Abstract
Background
Identifying the aetiological agent of atypical pneumonia in human can sometimes be a tedious process, especially in cases where Mycoplasma pneumoniae, Legionella species and Chlamydia pneumoniae are ruled out. In such cases, a correct anamnesis of the patient is basic to clarify which pathogens might have produced the infection. For this reason, health professionals including veterinarians and laboratory personnel working with zoonotic pathogens should keep their doctors informed.
Case presentation
A human case of atypical pneumonia linked to Chlamydia abortus is reported. A 47-year-old male, a veterinarian researcher into chlamydiae, developed respiratory symptoms, breathing problems and high fever. Serological analyses ruled out the involvement of several respiratory pathogens, such as M. pneumoniae, Legionella pneumophila, Rickettsia conorii and C. pneumoniae, and Chlamydia abortus was identified as the possible aetiological agent of the infection. The isolation of C. abortus from the patient’s sputum and subsequent molecular analysis confirmed the presence of this microorganism.
Conclusion
As far as we know, although C. abortus has not been previously described as capable of causing pneumonia in humans, this is the first reported case of atypical pneumonia in which C. abortus is thought to have played an aetiological role.
Keywords: Chlamydia abortus, Human, Atypical pneumonia, Zoonoses, OEA
Background
The term ‘atypical pneumonia’ is applied to pneumonia caused by Mycoplasma pneumoniae, Legionella species and Chlamydia pneumoniae, although some authors argue that other emerging atypical pneumonia pathogens should be included in the list [1].
The Family Chlamydiaceae includes 11 species grouped in a single genus, Chamydia [2]. These are Gram-negative, obligate intracellular bacteria with a unique bi-phasic developmental cycle, in which a small extracellular infectious elementary body (EB) and a metabolically active reticulate body (RB) play special roles. Chlamydial infections cause clinically and epidemiologically important diseases both in humans and in animals [3]. Respiratory tract infections and atypical pneumonia in humans are commonly associated with Chlamydia pneumoniae infections [4]. C. psittaci is the causative agent of psittacosis or ornithosis in birds. This disease is a zoonosis transmitted through aerosols that especially affects workers who come into contact with domestic poultry or wildfowl. The clinical course of this infection in humans starts with influenza-like symptoms, progresses as atypical pneumonia and may lead to systemic infections with serious complications in internal organs [5].
C. abortus infection is also considered as a zoonotic pathogen with serious effects for infected pregnant women and unborn children [6]. This bacterium is associated with enzootic abortion in small ruminants (OEA), and can also infect other animal species such as pigs, cattle and wild ungulates [3, 5, 7, 8]. To our knowledge, this is the first time that C. abortus has been reported as the likely causative agent of atypical pneumonia in humans.
Case Presentation
A 47-year-old male reported a seven day history of influenza-like symptoms, including general malaise, chills, dry cough, chest-pain, shortness of breath, and temperatures of up to 39.5 °C, which did not respond to paracetamol or ibuprofen. The patient worked as a veterinary researcher in a laboratory where experimental intranasal infections with C. abortus were developed in sheep. The patient carried out these infections using a suspension of C. abortus sprayed into both nostrils with a multi-dose spray pump, as described previously [9]. Ten days after the sheep infections, the patient showed the first symptoms.
The initial medical examination identified crackling sounds during lung auscultation. A chest x-ray showed areas of consolidation of the lower lobe of the left lung, indicating a pan-lobar pneumonia (Fig. 1). Blood and biochemical tests revealed a non-significant increase in mean corpuscular hemoglobin (MCH), as well as a slight increase in urea and creatinine levels: 50.3 and 1.3 mg/dl respectively. By contrast, the C-reactive protein level was very high, 8.9 mg/dl, normal values being <0.5 mg/dl. These high values suggested a bacterial infection rather than a viral infection, in which case the values would be lower [10].
Fig. 1.
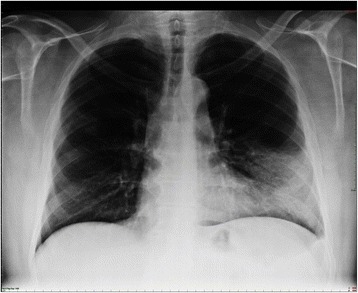
Chest x-ray of the patient with dense infiltration in the left lower lobe
Serological analyses with several ELISA tests (all of them from Vircell Microbiologist, Granada, Spain) using specific IgG and IgM monoclonal antibodies (MoAb) were negative against Mycoplasma pneumoniae, Legionella pneumophila (serogroup 1-7), Rickettsia conorii and Chlamydia pneumoniae.
Due to the suspicion of C. abortus infection, serum and sputum samples from the patient were sent to a laboratory at the Animal Health Department of the Murcia University (Spain) for further analysis.
A C. abortus-specific serological test, performed using an ELISA kit (ID Screen Chlamydophila abortus indirect multi-species, IDvet), revealed high IgM and IgG optical densities (OD) in the serum samples (Table 1). The serum samples were tested with a peroxidase-conjugated anti-human IgG or IgM (Sigma), and the OD were determined (DigiScan with DigiWin Software, ASYS Hitech). In addition, two serum samples from asymptomatic work colleagues were analyzed with the same ELISA kit. As might be expected, both colleagues showed antibody production against C. abortus, but with a lower OD than the patient, especially for IgM production (Table 1). It was therefore assumed that antibody production on the part of the patient was due to a clinical episode and not to a progressive sensitization to C. abortus.
Table 1.
IgG and IgM levels against C. abortus in serum samples from the patient and two asymptomatic work colleagues (Researcher 1 and Researcher 2) expressed as optical densities (OD) by ELISA
| IgG (OD) | IgM (OD) | |
|---|---|---|
| Patient | 1.746 | 0.627 |
| Researcher 1 | 1.235 | 0.137 |
| Researcher 2 | 0.866 | 0.112 |
C. abortus was isolated from the sputum using a McCoy cell monolayer, as described previously [11]. Positive cell cultures were identified by an immunofluorescence assay using the C. abortus-specific anti-MOMP FA2H10 MoAb [12]. The MoAb was produced using BALB/c mice and purified by immunoafinity, and was chosen because it is specific for an oligomer of the outer membrane protein of C. abortus (named as C. psittaci, serotype 1).
C. abortus DNA was detected in the sputum sample and also in the cell culture isolates by PCR analysis. Total DNA was extracted with a commercial kit (DNeasy tissue kit, Qiagen) and was used as a template for a C. abortus-specific PCR, using primers pmp-F (5′-CTC ACC ATT GTC TCA GGT GGA-3′) and pmp-R821 (5′-ACC GTA ATG GGT AGG AGG GGT-3′) for the target gen pmp 90/91 [13], which allow the sensitive amplification of 821-bp length DNA fragments. In order to confirm the specific presence of C. abortus in the sputum sample as well as in the cell isolates, the amplicons were sequenced (ABI Prism 3130). The PCR products showed 100 % identity to the C. abortus AB7 strain sequence obtained using MEGA5 software and BLAST® program. This C. abortus strain was the same strain as that used in the experimental infections in ewes carried out by the patient [9].
Once diagnosed, the patient was treated with antibiotics (levofloxacin, initial intravenous dose of 500 and 500 mg orally every 24 h for 10 days; and clarithromycin 500 mg every 12 h for 10 days), mucolytic carbocysteine lysine (2.7 g orally every 24 h), glucocorticoids (beclomethasone dipropionate inhaler 100 μg every 12 h) and non-steroidal anti-inflammatory drugs (paracetamol 1 g orally in case of fever or pain). This treatment resulted in successful recovery of the patient in 2 weeks without sequels.
Discussion
Atypical pneumonia caused by Chlamydia species, mainly C. pneumoniae and C. psittaci infections, has frequently been commonly reported in human patients [1]. In Spain, published data revealed the presence of C. pneumoniae in 14.3 % of pneumonia inpatients and in 25 % of outpatient cases, while C. psittaci was detected in 0.7 % of hospitalized pneumonia cases [14]. However, there is no previous published evidence that C. abortus can infect the human respiratory tract. Previous published research involving experimental infections with C. abortus has identified the ability of this pathogen to cause pulmonary disease in animal species such as sheep [9, 15], calves [16] and mice [17]. The detection of C. abortus in a broncho-alvolar lavage (BAL) would have been decisive to firmly confirm the etiological agent of the process. However, although this procedure was not performed, the findings observed in this report may suggest the role of C. abortus as the aetiological agent in this case of human pneumonia.
C. abortus is typically associated with abortive disorders in small ruminants and other animal species [3, 7, 8]. It is also known as a zoonotic agent, affecting pregnant women who have been in contact with infected animals [6, 18]. Therefore, farmers, veterinarians and other professionals who may come into contact with chlamydia should be alert when managing vaginal discharges, placentas from aborting females or aborted fetuses because of the risk of oronasal entry of C. abortus.
Marrie et al. [1] reviewed the role of atypical pathogens in community-acquired pneumonia and categorized new emerging atypical pneumonia agents. The present report suggests that C. abortus should be included within this group and should be taken into account for differential diagnoses in respiratory patients with a history of contact with aborted sheep or goats or their afterbirth.
Human chlamydial pneumonia is not usually a life-threatening condition and patients, following correct treatment, usually recover. Nevertheless, they should be closely monitored because chlamydiae can cause serious complications in internal organs after systemic infections [5, 18]. Treatments are similar for all chlamydial infections. So, in the present case, broad-spectrum antibiotic, mucolytic and glucocorticoid treatment led to a successful recovery with no pulmonary sequels.
Conclusions
In summary, the first suspected case of C. abortus zoonotic respiratory infection is reported, whereby, instead of being associated with reproductive problems, it is described as the probable causative agent of human atypical pneumonia. So, veterinarians, veterinary laboratory personnel, and public health officials should be aware of possible pulmonary infection due to C. abortus aerosol inhalation.
Abbreviations
BAL, broncho-alvolar lavage; DNA, deoxyribonucleic acid; EB, elementary body; ELISA, enzyme like immunoabsorbent assay; IgG, immunoglobulin G; IgM, immunoglobulin M; MCH, mean corpuscular hemoglobin; MoAb, monoclonal antibodies; MOMP, major outer membrane protein; OD, optical densities; OEA, ovine enzootic abortion; PCR, polimerase chain reaction; RB, reticulate body
Acknowledgments
We thank the professional medical from the Molina Hospital (Molina de Segura, Murcia, Spain), particularly Dr J.A. López-Morata, for their contribution in this case report.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Authors’ contribution
NO was in charge of molecular biology analyses and drafted the manuscript, JS and FC were in charge of ELISA tests, JS, MRC and AJB contributed in the design and final revision of the manuscript, MCG and AM were in charge of cellular culture studies, DA and LDR supervised the case and helped NO in the decision making. The authors read and approved the final version of this manuscript.
Competing interest
None of the authors of this paper has a financial or personal relationship with other people or organisations that could inappropriately influence or bias the content of the paper.
Consent for publication
The authors have the informed consent form the patient, who gave permission for information to be published in Irish Veterinary Journal.
Ethics approval and consent to participate
Not applicable. As this is a case report and not an experimental study, an Ethics committee approval was not necessary.
References
- 1.Marrie TJ, Costain N, La Scola B, Patrick W, Forgie S, Xu Z, McNeil SA. The role of atypical pathogens in community-acquired pneumonia. Semin Respir Cri Care Med. 2012;33:244–56. doi: 10.1055/s-0032-1315636. [DOI] [PubMed] [Google Scholar]
- 2.Sachse K, Bavoil PM, Kaltenboeck B, Stephens RS, Kuo CC, Rosselló-Móra R, Horn M. Emendation of the family chlamydiaceae: proposal of a single genus, chlamydia, to include all currently recognized species. Syst Appl Microbiol. 2015;38:99–103. doi: 10.1016/j.syapm.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 3.Longbottom D, Coulter LJ. Animal chlamydioses and zoonotic implications. J Comp Path. 2003;128:217–44. doi: 10.1053/jcpa.2002.0629. [DOI] [PubMed] [Google Scholar]
- 4.Choroszy-Król I, Frej-Mądrzak M, Hober M, Sarowska J, Jama-Kmiecik A. Infections caused by Chlamydophila pneumoniae. Adv Clin Exp Med. 2014;23:123–6. doi: 10.17219/acem/37035. [DOI] [PubMed] [Google Scholar]
- 5.Rohde G, Straube E, Essig A, Reinhold P, Sachse K. Chlamydial zoonoses. Dtsch Arztebl Int. 2010;107:174–80. doi: 10.3238/arztebl.2010.0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pospischil A, Thoma R, Hilbe M, Grest P, Zimmermann D, Gebbers JO. Abortion in humans caused by Chlamydophila abortus (Chlamydia psittaci serovar 1) Schweiz Arch Tierheilkd. 2002;144:463–6. doi: 10.1024/0036-7281.144.9.463. [DOI] [PubMed] [Google Scholar]
- 7.Salinas J, Ortega N, Borge C, Rangel MJ, Carbonero A, Perea A, Caro MR. Abortion associated with Chlamydia abortus in extensively reared Iberian sows. Vet J. 2012;194:133–4. doi: 10.1016/j.tvjl.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Salinas J, Caro MR, Vicente J, Cuello F, Reyes-García AR, Buendía AJ, Rodolakis A, Gortázar C. High prevalence of antibodies against Chlamydiaceae and Chlamydophila abortus in wild ungulates using two “in house” blocking-ELISA tests. Vet Microbiol. 2009;135:46–53. doi: 10.1016/j.vetmic.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Álvarez D, Salinas J, Buendía AJ, Ortega N, del Río L, Sánchez J, Navarro JA, Gallego MC, Murcia-Belmonte A, Cuello F, Caro MR. Intratracheal infection as an efficient route for testing vaccines against Chlamydia abortus in sheep. Vet J. 2015;205:393–8. doi: 10.1016/j.tvjl.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 10.Almirall J1, Bolíbar I, Toran P, Pera G, Boquet X, Balanzó X, Sauca G, Community-Acquired Pneumonia Maresme Study Group Contribution of C-reactive protein to the diagnosis and assessment of severity of community-acquired pneumonia. Chest. 2004;125:1335–42. doi: 10.1378/chest.125.4.1335. [DOI] [PubMed] [Google Scholar]
- 11.Buendía AJ, de Oca Montes R, Navarro JA, Sánchez J, Cuello F, Salinas J. Role of polymorphonuclear neutrophils in a murine model of Chlamydia psittaci-induced abortion. Infect Immun. 1999;67:2110–6. doi: 10.1128/iai.67.5.2110-2116.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Sa C, Souriau A, Bernard F, Salinas J, Rodolakis A. An oligomer of the major outer membrane protein of Chlamydia psittaci is recognized by monoclonal antibodies which protect mice from abortion. Infect Immun. 1995;63:4912–6. doi: 10.1128/iai.63.12.4912-4916.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berri M, Rekiki A, Boumedine KS, Rodolakis A. Simultaneous differential detection of Chlamydophila abortus, Chlamydophila pecorum and Coxiella burnetii from aborted ruminant’s clinical samples using multiplex PCR. BMC Microbiol. 2009;9:130. doi: 10.1186/1471-2180-9-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Almirall J, Boixeda R, Bolibar I, Bassa J, Sauca G, Vidal J, Serra-Prat M, Balanzó X. Differences in the etiology of community-acquired pneumonia according to site of care: a population-based study. Respir Med. 2007;101:2168–75. doi: 10.1016/j.rmed.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 15.Longbottom D, Livingstone M, Maley S, Van der Zon A, Rocchi M, Wilson K, Wheelhouse N, Dagleish M, Aitchison K, Wattegedera S, Nath M, Entrican G, Buxton D. Intranasal infection with Chlamydia abortus induces dose-dependent latency and abortion in sheep. PLoS One. 2013;8:e57950. doi: 10.1371/journal.pone.0057950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jaeger J, Liebler-Tenorio E, Kirschvink N, Sachse K, Reinhold P. A clinically silent respiratory infection with Chlamydophila spp. in calves is associated with airway obstruction and pulmonary inflammation. Vet Res. 2007;38:711–28. doi: 10.1051/vetres:2007027. [DOI] [PubMed] [Google Scholar]
- 17.Buendía AJ, Nicolás L, Ortega N, Gallego MC, Martínez CM, Sánchez J, Caro MR, Navarro JA, Salinas J. Characterization of a murine model of intranasal infection suitable for testing vaccines against Chlamydophila abortus. Vet Immunol Immunopathol. 2007;115:76–86. doi: 10.1016/j.vetimm.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 18.Walder G, Hotzel H, Brezinka C, Gritsch W, Tauber R, Würzner R, Ploner F. An unusual cause of sepsis during pregnancy: recognizing infection with Chlamydophila abortus. Obstet Gynecol. 2005;106:1215–7. doi: 10.1097/01.AOG.0000161060.69470.9c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


