Abstract
Plain abdominal radiographs remain an important aid for clinicians in the diagnosis of gastrointestinal perforation, especially in neonates and very sick children where clinical features of peritonitis may not be as prominent. Suggestive radiographic features are not always very obvious, especially when taken in the supine position and may lead to delayed or missed diagnosis. Through a pictorial review of plain radiographs, this article highlights a number of documented features of gastrointestinal perforation on X-ray in the paediatric setting, which increases the accuracy of diagnosis.
Key words: Children, perforation, pneumoperitoneum, radiograph, signs
INTRODUCTION
Gastrointestinal perforation is common in children and can result from many different underlying disorders. It usually, require prompt surgical intervention. Clinical signs of peritonitis (tenderness, guarding, and rebound tenderness) are not reliable in neonates and very sick children so radiological features are very useful when a diagnosis of gastrointestinal perforation is suspected.
The classical sub-diaphragmatic air (“air under the diaphragm”) seems to be the obvious radiographic sign most clinicians are familiar with, however it is positive in only about 55% of of patients with perforation.[1] Furthermore, the sub-diaphragmatic air is best seen in erect chest X-ray, a position that is often impracticable for sick children and neonates to assume.[2] As most plain abdominal X-rays are taken in supine position in children, identifying free air is often a challenge especially to emergency physicians and trainee surgeons[3] and diagnosis of gastrointestinal perforation can be missed or delayed when signs of pneumoperitonium are not recognized on supine radiographs. Though computed tomography is more sensitive in detecting free intra-peritoneal air,[4] plain radiography remains a very efficient, timely and cheap imaging modality. Lateral decubitus views can be very helpful when in doubt.
The diagnostic yield of plain abdominal X-rays for identifying pneumoperitoneum can be improved by careful search for other documented radiological features of free intra-peritoneal air, especially on a supine film.[5] A number of intra and extra-peritoneal radiographic signs have been described to diagnose gastrointestinal perforation. Awareness of these signs in order to make timely decisions, therefore, becomes critical in an emergency setting or in low resource regions where expert radiologist reporting may not be readily available or awaited.
A search through PubMed database was done using the following search terms and their synonyms: ‘Gastrointestinal perforation’, “radiographic signs” and “children.” Searching of libraries and articles from reference lists was also done. This showed that publications on radiographic features of peritoneal free air especially on supine view are quite few and often discussed in the context of other subjects. Furthermore, none discussed this topic with the peculiarities of children in focus. This article, therefore, provides a pictorial and concise review of X-ray signs in order to assist in making a diagnosis of gastrointestinal perforation in paediatric surgical cases. Majority of the signs are discussed in the paediatric setting, but they are also relevant to adult practice.
AIR UNDER THE DIAPHRAGM [FIGURE 1]
Figure 1.

Air under the right and left hemi-diaphragm and central tendon (Cupola sign) in a 2.5 year old following abdominal trauma
Source: Child Abuse Medical Provider Program (CHAMP)[10]
This is the first radiographic sign of pneumoperitoneum described in 1915 by Popper[6] and it is the most commonly known. Free air seen as an area of lucency can be found under the right or left hemi-diaphragm and also at the mid portion of the diaphragm trapped under the central tendon (called Cupola sign).[7] As little as 1-2 ml of air can be shown with erect chest radiograph, especially on the right.[8] In cases of massive pneumoperitoneum, free air can be seen as a continuous rim of sub-diaphragmatic lucency extending from the right to the left hemi-diaphragm called ‘continuous diaphragm sign’. This continuos diaphragm sign can also indicate pneumomediastinum however the air will be seen outlining the length of the diaphragm superiorly.[9]
LUCENCY OVER THE LIVER SHADOW [FIGURE 2]
Figure 2.

Arrow showing area of lucency over the right hemi-diaphragm obliterating the normal opacity of the liver in a neonate with perforated necrotizing enterocolitis
Source: Reproduced with permission from Rodriguez et al.[12]
The liver should be most radiopaque in the right upper part of the radiograph. An area of hyperlucency at the right upper quadrant obliterating the normal opacity of the liver is suggestive of free intraperitoneal air.[11] The lucency fades off towards the midline, and it is helpful to compare the opacities of the lateral aspect of the right upper quadrant with that of immediate right side of the midline.
TRIANGLE SIGN [FIGURE 3]
Figure 3.

Arrows showing the triangle sign in a preterm neonate with meconium ileus complicated with perforation. Air under the diaphragm (continuous diaphragm sign), Rigler sign and pneumoscrotum are also noticeable
Source: Auckland District Health Board[14]
In the normal situation, air is located within the lumen of the bowel and the outer walls of the bowel are apposed. When there is free air, the air pushes the two walls apart and creates sharp angles or “tirangles”. This is seen on supine view as air forming a triangle bounded by three bowel loops or two bowel loops and the lateral parietal peritoneum.[13] It is also referred to as ‘telltale triangle sign’.
FOOTBALL SIGN [FIGURE 4]
Figure 4.

Black arrows showing the football and Rigler signs
Source: Radiograph reproduced with permission from Prof H.J. Lee[16]
In supine position, air is displaced to the least dependent part i.e under the anterior abdominal wall. If there is a lot of free air, this is seen as an oval hyperlucency on supine radiograph that takes the shape of the American football. It signifies massive pneumoperitoneum.[15] Smaller “footballs” can be seen with lesser amount of free air.
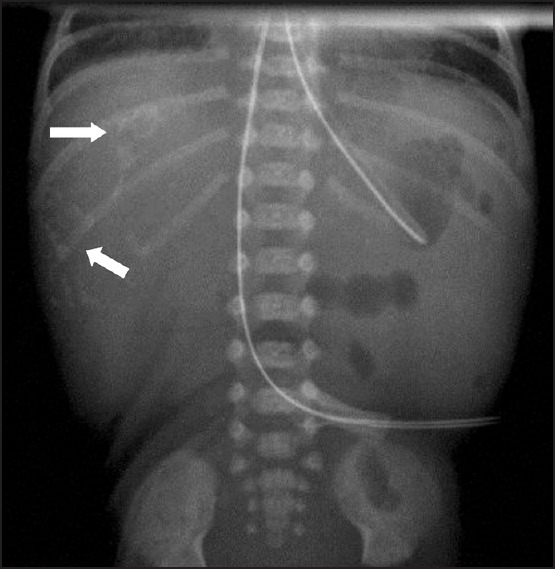
RIGLER SIGN [FIGURE 5]
Figure 5.

Arrows showing the Rigler sign in a neonate with massive pneumoperitoneum. There is also significant sub-diaphragmatic air (continuous diaphragm sign) and right upper quadrant luscency
Source: WikiRadiography[19]
In normal abdominal radiograph, air is seen within the different bowel loops separated by the walls of two loops demonstrating the standard bowel wall thickness we have come to understand. When there is air inside and outside of a single loop of bowel, it looks much thinner, the edges are crisper and it gives a characteristic appearance described by Rigler.[17] It is also known as ‘double-wall sign’ or ‘the bas-relief sign’.[18]
DOGE CAP SIGN [FIGURES 6A AND B]
Figure 6a.

Schematic diagram of the relations of the Morrison's pouch
Source: WikiRadiography[19]
Figure 6b.

Arrow showing the Doge cap sign in a neonate with perforated necrotizing enterocolitis
Source: Reproduced with permission from Brill PW, Olson SR, Winchester P. Neonatal necrotizing enterocolitis: Air in Morison pouch. Radiology 1990;174:469-71, Copyright© RSNA.[20]
This describes a collection of air in the Morrison's pouch (posterior hepatorenal space) seen on supine view as a triangular shaped lucency. It is seen at the inferio-medial aspect of the 11th rib.[6] The sign was named after the cap worn by Italian Doges, which is triangularly shaped at its top.
ACCENTUATION OF PERITONEAL LIGAMENTS [FIGURES 7A AND B]
Figure 7a.

Arrows showing the outlined falciform ligament
Source: Radiopaedia.org[21]
Figure 7b.

Arrows showing accentuated opacities of the lateral umbilical ligaments (inverted V sign). The falciform ligament and football signs are also noticeable
Source: Radiopaedia.org[21]
Air in the peritoneum can outline peritoneal folds that are normally not visible on supine plain abdominal radiographs. Signs of pneumoperitoneum that involve visualisation of ligaments include:
Falciform ligament sign: Seen as a longitudinal linear opacity outlining the falciform ligament on the right upper abdomen parallel to the right border of the spine.[3]
Inverted V sign; an outline of the two lateral umbilical ligaments. Seen as oblique linear opacities extending from the umbilicus to the pelvis. Only one of the ligaments may be visible in some cases.[6]
Urachus sign: An outline of the median umbilical ligament seen in the midline as a longitudinal linear opacity between the umbilicus and the bladder.[11]
PNEUMOSCROTUM [FIGURE 8]
Figure 8.

Arrow showing air in the left scrotum without obvious signs of pneumoperitoneum in a neonate with perforated ileal atresia. See also Figure 3 above for pneumoscrotum
Source: Koh and Sheu[26], reproduced with permission from Elsevier
Areas of lucency can be identified on plain radiographs of the abdomen showing the scrotum which indicates the presence of air in the scrotum. Pneumoscrotum usually originates from three sources; intra-peritoneal air passing through the patent processus vaginalis (referred to as scrotal pneumatocele), extra-peritoneal air (from retroperitoneum, mediastinum or lungs) dissecting through fascial layers into scrotal wall and local scrotal causes (trauma, gas gangrene).[22,23]
Gastro intestinal perforation produces free intra-peritoneal air that can flow into the scrotum through the processus vaginalis, which is patent in up to 90% of new-born males.[24] Pneumoscrotum can be an important radiographic sign especially in children to aid diagnosis of bowel perforation and it is usually found along with other signs of pneumoperitoneum. However, it has been reported as the only sign of intestinal perforation that was subsequently confirmed operatively in the absence of other evidence of pneumoperitoneum.[25,26]
PERITONEAL CALCIFICATION [FIGURE 9]
Figure 9.
Arrows showing areas of peritoneal calcifications
Source: Auckland District Health Board[14]
In utero intestinal perforation with leakage causes meconium peritonitis, evidence of which can be seen on abdominal X-ray taken in the neonatal period as intra-peritoneal calcifications.[27] Calcifications can be seen along with features of free intra-peritoneal air.[28] Scrotal calcifications arising due to the passage of meconium through the patent processus vaginalis have also been reported as a radiographic sign that can suggest in-utero bowel perforation.[29]
NON-INTESTINAL PERFORATION CAUSES OF PNEUMOPERITONEUM
Pneumoperitoneum is an important sign of gastrointestinal perforation, but it is important to bear in mind that in up to 10% of patients, free intra-peritoneal gas is not due to bowel perforation.[30] A number of other conditions especially in children have been documented to produce pneumoperitoneum without bowel perforation, and this is often termed loosely as ‘spontaneous’ or ‘non-surgical’ pneumoperitoneum.[31]
These conditions include; immediately post-abdominal surgery (laparotomy or laparoscopy) irrespective of the indication, peritoneal dialysis, pneumothorax and pneumomediastinum, following pneumonia, patients on mechanical ventilation, ruptured pneumatosis cystoides intestinalis, collagen vascular disease, scuba diving, gynaecological procedures and idiopathic causes.[31,32,33] It is important to consider these causes of pneumoperitoneum that are not due to bowel perforation especially when evaluating an asymptomatic patient.
CONCLUSION
This review has highlighted the radiographic signs of gastrointestinal perforation on both erect and supine films using pictorial illustrations. Though several other features have been described in the literature, only radiographic signs that have been shown to be valid and sensitive in diagnosing bowel perforation have been included in this article. As the common saying goes; ‘we diagnose what we look for and look for what we know’, it is important that clinicians are aware of these signs to increase the diagnostic yield of plain abdominal radiographs. A good knowledge of these X-ray signs is crucial for more accurate diagnosis and timely surgical intervention in patients with gastrointestinal perforation.
ACKNOWLEDGEMENT
The author is grateful to Mr. Hugh Grant, consultant paediatric surgeon at the John Radcliffe Hospital, Oxford, UK, for making available his expert opinion on this topic and editing this work.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Abantanga FA, Wiafe-Addai BB. Postoperative complications after surgery for typhoid perforation in children in Ghana. Pediatr Surg Int. 1998;14:55–8. doi: 10.1007/s003830050435. [DOI] [PubMed] [Google Scholar]
- 2.Lin AC, Wu CC, Su CT. Classic signs of pneumoperitoneum on supine abdominal radiograph. Am J Emerg Med. 2006;24:642–3. doi: 10.1016/j.ajem.2005.12.023. [DOI] [PubMed] [Google Scholar]
- 3.Chiu YH, Chen JD, Tiu CM, Chou YH, Yen DH, Huang CI, et al. Reappraisal of radiographic signs of pneumoperitoneum at emergency department. Am J Emerg Med. 2009;27:320–7. doi: 10.1016/j.ajem.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 4.Yeung KW, Chang MS, Hsiao CP, Huang JF. CT evaluation of gastrointestinal tract perforation. Clin Imaging. 2004;28:329–33. doi: 10.1016/S0899-7071(03)00204-3. [DOI] [PubMed] [Google Scholar]
- 5.Ekwunife OH, Ugwu J, Modekwe V, Osuigwe AN. Gastrointesinal perforation in neonates; aetiology and risk factors. J Neonatal Surg. 2013;2:30. [PMC free article] [PubMed] [Google Scholar]
- 6.Williams N, Everson NW. Radiological confirmation of intraperitoneal free gas. Ann R Coll Surg Engl. 1997;79:8–12. [PMC free article] [PubMed] [Google Scholar]
- 7.Marshall GB. The cupola sign. Radiology. 2006;241:623–4. doi: 10.1148/radiol.2412040700. [DOI] [PubMed] [Google Scholar]
- 8.Hokama A, Nakamura M, Kobashigawa C, Chinen H, Kishimoto K, Nakamoto M, et al. Education and imaging. Gastrointestinal: Signs of pneumoperitoneum. J Gastroenterol Hepatol. 2009;24:497. doi: 10.1111/j.1440-1746.2009.05835.x. [DOI] [PubMed] [Google Scholar]
- 9.Au-Yong I, Au-Yong A, Broderick N. On-Call X-Rays Made Easy. China: Churchill Livingstone Elsevier; 2010. [DOI] [PubMed] [Google Scholar]
- 10.Child Abuse Medical Provider Program (CHAMP) New York: SUNY Upstate Medical University Syracuse; 2006-2014. [Last accessed on 2014 Aug 03]. Available from: http://www.champprogram.com/question/19a.shtml . [Google Scholar]
- 11.Chiu HS, Chung CH. Pneumoperitoneum on supine abdominal X-ray: Case report and review of radiological signs. Hong Kong J Emerg Med. 2005;12:46–9. [Google Scholar]
- 12.Rodriguez LR, Gonzalez GA, Menendez CP, Sanchez SG, Mata NV, Rubio NS. Intestinal Pathology in Neonatal Period. Vienna: European Society of Radiology. 2014. [Last accessed on 2014 Aug 03]. Available from: http://www.posterng.netkey.at/esr/viewing/index.php?module=viewing_poster&task=viewsection&ti=372782 .
- 13.Frković M, Klapan T, Moscatello I, Frković M. Diagnostic value of pneumoperitoneum on plain abdominal film. Radiol Oncol. 2001;35:237–42. [Google Scholar]
- 14.Auckland District Health Board. Auckland: Ministry of Health, New Zealand Government; 2011. [Last updated on 2011 Nov 29; Last accessed on 2014 Aug 04]. Available from: http://www.adhb.govt.nz/newborn/teachingresources/radiology/otherabdominalradiographs.htm . [Google Scholar]
- 15.Rampton JW. The football sign. Radiology. 2004;231:81–2. doi: 10.1148/radiol.2311011290. [DOI] [PubMed] [Google Scholar]
- 16.Lee HJ. Plain abdominal radiography in infants and children. Korean J Paediatr Gastroenterol Nutr. 2011;14:130–6. [Google Scholar]
- 17.Rigler LG. Spontaneous pneumoperitoneum – A roentgenologic sign found in the supine position. Radiology. 1941;37:604–7. [Google Scholar]
- 18.Ly JQ. The Rigler sign. Radiology. 2003;228:706–7. doi: 10.1148/radiol.2283020302. [DOI] [PubMed] [Google Scholar]
- 19.Fuller MJ. WikiRadiography. WikiFoundry. 2007. [Last accessed on 2011 May 27; Last accessed on 2014 Aug 05]. Pneumoperitoneum; p. 2. Available from: http://www.wikiradiography.com/page/Pneumoperitoneum . [Google Scholar]
- 20.Brill PW, Olson SR, Winchester P. Neonatal necrotizing enterocolitis: Air in Morison pouch. Radiology. 1990;174:469–71. doi: 10.1148/radiology.174.2.2296656. [DOI] [PubMed] [Google Scholar]
- 21.Radiopaedia.org. Connecticut: UBM Medica Network. 2005-2014. [Last accessed on 2014 Aug 05]. Available from: http://www.radiopaedia.org/cases/football-sign .
- 22.Patel C, Barnacle AM. Pneumoscrotum: A complication of pneumatosis intestinalis. Pediatr Radiol. 2011;41:129. doi: 10.1007/s00247-010-1706-7. [DOI] [PubMed] [Google Scholar]
- 23.Lostoridis E, Gkagkalidis K, Varsamis N, Salveridis N, Karageorgiou G, Kampantais S, et al. Pneumoscrotum as complication of blunt thoracic trauma: A case report. Case Rep Surg 2013. 2013 doi: 10.1155/2013/392869. 392869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khan YA, Akhtar J. Pneumoscrotum: A rare presentation of gastric perforation in a neonate. APSP J Case Rep. 2010;1:15. [PMC free article] [PubMed] [Google Scholar]
- 25.Aslan Y, Sarihan H, Dinç H, Gedik Y, Aksoy A, Dereci S. Gastric perforation presenting as bilateral scrotal pneumatoceles. Turk J Pediatr. 1999;41:267–71. [PubMed] [Google Scholar]
- 26.Koh CC, Sheu JC. Intestinal atresia presenting as bilateral scrotal pneumatocele: A case report. J Pediatr Surg. 2002;37:E2. doi: 10.1053/jpsu.2002.29461. [DOI] [PubMed] [Google Scholar]
- 27.Milas Z, Atkinson G, Gow KW. Pediatric surgical images. Meconium peritonitis. J Pediatr Surg. 2004;39:245–6. doi: 10.1016/j.jpedsurg.2003.11.052. [DOI] [PubMed] [Google Scholar]
- 28.Abubakar AM, Odelola MA, Bode CO, Sowande AO, Bello MA, Chinda JY, et al. Meconium peritonitis in Nigerian children. Ann Afr Med. 2008;7:187–91. doi: 10.4103/1596-3519.55655. [DOI] [PubMed] [Google Scholar]
- 29.Elsayed M, Barrow TA, Tang V, Kaleem M. Abnormal neonatal bowel gas patterns on plain radiography — Back to basics. Vienna: European Society of Radiology; 2014. [Last accessed on 2014 Aug 12]. Available from: http://www.posterng.netkey.at/esr/viewing/index.php?module=viewing_poster&task=viewsection&pi=117653&ti=378723&searchkey . [Google Scholar]
- 30.Mularski RA, Ciccolo ML, Rappaport WD. Nonsurgical causes of pneumoperitoneum. West J Med. 1999;170:41–6. [PMC free article] [PubMed] [Google Scholar]
- 31.Karaman A, Demirbilek S, Akin M, Gürünlüoglu K, Irsi C. Does pneumoperitoneum always require laparotomy? Report of six cases and review of the literature. Pediatr Surg Int. 2005;21:819–24. doi: 10.1007/s00383-005-1489-3. [DOI] [PubMed] [Google Scholar]
- 32.Williams NM, Watkin DF. Spontaneous pneumoperitoneum and other nonsurgical causes of intraperitoneal free gas. Postgrad Med J. 1997;73:531–7. doi: 10.1136/pgmj.73.863.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chan DT, Wong KK, Tam PK. Spontaneous pneumoperitoneum after pneumonia in a child. J Paediatr Child Health. 2007;43:85–6. doi: 10.1111/j.1440-1754.2007.01009.x. [DOI] [PubMed] [Google Scholar]


