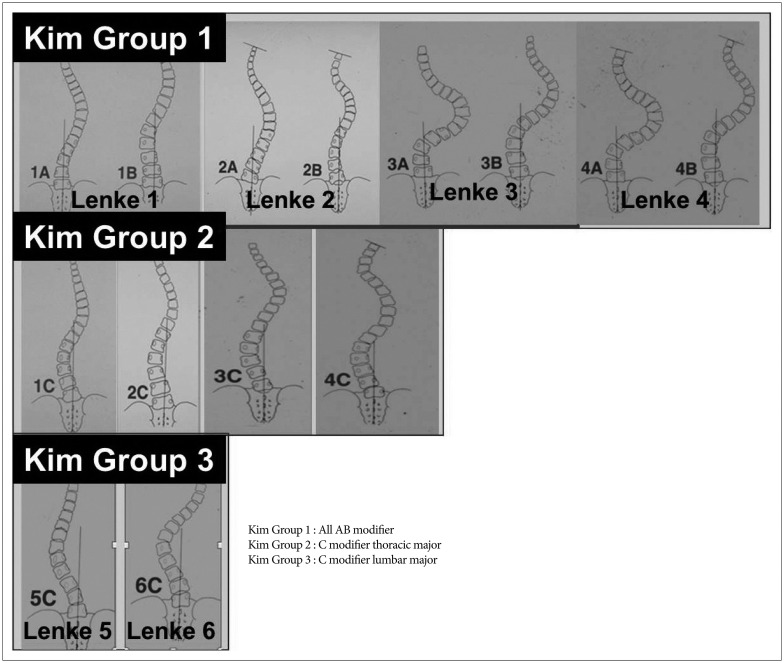
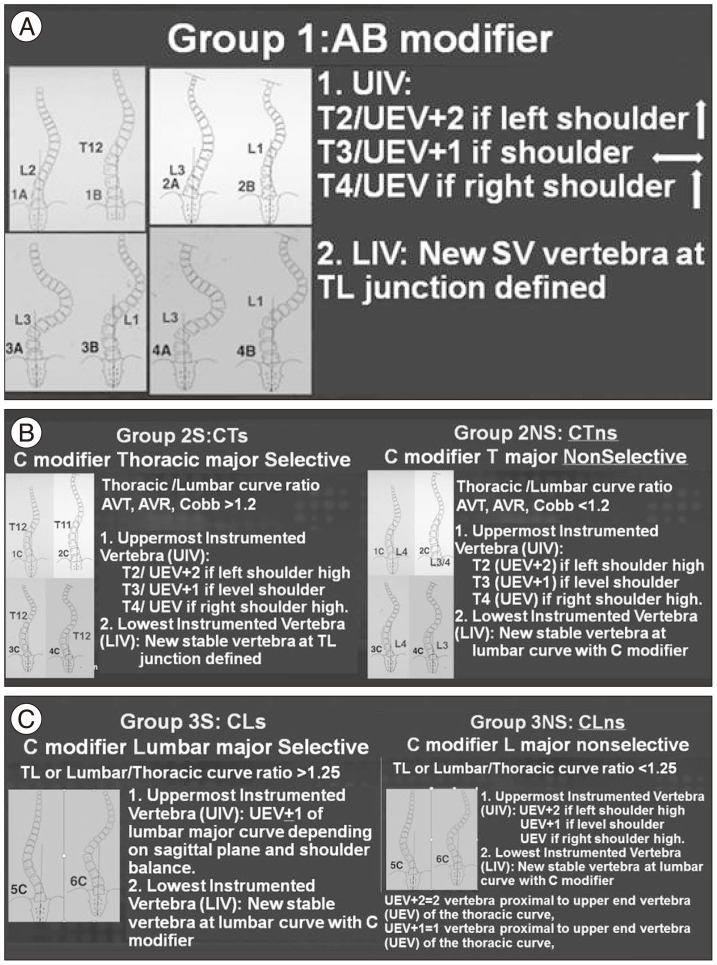
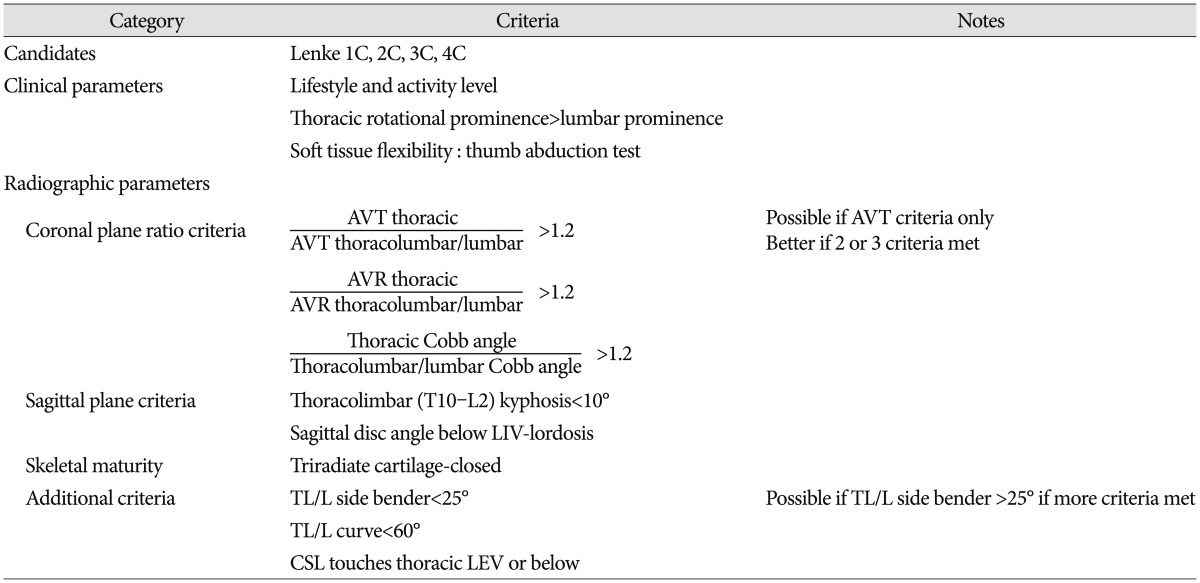
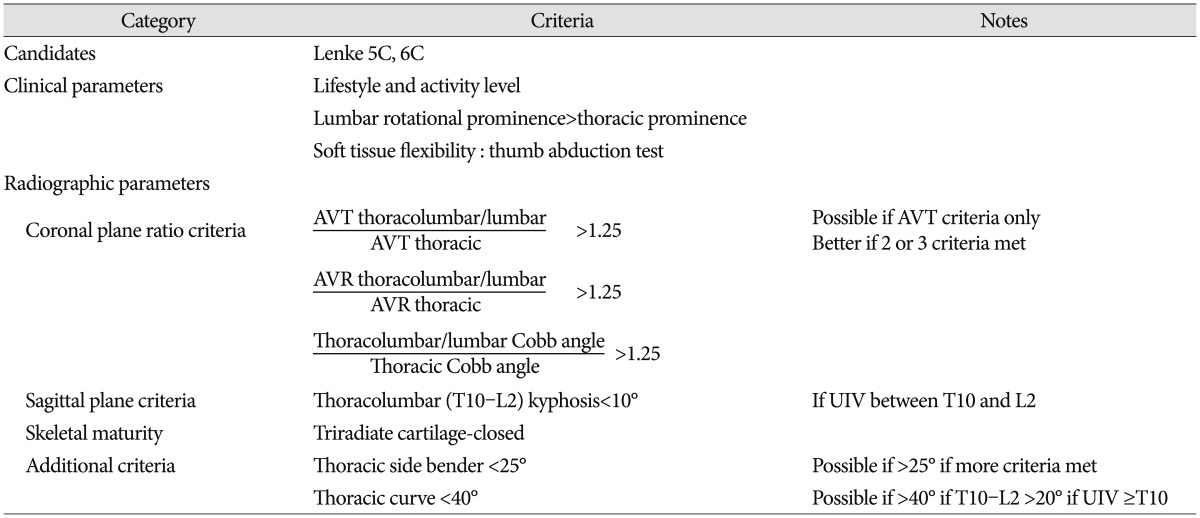
To overcome those limitations of Lenke classification, we developed a new classification for AIS and adult idiopathic scoliosis (Fig. 1). We made all curves into three groups according to lumbar modifier by Lenke classification. Group 1 includes all lumbar A or B modifier (Fig. 2A). Group 2 includes lumbar C modifier with thoracic major (Fig. 2B). Group 3 includes lumbar C modifier with lumbar major curve (Fig. 2C). Group 2 and 3 can be divided into 2 sub-groups by selective fusion criteria6,21,26) using apical vertebral translation (AVT), apical vertebral rotation (AVR) and Cobb angle (Table 1, 2). Classifying process is as follows. Step 1 is making center sacral vertical line (CSVL) per Lenke classification. If CSVL is touching a vertebral body at lumbar apex (lumbar A or B modifier), the curve is classified into group 1 and group 2 or 3 if not (lumbar C modifier). Step 2 is making proximal thoracic, major thoracic, and lumbar/thoracolumbar Cobb angle measurement for all curves. Among C modifiers, the curve is classified into group 2 if main thoracic curve is the major curve, the largest. If lumbar or thoracolumbar curve is the major curve, the largest and then the curve is classified into group 3. After definition of group 2 and 3, sub-group classification will follow the selective fusion criteria or not. Group 2 selective (Group 2S) includes curves with lumbar C modifier/main thoracic major curve/selective thoracic fusion only possible. Group 2 non-selective (Group 2NS) includes curves with lumbar C modifier/main thoracic major curve/selective thoracic fusion impossible. Group 3 selective (Group 3S) includes curves with lumbar C modifier/lumbar or thoracolumbar major curve/selective lumbar or thoracolumbar fusion only possible. Group 3 non-selective (Group 3 NS) includes curves with lumbar C modifier/lumbar or thoracolumbar major curve/selective lumbar or thoracolumbar fusion only impossible.
Fig. 1. Re-grouping of Lenke classification.
Fig. 2. A : Group 1. All lumbar AB modifier. B : Group 2. All lumbar C modifier with thoracic major curve. C : Group 3. All lumbar C modifier with lumbar major curve.
Table 1. Factors for selective fusion of thoracic curves in lumbar C modifiers.
Table 2. Factors for selective fusion of lumbar curves in lumbar C modifiers.
Proposal of a new selection of fusion level by new grouping of Lenke classification
Selection of the uppermost instrumented vertebra
The selection criteria of UIV selection comes in 2 categories, stop at upper thoracic area above the upper end vertebra of the thoracic major curve or stop around the upper end vertebra of the lumbar major curve. In case of UIV above the upper end vertebra of the thoracic major curve, T2 as UIV if left shoulder high, T3 if level shoulder and T4 if right shoulder high were recommended if proximal thoracic curve is structural by Lenke classification. Upper end vertebra (UEV) of thoracic major+2 (2 vertebra proximal) as UIV if left shoulder high, UEV+1 (1 vertebra proximal) if level shoulder, UEV if right shoulder high were recommended if proximal thoracic curve is non-structural by Lenke classification. These criteria are applicable for Group 1, Group 2S, Group 2NS, and Group 3NS. However, Group 3S includes fusion of lumbar major curve only. Upper end vertebra (UEV) of lumbar major was recommended. The short fusion strategy might involve instrumentation of the vertebra one level caudal to the UEV as an alternative to the conventional strategy, which includes instrumentation of the UEV via anterior/Posterior spinal fusion25).
Selection of the lowest instrumented vertebra
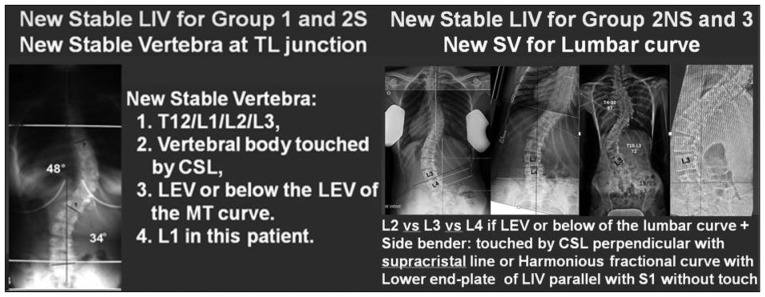
The selection criteria of LIV selection comes in 2 categories, stop around TL junction around the lower end vertebra (LEV) of the thoracic major curve or stop at L3/L4 at or below the lumbar major curve. The new stable vertebra (SV) around TL junction for Group 1 and Group 2S is defined as the most proximal vertebral body around TL junction touched by center sacral vertical line (CSVL), but at or below the LEV of the main thoracic curve (Case 1 in the online-only Data Supplement). Previous study demonstrated huge differences between LIV touch by CSVL and LIV not touched by CSVL17). The new stable vertebra (SV) around lower lumbar spine for Group 2NS and Group 3 is defined as the lowest vertebral body touched by CSVL with side-bender even though not touched by CSVL in standing PA X-ray or harmonious fractional curve with lower end-plate of LIV parallel with sacrum even though not touched by CSVL but LEV or below the LEV of the lumbar major curve (Fig. 3). No benefit was identified for fusing to LEV+1 (1 vertebra distal to LEV) in moderate TL/L idiopathic scoliosis patients undergoing posterior selective fusion with pedicle screws. For patients with TL/L Cobb angle more than 60°, the distal fusion level probably needs to be LEV+127).
Fig. 3. New stable vertebra at TL junction and lower lumbar spine.
Selection of fusion level (UIV and LIV) by New group
Group 1 (all lumbar AB modifier)
UIV selection criteria, select T2 or UEV+2 (2 vertebra proximal to UEV) of thoracic major as UIV if left shoulder high, T3 or UEV+1 (1 vertebra proximal to UEV) of thoracic major if level shoulder and T4 or UEV of the thoracic major if right shoulder high. LIV selection criteria includes new SV at the thoracolumbar junction as the most proximal vertebral body around TL junction touched by center sacral vertical line (CSVL), but at or below the LEV of the main thoracic curve.
Group 2 (all lumbar C modifier with thoracic major)
1) Selective fusion subgroup (Group 2S) determined by AVT, AVR, and Cobb angle if thoracic/lumbar ratio >1.2. UIV selection criteria are to choose T2/UEV+2 as UIV if left shoulder high, T3/UEV+1 if level shoulder, T4/UEV if right shoulder high. LIV selection criteria are to select new SV around TL junction as the LIV at the thoracolumbar junction as the most proximal vertebral body around TL junction touched by center sacral vertical line (CSVL), but at or below the LEV of the main thoracic curve (Case 2 in the online-only Data Supplement).
2) Non-selective fusion subgroup (Group 2NS) determined by AVT, AVR, and Cobb angle if thoracic/lumbar ratio <1.2. UIV selection criteria are to choose T2/UEV+2 as UIV if left shoulder high, T3/UEV+1 if level shoulder, T4/UEV if right shoulder high. LIV selection criteria are to choose new SV at lower lumbar spine as the lowest vertebral body touched by CSVL with side-bender even though not touched by CSVL in standing PA X-ray or harmonious fractional curve with lower end-plate of LIV parallel with sacrum even though not touched by CSVL but LEV or below the LEV of the lumbar major curve. No benefit was identified for fusing to LEV+1 (1 vertebra distal to LEV) in moderate TL/L idiopathic scoliosis patients undergoing posterior selective fusion with pedicle screws (Case 3 in the online-only Data Supplement). For patients with TL/L Cobb angle more than 60°, the distal fusion level probably needs to be LEV+127).
Group 3 (all lumbar C modifier with lumbar major)
1) Selective fusion subgroup (Group 3S) determined by AVT, AVR, and Cobb angle if lumbar/thoracic ratio >1.25. UIV selection criteria are to choose UEV or UEV-1 (1 vertebra below the UEV) of lumbar major curve depending on sagittal plane and shoulder balance. LIV selection criteria, select new SV as LIV at the lower lumbar curve (Case 4 in the online-only Data Supplement).
2) Non-selective fusion subgroup (Group 3NS) determined by AVT, AVR, and Cobb angle if lumbar/thoracic ratio <1.25. UIV selection criteria are to choose UEV of the main thoracic curve +2 as UIV if left shoulder high, UEV+1 if level shoulder, UEV if right shoulder high. LIV selection criteria are to choose new SV as LIV at the lower lumbar curve (Case 5 in the online-only Data Supplement).
DEGENERATIVE SCOLIOSIS OR DEGENERATIVE SAGITTAL IMBALANCE
The selection of appropriate treatment for degenerative ASD is challenging because the condition is heterogeneous with diverse presentation of symptoms, and the results are variable. Moreover, unlike the Lenke Classification system for AIS, no single system has become widely accepted and incorporated into daily practice. The Adult Spinal Deformity Committee of the Scoliosis Research Society (SRS) has undertaken an effort to develop a classification system for adult deformity based on the efforts by Schwab et al.22,24,28). This classification system appears more comprehensive, drawing parameters such as overall global balance and lumbar degenerative modifiers into consideration and including pelvic parameters. Although the SRS classification system does provide more comprehensive classification system, much work is still needed in attempting to link the patient's deformity to a treatment algorithm. Thus, we describe essential four steps of decision making for degenerative ASD.
Step 1. Decompression or not
Whether central or foraminal decompression should be chosen, it depends on patient's symptoms and radiological findings. Neurogenic claudication in the setting of central and lateral recess stenosis without significant axial back pain, segmental instability, or progressively worsening deformity would be treated with stand-alone decompression surgery. These may worsen over time, especially after decompression, and may require a revision operation hence stand-alone decompression is not frequently indicated.
Step 2. UIV from upper thoracic vs. thoracolumbar junction
To summarize the issue from literatures, 1) no clinical outcome difference to stop at UT or TL despite the preoperative sagittal imbalance16); 2) nonunion3,7,14) is more common in UT group; 3) proximal junctional kyphosis7,14) or failure is more common in TL group; and 4) UT recommended among patients with severe osteoporosis, thoracolumbar kyphosis, or significant sagittal/coronal imbalance3,14) (Case 8 in the online-only Data Supplement).
Step 3. L5 or S1 or pelvis?
LIV to L5 recommended if 1) normal L5–S1 disc and facet joint; 2) UIV is T10 or below; 3) without global sagittal imbalance; 4) no osteoporosis, and 5) young or less active patient. LIV to S1 recommended if 1) abnormal disc or facet joint at L5–S1; 2) long fusion from T9 or above; 3) sagittal imbalance operations, 4) osteoporosis, and old age (Case 6 in the online-only Data Supplement). Also pelvic fixation and 3rd or 4th rod should be added if UIV L2 or above and 3-column osteotomy is utilized2,5,11,13,16). The use of a multiple-rod construct is a simple and effective method to provide increased stability across 3-column osteotomy sites to significantly prevent implant failure and symptomatic pseudarthrosis vs. a standard 2-rod contruct11).
Step 4. Sagittal/coronal re-balance
to achieve optimal sagittal/coronal balance, we should take into account global (C7 plumb to sagittal/central sacral vertical line) as well as regional balance [T2–5/T5–12/T10–L2/T12–S1/sacral slope (SS)/pelvic incidence (PI)]. Furthermore, we should keep in mind reciprocal or sequential change after corrective surgery (Case 7 in the online-only Data Supplement). In our series, 33° increase of lordosis is achieved after single level pedicle subtraction osteotomy. The 33° increase is composed by 9° increase in SS and 24° increase in T12 low endplate angle. Surgical goal is esteemed by Kim Formula (TK+LL+PI) between 22° (ideal value) and 45° (acceptable value)10,12,15,23). Appropriate osteotomy can be selected by using Bridwell's algorithm for osteotomy1) (Case 9 in the online-only Data Supplement).
CONCLUSION
We described decision making algorithm and selection of fusion level for adolescent and adult spinal deformity surgery in terms of idiopathic, non-degenerative vs. degenerative deformity. Specially, we developed a new classification by re-grouping Lenke classification for AIS and adult idiopathic deformity without a significant degeneration to overcome the limitations of Lenke classification. Our classification adapted selective fusion criteria for Group 2 & 3 curves. Our treatment algorithm does not account for every exception, and further research is required to improve long-term surgical outcomes.
Acknowledgements
The submitted manuscript was presented by Yongjung J. Kim, M.D. as an invited speaker at the recent annual autumn meeting of The Korean Neurosurgical Society, 2015. The submitted manuscript does not contain information about medical devices or drugs.
Supplementary Materials
The online-only Data Supplement is available with this article at http://dx.doi.org/10.3340/jkns.2016.59.4.327.
15 year-old-girl with Group 1.
13 year-old-girl with Group 2S.
18 year-old-girl with Group 2NS.
15 year-old-girl with Group 3S.
15 year-old-girl with Group 3NS.
A: A 66-year old female with degenerative lumbar scoliosis with good sagittal balance underwent posterior spinal fusion from T10 to L5. Her sagittal balance was tolerable and her disc at L5–S1 was well-preserved before surgery. Radiographic and clinical outcomes were excellent in 3 years post operation. B: An 82-year old female with sagittal imbalance and distal junctional failure underwent posterior vertebral column resection at L1 and spinal fusion from T9 to L5. Radiographic and clinical outcomes were poor even after the reconstructive surgery.
A: A 60-year old female with degenerative lumbar kyphoscoliosis underwent anterior and posterior spinal fusion from T12 to pelvis. Her sagittal/coronal balance was nicely restored after surgery. Radiographical and clinical outcomes were excellent. B: A 74-year old female with sagittal/coronal imbalance and postoperative thoracic decompensation underwent multi-level Ponte osteotomies/prophylactic vertebroplasty at T9 and T10 and spinal instrumentation/fusion from T10 to pelvis via only posterior. Radiographical and clinical outcomes were excellent in 2 years postoperative.
A representative case requiring a pedicle subtraction osteotomy. A 71-year old female with degenerative thoracolumbar kyphosis underwent a pedicle subtraction osteotomy at L4 and 3-level Ponte osteotomies and spinal instrumentation/fusion from T3 to pelvis. Her sagittal balance was nicely restored after surgery. Radiographic and clinical outcomes were excellent in 3 years postoperative.
A 70-year old female with degenerative thoracolumbar kyphoscoliosis underwent a posterior vertebral column resection at the apex of the curve and spinal instrumentation/fusion from T9 to pelvis with prophylactic vertebroplasty. Her sagittal/coronal balance was nicely corrected after surgery. Radiographical and clinical outcomes were excellent in 2 years postoperative.
References
- 1.Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976) 2006;31(19 Suppl):S171–S178. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 2.Bridwell KH, Lewis SJ, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am. 2003;85-A:454–463. doi: 10.2106/00004623-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Cho SK, Shin JI, Kim YJ. Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J. 2014;23:2726–2736. doi: 10.1007/s00586-014-3531-4. [DOI] [PubMed] [Google Scholar]
- 4.Clements DH, Marks M, Newton PO, Betz RR, Lenke L, Shufflebarger H Harms Study Group. Did the Lenke classification change scoliosis treatment? Spine (Phila Pa 1976) 2011;36:1142–1145. doi: 10.1097/BRS.0b013e318207e9c4. [DOI] [PubMed] [Google Scholar]
- 5.Edwards CC, 2nd, Bridwell KH, Patel A, Rinella AS, Jung Kim Y, Berra AB, et al. Thoracolumbar deformity arthrodesis to L5 in adults : the fate of the L5-S1 disc. Spine (Phila Pa 1976) 2003;28:2122–2231. doi: 10.1097/01.BRS.0000084266.37210.85. [DOI] [PubMed] [Google Scholar]
- 6.Fischer CR, Kim Y. Selective fusion for adolescent idiopathic scoliosis : a review of current operative strategy. Eur Spine J. 2011;20:1048–1057. doi: 10.1007/s00586-011-1730-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ha Y, Maruo K, Racine L, Schairer WW, Hu SS, Deviren V, et al. Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum : a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine. 2013;19:360–369. doi: 10.3171/2013.5.SPINE12737. [DOI] [PubMed] [Google Scholar]
- 8.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44-A44-A:591–610. [PubMed] [Google Scholar]
- 9.Hibbs RA. A report of fifty-nine cases of scoliosis treated by the fusion operation. By Russell A. Hibbs, 1924. Clin Orthop Relat Res. 1988;(229):4–19. [PubMed] [Google Scholar]
- 10.Hyun SJ, Kim YJ, Rhim SC. Spinal pedicle subtraction osteotomy for fixed sagittal imbalance patients. World J Clin Cases. 2013;1:242–248. doi: 10.12998/wjcc.v1.i8.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hyun SJ, Lenke LG, Kim YC, Koester LA, Blanke KM. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976) 2014;39:1899–1904. doi: 10.1097/BRS.0000000000000556. [DOI] [PubMed] [Google Scholar]
- 12.Hyun SJ, Rhim SC. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients : a long-term follow-up data. J Korean Neurosurg Soc. 2010;47:95–101. doi: 10.3340/jkns.2010.47.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hyun SJ, Rhim SC, Kim YJ, Kim YB. A mid-term follow-up result of spinopelvic fixation using iliac screws for lumbosacral fusion. J Korean Neurosurg Soc. 2010;48:347–353. doi: 10.3340/jkns.2010.48.4.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion : minimum five-year follow-up. Spine (Phila Pa 1976) 2008;33:2179–2184. doi: 10.1097/BRS.0b013e31817c0428. [DOI] [PubMed] [Google Scholar]
- 15.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1 : can we predict ideal lumbar lordosis? Spine (Phila Pa 1976) 2006;31:2343–2352. doi: 10.1097/01.brs.0000238970.67552.f5. [DOI] [PubMed] [Google Scholar]
- 16.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Kim YW. Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine (Phila Pa 1976) 2007;32:2653–2661. doi: 10.1097/BRS.0b013e31815a5a9d. [DOI] [PubMed] [Google Scholar]
- 17.Kim YJ, Fischer CR, Lenke LG, Bridwell KH, Boachie-Adjei O, Clement J, et al. Optimal lower instrumented vertebra to avoid adding-on or distal junctional kyphosis for thoracic adolescent idiopathic scoliosis. Podium presentation no. 88; Proceeding of the Scoliosis Research Society Annual Meeting; 2011 Sep 14-17; Louisville, USA. Milwaukee, WI: SRS; 2011. [Google Scholar]
- 18.King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:1302–1313. [PubMed] [Google Scholar]
- 19.Lenke LG, Betz RR, Bridwell KH, Clements DH, Harms J, Lowe TG, et al. Intraobserver and interobserver reliability of the classification of thoracic adolescent idiopathic scoliosis. J Bone Joint Surg Am. 1998;80:1097–1106. doi: 10.2106/00004623-199808000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis : a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-A:1169–1181. [PubMed] [Google Scholar]
- 21.Lenke LG, Bridwell KH, Baldus C, Blanke K. Preventing decompensation in King type II curves treated with Cotrel-Dubousset instrumentation. Strict guidelines for selective thoracic fusion. Spine (Phila Pa 1976) 1992;17(8 Suppl):S274–S281. doi: 10.1097/00007632-199208001-00011. [DOI] [PubMed] [Google Scholar]
- 22.Lowe T, Berven SH, Schwab FJ, Bridwell KH. The SRS classification for adult spinal deformity : building on the King/Moe and Lenke classification systems. Spine (Phila Pa 1976) 2006;31(19 Suppl):S119–S125. doi: 10.1097/01.brs.0000232709.48446.be. [DOI] [PubMed] [Google Scholar]
- 23.Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976) 2009;34:785–791. doi: 10.1097/BRS.0b013e31819d0c86. [DOI] [PubMed] [Google Scholar]
- 24.Smith JS, Klineberg E, Schwab F, Shaffrey CI, Moal B, Ames CP, et al. Change in classification grade by the SRS-Schwab Adult Spinal Deformity Classification predicts impact on health-related quality of life measures : prospective analysis of operative and nonoperative treatment. Spine (Phila Pa 1976) 2013;38:1663–1671. doi: 10.1097/BRS.0b013e31829ec563. [DOI] [PubMed] [Google Scholar]
- 25.Sudo H, Kaneda K, Shono Y, Iwasaki N. Selection of the upper vertebra to be instrumented in the treatment of thoracolumbar and lumbar adolescent idiopathic scoliosis by anterior correction and fusion surgery using dual-rod instrumentation : a minimum 12-year follow-up study. Spine J. 2016;16:281–287. doi: 10.1016/j.spinee.2015.08.021. [DOI] [PubMed] [Google Scholar]
- 26.Suk SI, Lee SM, Chung ER, Kim JH, Kim SS. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis : more than 5-year follow-up. Spine (Phila Pa 1976) 2005;30:1602–1609. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 27.Sun Z, Qiu G, Zhao Y, Wang Y, Zhang J, Shen J. Lowest instrumented vertebrae selection for selective posterior fusion of moderate thoracolumbar/lumbar idiopathic scoliosis : lower-end vertebra or lower-end vertebra+1? Eur Spine J. 2014;23:1251–1257. doi: 10.1007/s00586-014-3276-0. [DOI] [PubMed] [Google Scholar]
- 28.Terran J, Schwab F, Shaffrey CI, Smith JS, Devos P, Ames CP, et al. The SRS-Schwab adult spinal deformity classification : assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery. 2013;73:559–568. doi: 10.1227/NEU.0000000000000012. [DOI] [PubMed] [Google Scholar]
- 29.Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:447–455. [PubMed] [Google Scholar]
- 30.Youssef JA, Orndorff DO, Patty CA, Scott MA, Price HL, Hamlin LF, et al. Current status of adult spinal deformity. Global Spine J. 2013;3:51–62. doi: 10.1055/s-0032-1326950. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
15 year-old-girl with Group 1.
13 year-old-girl with Group 2S.
18 year-old-girl with Group 2NS.
15 year-old-girl with Group 3S.
15 year-old-girl with Group 3NS.
A: A 66-year old female with degenerative lumbar scoliosis with good sagittal balance underwent posterior spinal fusion from T10 to L5. Her sagittal balance was tolerable and her disc at L5–S1 was well-preserved before surgery. Radiographic and clinical outcomes were excellent in 3 years post operation. B: An 82-year old female with sagittal imbalance and distal junctional failure underwent posterior vertebral column resection at L1 and spinal fusion from T9 to L5. Radiographic and clinical outcomes were poor even after the reconstructive surgery.
A: A 60-year old female with degenerative lumbar kyphoscoliosis underwent anterior and posterior spinal fusion from T12 to pelvis. Her sagittal/coronal balance was nicely restored after surgery. Radiographical and clinical outcomes were excellent. B: A 74-year old female with sagittal/coronal imbalance and postoperative thoracic decompensation underwent multi-level Ponte osteotomies/prophylactic vertebroplasty at T9 and T10 and spinal instrumentation/fusion from T10 to pelvis via only posterior. Radiographical and clinical outcomes were excellent in 2 years postoperative.
A representative case requiring a pedicle subtraction osteotomy. A 71-year old female with degenerative thoracolumbar kyphosis underwent a pedicle subtraction osteotomy at L4 and 3-level Ponte osteotomies and spinal instrumentation/fusion from T3 to pelvis. Her sagittal balance was nicely restored after surgery. Radiographic and clinical outcomes were excellent in 3 years postoperative.
A 70-year old female with degenerative thoracolumbar kyphoscoliosis underwent a posterior vertebral column resection at the apex of the curve and spinal instrumentation/fusion from T9 to pelvis with prophylactic vertebroplasty. Her sagittal/coronal balance was nicely corrected after surgery. Radiographical and clinical outcomes were excellent in 2 years postoperative.