Abstract
Objective:
To evaluate the clinical performance of brackets cured with a high-intensity, light-emitting diode (LED) with a shorter curing time.
Materials and Methods:
Thirty-four patients and a total of 680 brackets were examined using a randomized split-mouth design. The maxillary right and mandibular left quadrants were cured for 6 seconds with a high-intensity LED light (3200 mW/cm2) and the maxillary left and mandibular right quadrants were cured for 20 seconds with a standard-intensity LED light (1200 mW/cm2). Alternating patients had the quadrants inverted for the curing protocol. The number and date of each first-time bracket failure was recorded from 199 to 585 days posttreatment.
Results:
The bracket failure rate was 1.18% for both curing methods. The proportion of bracket failure was not significantly different between curing methods (P = 1.000), genders (P = 1.000), jaws (P = .725), sides (P = .725), or quadrants (P = .547). Posterior teeth exhibited a greater proportion of failures (2.21%) relative to anterior teeth (0.49%), although the difference was not statistically significant (P = .065).
Conclusions:
No difference was found in bond failure rates between the two curing methods. Both methods showed bond failure rates low enough to be considered clinically sufficient. The high-intensity LED light used with a shorter curing time may be considered an advantage due to the reduced chair time.
Keywords: Curing times, LED lights, Bracket failure rate
INTRODUCTION
One of the great advances in the profession of orthodontics has been the introduction of light-cured adhesives. Light-cure composite resins have become the most popular orthodontic adhesives.1 These adhesives have provided the practitioner the luxury of curing on demand. This gives the orthodontist a reduced risk of contamination, easier removal of excess adhesive, and more working time to position the brackets accurately.2
Over the past several years, curing lights have experienced vast improvements. Light-emitting diode (LED) technology is now the most common means of light curing for bracket bonding.3–5 Compared with the halogen curing system, LED lights can achieve clinical bonding success with shorter curing time.6–8 Curing-light manufacturers advertise that by increasing the light intensity, also referred to as power density, even less curing time is needed to reach adequate bond strengths.
However, no studies have examined the clinical performance of the new, third generation, high-intensity LED lights as to whether they allow further curing time reduction. In vitro studies provide information about certain aspects of physical and chemical adhesive properties of orthodontic bonding. However, studies completed under ideal laboratory conditions do not describe how materials will perform in the oral cavity.9,10
Therefore, the aim of this study was to analyze whether high-intensity LED lights used with reduced curing times provide adequate clinical bond strength to resist bracket failure. The clinical bond-failure rates of two different LED light-curing settings, a high-intensity LED (3200 mW/cm2) curing light with a 6-second curing time and a standard LED curing light (1200 mW/cm2) with a 20-second cure time were compared over a minimum of the first 6 months of orthodontic treatment. The null hypothesis was that there is no difference in hazard rate for bracket failure between the 20-second and the 6-second curing time groups.
MATERIALS AND METHODS
A total of 34 consecutive patients (17 males and 17 females, with an average age of 14.1 years and a range of 11.6 to 46.1 years), who received comprehensive orthodontic treatment at the Medical University of South Carolina, were enrolled for this study with approval of the Institutional Review Board. The patients had to meet the following criteria to be included in the study:
presence of a complete permanent dentition,
absence of occlusal interferences,
no need for extractions or orthognathic surgery,
absence of intra- and extraoral appliances,
no deleterious oral habits,
absence of any visible enamel malformation or restoration on the buccal surface of teeth.
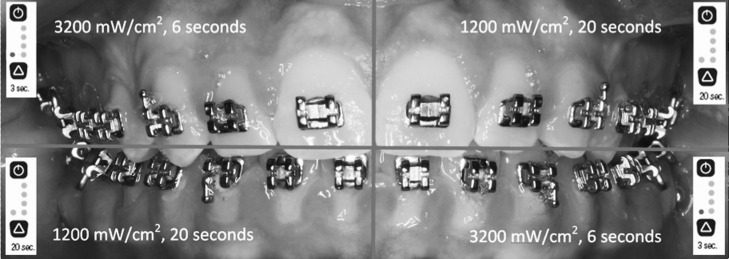
A randomized split-mouth design was used for this study (Figure 1). Each consecutive patient that participated in the study had alternating quadrants for the study and control settings. The patients were unaware of what curing setting was being used on each quadrant. For each patient, no teeth distal to the second premolars were included in the study. A total of 680 brackets were examined. Our power analysis showed that an overall sample size of 680 brackets (340 in each treatment group) achieves 85% power at a .050 significance level to detect a difference of 4% between the two treatment groups.
Figure 1.
Split-mouth design curing protocol.
The two different settings of a Valo Ortho LED curing light (Ultradent, South Jordan, UT), the standard setting (1200 mW/cm2) and the Xtra power quadrant setting (3200 mW/cm2), were used as the light resources for the control and study groups, respectively. Before the study began, the Valo light intensity was checked using a Demetron radiometer (Kerr Corporation, Orange, Calif). On 17 of the participants, the maxillary right and the mandibular left quadrants were cured with the 3200 mW/cm2 for a total of 6 seconds per tooth (two 3-second curing processes were repeated). The maxillary left and mandibular right quadrants were cured with the 1200 mW/cm2 setting for a total of 20 seconds per tooth (two 10-second curing processes were repeated). On the other 17 participants, the quadrants were inverted.
A direct bonding procedure was used to place the Opal Avex edgewise brackets (0.022-inch slot, MBT prescription; Ultradent) on the studied teeth. The teeth were isolated with a Nola cheek/lip retractor kit (Great Lakes Orthodontics, Tonawanda, NY), then rinsed and dried. The teeth were then etched on the entire facial surface with 37% phosphoric acid for 20 seconds. They were then rinsed and dried until the enamel appeared chalky white. Opal Seal adhesive primer (Ultradent) was then applied on the enamel surface. Opal Bond MV adhesive was applied directly on the bracket pad and then placed on the tooth with bracket placement pliers. Any excess adhesive paste was removed with an explorer. The initial archwire placed on all patients after the bonding was of 0.014-inch nickel titanium. If there were any tooth-bracket interferences, bite pads or turbos were placed either on the anterior teeth or the molars to open the bite. The patients were given written and oral instructions on caring for the fixed appliances. All patients were seen approximately every 4 weeks.
An observation period of a minimum of 6 months was chosen since it has been shown that 82% of bracket failures occur within the first 6 months of treatment.11 Data collection was through clinical observance and patients' reports. The location and date of bracket failures were recorded on the date observed by the operator. Patients were instructed to immediately contact the clinic if they suspected a detached bracket. Only first-time bond failures were recorded. In vitro studies have shown that reconditioning a bracket reduces bond strength and is statistically different from a new, stainless steel bracket.12,13
The proportion of bracket failures was examined by curing method, gender, maxillary vs mandibular, anterior vs posterior, right vs left, and quadrant. The number of bracket failures was compared between these groups using Fisher's exact test. Time to bracket failure was examined by treatment using the marginal Cox regression model approach, which accounts for repeated measures within a subject.14 All analyses were conducted in SAS 9.3 (SAS Institute, Cary, NC).
RESULTS
The study subjects were followed for a median of 305 days (10.02 months), a mean of 356 days (11.70 months), and a range from 199 to 585 days posttreatment (380 days; 12.5 months). During the follow-up period, 8 of the 680 brackets became detached (1.18%). Both the 6-second and 20-second curing methods had four (1.18%) bracket failures each.
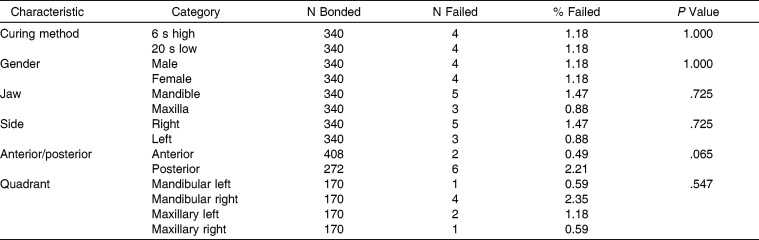
In addition to comparing the proportion of brackets that failed by curing method, bond failures were compared by gender, maxillary vs mandibular, anterior vs posterior, right vs left, and quadrant (Table 1). Both males and females had 1.18% of brackets fail (P = 1.000). The mandible had a failure rate of 1.47%, the maxilla, 0.88% (P = .725). The posterior teeth exhibited a greater proportion of failures (2.21%) relative to the anteriors (0.49%), although the difference was not statistically significant (P = .065). The right side experienced a 1.47% failure rate, while the left side had a 0.88% failure rate (P = .725). When divided into quadrants, the difference between the mandibular left (0.59%), mandibular right (2.35%), maxillary left (1.18%), and maxillary right (0.59%) was not significant (P = .547).
Table 1.
Proportion of Bracket Failures Between Different Groups
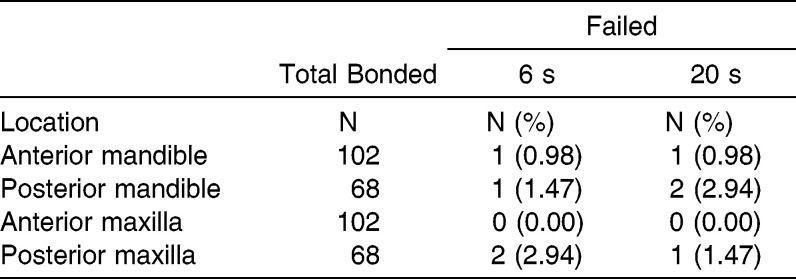
The maxilla and mandible were subdivided into anterior and posterior segments to analyze the proportion of brackets that failed using the two curing methods. No significant differences in the proportion of bracket failures were noted between treatment groups comparing anterior and posterior segments of the maxilla and mandible (Table 2).
Table 2.
Number and Percentage of Bond Failures in Each Treatment Group by Jaw and Anterior-Posterior Position
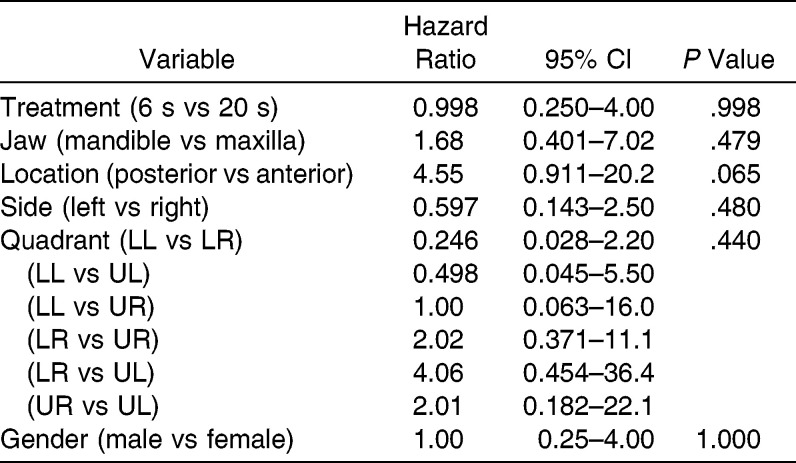
Time to bracket failure was also compared (Table 3). There was no difference in time to bracket failure between the 6-second and the 20-second curing times (P = .998, hazard ratio [HR] = 0.998). There were also no significant differences in time to bracket failure by gender, jaw, side, or quadrant. There was a marginally significant difference in time to failure between the posterior and anterior teeth, with the posterior brackets taking more time to fail (P = .065, HR = 4.55). Kaplan-Meier survival curves of time to bracket failure by curing methods and anterior or posterior placement are shown in Figures 2 and 3.
Table 3.
Univariate Log-rank Test Results Comparing Time to Bracket Failure
Figure 2.
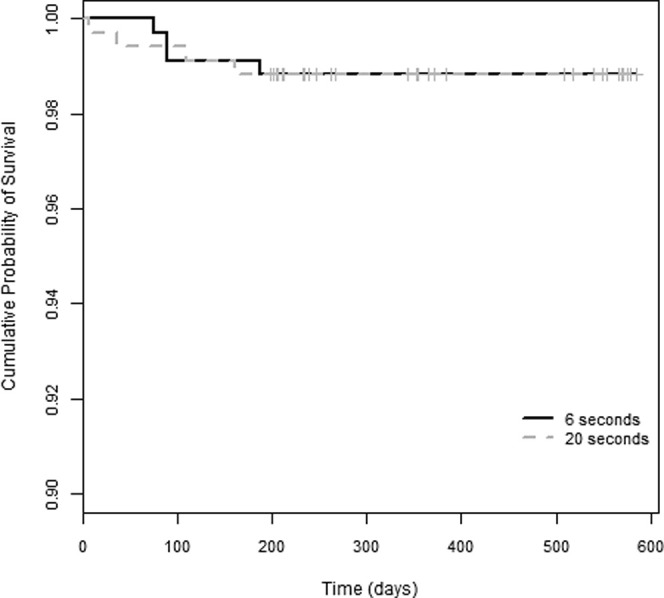
Survival plots for each curing method.
Figure 3.
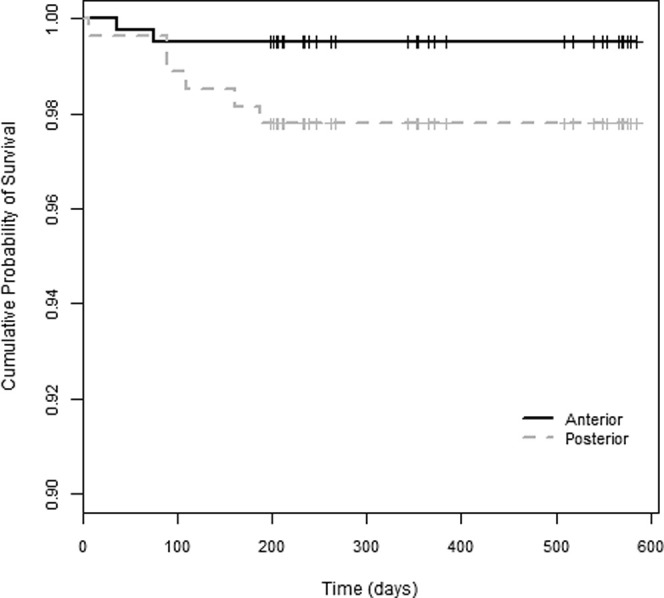
Survival plots for anterior-posterior position.
DISCUSSION
This is the first split-mouth study to show the clinical performance of a high-intensity LED over 2000 mW/cm2. We demonstrated that a 6-second curing time per tooth with a high-intensity curing light is sufficient to produce clinically adequate bond failure rates that are comparable to brackets cured with a standard intensity LED for 20 seconds.15–17 This finding extends our knowledge from previous clinical studies6–8 that compared halogen- and LED-curing-light performance. Mavropoulos et al.18 showed that sheer bond strength depends on energy density, but the relationship is nonlinear and is influenced by both power density and curing time. They stated that the ideal combination of exposure time and power density is 4 seconds with 3000 mW/cm.18 The curing light used in the current study used a curing time (6 seconds) that exceeded this minimum exposure time and had a power density (3200 mW/cm2) that met the maximum usefulness suggested.
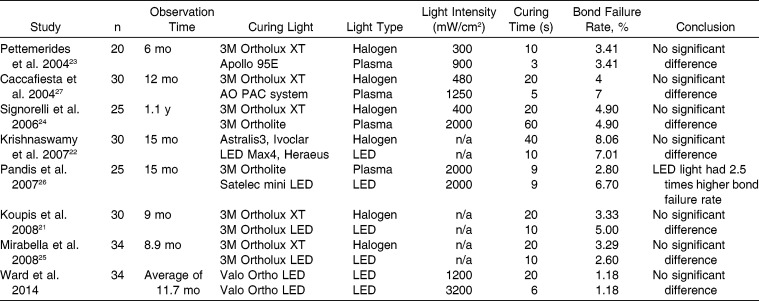
This study yielded an even lower bond failure rate than did other clinical studies (Table 4), with a slightly larger sample size and a comparable observation period. One factor that may have influenced the low bracket failure rate was the bonding system used. Our study used the same brand adhesive recommended for this bracket system and followed the manufacturer's protocol exclusively. In addition, we utilized the Nola retractor to ensure little or no contamination of the bonding surfaces. However, it is difficult to compare bond failure rates when most other studies7,8,19–22 did not clearly define their bonding systems and isolation protocols.
Table 4.
Clinical Studies of Orthodontic Bond Failure Rates With Different Curing Lights
In this study, there was no difference in bracket failure between males and females, which disagrees with what was reported in another study showing that more failures were found in males than in females.6 This might have been because the boys in that study were less attentive to diet and care of their fixed appliances during the observation period. We did not evaluate age and malocclusion type because previous studies found no significant differences.23,24
The distribution of failures between the two dental arches and the two sides has varied with prior studies.6,11,22,24–29 In our study, slightly more failures occurred in the mandibular arch and on the right side, but the difference was not statistically significant. Variability between studies could be due to differences in the mastication habits of patients. It could also be due to differences of moisture control and handling materials between right- and left-handed operators.
We found more failures in the posterior teeth than in the anteriors. This agrees with the results of previous studies.11,22,23,25–28,30,31 This has been attributed to the higher masticatory forces of the posterior teeth22,25 and access difficulties during the bonding procedure.23,25,27,28,30 Another causative factor could be the differences in the micromorphology and structure of the superficial enamel layer between posterior and anterior teeth.22,25,32
One possible clinical concern of the high-intensity LED light is its influence on tooth vitality from the heat generated during the curing process. It has been reported that an increase of 5.5°C is the critical value at which pulpal damage occurs.33 Malkoc et al.34 reported that the only light that caused pulp temperature to increase more than the critical value was the high-intensity halogen light for 40 seconds. The total light energy (light intensity × exposure time) of the Valo curing light is lower than the lights that caused significant temperature increases. The light energy is actually even less, because the teeth were cured first for 3 seconds, then for 3 more seconds later after the heat had already dissipated. Loney et al.35 has also shown that when a high-intensity plasma arc light is used, tooth temperature increases are less than when a halogen lamp is used. This is probably due to the shorter curing times used with high-intensity lights. Because of the short curing times used with the high-intensity LED in the current study, pulpal damage should not be a concern.
CONCLUSIONS
There were no significant differences in percentage of bond failures when using a 3200 mW/cm2 LED light for 6 seconds compared with a 1200 mW/cm2 LED light for 20 seconds.
The clinical application of high-intensity LED curing lights for shorter irradiation times is a clinically valid procedure that may decrease procedure time without increasing bond failures.
REFERENCES
- 1.Keim RG, Gottlieb EL, Nelson AH, Vogels DS., III 2002 JCO study of orthodontic diagnosis and treatment procedures. Part 1. Results and trends. J Clin Orthod. 2002;36:553–568. [PubMed] [Google Scholar]
- 2.Read MJ. The bonding of orthodontic attachments using a visible light cured adhesive. Br J Orthod. 1984;11:16–20. doi: 10.1179/bjo.11.1.16. [DOI] [PubMed] [Google Scholar]
- 3.Mills RW, Jandt KD, Ashworth SH. Dental composite depth of cure with halogen and blue light emitting diode technology. Br Dent J. 1999;186:388–391. doi: 10.1038/sj.bdj.4800120. [DOI] [PubMed] [Google Scholar]
- 4.Dunn WJ, Taloumis LJ. Polymerization of orthodontic resin cement with light-emitting diode curing units. Am J Orthod Dentofacial Orthop. 2002;122:236–241. doi: 10.1067/mod.2002.123949. [DOI] [PubMed] [Google Scholar]
- 5.Bishara SE, Ajlouni R, Oonsombat C. Evaluation of a new curing light on the shear bond strength of orthodontic brackets. Angle Orthod. 2003;73:431–435. doi: 10.1043/0003-3219(2003)073<0431:EOANCL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Koupis NS, Eliades T, Athanasiou AE. Clinical evaluation of bracket bonding using two different polymerization sources. Angle Orthod. 2008;78:922–925. doi: 10.2319/072807-351.1. [DOI] [PubMed] [Google Scholar]
- 7.Krishnaswamy NR, Sunitha C. Light-emitting diode vs halogen light curing of orthodontic brackets: a 15-month clinical study of bond failures. Am J Orthod Dentofacial Orthop. 2007;132:518–523. doi: 10.1016/j.ajodo.2005.09.038. [DOI] [PubMed] [Google Scholar]
- 8.Mirabella D, Spena R, Scognamiglio G, Luca L, Gracco A, Siciliani G. LED vs halogen light-curing of adhesive-precoated brackets. Angle Orthod. 2008;78:935–940. doi: 10.2319/042707-211.1. [DOI] [PubMed] [Google Scholar]
- 9.Fox NA, McCabe JF, Buckley JG. A critique of bond strength testing in orthodontics. Br J Orthod. 1994;21:33–43. doi: 10.1179/bjo.21.1.33. [DOI] [PubMed] [Google Scholar]
- 10.Eliades T, Brantley WA. The inappropriateness of conventional orthodontic bond strength assessment protocols. Eur J Orthod. 2000;22:13–23. doi: 10.1093/ejo/22.1.13. [DOI] [PubMed] [Google Scholar]
- 11.O'Brien KD, Read MJ, Sandison RJ, Roberts CT. A visible light-activated direct-bonding material: an in vivo comparative study. Am J Orthod Dentofacial Orthop. 1989;95:348–351. doi: 10.1016/0889-5406(89)90169-8. [DOI] [PubMed] [Google Scholar]
- 12.Cacciafesta V, Sfondrini MF, Melsen B, Scribante A. A 12 month clinical study of bond failures of recycled versus new stainless steel orthodontic brackets. Eur J Orthod. 2004;26:449–454. doi: 10.1093/ejo/26.4.449. [DOI] [PubMed] [Google Scholar]
- 13.Regan D, LeMasney B, van Noort R. The tensile bond strength of new and rebonded stainless steel orthodontic brackets. Eur J Orthod. 1993;15:125–135. doi: 10.1093/ejo/15.2.125. [DOI] [PubMed] [Google Scholar]
- 14.Lee EW, Wei LJ, Amato DA. Survival Analysis State of the Art. Dordrecht, The Netherlands: Kluwer Academic Publishers; 1992. [Google Scholar]
- 15.Cerekja E, Cakirer B. Effect of short curing times with a high-intensity light-emitting diode or high-power halogen on shear bond strength of metal brackets before and after thermocycling. Angle Orthod. 2011;81:510–516. doi: 10.2319/071810-412.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silta YT, Dunn WJ, Peters CB. Effect of shorter polymerization times when using the latest generation of light-emitting diodes. Am J Orthod Dentofacial Orthop. 2005;128:744–748. doi: 10.1016/j.ajodo.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 17.Niepraschk M, Rahiotis C, Bradley TG, Eliades T, Eliades G. Effect of various curing lights on the degree of cure of orthodontic adhesives. Am J Orthod Dentofacial Orthop. 2007;132:382–384. doi: 10.1016/j.ajodo.2007.04.029. [DOI] [PubMed] [Google Scholar]
- 18.Mavropoulos A, Cattani-Lorente M, Krejci I, Staudt CB. Kinetics of light-cure bracket bonding: power density vs exposure duration. Am J Orthod Dentofacial Orthop. 2008;134:543–547. doi: 10.1016/j.ajodo.2006.09.068. [DOI] [PubMed] [Google Scholar]
- 19.Pettemerides AP, Sherriff M, Ireland AJ. An in vivo study to compare a plasma arc light and a conventional quartz halogen curing light in orthodontic bonding. Eur J Orthod. 2004;26:573–577. doi: 10.1093/ejo/26.6.573. [DOI] [PubMed] [Google Scholar]
- 20.Signorelli MD, Kao E, Ngan PW, Gladwin MA. Comparison of bond strength between orthodontic brackets bonded with halogen and plasma arc curing lights: an in-vitro and in-vivo study. Am J Orthod Dentofacial Orthop. 2006;129:277–282. doi: 10.1016/j.ajodo.2004.07.043. [DOI] [PubMed] [Google Scholar]
- 21.Pandis N, Strigou S, Eliades T. Long-term failure rate of brackets bonded with plasma and high-intensity light-emitting diode curing lights: a clinical assessment. Angle Orthod. 2007;77:707–710. doi: 10.2319/062106-253. [DOI] [PubMed] [Google Scholar]
- 22.Cacciafesta V, Sfondrini MF, Scribante A. Plasma arc versus halogen light-curing of adhesive-precoated orthodontic brackets: a 12-month clinical study of bond failures. Am J Orthod Dentofacial Orthop. 2004;126:194–199. doi: 10.1016/j.ajodo.2003.05.004. [DOI] [PubMed] [Google Scholar]
- 23.Millett DT, Hallgren A, Cattanach D, et al. A 5-year clinical review of bond failure with a light-cured resin adhesive. Angle Orthod. 1998;68:351–356. doi: 10.1043/0003-3219(1998)068<0351:AYCROB>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Shammaa I, Ngan P, Kim H, et al. Comparison of bracket debonding force between two conventional resin adhesives and a resin-reinforced glass ionomer cement: an in vitro and in vivo study. Angle Orthod. 1999;69:463–469. doi: 10.1043/0003-3219(1999)069<0463:COBDFB>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Sunna S, Rock WP. Clinical performance of orthodontic brackets and adhesive systems: a randomized clinical trial. Br J Orthod. 1998;25:283–287. doi: 10.1093/ortho/25.4.283. [DOI] [PubMed] [Google Scholar]
- 26.Kinch AP, Taylor H, Warltier R, Oliver RG, Newcombe RG. A clinical trial comparing the failure rates of directly bonded brackets using etch times of 15 or 60 seconds. Am J Orthod Dentofacial Orthop. 1988;94:476–483. doi: 10.1016/0889-5406(88)90005-4. [DOI] [PubMed] [Google Scholar]
- 27.Lovius BB, Pender N, Hewage S, O'Dowling I, Tomkins A. A clinical trial of a light activated bonding material over an 18 month period. Br J Orthod. 1987;14:11–20. doi: 10.1179/bjo.14.1.11. [DOI] [PubMed] [Google Scholar]
- 28.Trimpeneers LM, Dermaut LR. A clinical trial comparing the failure rates of two orthodontic bonding systems. Am J Orthod Dentofacial Orthop. 1996;110:547–550. doi: 10.1016/s0889-5406(96)70064-1. [DOI] [PubMed] [Google Scholar]
- 29.Chung CH, Piatti A. Clinical comparison of the bond failure rates between fluoride-releasing and non-fluoride-releasing composite resins. J Clin Orthod. 2000;34:409–412. [PubMed] [Google Scholar]
- 30.Mizrahi E. Success and failure of banding and bonding. A clinical study. Angle Orthod. 1982;52:113–117. doi: 10.1043/0003-3219(1982)052<0113:SAFOBA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Kula K, Schreiner R, Brown J, Glaros A. Clinical bond failure of pre-coated and operator-coated orthodontic brackets. Orthod Craniofac Res. 2002;5:161–165. doi: 10.1034/j.1600-0544.2002.02199.x. [DOI] [PubMed] [Google Scholar]
- 32.Whittaker DK. Structural variations in the surface zone of human tooth enamel observed by scanning electron microscopy. Arch Oral Biol. 1982;27:383–392. doi: 10.1016/0003-9969(82)90147-9. [DOI] [PubMed] [Google Scholar]
- 33.Zach L, Cohen G. Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol. 1965;19:515–530. doi: 10.1016/0030-4220(65)90015-0. [DOI] [PubMed] [Google Scholar]
- 34.Malkoc S, Uysal T, Usumez S, Isman E, Baysal A. In-vitro assessment of temperature rise in the pulp during orthodontic bonding. Am J Orthod Dentofacial Orthop. 2010;137:379–383. doi: 10.1016/j.ajodo.2008.02.028. [DOI] [PubMed] [Google Scholar]
- 35.Loney RW, Price RB. Temperature transmission of high-output light-curing units through dentin. Oper Dent. 2001;26:516–520. [PubMed] [Google Scholar]