Abstract
Background
More than 1 in 4 Americans report difficulty paying medical bills. Cost-reducing strategies discussed during outpatient physician visits remain poorly characterized.
Objective
We sought to determine how often patients and physicians discuss healthcare costs during outpatient visits and what strategies, if any, they discussed to lower patient out-of-pocket costs.
Design
Retrospective analysis of dialogue from 1,755 outpatient visits in community-based practices nationwide from 2010–2014. The study population included 677 patients with breast cancer, 422 with depression, and 656 with rheumatoid arthritis visiting 56 oncologists, 36 psychiatrists, and 26 rheumatologists, respectively.
Results
Thirty percent of visits contained cost conversations (95% confidence interval [CI], 28 to 32). Forty-four percent of cost conversations involved discussion of cost-saving strategies (95% CI, 40 to 48; median duration, 68 seconds). We identified 4 strategies to lower costs without changing the care plan – in order of overall frequency, (1) Changing logistics of care; (2) Facilitating copay assistance; (3) Providing free samples; (4) Changing/adding insurance plans – and 4 strategies to reduce costs by changing the care plan – (1) Switching to lower-cost alternative therapy/diagnostic; (2) Switching from brand name to generic; (3) Changing dosage/frequency; (4) Stopping/withholding interventions. Strategies were relatively consistent across health conditions, except for switching to lower-cost alternative (more common in breast oncology), and providing free samples (more common in depression).
Limitation
Focus on three conditions with potentially high out-of-pocket costs.
Conclusions
Despite price opacity, physicians and patients discuss a variety of out-of-pocket cost reduction strategies during clinic visits. Almost half of cost discussions mention one or more cost-saving strategies, with more frequent mention of those not requiring care-plan changes.
INTRODUCTION
In 2012, more than 1 in 4 Americans reported difficulty paying medical bills.1,2 This is not an isolated problem of the uninsured; 70% of Americans with medical debt have health insurance.3 Key contributors to high out-of-pocket healthcare costs include increases in patient cost sharing, growth in high deductible healthcare plans, and increased use of expensive biologic or designer drugs.2,4–7 In addition to depleting financial savings and damaging credit, high out-of-pocket medical costs negatively impact quality of life, medication adherence, and a variety of health outcomes.3,6,8–12
Sometimes patients have a choice about how much to pay out-of-pocket for their healthcare services.13,14 They might be able to find financial assistance for the services in question, turn to less expensive alternatives, or forgo the services altogether.15,16 Most patients, however, are not fully informed about these alternatives and may desire assistance from clinicians in identifying cost-reducing options and weighing potential medical-financial trade-offs.2,8,17–19 Indeed, surveys show that 59–80% of patients wish to discuss out-of-pocket costs during clinic visits and 91% of physicians believe that managing patient costs is important.20–23 Accordingly, physician experts and patient advocacy groups contend that out-of-pocket costs ought to be routinely discussed during clinic visits to mitigate or prevent avoidable financial distress.24–27
Despite increased attention on physician-patient cost communication in recent years, many aspects of this topic remain undetermined.28 The prevalence of such discussions is unknown, with wide variation in published estimates from as few as 14–15% of patients ever discussing their healthcare costs with physicians29,30 to as many as 44% of patients discussing their healthcare costs with physicians in a single year.21 Additionally, the duration of physician-patient cost discussions is unknown, given few studies of actual cost communication behavior.31,32 Lastly and perhaps most importantly, the types and frequencies of cost-reducing strategies discussed by physicians and patients remain unclear.
To shed light on these areas, we analyzed naturally occurring dialogue from 1,755 community-based, outpatient clinic visits taking place between 2010–2014. We targeted three clinical settings – breast cancer, depression, and rheumatoid arthritis – since they are prevalent diseases, can be associated with high out-of-pocket costs, and represent the varied contexts of a life-threatening condition, a chronic debilitating condition, and a mental health condition, respectively.8,30,33–35 By exploring the frequency and duration of healthcare cost discussions in these diverse encounters, as well as the cost-reducing strategies addressed therein, we provide novel insights about the out-of-pocket cost management efforts discussed by physicians and patients in outpatient settings.
METHODS
Sample Description
Patient visits were sampled from the Verilogue Point-of-Practice™ database of audio-recorded clinical encounters. Verilogue recruited physicians randomly from available lists of active, board certified physicians, and paid them to record patient visits for the purpose of marketing or health services research. Physicians and patients were unaware of the research questions for which their recorded visits would be used. Patients were approached and consented prior to initiation of the visit; approximately 80% of patients agreed to participate. All protected health information was removed during the transcription process. This study was approved by the Duke University Institutional Review Board.
We obtained the most recent 1,000 encounters for management of breast cancer, depression, and rheumatoid arthritis. From this sample of 3,000 transcripts, we excluded visits that were conducted by primary care physicians, nurse practitioners, or nurses (N=800); occurred outside of the United States (N=350); involved patients less than 18 years of age (N=41); were primarily concerned with management of axial spondyloarthropathy, rather than rheumatoid arthritis (N=42); or contained only physician dictations (N=12). The final sample consisted of 1755 visits: 677 breast oncology encounters, 656 rheumatoid arthritis encounters, and 422 psychiatry encounters. These encounters occurred between May 2010 and February 2014 in outpatient, private-practice offices across the United States. More specifically, visits occurred in 9 major US geographic regions (e.g. New England, Middle Atlantic, Mountain, Pacific), 34 states, and 113 zip codes (see Table 1, Table S1, and Table S2 for additional details). Visits were classified as taking place in urbanized areas, urban clusters, or rural areas by matching zip codes in our sample with population measures from the 2010 US Census, and applying definitions formalized in the Urban Area Criteria for the 2010 Census.36
Table 1.
Physician, Patient, and Visit Characteristics*
| Characteristics | Breast Cancer | Depression | Rheumatoid Arthritis |
|---|---|---|---|
| Patients (N) | 677 | 422 | 656 |
|
| |||
| Age, years (%) | |||
| 19–34 | 1 | 23 | 5 |
| 35–54 | 28 | 44 | 29 |
| 55–74 | 54 | 33 | 53 |
| 75+ | 17 | 1 | 13 |
|
| |||
| Gender, Female (%) | 99 | 66 | 78 |
|
| |||
| Race (%) | |||
| Caucasian | 71 | 83 | 75 |
| African-American | 19 | 7 | 11 |
| Hispanic | 6 | 5 | 9 |
| Other | 4 | 4 | 5 |
|
| |||
| Insurance Status (%) | |||
| Private | 49 | 49 | 54 |
| Public | 51 | 43 | 41 |
| Uninsured | 0 | 8 | 4 |
|
| |||
| Physicians (N) | 56 | 36 | 26 |
|
| |||
| Visits recorded, median (N), (IQR) | 9 (5–19) | 13(4–17) | 28 (5–41) |
|
| |||
| Gender, Male (%) | 89 | 100 | 81 |
|
| |||
| Years in Practice (%) | |||
| 0–10 | 37 | 16 | 11 |
| 11–20 | 44 | 34 | 58 |
| 21–30 | 15 | 44 | 14 |
| 31+ | 4 | 6 | 16 |
|
| |||
| Visit Dates | Jun 2010 – Aug 2013 | May 2010 – Jan 2014 | Mar 2012 – Feb 2014 |
|
| |||
| Visit Locations by US region† (N) | |||
| East North Central | 98 | 105 | 47 |
| East South Central | 23 | 21 | 69 |
| Middle Atlantic | 56 | 85 | 100 |
| Mountain | 80 | 22 | 0 |
| New England | 41 | 39 | 20 |
| Pacific | 74 | 18 | 177 |
| South Atlantic | 222 | 41 | 50 |
| West North Central | 23 | 55 | 102 |
| West South Central | 60 | 36 | 91 |
Values are percentages of total non-missing observations unless otherwise indicated. Less than 1% of observations are missing. Percentage totals do not all sum to 100 due to rounding.
List of states comprising each United States geographic region is provided in the supplementary material. Overall, 34 states and 113 zip codes are represented in our sample.
Abbreviation: IQR indicates inter-quartile range.
Analytic Approach
To mitigate individual coder biases and errors, encounters were analyzed independently by at least two team members. The following cost-related measures were evaluated: (1) Presence or absence of cost conversation; if a cost conversation was present, then (2) duration of the cost conversation; (3) to which intervention the cost conversation was related; (4) discussion of cost-saving strategies. A team member experienced in conversation analysis assessed coder agreement on each of the above measures. In cases of agreement, the corresponding decision was assigned as ‘final’. When discrepant, the final coding decision was decided by group consensus. Team members with clinical experience (PAU, WGH) supervised coder training and discrepancy resolution to ensure proper interpretation of clinical matters. All coding was applied using NVivo software (QSR International Pty Ltd. Version 10, 2014).
Cost-Related Measurements
Visits were first reviewed to determine whether a cost conversation was present. Cost conversation was defined as any mention of the patient’s financial costs or insurance coverage related to a specific intervention. If a cost conversation was present, we determined the initiator, defined as the party making the first explicit statement related to the patient’s health care costs during the clinic visit. We also determined the duration of the cost conversation. Total visit duration was provided for each transcript, but no line-wise time stamps or other direct time indicators were available for this analysis. Accordingly, we calculated cost conversation duration in each clinic visit by multiplying the total number of cost-related words by the average rate of words spoken. This average rate was calculated by dividing total number of words spoken in clinic visits by duration of visit in a random 10% sample of encounters. Our estimate for average speech rate (words per minute, mean ± standard deviation = 164 ± 29) was consistent with average speech rates from prior linguistic analyses.37,38
Additionally, we determined whether each cost conversation contained discussion about cost-saving strategies. We further assessed cost-saving strategies to determine whether they included (1) strategies involving care-plan changes (e.g. replacing an intervention with a lower cost alternative or stopping, withholding, or reducing the amount of an intervention) and (2) strategies NOT involving care-plan changes (e.g. signing up for a copay assistance program, switching pharmacies to get a better price, or changing insurance plans to reduce costs).
Statistical Analysis
We calculated 95% confidence intervals for all proportions using Clopper and Pearson’s exact method.39 We used Pearson’s chi-square test to compare the frequencies of coding measures. Distributions of cost conversation durations were non-normal, so the non-parametric Kruskal-Wallis and Mann-Whitney U tests were used to compare cost discussion durations. Demographic characteristics were compared using Pearson’s Chi-Square test and ANOVA. Since each patient is recorded once, our unit of measurement is the encounter, which we grouped by disease state for ease of presentation. Statistical analyses were performed by W.G.H. and P.A.U using R software (R Core Team (2013), Version 3.0.1, http://www.R-project.org/). The authors had full access to the data and take responsibility for its integrity.
Role of the Funding Source
The Robert Wood Johnson Foundation and the National Institutes of Health provided financial support for this investigation, but had no involvement in the study design, in the collection, analysis, and interpretation of data, or in the preparation of this manuscript.
RESULTS
Study Population
A total of 1,755 outpatient appointments were analyzed in this study. The baseline characteristics of the patients and physicians are shown in Table 1. The age, gender, and insurance coverage distribution for patients are in alignment with national figures. The percentage of male physicians in each setting is higher than national averages at the time of sample collection: 89% male oncologists in our population versus 73% in the entire US, 100% male psychiatrists compared with 65% nationally, and 81% male rheumatologist versus for 63% nationally.40 The median number of visits recorded by each physician was 12 (interquartile range (IQR), 4 to 22).
Visits occurred throughout the United States in 9 geographic regions, 34 states, and 113 zip codes (Tables 1, S1, and S2). Visits were well distributed across the regions, with the highest percentage of visits occurring in the South Atlantic region (18% of the overall sample; comprised of Delaware, District of Columbia, Florida, Georgia, Maryland, Virginia, West Virginia, North and South Carolina), and the lowest percentage of visits occurring in New England (6% of overall sample; comprised of Connecticut and Massachusetts). New York, Georgia, Texas, and Ohio were the states having the greatest numbers of visits, constituting 9%, 9%, 7%, and 6% of the overall sample, respectively. Greater than 90% of visits occurred in urbanized areas (population greater than 50,000) or urban clusters (population 2,500–50,000), and less than 10% of visits occurred in rural areas (population less than 2,500), as defined by the United States Bureau of the Census.36
Frequency, Initiators, and Duration of Cost Conversations
Overall, 527 of 1755 clinic visits (30%, 95% Confidence Interval [CI], 28 to 32) contained conversations about the patient’s healthcare costs. Physicians initiated 58% of cost conversations (95% CI, 53 to 62), whereas patients and their caregivers initiated 40% (95% CI, 36 to 45) and 2% (95% CI, 0 to 3), respectively. Forty-four percent of these 527 cost conversations included discussion of cost-saving strategies (95% CI, 40 to 48), a figure that did not differ significantly across the three clinical settings: breast oncology, 38%; depression, 45%; rheumatoid arthritis, 47%; P=0.23 (Figure 1).
Figure 1.
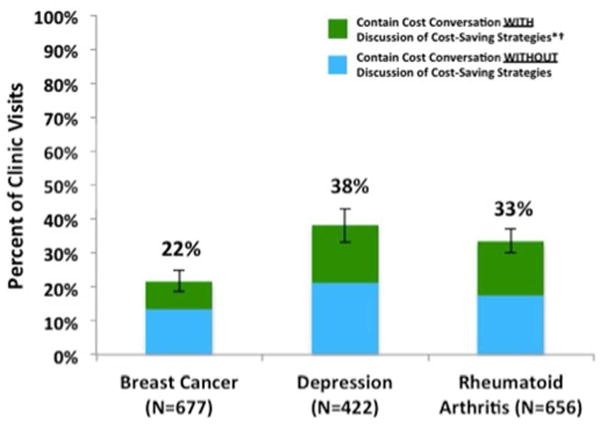
Prevalence of cost conversations with and without discussion of cost-saving strategies. All visits were between patients >18 years old and specialist physicians in community-based clinics across the United States.
*Cost conversation was defined as any mention of the financial costs or insurance coverage associated with the patient’s healthcare.
†Discussion of cost-saving strategy was defined as any mention of one or more methods to reduce the patient’s out-of-pocket costs. No evidence was required that the cost-saving strategy was used or pursued, only that it was discussed.
The median visit length in our study was 9 minutes and 56 seconds (interquartile range (IQR), 6 minutes and 1 second to 13 minutes and 31 seconds). In encounters where patients and physicians discussed cost-saving strategies, they spent a median of 68 seconds discussing healthcare costs (IQR, 34 to 117 seconds), a duration that did not differ across disease settings (P=0.63). Fifty-three percent of these cost conversations lasted longer than 1 minute (Figure 2).
Figure 2.
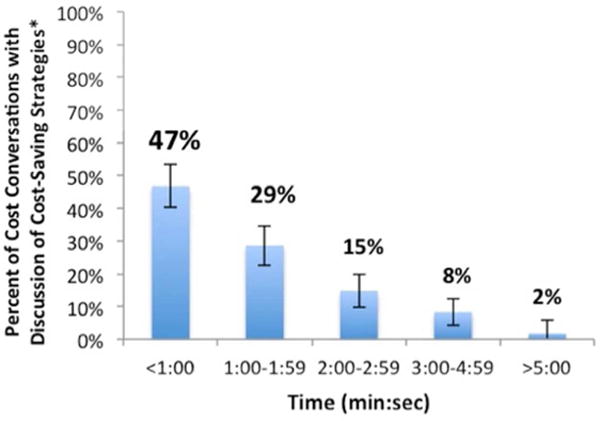
Duration of cost conversations with discussion of cost-saving strategies. The median duration of cost conversations containing discussion of cost-saving strategies (N=231) was 68 seconds (interquartile range, 34 to 117 seconds). The median duration of clinic visits was 9 minutes and 57 seconds.
*Discussion of cost-saving strategy was defined as any mention of one or more methods to reduce the patient’s out-of-pocket costs. No evidence was required that the cost-reducing strategy was used or pursued, only that it was discussed.
Out-of-Pocket Cost Saving Strategies
Patients and physicians discussed a wide range of strategies to lower out-of-pocket costs. (See Table 2 for example quotes.) These strategies can be divided into two broad categories – strategies that lower costs by changing the plan of care, (e.g. switching to lower-cost alternatives), versus strategies that lower costs without changing the plan of care (e.g. obtaining co-pay assistance for a previously prescribed drug). Below we provide more detail on each of these strategies.
Table 2.
Examples of Strategies to Reduce Out-of-Pocket Costs*
| Strategies INVOLVING Care-Plan Changes | |
|---|---|
| Switch to Lower Cost Alternative Therapy or Diagnostic Plan | DR: Need anything else? PT: The one I take for my ulcer…what do you call that? DR: Omeprazole? Zantac? Nexium? PT: Nexium. DR: That’s expensive though. PT: Ain’t no more expensive than the Micardis I have to pay for. DR: How much is that? PT: $150. DR: Why don’t you ask the pharmacist which [peptic ulcer medication] is the least expensive and have him call me. |
| Switch to Generic Form of Same Medication | DR: I’m going to put you on the generic one, alendronate, which is a cheaper version, but with the same instructions. |
| Stop or Withhold Intervention | DR: Do you want the tramadol where you could take it as needed for pain? PT: Um, I guess I could try it. I mean I don’t know. DR: We could try 60 of them. It’s a generic, so hopefully the cost would not be bad…if it was bad, you could just say, no, I’ll skip it. |
| Changing Dose or Frequency of Intervention | PT: Last time I was here, we were going to go with 40 mg of Oxycontin…. We were going to do it three times a day, but that’s not going to work for me. DR: What’s going to work for you? PT: I have to spend $200 on pain medication, that’s how much those pills cost me…. So, I’d rather just go back to the 80s. |
| Strategies NOT INVOLVING Care-Plan Changes | |
| Changing Logistics of Intervention | DR: For this medication, it’s cheaper to buy it directly from the company, rather than from the pharmacy. [The company] won’t mark it up. They sell it for, I think, $48 a month. |
| Facilitating Copay Assistance or Charity Care | DR: The copay you have with the Xgeva, there’s supposed to be copay assistance programs and all. Did you look into those? |
| Free Samples | DR: What are your thoughts? Do you feel it’s best to stay off the Abilify? We can get you samples of it…I don’t want cost to be the issue. PT: Well, that’s the big issue, that’s why I’ve been off of it. |
| Change or Add Insurance Plans | DR: If you get a secondary coverage, they would pay [for your infusions]. Have you looked into getting a secondary? CG: We’ve called everywhere… PT: Because of my age. DR: You’re too young? CG: Yes. Does the Medicare part D pay for those [infusions]? DR: They pay on the prescriptions…but that’s another good alternative, to get a part D plan. DR: Right now, are you paying for your prescriptions? CG: Yeah. DR: But that’s something that I would definitely consider…is to get on a part D plan. |
Fillers (e.g. “um”, “you know”) have been removed from dialogue for brevity and punctuation has been added to improve readability.
Abbreviations: DR. indicates doctor; PT., patient; CG, caregiver.
Strategies Involving Care-Plan Changes
1. Switching to a lower cost alternative therapy or diagnostic
In 22% of cost conversations, physicians and patients discussed reducing out-of-pocket costs by switching to lower-cost alternatives (see Table 3). This strategy was discussed significantly more often in breast oncology encounters than depression and rheumatoid arthritis (P=0.01). For example, when treating bone metastases in elderly women with breast cancer, some oncologists proposed reducing out-of-pocket costs by switching patients from oral therapies with high copays (e.g. Boniva, Fosamax) to intravenous infusion therapies (e.g. Zometa), which were described as having little or no copays. When treating rheumatoid arthritis, rheumatologists sometimes proposed reducing out-of-pocket costs by switching patients from in-office infusions (e.g. Remicade, Rituxan) or injections (e.g. Enbrel, Humira) to cheaper, oral, non-biologic agents (e.g. Plaquenil, Arava). In general, switching to a lower cost alternative almost exclusively applied to medications; however, there were a few instances in which physicians and patients discussed switching to lower cost alternatives for procedures. For example, in one encounter, a psychiatrist discussed the cost-savings associated with using electroconvulsive therapy for depression treatment instead of transcranial magnetic stimulation, since the latter would not be covered by Medicare.
Table 3.
Cost-Saving Strategies Discussed in Three Clinical Settings
| Overall Sample (N=231) | Breast Cancer (N=56) | Depression (N=72) | Rheumatoid Arthritis (N=103) | P* | |
|---|---|---|---|---|---|
| Strategies INVOLVING Care-Plan Changes | |||||
| Changing to Lower Cost Alternative Intervention | 22% | 34% | 15% | 20% | 0.01 |
| Switching to Generic Form of Intervention | 7% | 11% | 7% | 5% | 0.33 |
| Changing Dosage/Frequency of Intervention | 5% | 5% | 8% | 3% | 0.29 |
| Stopping or Withholding Intervention | 4% | 2% | 4% | 5% | 0.52 |
| TOTAL: Any Strategy INVOLVING Care-Plan Changes | 38% | 51% | 34% | 34% | 0.04 |
| Strategies NOT Involving Care-Plan Changes | |||||
| Changing Logistics of Care | 23% | 23% | 21% | 25% | 0.80 |
| Facilitating Co-pay Assistance or Coupons | 21% | 14% | 21% | 25% | 0.18 |
| Providing Free Samples | 13% | 6% | 23% | 9% | <0.01 |
| Changing or Adding Insurance Plans | 5% | 6% | 2% | 7% | 0.18 |
| TOTAL: Any Strategy WITHOUT Care-Plan Changes | 63% | 49% | 66% | 66% | 0.04 |
Percentages represent the portion of all cost-reducing strategies discussed in the overall sample or disease setting as indicated. Values do not all sum to their respective totals due to rounding.
P values are results of omnibus chi-square tests comparing frequencies across the three disease settings.
2. Switching from a brand name drug to its generic formulation
In 7% of cost conversations, physicians and patients discussed switching to generics as a method of reducing the patient’s costs. Cost conversations involving this strategy were usually brief (median duration, 28 seconds, IQR 10 to 64 seconds).
3. Changing dosage or frequency of intervention
In 5% of cost conversations, physicians and patients discussed reducing out-of-pocket costs by changing the dosage or frequency of medications, office visits or diagnostic tests. For example, when patients complained about the costs of PET scans, some physicians responded by offering patients the option of undergoing PET scans less frequently. Similarly, when patients with depression brought up high copays for psychotherapy, psychiatrists suggested reducing the amount of therapy by moving from weekly therapy sessions to monthly or bimonthly sessions.
4. Stopping or withholding interventions
In 4% of cost conversations, patients and physicians discussed reducing out-of-pocket costs by stopping or withholding interventions. This strategy was least frequent in breast cancer encounters, with only one of 677 breast oncology encounters involving discussion of discontinuing a chemotherapeutic agent to reduce out-of-pocket costs (Table 3). In depression and rheumatology settings, this strategy was suggested as a sort of contingency plan, with the physician recommending that the patient forgo the medication in question if they found their copay to be too high when filling it at the pharmacy. In most of these cases, the physician admitted lack of knowledge with regards to the expected costs, and thus discussed this strategy as a means of protecting patients against potentially high out-of-pocket costs.
Strategies NOT Involving Care-Plan Changes
1. Changing Logistics of Care
In 23% of cost conversations, patients and physicians discussed reducing out-of-pocket costs by changing the timing, source, or location of the patient’s healthcare. When discussing medications, physicians often suggested that patients’ fill prescriptions at particular pharmacies to save money. In other cases, patients requested that physicians write their prescriptions in a manner that would result in the lowest possible copays. For instance, several patients requested 90-day supplies of their medications instead of 30-day supplies, since the former resulted in lower total copays over the course of the year. Purchasing medications from outside the United States was only discussed in one visit as a means to reduce out-of-pocket costs.
When discussing diagnostic tests, physicians and patients often mentioned the status of their deductible, and scheduled the tests in a way that would minimize out-of-pocket costs. For example, positron emission tomography and radionuclide angiography tests were noted to be expensive in the setting of breast cancer, and were often scheduled at the end of the calendar year to take advantage of the better coverage for patients who had already met their deductible. This scheduling of diagnostic tests to minimize out-of-pocket costs was carried out even if the timing was not in alignment with evidence-based surveillance guidelines. When discussing procedures, physicians sometimes suggested that the patient get as many pertinent procedures performed at the same time to save money; for instance, one physician encouraged his patient to undergo a breast reconstruction and reduction at the same time to minimize costs, effectively getting “two things done for the price of one.”
2. Facilitating Copay Assistance or Drug Coupons
In 21% of cost conversations, patients and physicians discussed reducing out-of-pocket costs through co-pay assistance or drug coupons. This strategy was most commonly brought up by physicians when starting patients on new brand-name medications. While copay assistance programs, drug coupons, and charity foundations were mentioned as helpful means of reducing the patients’ costs, very rarely did physicians and patients mention (a) how long patients would be eligible to benefit from these programs or (b) how much they would actually reduce out-of-pocket costs for potentially expensive medications such as biologic anti-rheumatic drugs or newer brand name chemotherapeutics for breast cancer.
3. Providing Free Samples to Reduce Patient Costs
In 13% of cost conversations, patients and physicians discussed reducing out-of-pocket costs through the use of free samples. This was the most frequently discussed strategy in the setting of depression (23% of cost-saving strategies in depression; Table 3). At times, patients and physicians discussed samples as a way to start or continue an otherwise cost-prohibitive medication (Table 1). Additionally, free samples were discussed as a way in which patients could try out new medications for several weeks to determine its short-term effectiveness without having to pay out-of-pocket. Samples were most frequently brand name drugs, and discussions of them rarely mentioned the out-of-pocket costs that the patient would face when actually filling the corresponding prescription.
4. Changing or Adding Insurance Plans
In 5% of cost conversations, patients and physicians discussed reducing out-of-pocket costs by changing or adding insurance plans. This strategy often came up in visits with elderly patients who had Medicare but did not have a supplemental insurance plan covering prescription drugs. When these patients complained about high costs related to their prescription medications, physicians queried about their insurance status and encouraged them to enroll in supplemental plans to help decrease their out-of-pocket expenses for medications. Additionally, we observed a number of circumstances in which physicians encouraged their patients to apply for disability as a means of reducing their out-of-pocket costs.
DISCUSSION
Despite receiving greater attention in recent years,24–27 physician-patient communication about out-of-pocket costs has remained poorly characterized.28 Published estimates of the prevalence of such discussions vary widely, with some surveys suggesting fewer than 1 in 6 patients ever discuss healthcare costs with their physicians.20,41 In contrast, this analysis of actual clinical dialogue found that cost conversations occur more commonly - in approximately 1 in 5 breast cancer visits and 1 in 3 depression and rheumatoid arthritis visits. We also found that the majority of cost conversations were initiated by physicians. Importantly, nearly half of all cost conversations involved discussion of cost-saving strategies, which on average lasted about one minute. Our results demonstrate that despite price opacity and time-pressure in outpatient visits, physicians are willing and able to engage with their patients about cost-related issues and discuss a wide array of cost-saving strategies to lower out-of-pocket costs.42
Importantly, physicians and patients most frequently discussed cost-reducing strategies that did not involve care-plan changes. Specifically, copay assistance programs, drug coupons, and free samples accounted for over one-third of all strategies mentioned. Although these strategies often provide robust short-term cost-savings,43,44 their long-term effect on patients’ out-of-pocket costs is unclear.45–47 After the assistance expires or they no longer meet eligibility requirements, patients may find themselves facing the full copay for brand name drugs, which may be burdensome or even prohibitive (e.g. DR: Have you taken Provigil or Nuvigil before? PT: You got me a free sample online, and then my insurance wouldn’t cover it.)46,48 In contrast, strategies involving care-plan changes, such as switching to a lower cost alternative, using generics, and stopping or withholding interventions, are neither subject to expiration dates nor potential eligibility issues and may be more likely to result in long-term cost-savings.
While our study shows that cost conversations are more frequent than some prior surveys suggested,29,30,41 and that such conversations regularly lead to discussion of strategies to reduce patient out-of-pocket costs, it in no way establishes that such conversations are as productive as they could be. In some encounters, neither patients nor physicians could accurately determine the cost of specific interventions and struggled to figure out what could be done to reduce out-of-pocket costs. Frustration with the complexities of healthcare reimbursement was a recurring theme throughout these conversations. Greater price transparency and more comprehensible information on insurance coverage could alleviate some of these difficulties and facilitate identification of cost-saving options.19,42 Further development of pricing applications that provide real-time, individualized copay estimates may address these barriers.
Our findings have important clinical and policy implications. Despite Medicaid expansion and closure of key coverage gaps, over a quarter of Americans still report financial burden due to their medical bills, either paying these bills late or not paying them at all.1–3 This is occurring in the context of widespread increases in patient cost-sharing and rapid growth in enrollment in high-deductible health plans.2,4–7 Consequently, Americans have more financial ‘skin in the game’ than ever before, and 59–80% of patients want to discuss healthcare costs with their physicians.20,49–51 With nearly half of cost discussions involving cost-reducing strategies, our findings suggest that patient-physician discussion about out-of-pocket costs may be a helpful tool in addressing patients’ financial distress. However, since the majority of clinic visits did not contain cost discussions, our study may highlight a need for additional efforts in promoting physician-patient cost communication.20–27 Systematic screening for healthcare related financial distress on intake questionnaires and initial nursing evaluations could enhance physician and patient awareness of cost concerns, potentially prompting further discussion as is routinely done for physical or mental health complaints. While these interventions may increase prevalence of cost discussion, targeted educational initiatives may be needed to improve the quality of these discussions, as few physicians or nurses have received formalized training on effective cost communication.
Even if physicians and patients are cognizant of relevant cost concerns, they still must overcome additional barriers to discuss these costs during clinic visits. One often-cited barrier to cost communication is the perception of insufficient time to discuss costs in already rushed clinic visits.24,42 Interestingly, these perceptions do not seem to be based in any objective data; to our knowledge, this investigation features the first analysis of cost discussion duration to date. Herein, we observed that cost conversations involving discussion of cost-reducing strategies lasted approximately one minute, which often constituted 10% or more of the total visit time. Such a time commitment may still seem prohibitive to some clinicians; thus, further work will be required to characterize communication practices that not only improve the quality and patient-centeredness of cost discussions, but also their efficiency.
Our study has several limitations. First, the population in our study limits the generalizability of our findings. However, given the relatively large sample size (in comparison to other analyses of actual dialogue), geographic diversity, and variety in patient age and type of insurance coverage, our study has broader generalizability than populations studied to date. Second, we had access to one visit per patient, so we could not determine whether cost was discussed during visits prior to the ones we analyzed. It is possible that some of these patients discussed out-of-pocket costs on earlier visits, thereby reducing the necessity of discussing this topic during the recorded encounter. Third, our study focused on three health conditions, which we chose because they may expose patients to high out-of-pocket costs and represent varied contexts of a life-threatening condition (breast cancer), a chronic debilitating condition (rheumatoid arthritis), and a mental health condition (depression).8,30,33–35 Other clinical conditions may have very different rates of cost discussion. Fourth, our study focused on identifying and characterizing the strategies patients and physicians discussed to lower out-of-pocket costs; it was not designed to identify available strategies that neither party discussed during the encounter.
CONCLUSIONS
In this investigation of actual clinical dialogue from outpatient clinics, we observed physicians and patients discussing a wide variety of cost-reducing strategies to lower patients’ out-of-pocket costs. These strategies were mentioned in nearly half of all visits containing any discussion of the patient’s healthcare costs, with the majority mentioning strategies not requiring care-plan changes. In encounters where patients and physicians discuss strategies to lower out-of-pocket costs, such discussions lasted about one minute. Although brief in absolute terms, this often comprised more than 10% of the total encounter, which could present a barrier to more frequent cost communication. Overall, we found that almost one-third of visits included discussion of healthcare costs, which was higher than some prior surveys.20,30,41 The majority of these cost conversations were initiated by physicians. Further investigation is needed to determine effective and efficient cost communication strategies and assess the impact of such communication on subsequent financial distress, health outcomes, and overall patient satisfaction.
Supplementary Material
Acknowledgments
Contributors: We thank Annabel Wang, Carmen Cummings B.A., M.P.P., and Robin Fail B.A., M.P.P., for their assistance in data analysis.
Funding: Financial support for this study was provided in part by a grant from the Robert Wood Johnson Foundation to Dr. Ubel. Additional support was provided to Mr. Hunter by training grant TL1TR001116 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The content of this article is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health or the Robert Wood Johnson Foundation. These funding agreements ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Footnotes
Prior Presentations: This work was previously presented at the AcademyHealth Annual Research Meeting (June 15, 2015) and the Duke Alpha Omega Alpha Student Research Day (August 7, 2015).
Conflicts of interest: Ashley Hesson, Ph.D was previously employed and served as a consultant to Verilogue Inc.; Jamison Barnett B.A., M.S., is co-founder and chief technical officer of Verilogue Inc.; Peter Ubel, M.D. serves as a consultant to Humana.
Contributor Information
Cecilia Z. Zhang, Email: Cecilia.z.zhang@dm.duke.edu.
Ashley Hesson, Email: Ashley.bartell@gmail.com.
J. Kelly Davis, Email: jkelly.davis@duke.edu.
Christine Kirby, Email: Christine.kirby@duke.edu.
Lillie D. Williamson, Email: lilliewilliamson11@gmail.com.
Jamison A. Barnett, Email: jbarnett@verilogue.com.
Peter A. Ubel, Email: peter.ubel@duke.edu.
References
- 1.Richman IB, Brodie M. A National study of burdensome health care costs among non-elderly Americans. BMC Health Serv Res. 2014;14(1):435. doi: 10.1186/1472-6963-14-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen RA, Kirzinger WK. Financial burden of medical care: a family perspective. NCHS Data Brief. 2014;142:1–8. [PubMed] [Google Scholar]
- 3.Pollitz K, Cox C, Lucia K, Keith K. Medical Debt among People with Health Insurance. 2014 Jan; http://kff.org/private-insurance/report/medical-debt-among-people-with-health-insurance/.
- 4.Dolan PL. High-deductible impact. Balancing rising out-of-pocket costs and outcomes. Med Econ. 2014;91(9):17–20. doi: 10.1111/j.1475-6773.2010.01191.x. [DOI] [PubMed] [Google Scholar]
- 5.Dusetzina SB, Winn AN, Abel GA, Huskamp HA, Keating NL. Cost Sharing and Adherence to Tyrosine Kinase Inhibitors for Patients With Chronic Myeloid Leukemia. J Clin Onc. 2014;32(4):306–311. doi: 10.1200/JCO.2013.52.9123. [DOI] [PubMed] [Google Scholar]
- 6.Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381–390. doi: 10.1634/theoncologist.2012-0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harrold LR, Peterson D, Beard AJ, Gurwitz JH, Briesacher BA. Time trends in medication use and expenditures in older patients with rheumatoid arthritis. Am J Med. 2012;125(9):937.e9–e15. doi: 10.1016/j.amjmed.2011.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zafar SY, Abernethy AP. Financial toxicity, Part I: a new name for a growing problem. Oncology (Williston Park, NY) 2013;27(2):80-1–149. [PMC free article] [PubMed] [Google Scholar]
- 9.Cook K, Dranove D, Sfekas A. Does Major Illness Cause Financial Catastrophe? Health Serv Res. 2010;45(2):418–436. doi: 10.1111/j.1475-6773.2009.01049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Himmelstein DU, Thorne D, Warren E, Woolhandler S. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122(8):741–746. doi: 10.1016/j.amjmed.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 11.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 12.Neugut AI, Subar M, Wilde ET, et al. Association between prescription co-payment amount and compliance with adjuvant hormonal therapy in women with early-stage breast cancer. J Clin Oncol. 2011;29(18):2534–2542. doi: 10.1200/JCO.2010.33.3179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cox C. Medical Debt among People with Health Insurance. 2014 Jan;:1–43. [Google Scholar]
- 14.Beach MC, Asch DA, Jepson C, et al. Public response to cost-quality tradeoffs in clinical decisions. Med Decis Making. 2003;23(5):369–378. doi: 10.1177/0272989X03256882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tseng CW, Brook RH, Keeler E, Steers WN, Mangione CM. Cost-lowering strategies used by Medicare beneficiaries who exceed drug benefit caps and have a gap in drug coverage. JAMA. 2004;292(8):952–960. doi: 10.1001/jama.292.8.952. [DOI] [PubMed] [Google Scholar]
- 16.Alexander GC, Tseng C-W. Six strategies to identify and assist patients burdened by out-of-pocket prescription costs. Cleve Clin J Med. 2004;71(5):433–437. doi: 10.3949/ccjm.71.5.433. [DOI] [PubMed] [Google Scholar]
- 17.Wong Y-N, Egleston BL, Sachdeva K, et al. Cancer patients’ trade-offs among efficacy, toxicity, and out-of-pocket cost in the curative and noncurative setting. Med Care. 2013;51(9):838–845. doi: 10.1097/MLR.0b013e31829faffd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brill S. Bitter Pill: Why Medical Bills Are Killing Us. Time. 2013 Feb; [Google Scholar]
- 19.Farrell KS, Finocchio LJ, Trivedi AN, Mehrotra A. Does price transparency legislation allow the uninsured to shop for care? J Gen Intern Med. 2010;25(2):110–114. doi: 10.1007/s11606-009-1176-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alexander GC. Patient-Physician Communication About Out-of-Pocket Costs. JAMA. 2003;290(7):953–958. doi: 10.1001/jama.290.7.953. [DOI] [PubMed] [Google Scholar]
- 21.Schmittdiel JA, Steers N, Duru OK, et al. Patient-provider communication regarding drug costs in Medicare Part D beneficiaries with diabetes: a TRIAD Study. BMC Health Serv Res. 2010;10(1):164. doi: 10.1186/1472-6963-10-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pham HH, Alexander GC, O’Malley AS. Physician consideration of patients’ out-of-pocket costs in making common clinical decisions. Arch Intern Med. 2007;167(7):663–668. doi: 10.1001/archinte.167.7.663. [DOI] [PubMed] [Google Scholar]
- 23.Shrank WH. Physicians“ Perceived Knowledge of and Responsibility for Managing Patients” Out-of-Pocket Costs for Prescription Drugs. Ann Pharmacotherapy. 2006;40(9):1534–1540. doi: 10.1345/aph.1H158. [DOI] [PubMed] [Google Scholar]
- 24.Riggs KR, Ubel PA. Overcoming Barriers to Discussing Out-of-Pocket Costs With Patients. JAMA Intern Med. 2014;174(6):849–850. doi: 10.1001/jamainternmed.2014.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ubel PA, Abernethy AP, Zafar SY. Full disclosure—out-of-pocket costs as side effects. N Engl J Med. 2013;369(16):1484–1486. doi: 10.1056/nejmp1306826. [DOI] [PubMed] [Google Scholar]
- 26.Moriates C, Shah NT, Arora VM. First, Do No (Financial) Harm. JAMA. 2013;310(6):577–578. doi: 10.1001/jama.2013.7516. [DOI] [PubMed] [Google Scholar]
- 27.Zafar SY, Tulsky JA, Abernethy AP. It’s time to have ‘the talk’: cost communication and patient-centered care. Oncology (Williston Park, NY) 2014;28(6):479–480. [PMC free article] [PubMed] [Google Scholar]
- 28.Hunter WG, Ubel PA. The Black Box of Out-of-Pocket Cost Communication. A Path Toward Illumination. Ann Am Thorac Soc. 2014;11(10):1608–1609. doi: 10.1513/AnnalsATS.201410-475ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. JAMA. 2003;290(7):953–958. doi: 10.1001/jama.290.7.953. [DOI] [PubMed] [Google Scholar]
- 30.Bestvina CM, Zullig LL, Rushing C, et al. Patient-oncologist cost communication, financial distress, and medication adherence. J Oncol Pract. 2014;10(3):162–167. doi: 10.1200/JOP.2014.001406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beard AJ, Sleath B, Blalock SJ, et al. Predictors of rheumatoid arthritis patient-physician communication about medication costs during visits to rheumatologists. Arthritis Care Res. 2010;62(5):632–639. doi: 10.1002/acr.20083. [DOI] [PubMed] [Google Scholar]
- 32.Tarn DM, Paterniti DA, Heritage J, Hays RD, Kravitz RL, Wenger NS. Physician communication about the cost and acquisition of newly prescribed medications. Am J Manag Care. 2006;12(11):657–664. [PubMed] [Google Scholar]
- 33.Dennehy EB, Robinson RL, Stephenson JJ, et al. Impact of non-remission of depression on costs and resource utilization: from the COmorbidities and symptoms of DEpression (CODE) study. Curr Med Res Opin. 2015;31(6):1165–1177. doi: 10.1185/03007995.2015.1029893. [DOI] [PubMed] [Google Scholar]
- 34.Choi S, Hasche L, Nguyen D. Effects of depression on the subsequent year’s healthcare expenditures among older adults: two-year panel study. Psychiatr Q. 2015;86(2):225–241. doi: 10.1007/s11126-014-9324-4. [DOI] [PubMed] [Google Scholar]
- 35.Wolfe F, Michaud K. Out-of-pocket expenses and their burden in patients with rheumatoid arthritis. Arthritis & Rheumatism. 2009;61(11):1563–1570. doi: 10.1002/art.24724. [DOI] [PubMed] [Google Scholar]
- 36.Bureau of the Census. Urban Area Criteria for the 2010 Census. Federal Register. 2011;76(164):1–15. http://www2.census.gov/geo/pdfs/reference/fedreg/fedregv76n164.pdf. Last accessed Nov 27, 2015. [Google Scholar]
- 37.Pimsieur P, Hancock C, Furey P. Speech rate and listening comprehension. In: Burt MK, Dulay HC, Finocchiaro MB, editors. Viewpoints on English as a Second Language. 1977. p. 265. Vol. [Google Scholar]
- 38.Tauroza S, Allison D. Speech Rates in British English. Applied Linguistics. 1990;11(1):90–105. doi: 10.1093/applin/11.1.90. [DOI] [Google Scholar]
- 39.Clopper CJ, Pearson ES. The Use of Confidence or Fiducial Limits Illustrated in the Case of the Binomial. Biometrika. 1934;26(4):404–413. [Google Scholar]
- 40.2012 Physician Specialty Databook. 2012 Nov;:1–43. [Google Scholar]
- 41.Irwin B, Kimmick G, Altomare I, et al. Patient experience and attitudes toward addressing the cost of breast cancer care. Oncologist. 2014;19(11):1135–1140. doi: 10.1634/theoncologist.2014-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alexander GC, Casalino LP, Tseng C-W, McFadden D, Meltzer DO. Barriers to patient-physician communication about out-of-pocket costs. J Gen Intern Med. 2004;19(8):856–860. doi: 10.1111/j.1525-1497.2004.30249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Starner CI, Alexander GC, Bowen K, Qiu Y, Wickersham PJ, Gleason PP. Specialty drug coupons lower out-of-pocket costs and may improve adherence at the risk of increasing premiums. Health Aff (Millwood) 2014;33(10):1761–1769. doi: 10.1377/hlthaff.2014.0497. [DOI] [PubMed] [Google Scholar]
- 44.Choudhry NK, Lee JL, Agnew-Blais J, Corcoran C, Shrank WH. Drug Company-Sponsored Patient Assistance Programs: A Viable Safety Net? Health Aff (Millwood) 2009;28(3):827–834. doi: 10.1377/hlthaff.28.3.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ross JS, Kesselheim AS. Prescription-drug coupons–no such thing as a free lunch. N Engl J Med. 2013;369(13):1188–1189. doi: 10.1056/NEJMp1301993. [DOI] [PubMed] [Google Scholar]
- 46.Don’t get hooked on prescription–drug coupons. Consumer Reports. 2012 Mar; http://www.consumerreports.org/cro/2012/03/don-t-get-hooked-on-prescription-drug-coupons/index.htm.
- 47.Felder TM, Palmer NR, Lal LS, Mullen PD. What is the evidence for pharmaceutical patient assistance programs? A systematic review. J Health Care Poor Underserved. 2011;22(1):24–49. doi: 10.1353/hpu.2011.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pollack A. Coupons for Patients, but Higher Bills for Insurers. The New York Times. http://www.nytimes.com/2011/01/02/business/02coupon.html. Published January 2, 2011.
- 49.Bullock AJ, Hofstatter EW, Yushak ML, Buss MK. Understanding patients’ attitudes toward communication about the cost of cancer care. J Oncol Pract. 2012;8(4):e50–e58. doi: 10.1200/JOP.2011.000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tseng C-W, Dudley RA, Brook RH, et al. Elderly patients’ preferences and experiences with providers in managing their drug costs. J Am Geriatr Soc. 2007;55(12):1974–1980. doi: 10.1111/j.1532-5415.2007.01445.x. [DOI] [PubMed] [Google Scholar]
- 51.Danis M, Sommers R, Logan J, et al. Exploring Public Attitudes Towards Approaches to Discussing Costs in the Clinical Encounter. J Gen Intern Med. 2014;29(1):223–229. doi: 10.1007/s11606-013-2543-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


