Abstract
Objective
To determine 20- and 40-week fetal outcomes following documentation of fetal cardiac activity (FCA) and intrauterine pregnancy (IUP) in women at less than 20 weeks’ gestation presenting to the emergency department (ED) with vaginal bleeding.
Design
Prospective observational cohort study.
Setting
Single-centre tertiary care ED.
Participants
Pregnant women at less than 20 weeks’ gestation presenting to the ED with vaginal bleeding.
Intervention
All study participants underwent ED point-of-care ultrasound (POCUS) to document IUP and FCA.
Main outcome measures
Prevalence of spontaneous abortion or pregnancy loss by 40 weeks’ gestational age following ED POCUS documentation of FCA or IUP in women at less than 20 weeks’ gestation.
Results
A total of 85 of 111 eligible patients were enrolled; FCA and IUP were detected in 43 (50.6%) and 54 (63.5%) participants, respectively. Participants with documented FCA on ED POCUS were less likely to experience pregnancy loss than participants without documented FCA were (5.0% vs 92.7%; Δ = 87.7%; 95% CI 71.0% to 93.7%), and participants with documented IUP were less likely to experience pregnancy loss than participants without documented IUP were (22.0% vs 93.5%; Δ = 71.5%; 95% CI 52.1% to 81.9%). Compared with radiologist-interpreted ultrasound, ED POCUS had sensitivity of 88.9% (95% CI 75.9% to 96.2%) and specificity of 100.0% (95% CI 89.6% to 100.0%) for documenting FCA, and sensitivity of 96.0% (95% CI 86.3% to 99.4%) and specificity of 93.1% (95% CI 77.2% to 99.0%) for documenting IUP.
Conclusion
In this cohort of women presenting to the ED with bleeding in the first 20 weeks of pregnancy, detection of IUP and especially FCA using POCUS performed by providers certified by the Canadian Emergency Ultrasound Society was associated with ongoing viable pregnancy at 20 and 40 weeks’ gestational age. These data might be useful for ED physicians counseling women with symptomatic early pregnancies about the chance of miscarriage after an episode of vaginal bleeding.
Résumé
Objectif
Déterminer les incidences sur le fœtus à 20 et à 40 semaines après la documentation d’une activité cardiaque fœtale (ACF) et d’une grossesse intrautérine (GIU) chez des femmes à moins de 20 semaines de gestation qui se sont présentées à l’urgence avec des saignements vaginaux.
Conception
Étude observationnelle et prospective de cohortes.
Contexte
L’urgence d’un centre de soins tertiaires.
Participantes
Des femmes enceintes à moins de 20 semaines de gestation qui se sont présentées à l’urgence avec des saignements vaginaux.
Intervention
Toutes les participantes à l’étude ont subi une échographie au point d’intervention (EGPDI) à l’urgence pour documenter la GIU et l’ACF.
Principaux paramètres à l’étude
La prévalence d’avortements spontanés ou d’interruptions de grossesse à 40 semaines d’âge gestationnel après la documentation par EGPDI de l’ACF ou de la GIU chez des femmes à moins de 20 semaines de gestation.
Résultats
Au total, 85 des 111 femmes admissibles ont participé à l’étude; une ACF et la GIU ont été détectées respectivement chez 43 (50,6 %) et 54 (63,5 %) participantes. Les participantes chez qui une ACF a été détectée par EGPDI à l’urgence ont été moins susceptibles de vivre une interruption de grossesse que celles sans ACF documentée (5,0 % c. 92,7 %; Δ = 87,7 %; IC à 95 % de 71,0 à 93,7 %), et les participantes dont la GIU a été documentée ont été moins susceptibles de vivre une interruption de grossesse par rapport à celles dont la GIU n’a pas été documentée (22,0 % c. 93,5 %; Δ = 71,5 %; IC à 95 % de 52,1 à 81,9 %). En comparaison des échographies interprétées par un radiologiste, l’EGPDI à l’urgence avait une sensibilité de 88,9 % (IC à 95 % de 75,9 à 96,2 %) et une spécificité de 100,0 % (IC à 95 % de 89,6 à100,0 %) pour documenter l’ACF et une sensibilité de 96,0 % (IC à 95 % de 86.3 à 99.4 %) et une spécificité de 93,1 % (IC à 95 % de 77,2 à 99,0 %) pour documenter la GIU.
Conclusion
Dans cette cohorte de femmes qui se sont présentées à l’urgence avec des saignements vaginaux durant les 20 premières semaines de grossesse, la détection de la GIU et surtout de l’ACF à l’aide d’une EGPDI, effectuée par des professionnels certifiés par la Société canadienne d’échographie au département d’urgence, a été associée à une grossesse viable sans interruption à 20 et à 40 semaines d’âge gestationnel. Cette information pourrait être utile aux médecins à l’urgence pour conseiller les femmes en début de grossesse symptomatique au sujet des risques d’avortement spontané après un épisode de saignements vaginaux.
Spontaneous abortion (SAB) occurs in approximately 20% of all pregnancies; 80% of these occur in the first 12 weeks of gestation.1 In Canada, emergency department (ED) and family physicians are often the first to evaluate women for complications arising in early pregnancy.2 Previous research has stated that 6% to 13% of patients presenting to a health care provider with vaginal bleeding or abdominal pain will have an ectopic pregnancy.3 Therefore, excluding ectopic pregnancy and confirming fetal viability are critical when caring for women presenting with vaginal bleeding or abdominal pain in early pregnancy.
Previous studies report that components of the clinical history such as the amount of vaginal bleeding or the location of abdominal pain are of limited value (likelihood ratio < 1.5) in the diagnosis of ectopic pregnancy, suggesting any patient with symptoms that raise suspicion of ectopic pregnancy should undergo an urgent transvaginal ultrasound (US).2 To receive a same-day, urgent transvaginal US, many patients will be sent to the ED, but even then, obtaining transvaginal US outside daytime hours is often difficult and can substantially prolong the patient’s length of stay in the ED.4
With the advent of ED point-of-care ultrasound (POCUS), patients can now undergo timely US assessment by a credentialed ED provider at the bedside and have immediate access to information about the pregnancy, such as the presence of an intrauterine pregnancy (IUP) and fetal cardiac activity (FCA), to help guide the evaluation and management. Once an ectopic pregnancy has been excluded in the ED, patients are often discharged home with appropriate outpatient follow-up.
However, there is uncertainty regarding how to counsel patients about their ongoing risk of SAB after documenting FCA in the ED. To date, only 2 retrospective studies and 1 prospective study have followed patients’ ongoing fetal viability after presentation to an ED with vaginal bleeding or abdominal pain in early pregnancy. In these studies, 10% to 30% of patients experienced SAB following documentation of either a yolk sac or FCA using POCUS in the ED or with radiologist-interpreted US.5–7
The objective of this study was to determine 20- and 40-week fetal outcomes following ED POCUS documentation of FCA and IUP in pregnant women at less than 20 weeks’ gestation presenting to the ED with vaginal bleeding. Secondary objectives were to assess the diagnostic accuracy of Canadian Emergency Ultrasound Society Independent Practitioner (CEUS-IP) emergency providers using POCUS to identify FCA and IUP compared with radiologist-interpreted transvaginal US.
METHODS
Study design and population
This was a prospective, observational cohort study conducted in the ED of an academic tertiary care hospital in Toronto, Ont, (annual census 55 000) from September 2013 to February 2014. Adult (older than 17 years) pregnant women at less than 20 weeks’ gestation (defined as less than 20 weeks since the first day of their last menstrual period) presenting to the ED with vaginal bleeding were eligible for enrolment. Triage nurses screened potential patients, and once eligibility was confirmed by the attending physician, informed written consent was obtained by trained research personnel (when available) or by the attending physician or nurse. Pregnancy was confirmed with a serum β–human chorionic gonadotropin (β-hCG) measurement for all study participants. Patients with confirmed ectopic pregnancy, missed abortion on previous imaging, or other pregnancy-related complaints without vaginal bleeding were excluded from this study. The study protocol was approved by the Mount Sinai Hospital Research Ethics Board.
Study participants underwent a focused transabdominal bedside POCUS using a SonoSite M-Turbo performed by a CEUS-IP–certified ED provider (22 emergency physicians and 1 nurse practitioner). Participants either had a same-day radiologist-interpreted transvaginal US or returned as outpatients for follow-up transvaginal US in the radiology department within 72 hours of ED discharge. An IUP was defined by CEUS-IP ED providers and radiologists as the identification of a yolk sac or fetal pole inside the uterus.
A trained research team member (S.C.) extracted demographic and clinical parameters from paper and electronic charts using a standardized data collection tool. Patients were contacted by telephone at 20 (± 2) and 40 (± 2) weeks’ gestation to determine fetal viability. If patients could not be contacted by telephone, an electronic chart review was conducted by research assistants to determine if pregnancy outcomes were documented in the hospital electronic medical record.
Sample size calculation
Assuming a normal distribution, for pregnant women presenting to the ED with vaginal bleeding at less than 20 weeks’ gestation, we predicted the prevalence of SAB after ED POCUS detection of FCA or IUP to be approximately 30%. Using a desired precision level of 10% and a specified level of confidence of 95%, we estimated the sample size required to be 81 patients based on the following formula, where Z is the value from standard normal distribution corresponding to the desired confidence level (Z = 1.96 for 95% confidence), p is the expected prevalence of SAB, and d is the desired precision8:
Outcome measures
Our primary outcome was the prevalence of SAB or pregnancy loss by 40 weeks’ gestational age (GA) following ED POCUS documentation of FCA and IUP in pregnant women at less than 20 weeks’ gestation. Secondary outcome measures of sensitivity, specificity, positive and negative predictive values, and interrater agreement of transabdominal POCUS performed by CEUS-IP–certified ED providers were compared with transvaginal US interpreted by board-certified radiologists.
Data analyses
Data were entered into a study-specific Microsoft Excel database. Baseline continuous variables for the study cohort were described using means and SDs or medians and interquartile ranges. Proportional differences with 95% CIs were estimated using χ2 statistics as appropriate. Diagnostic accuracy (ie, sensitivity, specificity, positive and negative predictive values) with 95% CIs were calculated using standard equations from 2 × 2 contingency tables. The reference standard was the radiologist-interpreted transvaginal US. Interrater agreement for the diagnostic accuracy of ED POCUS versus radiologist-interpreted US for IUP and FCA was estimated using Cohen κ statistics. Statistical analysis was conducted using SAS software, version 9.3.
RESULTS
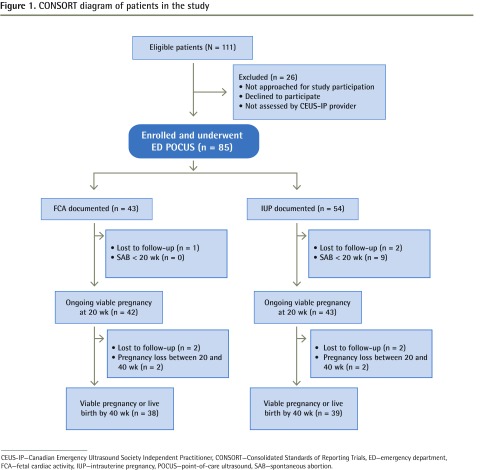
During the 6-month period, a total of 111 patients were screened for eligibility and 85 patients were enrolled (Figure 1). Characteristics of these patients are summarized in Table 1. There were 23 CEUS-IP certified ED providers (22 physicians and 1 nurse practitioner) performing ED POCUS. Six participants did not undergo subsequent radiologist-interpreted US. Fetal cardiac activity and IUP were detected in 43 (50.6%) and 54 (63.5%) participants, respectively. Table 2 shows ED POCUS and radiologist-interpreted US results stratified by serum β-hCG level. All patients with a serum β-hCG level less than 1000 IU/L reported nonviable pregnancies by 20 weeks’ GA.
Figure 1.
CONSORT diagram of patients in the study
CEUS-IP—Canadian Emergency Ultrasound Society Independent Practitioner, CONSORT—Consolidated Standards of Reporting Trials, ED—emergency department, FCA—fetal cardiac activity, IUP—intrauterine pregnancy, POCUS—point-of-care ultrasound, SAB—spontaneous abortion.
Table 1.
Patient characteristics: N = 85.
| CHARACTERISTICS | VALUE |
|---|---|
| Mean (SD) age, y | 33.8 (5.2) |
| Age group, n (%) | |
| • 20–24 y | 3 (3.5) |
| • 25–29 y | 12 (14.1) |
| • 30–34 y | 35 (41.2) |
| • 35–39 y | 24 (28.2) |
| • ≥ 40 y | 11 (12.9) |
| Mean (SD) gestational age, wk | 9.5 (2.7) |
| Mean (SD) serum β-hCG, IU/L | 43 882 (45 891) |
| Timing of radiologist-interpreted US after ED visit, n (%) | |
| • ≤ 24 h | 63 (74.1) |
| • 24–48 h | 10 (11.8) |
| • > 48–72 h | 6 (7.1) |
| • Did not have radiologist-interpreted US | 6 (7.1) |
ED—emergency department, hCG—human chorionic gonadotropin, US—ultrasound.
Table 2.
Results of ED POCUS and radiologist-interpreted US for study participants who underwent both, stratified by serum β-hCG level
| SERUM β-HCG LEVEL, IU/L | N | IUPs DOCUMENTED BY ED POCUS, N (%) | FCA DOCUMENTED BY ED POCUS, N (%) | IUPs DOCUMENTED BY RADIOLOGIST-INTERPRETED US, N (%) | FCA DOCUMENTED BY RADIOLOGIST-INTERPRETED US, N (%) |
|---|---|---|---|---|---|
| < 1000 | 10 | 1 (10.0) | 0 (0.0) | 1 (10.0) | 0 (0.0) |
| 1000–5000 | 12 | 2 (16.7) | 0 (0.0) | 1 (8.3) | 0 (0.0) |
| 5001–10 000 | 9 | 3 (33.3) | 0 (0.0) | 2 (22.2) | 1 (11.1) |
| 10 001–30 000 | 5 | 2 (40.0) | 1 (20.0) | 3 (60.0) | 2 (40.0) |
| 30 001–50 000 | 11 | 10 (90.9) | 9 (81.8) | 11 (100.0) | 11 (100.0) |
| > 50 000 | 32 | 32 (100.0) | 30 (93.8) | 32 (100.0) | 30 (93.8) |
| Total | 79 | 50 (63.3) | 40 (50.6) | 50 (69.4) | 44 (55.7) |
ED—emergency department, FCA—fetal cardiac activity, hCG—human chorionic gonadotropin, IUP—intrauterine pregnancy, POCUS—point-of-care ultrasound, US—ultrasound.
Fetal cardiac activity
By 20 weeks’ gestation, 1 patient with FCA on ED POCUS was lost to follow-up and excluded from the outcome analysis. Of the 42 remaining patients with FCA on ED POCUS, none experienced SAB at 20 weeks’ gestation (Figure 1). By 40 weeks’ gestation, 2 additional patients were lost to follow-up, leaving 40 in our analysis. Of those, 2 (5.0%) experienced pregnancy loss (1 termination, 1 fetal loss at 22 weeks). Of the 42 patients without FCA on ED POCUS, 1 patient was lost to follow-up and 38 of 41 (92.7%) experienced SAB or pregnancy loss by 40 weeks’ gestation. Participants who had documented FCA on ED POCUS were less likely to experience pregnancy loss than participants without documented FCA were (5.0% vs 92.7%; Δ = 87.7%; 95% CI 71.0% to 93.7%).
Intrauterine pregnancy
By 20 weeks’ gestation, 2 patients with IUP on ED POCUS were lost to follow-up and excluded from analysis. Of the 52 remaining patients with IUP on ED POCUS, 9 (17.3%) experienced SAB at 20 weeks’ gestation (Figure 1). By 40 weeks’ gestation, 2 additional patients were lost to follow-up, leaving 50 in our analysis. Of those, 11 (22.0%) experienced pregnancy loss. Of the 31 patients without IUP on ED POCUS, 29 (93.5%) experienced SAB or pregnancy loss by 40 weeks’ gestation. Participants who had documented IUP on ED POCUS were less likely to experience pregnancy loss than participants without documented IUP were (22.0% vs 93.5%; Δ = 71.5%; 95% CI 52.1% to 81.9%).
There were 3 patients with ectopic pregnancies diagnosed in this cohort. None of these patients had IUPs documented on ED POCUS, and the 3 ectopic pregnancies were visualized on subsequent radiologist-interpreted US.
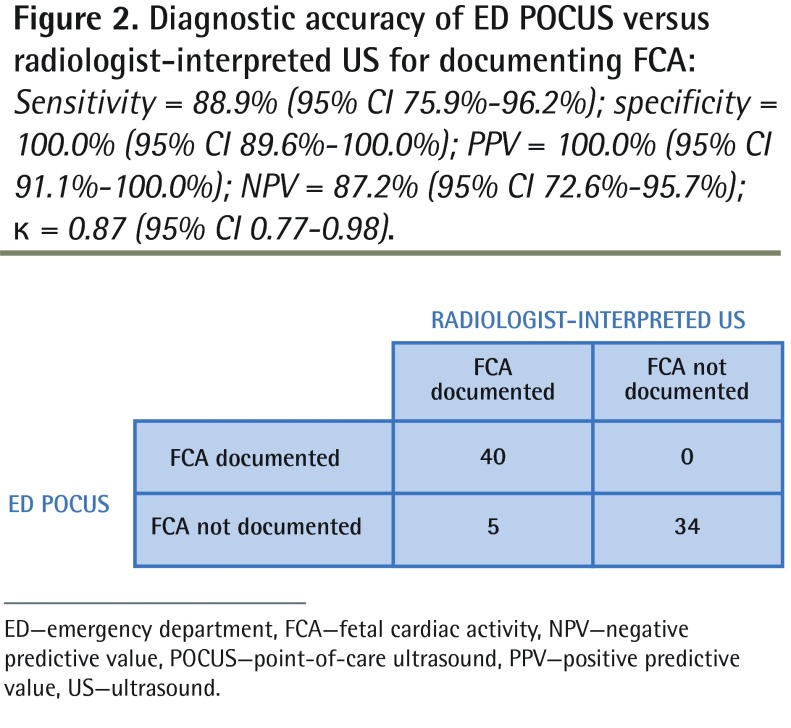
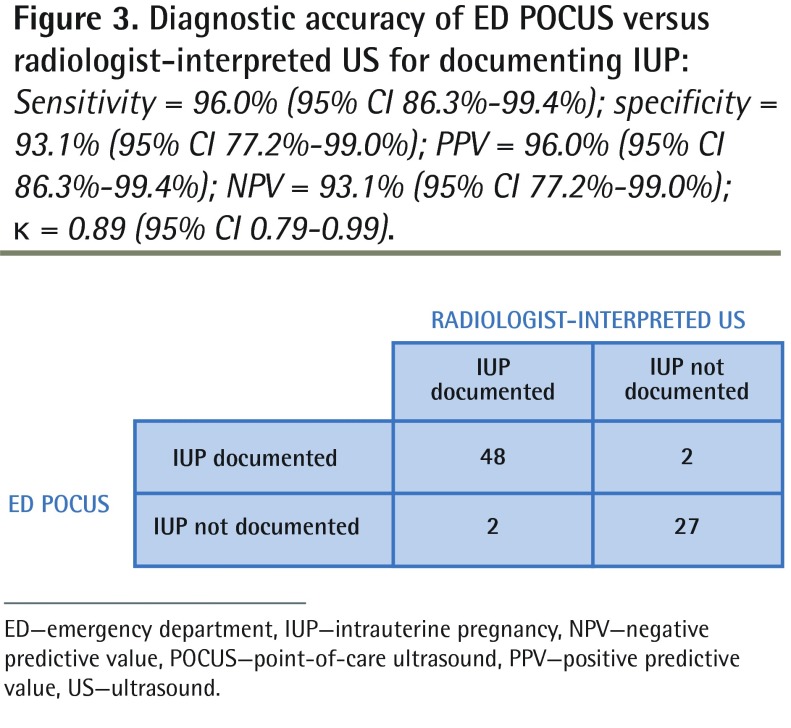
Diagnostic accuracy
The diagnostic accuracy of ED POCUS compared with radiologist-interpreted US for detecting FCA and IUP is shown in Figures 2 and 3, respectively. In this cohort, 2 patients were documented as having IUP in the ED but subsequently had radiologist-interpreted US documenting SAB within 72 hours of discharge. In both instances the radiologist documented a gestational sac and intrauterine contents consistent with SAB. More important, these were not ectopic pregnancies.
Figure 2.
Diagnostic accuracy of ED POCUS versus radiologist-interpreted US for documenting FCA: Sensitivity = 88.9% (95% CI 75.9%–96.2%); specificity = 100.0% (95% CI 89.6%–100.0%); PPV = 100.0% (95% CI 91.1%–100.0%); NPV = 87.2% (95% CI 72.6%–95.7%); κ = 0.87 (95% CI 0.77–0.98).
ED—emergency department, FCA—fetal cardiac activity, NPV—negative predictive value, POCUS—point-of-care ultrasound, PPV—positive predictive value, US—ultrasound.
Figure 3.
Diagnostic accuracy of ED POCUS versus radiologist-interpreted US for documenting IUP: Sensitivity = 96.0% (95% CI 86.3%–99.4%); specificity = 93.1% (95% CI 77.2%–99.0%); PPV = 96.0% (95% CI 86.3%–99.4%); NPV = 93.1% (95% CI 77.2%–99.0%); κ = 0.89 (95% CI 0.79–0.99).
ED—emergency department, IUP—intrauterine pregnancy, NPV—negative predictive value, POCUS—point-of-care ultrasound, PPV—positive predictive value, US—ultrasound.
DISCUSSION
In this prospective study evaluating fetal outcomes of women at 20 and 40 weeks’ gestation, patients with documented FCA on ED POCUS were less likely to experience pregnancy loss than participants without documented FCA. Similar results were found for the detection of IUP by ED POCUS.
These results are consistent with previously published studies suggesting that visualization of FCA might provide more accurate information for counseling in the ED for this patient population compared with identification of IUP alone.5–7,9 In a 2006 prospective study of 370 women presenting to an obstetric clinic with first-trimester bleeding and documented FCA, Poulose et al reported an overall SAB rate of 11.1%.9 A recent prospective cohort study of 71 ED patients with first-trimester complaints found the rate of SAB after 30 days of follow-up to be 14.8% (95% CI 8.7% to 23.9%) after documented FCA on US during the ED visit.5 We included patients beyond their first-trimester (up to 20 weeks’ gestation), possibly explaining why we found a lower proportion of pregnancy loss in our cohort.
Participants with documented FCA on ED POCUS were less likely to experience pregnancy loss than were participants with IUP alone. In a retrospective cohort study, Hessert and Juliano sought to determine fetal outcomes for women following ED evaluation for first-trimester pelvic pain or vaginal bleeding and found 30% of women with documented IUP in the ED experienced fetal loss by 20 weeks’ gestation.6 Additionally, Juliano and Sauter performed a retrospective analysis of consecutive ED patients with indeterminate findings on transvaginal US performed by an emergency physician or through the radiology department during their ED visit and found an 89.2% rate of fetal loss.7 These results are consistent with our study’s findings, suggesting the absence of an IUP in the setting of first-trimester vaginal bleeding or abdominal pain is indicative of poor fetal outcomes. One limitation of ED POCUS, however, is the lack of characterization of the quality of the yolk sac and embryonic plate, both indicators that affect the occurrence of SAB that are usually included in reports by radiologists.
The CEUS-IP–certified providers in our study were able to accurately document FCA and rule out ectopic pregnancy without false reassurance of fetal viability or location. Our findings are in agreement with previous systematic reviews that have summarized the use of emergency physician ultrasonography in the evaluation of patients at risk of ectopic pregnancy.10,11 The results of a meta-analysis by Stein et al, incorporating 10 studies with a total of 2057 patients, reported high sensitivity (99.3%, 95% CI 96.6% to 100%) and negative predictive value (99.9%, 95% CI 99.6% to 100%) in the use of bedside ultrasonography by emergency physicians as a diagnostic test for ectopic pregnancy.10 In a systematic review by McRae et al, ED targeted ultrasonography by experienced ED US providers to exclude ectopic pregnancy was reported to be “excellent,” with specificity exceeding 97% and sensitivity ranging from 71% to 100%. However, for inexperienced ED US providers, the specificity to exclude ectopic pregnancy was less robust (from 86%).11 The authors concluded that ED targeted ultrasonography reduces the frequency of missed ectopic pregnancies, decreases time to surgery for ectopic pregnancy, shortens the length of stay for patients with normal pregnancies, and might be more cost-effective than diagnostic strategies requiring formal ultrasonography.11 The results of this study further affirm ED POCUS can be used to safely exclude ectopic pregnancy when an IUP is documented. Once ectopic pregnancy is excluded, emergent radiologist-interpreted US can be deferred, and the patient can undergo appropriate, timely follow-up.
Increasingly, POCUS is becoming an extension of the physical examination to answer highly focused clinical questions in a binary manner quickly, affecting bedside patient care. For this reason, POCUS is receiving growing interest in office-based family medicine.12 Family physicians provide most first-trimester pregnancy care in Canada and are often first to evaluate early pregnancy complications. Particularly in resource-limited, rural areas, small numbers of family physicians are using POCUS to defer costly, urgent transfers to larger centres where a radiologist is available to exclude ectopic pregnancy. Future studies should evaluate the use of POCUS in these clinical practices.
Limitations
There are several limitations to this study. It was conducted in a single-centre tertiary care institution with a high-acuity obstetric care program, and the results might not be generalizable to other settings. Additionally, patient characteristics such as the amount of vaginal bleeding or history of previous SAB were not collected nor adjusted for in the analysis. This study was a descriptive, observational cohort study and was not designed to identify independent risk factors for SAB and fetal loss. Fetal loss, particularly beyond the first trimester, is a multifactorial and complex issue, with numerous maternal and fetal factors modulating fetal survival. Finally, it should be noted the US transducers and anatomic location of assessment (transabdominal for ED providers vs transvaginal for radiologist-interpreted US) compared in this study are not equivalent. Transvaginal assessments are more likely to produce superior visualization of intrauterine contents.13 Notwithstanding the differences between these methods, the diagnostic accuracy of transabdominal ED POCUS was found to be excellent in this study.
Conclusion
In this cohort of women presenting to the ED with bleeding in the first 20 weeks of pregnancy, detection of IUP and especially FCA on POCUS performed by CEUS-IP–certified providers was associated with ongoing viable pregnancy at 20 and 40 weeks’ GA. These data might be useful for ED physicians counseling women with symptomatic early pregnancies about the chance of SAB after an episode of vaginal bleeding.
EDITOR’S KEY POINTS
Availability of point-of-care ultrasound (POCUS) in the emergency department (ED) has improved access to timely ultrasound assessment for pregnant women presenting with vaginal bleeding; however, there is uncertainty about how to counsel patients about their ongoing risk of spontaneous abortion after documenting fetal cardiac activity (FCA) or intrauterine pregnancy (IUP).
The objective of this study was to determine 20- and 40-week fetal outcomes following ED POCUS documentation of FCA and IUP in women at less than 20 weeks’ gestation presenting to the ED with vaginal bleeding. The authors found that detection of IUP and FCA on POCUS performed by certified providers was associated with ongoing viable pregnancy at 20 and 40 weeks’ gestation. Participants with documented FCA were less likely to experience pregnancy loss than were participants with documented IUP alone.
The diagnostic accuracy of ED POCUS in this study was excellent compared with radiologist-interpreted ultrasound, suggesting ED POCUS by experienced providers can be safely used to rule out ectopic pregnancy without false reassurance of fetal viability.
POINTS DE REPÈRE DU RÉDACTEUR
L’accessibilité à une échographie au point d’intervention (EGPDI) à l’urgence a amélioré la possibilité d’une évaluation échographique en temps opportun chez des femmes enceintes ayant des saignements vaginaux; toutefois, la façon de conseiller les patientes au sujet de leur risque constant d’un avortement spontané après avoir confirmé l’activité cardiaque fœtale (ACF)ou la grossesse intrautérine (GIU) n’a pas été déterminée.
Cette étude avait pour objectif de déterminer les incidences sur le foetus à 20 et à 40 semaines après la documentation par EGPDI de l’ACF et de la GIU dans les cas de femmes à moins de 20 semaines de gestation qui se sont présentées à l’urgence avec des saignements vaginaux. Les auteurs ont constaté que la détection de la GIU et de l’ACF par EGPDI effectuée par des professionnels certifiés était associée avec une grossesse viable sans interruption à 20 et à 40 semaines de gestation. Les patientes chez qui l’ACF a été documentée ont été moins susceptibles de vivre une interruption de grossesse par rapport aux participantes chez qui seule la GIU avait été documentée.
L’exactitude diagnostique de l’EGPDI dans cette étude était excellente en comparaison de celle d’une échographie interprétée par un radiologiste, ce qui fait valoir qu’une EGPDI effectuée par des professionnels expérimentés peut être utilisée en toute sécurité pour exclure la possibilité d’une grossesse ectopique sans fausse sécurité quant à la viabilité fœtale.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Dr Varner conceived the study idea, designed the study protocol, and completed data analysis. Dr Balaban performed study participant follow-up. Ms McLeod assisted with data analysis. Dr Borgundvaag assisted with study protocol design. Ms Carver performed study enrolment and data collection. All authors contributed to manuscript preparation and have given approval for its submission.
Competing interests
None declared
References
- 1.Everett C. Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice. BMJ. 1997;315(7099):32–4. doi: 10.1136/bmj.315.7099.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.College of Family Physicians of Canada . Family medicine maternity care: implications for the future. Mississauga, ON: College of Family Physicians of Canada; 2009. [Google Scholar]
- 3.Barnhart KT. Clinical practice. Ectopic pregnancy. N Engl J Med. 2009;361(14):379–87. doi: 10.1056/NEJMcp0810384. [DOI] [PubMed] [Google Scholar]
- 4.Shih CH. Effect of emergency physician–performed pelvic sonography on length of stay in the emergency department. Ann Emerg Med. 1997;29(3):348–52. doi: 10.1016/s0196-0644(97)70346-9. [DOI] [PubMed] [Google Scholar]
- 5.Mallin M, Dawson M, Schroeder E, Hatch B, Jackson I, Ahern M, et al. Prospective outcomes of pregnant ED patients with documented fetal cardiac activity on ultrasound. Am J Emerg Med. 2012;30(3):472–5. doi: 10.1016/j.ajem.2010.12.023. Epub 2011 Feb 18. [DOI] [PubMed] [Google Scholar]
- 6.Hessert MJ, Juliano ML. Fetal loss in symptomatic first-trimester pregnancy with documented yolk sac intrauterine pregnancy. Am J Emerg Med. 2012;30(3):399–404. doi: 10.1016/j.ajem.2010.12.021. Epub 2011 Feb 18. [DOI] [PubMed] [Google Scholar]
- 7.Juliano ML, Sauter BM. Fetal outcomes in first trimester pregnancies with an indeterminate ultrasound. J Emerg Med. 2012;43(3):417–22. doi: 10.1016/j.jemermed.2011.05.021. Epub 2011 Feb 18. [DOI] [PubMed] [Google Scholar]
- 8.Daniel WW. Biostatistics: a foundation for analysis in the health sciences. 7th ed. New York, NY: John Wiley & Sons; 1999. [Google Scholar]
- 9.Poulose T, Richardson R, Ewings P, Fox R. Probability of early pregnancy loss in women with vaginal bleeding and singleton live fetus on ultrasound scan. J Obstet Gynaecol. 2006;26(8):782–4. doi: 10.1080/01443610600984412. [DOI] [PubMed] [Google Scholar]
- 10.Stein JC, Wang R, Adler N, Boscardin J, Jacoby VL, Won G, et al. Emergency physician ultrasonography for evaluating patients at risk for ectopic pregnancy: a meta-analysis. Ann Emerg Med. 2010;56(6):674–83. doi: 10.1016/j.annemergmed.2010.06.563. Epub 2010 Sep 15. [DOI] [PubMed] [Google Scholar]
- 11.McRae A, Murray H, Edmunds M. Diagnostic accuracy and clinical utility of emergency department targeted ultrasonography in the evaluation of first-trimester pelvic pain and bleeding: a systematic review. CJEM. 2009;11(4):355–64. doi: 10.1017/s1481803500011416. [DOI] [PubMed] [Google Scholar]
- 12.Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can Fam Physician. 2012;58:e172–8. Available from: www.cfp.ca/content/58/3/e172.full.pdf+html. Accessed 2016 May 27. [PMC free article] [PubMed] [Google Scholar]
- 13.Canadian Emergency Ultrasound Society . Recommendations and standards. Canadian Emergency Ultrasound Society; Available from: www.ceus.ca/about-ultrasound-society/uses-ed-us. Accessed 2015 Mar 15. [Google Scholar]