Abstract
Septic arthritis is the result of bacterial infection of the hip joint and is often found in infants and toddlers. It is the most common septic joint condition during growth and may cause the most devastating complications without prompt and proper treatment. Early diagnosis and intervention are required to avoid irreversible complications. This review documents the systematic approach to diagnosis and management of septic arthritis in children.
Keywords: Septic arthritis, hip joint, management, children
INTRODUCTION
Septic arthritis of the hip commonly occurs in infants and toddlers. It is the most common septic joint condition during growth and may cause the most devastating complications without prompt and proper treatment. Diagnosis therefore should be made as fast as possible and treatment should be started as an emergency.[1,2] Most authors make the clinical diagnosis on a combination of clinical signs, laboratory tests and imaging.[3,4,5] Clinical findings include fever, poor general condition, loss of weight bearing and restriction of the joint movement, especially internal rotation. In neonates and infants, the diagnosis can often be difficult because the typical symptoms and signs may be lacking.[6,7] Positive laboratory tests include a white blood cell (WBC) count >12 × 109/L, erythrocyte sedimentation rate >20 mm/h and C-reaction protein (CRP) >20 mg/L. Elevation of CRP is still the highest predictive value for septic arthritis.[8,9,10] X-ray examination should be carried out in every case, whereas soft tissue swelling and loss of tissue planes may show within 3 days of infection onset, and bone changes may not appear before a history of 5 days or more. Widening of the hip joint space is not an early sign, and septic arthritis cannot be excluded without its absence. An ultrasound scan is particularly helpful for diagnosing the capsular distension in case of a hip joint effusion, but cannot distinguish between septic and non-septic arthritis, as capsular distension is not a specific ultrasound finding.[3,11,12] When septic arthritis of the hip is suspected, a diagnostic hip aspiration under the ultrasound or fluoroscopy guidance is considered to be the investigation of choice for the confirmation of septic arthritis. Following laboratory results are accepted as confirmation for septic arthritis of the hip: A positive synovial fluid culture, or a positive Gram-stain in synovial fluid, or a WBC count in synovial fluid >50,000/mm3 with a predominance of polymorphonuclear cells or a positive blood culture.[7,13,14] Treatment options include antibiotic therapy and surgical management. After aspiration of joint effusion, an instantaneous initiation of empiric antibiotic therapy is indicated and then switched to a targeted antibiotic therapy as soon as the joint fluid or blood culture and the sensitivity testing are available. Initial antibiotic therapy should be intravenous, then oral, although the timing for transition to oral medication remains controversial. The duration of antibiotic therapy is at least 2 weeks in general. If good clinical response and normalisation of CRP level are achieved within 24 h after initiation of the antibiotic therapy, no further surgical interventions are needed, and the duration of the whole antibiotic therapy may be shortened to 10 days.[15,16,17] If the clinical features or the biological inflammatory response deteriorate, then surgical interventions are recommended definitely, and antibiotic therapy is continued until good clinical response and normalisation of CRP level are obtained.[2,5] At present in the literature, there are three major surgical options which are:
-
(1)
Repeated aspiration (ultrasound- or fluoroscopy-guided),
-
(2)
Arthroscopy drainage and irrigation and
-
(3)
Ppen arthrotomy.
In recent years, there is a tendency to perform less-aggressive surgery for treatment of septic arthritis although arthrotomy remains the gold standard. The aim of this review is to introduce these surgical procedures in details and provide guidelines for the surgery.
SURGICAL MANAGEMENTS
Aspiration
Ultrasound- or fluoroscopy-guided aspiration of the hip joint should be performed as soon as possible when septic arthritis is suspected because cell count, Gram stain and culture can be obtained directly through this procedure. An anterior, lateral, or medial approach can be used to aspirate the hip joint. As the hip joint is deep, aspiration under image intensifier makes intra-capsular needle placement more certain especially combined with an arthrogram. Ultrasound-guided aspiration is a useful technique that is more accessible and avoids radiation exposure in children.
Anterior approach
With the patient supine, palpate the femoral artery in line with the inguinal ligament and then insert an 18-gauge spinal needle approximately 2 cm distal and 2 cm lateral to this point. Advance the needle at an angle of 45-60° posteromedially into the joint. Confirm the position of the needle using image intensifier or ultrasound.
Lateral approach
Insert the needle just anterior and inferior to the tip of the greater trochanter. Then advance the needle into the joint in proximal and medial directions with the hip internally rotated.
Medial approach
Flex and abduct the hip. Insert the needle inferior to the proximal adductor longus tendon and advance it toward the femoral head. We use this approach only in children under 1 year.
In 2004, Givon et al. described a technique of daily repeated ultrasound-guided aspiration and irrigation to treat septic arthritis of the hip.[18] The aspiration was performed with an 18-gauge spinal needle under ultrasound guidance and local anaesthesia or sedation. The entry point is where the coronal and transverse lines of the hip intersect, which is determined by an ultrasound technician. After the aspiration, the hip was irrigated and the procedure was repeated daily, with an average of 3.6 (range 3-5) times. Three-fourth cases resumed weight-bearing within 24 h and all of them returned to normal gait in 4 days. Eighty-six per cent of the children were treated successfully by this procedure, and no complications were found in all cases. The authors concluded that procedure combined with an antibiotic therapy is safe and efficacious not only prevents surgery and general anaesthesia but also provides a faster return to normal activity. Recently, some authors only aspirated the hip on a single occasion, which has a similar successful rate as Givon's technique.[19,20] However, because needle aspiration cannot effectively drainage the viscous pus and remove the connective tissue septa in a case with a prolonged history, this technique has long been controversial and most authors recommend that this technique is only used in a child with an early presentation of no more than 5 days since onset of symptoms or a previous healthy status [Figure 1].[2,5]
Figure 1.
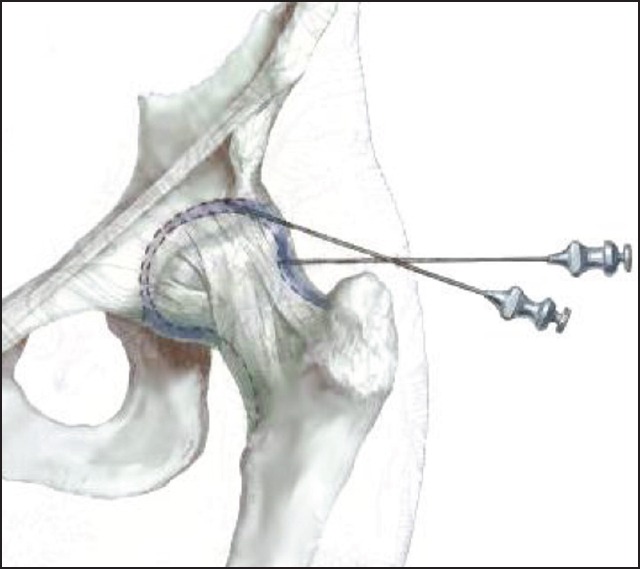
Aspiration of the hip
Arthroscopy
In 2008, El-Sayed published a prospective controlled study comparing the outcome of open arthrotomy and arthroscopic drainage and irrigation in early cases of septic arthritis of the hip in children.[21] The results showed a similar successful rate as open arthrotomy and a significant shorter hospitalisation. He concluded that arthroscopy combined with an antibiotic treatment is an effective method with minimal invasion and less hospital stay in treating septic arthritis of the hip, provided that the orthopaedic surgeon is skilled in paediatric arthroscopy. For the same reasons as needle aspiration, arthroscopy is not fit for a child with a late presentation of more than 5 days since onset of symptoms or a child without a previous healthy status.
Three standard portals of the hip may be used: Anterolateral, anterior and posterolateral[22] [Figure 2]. The patient lies on a fracture table under general anaesthesia and the guidance of fluoroscopy. Gentle and sufficient traction is applied to distract the joint 5 mm in young children and 10 mm in older ones as observed on the image intensifier. Do not penetrate the labrum when making the portals. The anterolateral portal is established first and is the safest in regard to the neurovascular structures. This portal is placed at the proximal anteromedial margin of the greater trochanter and penetrates the gluteus medius muscle. After that, the other portals can be made under direct view. The anterior portal is made at the intersection of a line drawn from the anterior superior iliac spine and a transverse line drawn from the tip of the greater trochanter and penetrates the sartorius and rectus femoris. The posterolateral portal is located just superior to the margin of the greater trochanter at its posterior border, penetrates the gluteus medius and minimus muscle and converges toward the anterolateral portal. It is important to keep the hip in neutral position while making the posterolateral portal ensure that the sciatic nerve is not at risk. After establishing the portals, 30° and 70° arthroscopes are alternatively used between the portals for complete visualisation of the hip.
Figure 2.
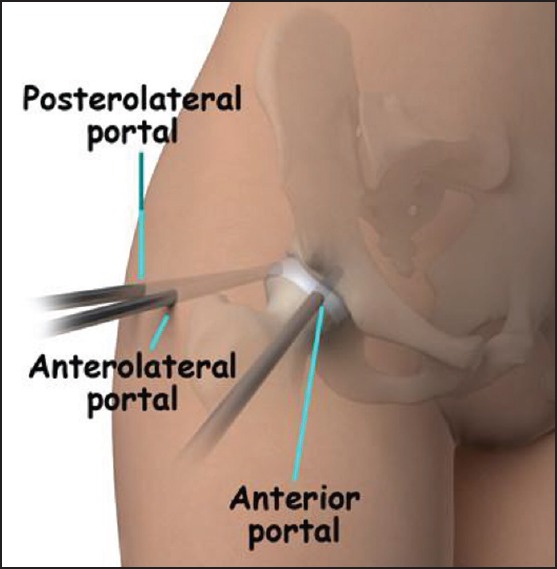
Three standard portals for hip arthroscopy
The hip joint is divided into the central compartment (the intra-articular region) and the peripheral compartment (the intra-capsular but extra-articular region). Thoroughly inspect the central compartment with the hip distracted. A systematic approach includes labrum, fovea, ligamentum teres, articular surface of the femoral head and acetabulum and joint recesses. Then, release the traction and observe the peripheral compartment. Arthroscopic debridement, irrigation and drainage of the hip are carried out in order and a suction drain is used. Post-operatively, simple bed rest with skin traction is used for pain relief. Early range of motion of the hip is encouraged as soon as the pain became tolerable. In our opinion, hip arthroscopy and irrigation are superior to open arthrotomy, but it is technically more demanding. By hip arthrotomy, a better overview of the joint and sufficient irrigation can be provided.
Open arthrotomy
Most authors still support an urgent arthrotomy with drainage.[1,2,5] In fact, open arthrotomy remains the gold standard for treatment of septic arthritis of the hip by far. It is a procedure with which most orthopaedic surgeons are familiar and can be performed with little-specialised equipment and less training. Anterior and lateral approaches of the hip are most frequently used in children because damage to the blood supply to the femoral head is avoided.
Anterior approach
This approach is actually the lower part of Smith-Peterson approach. Make a vertical incision beginning about 1 cm below the anterior superior iliac spine inferiorly. Protect the lateral femoral cutaneous nerve and retract it to the medial side. Expose the sartorius muscle on the medial side and the tensor fasciae latae and vastus lateralis muscles on the lateral side. Use blunt dissection to separate these muscles. Identify the lateral border of the rectus femoris and retract it medially, thus exposes the hip joint capsule. Protect the ascending branch of the lateral femoral circumflex artery as far as possible. Open the capsule, evacuate the pus, remove all non-viable tissue and irrigate the joint. Leave the capsule open, but close the skin loosely over drains. If a wider exposure is needed, extended the skin incision proximally onto the iliac crest and sub-periosteally detach the origins of the tensor fasciae latae and gluteal muscles from the ilium. Acute septic arthritis does not require synovectomy and often can be closed over drains after a single surgical procedure, whereas more chronic infections may benefit from serial debridement. Chronic infection or recurrent septic arthritis may result in a thick rind of tissue that lines the joint cavity and must be removed. Pathology and cultures are obligatory.
Lateral approach
Make a longitudinal incision parallel with the anterior border of the greater trochanter. Incise the tensor fasciae latae, exposing the vastus lateralis. Detach the anterior portion of the vastus lateralis and retract the abductor muscles proximally to expose the anterior capsule of the hip. A classical Watson-Jones approach can be used either: Begin an incision 2.5 cm distal and lateral to the anterior superior iliac spine and curve it distally and posteriorly over the lateral aspect of the greater trochanter and lateral surface of the femoral shaft. Expose the anterosuperior capsule of the hip joint between the gluteus medius and tensor fasciae latae.
After treatment
A spica cast in moderate abduction may be a treatment option in toddlers to prevent hip dislocation. For older children and adolescents, bed rest and skin traction are recommended until the wound has healed and the patient can control the leg. Then, partial weight-bearing is permitted, and active range-of-motion exercises are started.
Summary
Septic arthritis of the hip in children is an emergency. The earlier the diagnosis and treatment begin, the less probably invasive the treatment may be, and the better the prognosis is. For a case with a history shorter than 5 days and a previous healthy status, after the diagnosis is confirmed, repeated ultrasound- or fluoroscopy-guided aspiration and irrigation or arthroscopic drainage and irrigation of the hip may be attempted. If clinical features or the biological inflammatory response does not improve within 1-2 days or even deteriorate, or for a case with a history longer than 5 days, open arthrotomy is the choice of treatment undoubtedly. In any case, if intra-articular pus is detected, arthroscopic irrigation or open arthrotomy should be carried out as an emergency.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rutz E. Septic arthritis of the hip joint in children is an emergency. Afr J Paediatr Surg. 2012;9:1–2. doi: 10.4103/0189-6725.93292. [DOI] [PubMed] [Google Scholar]
- 2.Rutz E, Brunner R. Septic arthritis of the hip — Current concepts. Hip Int. 2009;19(Suppl 6):S9–12. doi: 10.1177/112070000901906s03. [DOI] [PubMed] [Google Scholar]
- 3.Al Saadi MM, Al Zamil FA, Bokhary NA, Al Shamsan LA, Al Alola SA, Al Eissa YS. Acute septic arthritis in children. Pediatr Int. 2009;51:377–80. doi: 10.1111/j.1442-200X.2008.02791.x. [DOI] [PubMed] [Google Scholar]
- 4.Frick SL. Evaluation of the child who has hip pain. Orthop Clin North Am. 2006;37:133–40, v. doi: 10.1016/j.ocl.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Kang SN, Sanghera T, Mangwani J, Paterson JM, Ramachandran M. The management of septic arthritis in children: Systematic review of the English language literature. J Bone Joint Surg Br. 2009;91:1127–33. doi: 10.1302/0301-620X.91B9.22530. [DOI] [PubMed] [Google Scholar]
- 6.Nunn TR, Cheung WY, Rollinson PD. A prospective study of pyogenic sepsis of the hip in childhood. J Bone Joint Surg Br. 2007;89:100–6. doi: 10.1302/0301-620X.89B1.17940. [DOI] [PubMed] [Google Scholar]
- 7.Shah SS. Abnormal gait in a child with fever: Diagnosing septic arthritis of the hip. Pediatr Emerg Care. 2005;21:336–41. doi: 10.1097/01.pec.0000159063.24820.73. [DOI] [PubMed] [Google Scholar]
- 8.Kocher MS, Mandiga R, Zurakowski D, Barnewolt C, Kasser JR. Validation of a clinical prediction rule for the differentiation between septic arthritis and transient synovitis of the hip in children. J Bone Joint Surg Am. 2004;86-A:1629–35. doi: 10.2106/00004623-200408000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Kocher MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis and transient synovitis of the hip in children: An evidence-based clinical prediction algorithm. J Bone Joint Surg Am. 1999;81:1662–70. doi: 10.2106/00004623-199912000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Caird MS, Flynn JM, Leung YL, Millman JE, D’Italia JG, Dormans JP. Factors distinguishing septic arthritis from transient synovitis of the hip in children. A prospective study. J Bone Joint Surg Am. 2006;88:1251–7. doi: 10.2106/JBJS.E.00216. [DOI] [PubMed] [Google Scholar]
- 11.Zamzam MM. The role of ultrasound in differentiating septic arthritis from transient synovitis of the hip in children. J Pediatr Orthop B. 2006;15:418–22. doi: 10.1097/01.bpb.0000228388.32184.7f. [DOI] [PubMed] [Google Scholar]
- 12.Gordon JE, Huang M, Dobbs M, Luhmann SJ, Szymanski DA, Schoenecker PL. Causes of false-negative ultrasound scans in the diagnosis of septic arthritis of the hip in children. J Pediatr Orthop. 2002;22:312–6. [PubMed] [Google Scholar]
- 13.Jung ST, Rowe SM, Moon ES, Song EK, Yoon TR, Seo HY. Significance of laboratory and radiologic findings for differentiating between septic arthritis and transient synovitis of the hip. J Pediatr Orthop. 2003;23:368–72. [PubMed] [Google Scholar]
- 14.Luhmann SJ, Jones A, Schootman M, Gordon JE, Schoenecker PL, Luhmann JD. Differentiation between septic arthritis and transient synovitis of the hip in children with clinical prediction algorithms. J Bone Joint Surg Am. 2004;86-A:956–62. doi: 10.2106/00004623-200405000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Peltola H, Pääkkönen M, Kallio P, Kallio MJ. Osteomyelitis-Septic Arthritis (OM-SA) Study Group. Prospective, randomized trial of 10 days versus 30 days of antimicrobial treatment, including a short-term course of parenteral therapy, for childhood septic arthritis. Clin Infect Dis. 2009;48:1201–10. doi: 10.1086/597582. [DOI] [PubMed] [Google Scholar]
- 16.Peltola H, Pääkkönen M, Kallio P, Kallio MJ. OM-SA Study Group. Clindamycin vs. first-generation cephalosporins for acute osteoarticular infections of childhood — A prospective quasi-randomized controlled trial. Clin Microbiol Infect. 2012;18:582–9. doi: 10.1111/j.1469-0691.2011.03643.x. [DOI] [PubMed] [Google Scholar]
- 17.Pääkkönen M, Kallio MJ, Peltola H, Kallio PE. Pediatric septic hip with or without arthrotomy: Retrospective analysis of 62 consecutive nonneonatal culture-positive cases. J Pediatr Orthop B. 2010;19:264–9. doi: 10.1097/BPB.0b013e32833822be. [DOI] [PubMed] [Google Scholar]
- 18.Givon U, Liberman B, Schindler A, Blankstein A, Ganel A. Treatment of septic arthritis of the hip joint by repeated ultrasound-guided aspirations. J Pediatr Orthop. 2004;24:266–70. doi: 10.1097/00004694-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Griffet J, Oborocianu I, Rubio A, Leroux J, Lauron J, Hayek T. Percutaneous aspiration irrigation drainage technique in the management of septic arthritis in children. J Trauma. 2011;70:377–83. doi: 10.1097/TA.0b013e31820318f0. [DOI] [PubMed] [Google Scholar]
- 20.Journeau P, Wein F, Popkov D, Philippe R, Haumont T, Lascombes P. Hip septic arthritis in children: Assessment of treatment using needle aspiration/irrigation. Orthop Traumatol Surg Res. 2011;97:308–13. doi: 10.1016/j.otsr.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 21.El-Sayed AM. Treatment of early septic arthritis of the hip in children: Comparison of results of open arthrotomy versus arthroscopic drainage. J Child Orthop. 2008;2:229–37. doi: 10.1007/s11832-008-0094-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roy DR. Arthroscopy of the hip in children and adolescents. J Child Orthop. 2009;3:89–100. doi: 10.1007/s11832-008-0143-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


