Abstract
Background
Acupuncture is often used for prevention of tension‐type headache but its effectiveness is still controversial. This is an update of our Cochrane review originally published in Issue 1, 2009 of The Cochrane Library.
Objectives
To investigate whether acupuncture is a) more effective than no prophylactic treatment/routine care only; b) more effective than 'sham' (placebo) acupuncture; and c) as effective as other interventions in reducing headache frequency in adults with episodic or chronic tension‐type headache.
Search methods
We searched CENTRAL, MEDLINE, EMBASE and AMED to 19 January 2016. We searched the World Health Organization (WHO) International Clinical Trials Registry Platform to 10 February 2016 for ongoing and unpublished trials.
Selection criteria
We included randomised trials with a post‐randomisation observation period of at least eight weeks, which compared the clinical effects of an acupuncture intervention with a control (treatment of acute headaches only or routine care), a sham acupuncture intervention or another prophylactic intervention in adults with episodic or chronic tension‐type headache.
Data collection and analysis
Two review authors checked eligibility; extracted information on participants, interventions, methods and results; and assessed study risk of bias and the quality of the acupuncture intervention. The main efficacy outcome measure was response (at least 50% reduction of headache frequency) after completion of treatment (three to four months after randomisation). To assess safety/acceptability we extracted the number of participants dropping out due to adverse effects and the number of participants reporting adverse effects. We assessed the quality of the evidence using GRADE (Grading of Recommendations Assessment, Development and Evaluation).
Main results
Twelve trials (11 included in the previous version and one newly identified) with 2349 participants (median 56, range 10 to 1265) met the inclusion criteria.
Acupuncture was compared with routine care or treatment of acute headaches only in two large trials (1265 and 207 participants), but they had quite different baseline headache frequency and management in the control groups. Neither trial was blinded but trial quality was otherwise high (low risk of bias). While effect size estimates of the two trials differed considerably, the proportion of participants experiencing at least 50% reduction of headache frequency was much higher in groups receiving acupuncture than in control groups (moderate quality evidence; trial 1: 302/629 (48%) versus 121/636 (19%); risk ratio (RR) 2.5; 95% confidence interval (CI) 2.1 to 3.0; trial 2: 60/132 (45%) versus 3/75 (4%); RR 11; 95% CI 3.7 to 35). Long‐term effects (beyond four months) were not investigated.
Acupuncture was compared with sham acupuncture in seven trials of moderate to high quality (low risk of bias); five large studies provided data for one or more meta‐analyses. Among participants receiving acupuncture, 205 of 391 (51%) had at least 50% reduction of headache frequency compared to 133 of 312 (43%) in the sham group after treatment (RR 1.3; 95% CI 1.09 to 1.5; four trials; moderate quality evidence). Results six months after randomisation were similar. Withdrawals were low: 1 of 420 participants receiving acupuncture dropped out due to adverse effects and 0 of 343 receiving sham (six trials; low quality evidence). Three trials reported the number of participants reporting adverse effects: 29 of 174 (17%) with acupuncture versus 12 of 103 with sham (12%; odds ratio (OR) 1.3; 95% CI 0.60 to 2.7; low quality evidence).
Acupuncture was compared with physiotherapy, massage or exercise in four trials of low to moderate quality (high risk of bias); study findings were inadequately reported. No trial found a significant superiority of acupuncture and for some outcomes the results slightly favoured the comparison therapy. None of these trials reported the number of participants dropping out due to adverse effects or the number of participants reporting adverse effects.
Overall, the quality of the evidence assessed using GRADE was moderate or low, downgraded mainly due to a lack of blinding and variable effect sizes.
Authors' conclusions
The available results suggest that acupuncture is effective for treating frequent episodic or chronic tension‐type headaches, but further trials ‐ particularly comparing acupuncture with other treatment options ‐ are needed.
Keywords: Humans, Acupuncture Therapy, Acupuncture Therapy/methods, Exercise, Massage, Physical Therapy Modalities, Randomized Controlled Trials as Topic, Tension‐Type Headache, Tension‐Type Headache/prevention & control
Plain language summary
Acupuncture for tension‐type headache
Bottom line
The available evidence suggests that a course of acupuncture consisting of at least six treatment sessions can be a valuable option for people with frequent tension‐type headache.
Background
Tension‐type headache is a common type of headache. Mild episodes may be treated adequately by pain‐killers. In some individuals, however, tension‐type headache occurs frequently and significantly impairs their quality of life. Acupuncture is a therapy in which thin needles are inserted into the skin at particular points. It originated in China and is now used in many countries to treat tension‐type headache. We found randomised controlled trials to evaluate whether acupuncture prevents tension‐type headache. We looked mainly at the numbers of people who responded to treatment, which means a halving of the number of days on which they experienced a headache.
Key results
We reviewed 12 trials with 2349 adults, published up to January 2016. One new trial is included in this updated review.
Acupuncture added to usual care or treatment of headaches only on onset (usually with pain‐killers) in two large trials resulted in 48 in 100 participants having headache frequency at least halved, compared to 17 of 100 participants given usual care only.
Acupuncture was compared with 'fake' acupuncture, where needles are inserted at incorrect points or do not penetrate the skin, in six trials. Headache frequency halved in 52 of 100 participants receiving true acupuncture compared with 43 of 100 participants receiving 'fake' acupuncture. The results were dominated by one large, good quality trial (with about 400 participants), which showed that the effect of true acupuncture was still present after six months. There were no differences in the number of side effects of real and 'fake' acupuncture, or the numbers dropping out because of side effects.
Acupuncture was compared with other treatments such as physiotherapy, massage or relaxation in four trials, but these had no useful information.
Quality of the evidence
Overall the quality of the evidence was moderate.
Background
This review is an update of a previously published review in the Cochrane Database of Systematic Reviews (2009, Issue 1) on 'Acupuncture for tension‐type headache' (Linde 2009).
Description of the condition
Patients with tension‐type headache suffer from episodes of pain that is typically bilateral, pressing or tightening in quality, of mild to moderate intensity, and which does not worsen with routine physical activity (IHS 2004; IHS 2013). There is no nausea, but photophobia or phonophobia (fear of bright light or loud sounds) may be present. Infrequent episodic tension‐type headache (episodes of headache lasting minutes to days, which occur once per month or less often) often has limited impact on individuals. If headaches occur on more than one but fewer than 15 days per month, this is classified as frequent episodic tension‐type headache. In some patients this can evolve into chronic tension‐type headache (on 15 or more days per month). Tension‐type headache should not be confused with migraine, which is characterised by recurrent attacks of mostly one‐sided, severe headache, although some patients suffer from both types of headaches. Tension‐type headache is the most common type of primary headache and the disability attributable to it is larger worldwide than that due to migraine (Stovner 2007). Epidemiological studies report highly variable prevalence, depending on case definition and country (Stovner 2007). According to the International Headache Society (IHS), the lifetime prevalence in the general population varies between 30% and 78% (IHS 2013). If headache episodes are not too frequent (up to a maximum of 10 days per month), unbearable pain can be treated with analgesic drugs or non‐steroidal anti‐inflammatory drugs (Pfaffenrath 1998). In patients with chronic tension‐type headache, guidelines recommend antidepressants such as amitriptyline (Pfaffenrath 1998). In addition to, or instead of drug therapy, behavioural interventions such as relaxation or biofeedback have been shown to be beneficial (McCrory 2000). However, additional effective intervention tools with good tolerability are desirable.
Description of the intervention
Acupuncture, in the context of this review, is defined as the needling of specific points of the body. It is one of the most widely used complementary therapies in many countries (Bodeker 2005). For example, according to a population‐based survey in the year 2002 in the United States, 4.1% of the respondents reported lifetime use of acupuncture and 1.1% recent use (Burke 2006). A similar survey in Germany performed in the same year found that 8.7% of adults between 18 and 69 years of age had received acupuncture treatment in the previous 12 months (Härtel 2004). Acupuncture was originally developed as part of Chinese medicine wherein the purpose of treatment is to bring the patient back to the state of equilibrium postulated to exist prior to illness (Endres 2007a). Some acupuncture practitioners have dispensed with these concepts and understand acupuncture in terms of conventional neurophysiology. Acupuncture is often used as an intervention to reduce the frequency and intensity of headaches. For example, 9.9% of the acupuncture users in the US survey mentioned above stated that they had used acupuncture for treating migraine or other headaches (Burke 2006). Practitioners typically claim that a single course of treatment, such as 12 sessions over a three‐month period, can have a long‐term impact on the frequency and intensity of headache episodes.
How the intervention might work
Multiple studies have shown that acupuncture has short‐term effects on a variety of physiological variables relevant to analgesia (Bäcker 2004; Endres 2007a). However, it is unclear to what extent these observations from experimental settings are relevant to the long‐term effects reported by practitioners. It is assumed that a variable combination of peripheral and local effects; spinal and supraspinal mechanisms; and cortical, psychological or 'placebo' mechanisms contribute to the clinical effects in routine care (Carlsson 2002). While there is little doubt that acupuncture interventions cause neurophysiological changes in the human body, the traditional concepts of acupuncture involving specifically located points on a system of 'channels' called meridians are controversial (Kaptchuk 2002).
Why it is important to do this review
Despite its widespread use for a variety of chronic pain conditions the effectiveness of acupuncture is still controversial. In 2009 we published the first version of our systematic review of acupuncture for tension‐type headache (Linde 2009). After six years an update of the review was overdue.
Objectives
To investigate whether acupuncture is a) more effective than no prophylactic treatment/routine care only; b) more effective than 'sham' (placebo) acupuncture; and c) as effective as other interventions in reducing headache frequency in participants with episodic or chronic tension‐type headache.
Methods
Criteria for considering studies for this review
Types of studies
We included controlled trials in which allocation to treatment was explicitly randomised, and in which participants were followed up for at least eight weeks after randomisation. We excluded trials in which a clearly inappropriate method of randomisation (for example, open alternation) was used.
Types of participants
We included trials conducted among adult participants with episodic and/or chronic tension‐type headache. We excluded studies including participants with headaches of various types (e.g. 50% participants with migraine and 50% participants with tension‐type headache) unless separate results were presented for participants with tension‐type headache. Duration of disease had to be at least six months in the great majority (> 80%) of participants. We considered this criterion met if 1) duration ≥ 6 months was an inclusion criterion; OR 2) the mean duration – 1 standard deviation was > 6 months; OR 3) the mean duration (standard deviation not reported) was > 5 years; OR 4) other information was presented that made it highly likely that the criterion was met (e.g. proportions with duration ranges were presented).
Change to the previous version of this review: we have added the criterion regarding disease duration (to better comply with common diagnostic standards).
Types of interventions
Experimental interventions considered were:
Any treatment involving needle insertion (with or without manual or electrical stimulation) at acupuncture points, pain points or trigger points, described as acupuncture. The planned treatment course must have had at least six treatment sessions and been given at least once per week. We included trials with individualised strategies if the median or mean number of treatments was at least six sessions and there was no reason to believe that treatments were given less frequently than once per week in the majority of participants.
We excluded studies 1) exclusively investigating acupuncture at specific 'micro‐systems' (e.g. scalp or ear acupuncture ‐ trials using micro‐system points in addition to body acupuncture were included); 2) studies investigating other methods of stimulating acupuncture points without needle insertion (for example, acupressure, laser stimulation or transcutaneous electrical stimulation); 3) studies in which fluids were injected at acupuncture points.
Control interventions considered were:
no treatment other than treatment of acute headaches or routine care (which typically includes acute treatment, but might also include other treatments; however, trials normally require that no new experimental or standardised treatment be initiated during the trial period);
sham interventions (interventions mimicking 'true' acupuncture/true treatment, but deviating in at least one aspect considered important by acupuncture theory, such as skin penetration or correct point location);
other active treatments, such as pharmacological, cognitive and physical treatment. We excluded trials comparing acupuncture to food supplements, herbal drugs or combinations of herbal drugs.
We also excluded trials that only compared different forms of acupuncture.
Changes to the previous version of this review: 1) we added a minimum number of six acupuncture sessions, given at least once per week, for inclusion, to warrant that participants received an adequate minimum dose of treatment; 2) we limited eligible other active treatments to pharmacological, cognitive and physical treatment to sharpen the focus of the review.
Types of outcome measures
Studies had to measure and report at least one of the following outcome measures for at least eight weeks after randomisation: headache frequency (days, hours, headache‐free days) per defined time period, response (≥ 50% frequency reduction documented in a headache diary), pain intensity, disability or quality of life with a validated measure.
We excluded trials only reporting measures such as 'total effectiveness rate' (e.g. proportion of participants healed, much improved, improved, unchanged); trials reporting only physiological or laboratory parameters; trials with outcome measurement periods of less than eight weeks (from randomisation to final observation); and trials focusing on the treatment of acute headache.
Change to the previous version: acceptable outcome measures are now more explicitly defined.
Primary outcomes
Response (at least 50% reduction of headache frequency) after completion of treatment (three to four months after randomisation).
(See section Measures of treatment effect for details).
Secondary outcomes
Response at other time points.
Number of headache days.
Headache intensity.
Frequency of analgesic use.
Headache scores.
(See section Measures of treatment effect for details).
To assess safety/acceptability we used:
the number of participants dropping out due to adverse effects; and
the number of participants reporting adverse effects.
Search methods for identification of studies
We performed the search for this update together with the literature search for the update of the review on the prophylaxis of episodic migraine (Linde 2016).
Electronic searches
For this update we searched the following databases without language restrictions:
Cochrane Central Register of Controlled Trials (CENTRAL 2016, Issue 1), searched for years 2008 to 2016;
MEDLINE (via PubMed) 2008 to week 1 of January 2016;
EMBASE (via Ovid) 2008 to 19 January 2016;
AMED (via OVID) 1985 to January 2016.
The search strategies are reported in Appendix 1. For additional searches we also regularly checked PubMed new entries using a simple search string ('acupuncture headache'; last search 10 February 2016). For the previous version of this review (Linde 2009), we searched the Cochrane Complementary Medicine Field Trials Register (whose results are now included in CENTRAL without relevant delay) and the Cochrane Pain, Palliative & Supportive Care Trials Register (no longer updated).
Searching other resources
We searched the World Health Organization (WHO) International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/) for completed or ongoing trials using the search string 'acupuncture AND headache'. The last update search was on10 February 2016.
We also searched the reference lists of all eligible studies and previous systematic reviews (Davis 2008; Endres 2007a; Hao 2013; McCrory 2000; Wang 2007) for additional studies.
Data collection and analysis
Selection of studies
Two review authors screened all abstracts identified by the updated search and excluded those that were clearly irrelevant (for example, studies focusing on other conditions, reviews, etc.). We obtained the full texts of all remaining references and again screened them to exclude clearly irrelevant papers. Two review authors then formally checked for eligibility all remaining articles and all trials included in the previous version of our review (Linde 2009) , according to the above‐mentioned selection criteria. We resolved disagreements by discussion.
Data extraction and management
At least two review authors independently extracted information on participants, methods, interventions, outcomes and results using a specially designed form, before entry into Review Manager (RevMan 2014). In particular, we extracted exact diagnoses; headache classifications used; number and type of centres; age; sex; duration of disease; number of participants randomised, treated and analysed; number of, and reasons for, dropouts; duration of baseline, treatment and follow‐up periods; details of acupuncture treatments (such as selection of points; number, frequency and duration of sessions; achievement of de‐chi (an irradiating feeling considered to indicate effective needling); number, training and experience of acupuncturists); and details of control interventions (sham technique, type and dosage of drugs). For details regarding methodological issues and study results, see below.
Where necessary, we sought additional information from the first or corresponding authors of the included studies.
For three trials included in the individual patient database of the Acupuncture Trialists Collaboration (ATC), an international collaborative network for high quality randomised trials of acupuncture for chronic pain (see Vickers 2010; Vickers 2012 and https://www.mskcc.org/cancer‐care/treatments/symptom‐management/integrative‐medicine/acupuncture‐trialists‐collaboration), we obtained uniformly re‐analysed summary data for number of headache days and the number of responders for calculation of effect sizes (Jena 2008; Melchart 2005; Vickers 2004). We use these data a) to make our findings as comparable to the results of the ATC as possible and b) to make sure that a comparable high quality analysis method was used. For each trial, we created an ANCOVA model for each numeric outcome at each time point and adjusted for the baseline value of that outcome, treatment group (acupuncture or control) and any variables that were used to stratify randomisation in the original trial. Using this model, we calculated the adjusted mean outcome values for each group (acupuncture and control), and we used the standard error for the effect of treatment from the ANCOVA model to calculate the standard deviation for the difference in adjusted means. Therefore, effect sizes calculated in our analyses might to some degree deviate from those in the original publications of the six trials. Use of raw data also allowed us to calculate response rates, such as for a 50% reduction in pain, even if this was not reported in the original trial publication.
In addition to the ATC data we received additional data relevant for effect size calculation from the authors of one study (Karst 2001). We received some additional information for a further three trials (Carlsson 1990; Söderberg 2006; Wylie 1997). In two trials, additional information was not needed (White 1996; White 2000), and for two older trials, we were unable to contact the study authors (Ahonen 1984; Tavola 1992). The first author of the new trial did not respond to inquiries (Kwak 2007).
Assessment of risk of bias in included studies
For the assessment of study quality, we used the risk of bias approach for Cochrane reviews (Higgins 2011). We used the following six separate criteria:
adequate sequence generation;
allocation concealment;
blinding;
incomplete outcome data addressed (up to three months after randomisation);
incomplete follow‐up outcome data addressed (4 to 12 months after randomisation);
freedom from selective reporting.
We did not include the item 'other potential threats to validity' in a formal manner, but we noted if relevant flaws were detected.
In a first step, we copied information relevant for making a judgement on a criterion from the original publication into an assessment table. If additional information from the study authors was available, we also entered this in the table, along with an indication that this was unpublished information. At least two review authors independently made a judgement as to whether the risk of bias for each criterion was considered low, high or unclear. We resolved disagreements by discussion.
For the operationalisation of the first five criteria, we followed the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For the 'selective reporting' item, we used a more liberal definition. Headache trials typically measure a multiplicity of headache outcomes at several time points using diaries and there are a plethora of slightly different outcome measurement methods. While a single primary endpoint is sometimes predefined, the overall pattern of a variety of outcomes is necessary to get a clinically interpretable picture. If the strict Handbook guidelines had been applied, almost all trials would have been rated 'unclear' for the 'selective reporting' item. We considered trials as having a low risk of bias for this item if they reported the results of the most relevant headache outcomes assessed (typically a frequency measure, intensity, analgesic use and response) for the most relevant time points (end of treatment and, if done, follow‐up), and if the outcomes and time points reported made it unlikely that authors had picked them out because they were particularly favourable or unfavourable.
We considered trials that met all criteria, or all but one criterion, to be of higher quality. Some trials had both blinded sham control groups and unblinded comparison groups receiving no prophylactic treatment or drug treatment. In the 'Risk of bias' tables, the 'Judgement' column always relates to the comparison with sham interventions. In the 'Description' column, we also include the assessment for the other comparison group(s). As the 'Risk of bias' table does not include a 'not applicable' option, we rated the item 'incomplete follow‐up outcome data addressed (4 to 12 months after randomisation)?' as 'unclear' for trials that did not follow up participants for longer than three months.
Assessment of the adequacy of the acupuncture intervention
We also attempted to provide a crude estimate of the quality of acupuncture. Two review authors (mostly GA and BB, or, for trials in which one of these review authors was involved, AW) who are trained in acupuncture and have several years of practical experience, answered two questions. The trial from Korea was assessed by only one review author (BCS). First, review authors were asked how they would treat the participants included in the study. Answer options were 'exactly or almost exactly the same way', 'similarly', 'differently', 'completely differently' or 'could not assess' due to insufficient information (on acupuncture or on the participants). Second, they were asked to rate their degree of confidence that acupuncture was applied in an appropriate manner on a 100 mm visual scale (with 0% = complete absence of evidence that the acupuncture was appropriate, and 100% = total certainty that the acupuncture was appropriate). The latter method was proposed by a member of the review team (AW) and has been used in a systematic review of clinical trials of acupuncture for back pain (Ernst 1998). In the Characteristics of included studies table, the acupuncturists' assessments are summarised under 'Methods' (for example, 'similarly/70%' indicates a trial where the acupuncturist‐review author would treat 'similarly' and is 70% confident that acupuncture was applied appropriately).
Measures of treatment effect
For the purposes of summarising results, we categorised the included trials according to control groups: 1) comparisons with no acupuncture (treatment of acute headaches only or routine care); 2) comparisons with sham acupuncture interventions; and 3) comparisons with other treatments.
We defined four time windows for which we tried to extract and analyse study findings:
up to eight weeks/two months after randomisation;
three to four months after randomisation;
five to six months after randomisation; and
more than six months after randomisation.
In all included studies acupuncture treatment started immediately or very soon after randomisation.
If more than one data point was available for a given time window, we used: for the first time window, preferably the data closest to eight weeks; for the second window, the data closest to four weeks after completion of treatment (for example, if treatment lasted eight weeks, data for weeks 9 to 12); for the third window, the data closest to six months; and for the fourth window, data closest to 12 months.
We extracted data for the following outcomes (taking the guidelines of the International Headache Society Clinical Trials Subcommittee (IHS Clinical Trials Subcommittee 2009) into account).
Proportion of 'responders'. For trials investigating the superiority of acupuncture compared to no acupuncture or sham intervention, we used, if available, the number of participants with a reduction of at least 50% in the number of headache days per four weeks and divided it by the number of participants randomised to the respective group. In studies comparing acupuncture with other therapies, we used for the denominator the number of participants analysed. If the number of responders regarding headache days was not available, we used global assessment measures by participants or physicians. We calculated responder rate ratios (risk ratio of having a response) and 95% confidence intervals as effect size measures.
Number of headache days (means and standard deviations) per four‐week period (calculation of mean differences).
Headache intensity (any measures available, extraction of means and standard deviations, calculation of standardised mean differences).
Frequency of analgesic use (any continuous or rank measures available, extraction of means and standard deviations, calculation of standardised mean differences).
Headache score (any measures available, extraction of means and standard deviations, calculation of standardised mean differences).
The main outcome measure was the proportion of responders for the three‐ to four‐month window (close to the end of the treatment cycle and a time point for which outcome data are often available). Secondary outcomes of major interest were responder proportions at other time points and the number of headache days (all four time points; this outcome is recommended as a primary outcome for randomised trials by the International Headache Society Clinical Trials Subcommittee). We calculated risk ratios of having a response and 95% confidence intervals as effect size measures. Risk ratios > 1 indicate that there were more responders in the acupuncture group compared to the comparator group. For headache days we calculated mean differences and their respective 95% confidence intervals. For continuous measures, we used, if available, the data from intention‐to‐treat analyses with missing values replaced; otherwise we used the data presented on available cases. All these outcomes rely on patient reports, mainly collected in headache diaries.
As safety/acceptability outcomes we used the number of participants dropping out due to adverse effects and the number of participants reporting at least one adverse event or effect. As the number of events was typically low we calculated odds ratios instead of risk ratios. Odds ratios > 1 indicate more events (e.g. dropouts) in the acupuncture group.
Unit of analysis issues
The unit of analysis was the individual participant.
Dealing with missing data
If publications reported study findings with insufficient detail or in an inconsistent manner we attempted to obtain further information from the authors. Regarding missing patient data due to dropout or loss to follow‐up in the included studies we used the following strategies: for continuous measures we used, if available, the data from intention‐to‐treat analyses with missing values replaced; otherwise, we used the data presented on available cases. For response we used the number of responders and divided it by the number of participants randomised to the respective group (counting missing information as non‐response).
Assessment of heterogeneity
We pooled individual studies only for the comparison versus sham. We assessed heterogeneity with the Cochrane Chi² test and the I² statistic.
Assessment of reporting biases
Given the low number of trials per comparison we did not use formal methods for assessing reporting biases.
Data synthesis
As the only two trials comparing acupuncture and no acupuncture differed strongly regarding participants and care in the control group (details see below), we did not pool the findings of these trials and only present the effect size of the individual studies at the available time points. For the comparison versus sham we calculated pooled fixed‐effect estimates, their 95% confidence intervals, the Chi2 test for heterogeneity and the I2 statistic. If the P value of the Chi² test for heterogeneity was < 0.2 and/or the I² > 40% we reported random‐effects estimates in addition. Following the recommendation of the Cochrane Pain, Palliative and Supportive Collaborative Review Group we presented forest plots only if there were at least two trials and 200 participants (for at least one time window).
We have summarised findings from trials comparing acupuncture with other active treatment descriptively due to insufficient data presentation and the great diversity of the available trials.
Change to the previous version:
Based on the recommendation of the statistician in our team (AV) we now use fixed‐effect models for calculating pooled estimates. This is primarily because a fixed‐effect analysis constitutes a valid test of the null hypothesis. Moreover, due to very large discrepancies in sample size, a random‐effects model would have participants in small studies counting considerably more than participants in large studies. Nonetheless, if the P value of the Chi² test for heterogeneity was < 0.2 and/or the I² > 40% we reported random‐effects estimates in addition.
Quality of the evidence
We used the GRADE approach to assess the quality of evidence related to key outcomes as appropriate (GRADEpro GDT 2015; Schünemann 2011). Key outcomes were our primary outcome, response three to four months after randomisation, the number of headache days for the same time window, the number of patients dropping out due to adverse effects and the number of patients reporting adverse effects. The GRADE Working Group grades of evidence are:
High quality: We are very confident that the true effect lies close to that of the estimate of the effect.
Moderate quality: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low quality: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect.
Very low quality: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
We decreased the grade due to:
serious (‐1) or very serious (‐2) limitation to study quality;
important inconsistency (‐1);
some (‐1) or major (‐2) uncertainty about directness;
imprecise or sparse data (‐1);
high probability of reporting bias (‐1).
Results
Description of studies
Results of the search
The common update searches performed for this review and the update of the review on the prophylaxis of episodic migraine (Linde 2016) identified 527 hits (517 by database searches, five by checking references and alerts, and four from checking entries in trials registries not otherwise identified). The majority of the 75 full‐text publications obtained and all four additional entries from clinical trial registries addressed migraine. We formally checked eight publications, which we deemed potentially eligible, against the eligibility criteria (see Figure 1). Only one new trial could be included (Kwak 2007). For one trial already included in the previous version (Söderberg 2006), a new, additional publication was available. However, this new publication did not report information that was directly usable in our review.
1.
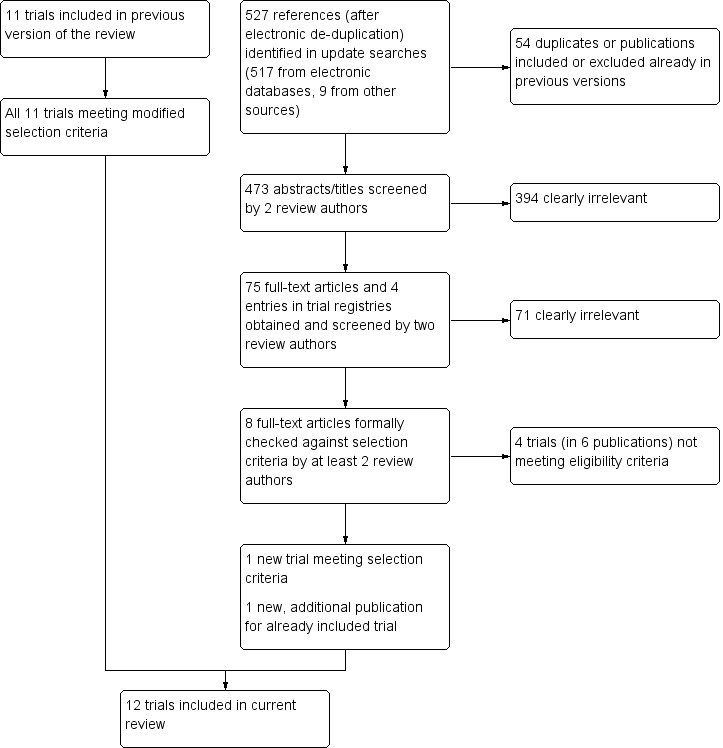
Flow diagram.
Included studies
This update includes 12 trials described in 22 publications (including published protocols and papers reporting additional aspects such as treatment details or cost‐effectiveness analyses) (Ahonen 1984; Carlsson 1990; Endres 2007; Jena 2008; Karst 2001; Kwak 2007Melchart 2005; Söderberg 2006; Tavola 1992; White 1996; White 2000; Wylie 1997).
A total of 2349 participants with tension‐type headache were included in the studies (median 56, range 10 to 1265). Five were multicentre trials (Endres 2007; Jena 2008; Melchart 2005; Söderberg 2006; White 2000); the remaining seven were performed in a single centre. Four trials originated from Germany (Endres 2007; Jena 2008; Karst 2001; Melchart 2005), three from the UK (White 1996; White 2000; Wylie 1997), two from Sweden (Carlsson 1990; Söderberg 2006), and one each from Finland (Ahonen 1984), Italy (Tavola 1992), and Korea (Kwak 2007). Two trials included only participants with episodic tension‐type headache (White 1996; White 2000), and three only participants with chronic tension‐type headache (Carlsson 1990; Kwak 2007; Söderberg 2006). The remaining trials either explicitly stated that they included both forms (Endres 2007; Jena 2008; Karst 2001; Melchart 2005), or made no clear statement (Ahonen 1984; Tavola 1992; Wylie 1997).
All trials used a parallel‐group design (no cross‐over trials). Ten trials had two groups (one acupuncture group and one control group), and two trials had two control groups (Melchart 2005; Söderberg 2006). In two trials acupuncture was compared to routine care (Jena 2008), or treatment of acute headaches only (Melchart 2005). Seven trials used a sham control but the actual techniques varied. In four trials, non‐acupuncture points were needled (Endres 2007; Kwak 2007; Melchart 2005; Tavola 1992), while in the remaining three non‐skin‐penetrating techniques were used (Karst 2001; White 1996; White 2000) (see Characteristics of included studies for details). Three trials compared acupuncture with physiotherapy (Ahonen 1984; Carlsson 1990; Söderberg 2006); one of these had an additional relaxation control group (Söderberg 2006). Wylie 1997 compared acupuncture with a combination of massage and relaxation. There was no trial that compared acupuncture with prophylactic drug treatment.
The largest study by far used a quite unusual approach and has to be described in greater detail (Jena 2008). In this very large, highly pragmatic study, 15,056 headache participants recruited by more than 4000 physicians in Germany were included. A total of 11,874 participants who did not give consent to randomisation received up to 15 acupuncture treatments within three months and were followed up for an additional three months. This was also the case for 1613 participants randomised to immediate acupuncture, while the remaining 1569 participants remained on routine care (not further defined) for three months and then received acupuncture. The published analysis of this trial is on all randomised participants, but the authors and the Acupuncture Trialists Collaboration provided us with unpublished results of subgroup analyses on the 1265 participants with tension‐type headache. The large number of practitioners involved and the pragmatic approach make it likely that there is some diagnostic uncertainty as to whether all participants truly had tension‐type headache.
The number of acupuncture sessions varied between 6 and 15. Three trials selected acupuncture points in an individualised manner (Jena 2008; Tavola 1992; Wylie 1997), and eight in a semi‐standardised manner (either by having some mandatory points in all participants plus individualised points, or by using predefined point selections depending on syndrome diagnoses according to Chinese medicine) (Ahonen 1984; Endres 2007; Karst 2001; Kwak 2007; Melchart 2005; Söderberg 2006; White 1996; White 2000). One trial used a standardised point selection (Carlsson 1990). In two trials, brief needling was used (needles inserted for a few seconds only) (White 1996; White 2000). For one trial, both acupuncturist‐reviewers considered the treatment 'inadequate' (Carlsson 1990). Both acupuncturist‐review authors would have used different treatment approaches for the participants in a further four trials (Ahonen 1984; Karst 2001; Söderberg 2006; White 2000). In trials using individualised strategies, assessments were difficult because of a lack of detail about the actual interventions used.
Post‐randomisation observation periods varied between 8 and 64 weeks. Apart from three trials (Ahonen 1984; Carlsson 1990; Jena 2008), all trials used diaries for the measurement of the most important headache outcomes. All but two trials, Ahonen 1984 and Jena 2008, included a baseline observation period before randomisation. The trials comparing acupuncture to other therapies rarely presented their findings in a manner allowing effect size calculation, while for trials comparing acupuncture with no acupuncture or sham acupuncture, effect size estimates could be calculated for the most relevant outcomes.
Excluded studies
We excluded four newly identified trials for this update. Chassot 2015 was a cross‐over trial in which the observation period per phase was less than eight weeks. Guerreiro da Silva 2012 included only pregnant women in whom headache started during pregnancy. Hong 2007 followed participants for only three weeks after randomisation (two weeks treatment and one‐week follow‐up observation); furthermore, it seems that participants with recent onset of headache were included. Sozen 2013 was a trial in participants with chronic daily headache (chronic migraine or chronic tension‐type headache); results for participants with tension‐type headache were not available separately.
Risk of bias in included studies
Figure 2 provides a summary of the assessments of risks of bias in the individual studies; Figure 3 provides an overview across studies for the single items. It has to be taken into account that the four trials without long‐term follow‐up had to be rated unclear although this criterion has to be considered as not applicable (Ahonen 1984; Jena 2008; White 1996; Wylie 1997). Five trials have major risks of bias, important uncertainties or are reported so insufficiently that a reliable assessment was not possible (Ahonen 1984; Carlsson 1990; Kwak 2007; Söderberg 2006; Wylie 1997).
2.
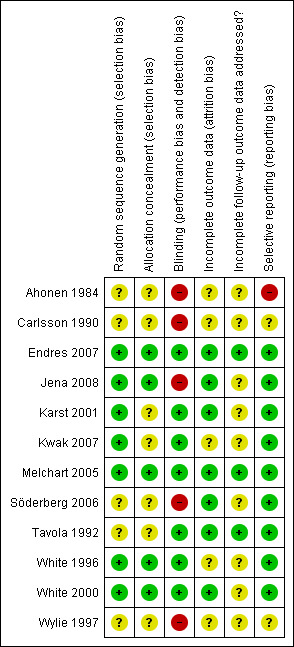
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
3.
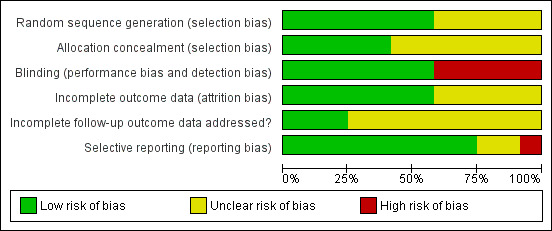
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
An adequate method of sequence generation was reported for seven trials (Endres 2007; Jena 2008; Karst 2001; Kwak 2007; Melchart 2005; White 1996; White 2000) (low risk of bias), and an adequate method for allocation concealment for five (Endres 2007; Jena 2008; Melchart 2005; White 1996; White 2000).
Blinding
Participants were blinded only in the seven sham‐controlled trials (Endres 2007; Karst 2001; Kwak 2007; Melchart 2005; Tavola 1992; White 1996; White 2000 (low risk of bias). We judged the remaining five studies to be at high risk of bias.
Incomplete outcome data
Attrition was low or adequately accounted for in analyses up to three months after randomisation in seven trials (Endres 2007; Jena 2008; Karst 2001; Melchart 2005; Söderberg 2006; Tavola 1992; White 2000), and in three of seven trials that had a follow‐up longer than three months (Endres 2007; Melchart 2005; Tavola 1992). We judged the remaining five studies to be at unclear risk of bias.
Selective reporting
While the reporting of study results was variable and often not easily usable for effect size calculation, we considered the risk of selective reporting to be low in 10 of 12 studies. We judged two studies to be at unclear risk of bias (Carlsson 1990; Wylie 1997), and the remaining study to be at high risk of bias (Ahonen 1984).
Other potential sources of bias
We did not assess the included studies for other potential sources of bias.
Effects of interventions
Comparisons with routine care/treatment of acute headaches only
The two trials comparing acupuncture to routine care only (Jena 2008; n = 1265) or treatment of acute headaches only (Melchart 2005; n = 207) were unblinded but otherwise had a low risk of bias. In both trials, participants received acupuncture three months after randomisation (waiting list condition), so it is only possible to assess short‐term effects up to three months after the start of the treatment. We did not calculate pooled effect size estimates, as headache baseline frequency and management in the control groups of the two trials were quite different. The participants included in Melchart 2005 (n = 207) had much more frequent headaches at baseline (mean 17.6 days/month) than those in Jena 2008 (7.0 days). While the effect size estimates of the two trials differed considerably the proportion of participants experiencing at least 50% reduction of headache frequency was much higher in groups receiving acupuncture than in control groups (moderate quality evidence; trial 1: 302/629 (48%) versus 121/636 (19%); risk ratio (RR) 2.52; 95% confidence interval (CI) 2.11 to 3.02; number needed to treat 3; 95% CI 3 to 5; trial 2: 60/132 (45%) versus 3/75 (4%); RR 11.36; 95% CI 3.69 to 34.98; number needed to treat 2; 95% CI 1 to 9; see Analysis 1.1).
1.1. Analysis.
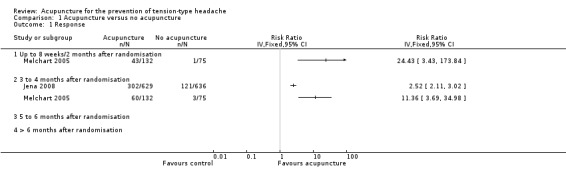
Comparison 1 Acupuncture versus no acupuncture, Outcome 1 Response.
The differences between acupuncture and waiting list groups for the number of headache days at three months were 5.8 days (95% CI 4.0 to 7.5) and 3.9 days (95% CI 3.3 to 4.6), respectively (Analysis 1.2). Again, while the effect size in the two trials differed, both showed a clinically important difference (moderate quality evidence). We downgraded the quality of the evidence for both headache days and reduction by at least 50% to moderate due to the variable effect sizes and lack of blinding.
1.2. Analysis.
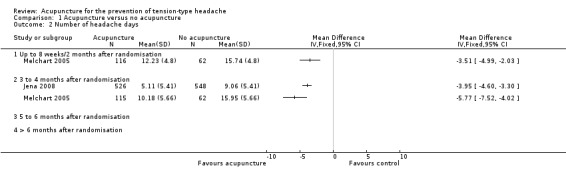
Comparison 1 Acupuncture versus no acupuncture, Outcome 2 Number of headache days.
Large differences were also found for headache intensity (Analysis 1.3).
1.3. Analysis.
Comparison 1 Acupuncture versus no acupuncture, Outcome 3 Headache intensity.
Only the Melchart 2005 trial reported on days with analgesic use and headache score findings. For both outcomes acupuncture showed significant and clinically relevant benefits over waiting list.
As adverse effects and the number of participants dropping out due to adverse effects were not measured in the waiting list groups comparative results for these outcomes are not available.
Comparisons with sham treatment
Five of the six interpretable trials with sham comparisons had comparably good quality (Endres 2007; Karst 2001; Melchart 2005; Tavola 1992; White 2000), despite some problems with attrition during long‐term follow‐up (Karst 2001; White 2000), and some uncertainties regarding the details of randomisation (Karst 2001; Tavola 1992). In one trial it was difficult to assess quality reliably due to insufficient reporting (Kwak 2007). Four trials had follow‐up periods of about six months after randomisation and one more than 12 months (Tavola 1992). Five trials reported findings on response and headache in a manner that allowed effect size calculation for at least one time window (Endres 2007; Karst 2001; Melchart 2005; Tavola 1992; White 2000).
After treatment (time window three to four months) 205 of 391 (52%) participants receiving acupuncture had at least 50% reduction of headache frequency compared to 133 of 312 (43%) in the sham group (RR 1.27; 95% CI 1.09 to 1.48; I2 = 0%; four trials; moderate quality evidence; Analysis 2.1; Figure 4). We downgraded the quality of the evidence to moderate given the small number of trials, the limited precision of the effect estimate and the dominance of one large trial. This corresponds to a number needed to treat of 8 (95% CI 5 to 25). The findings are very similar in the time windows up to two months after randomisation (RR 1.26; 95% CI 1.10 to 1.45) and up to six months after randomisation (RR 1.17; 95% CI 1.02 to 1.35; Figure 4). Only one small trial (n = 30) provided data for the time window more than six months after randomisation (RR 1.50; 95% CI 0.53 to 4.26).
2.1. Analysis.
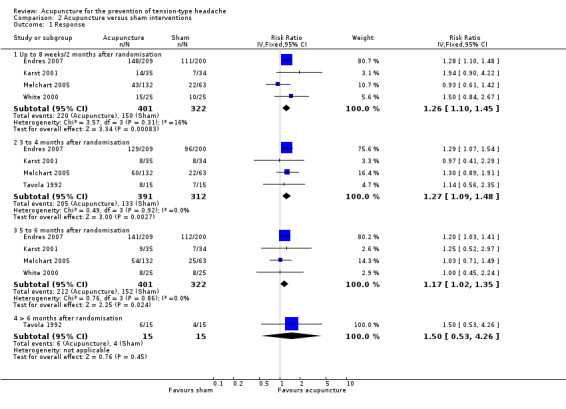
Comparison 2 Acupuncture versus sham interventions, Outcome 1 Response.
4.
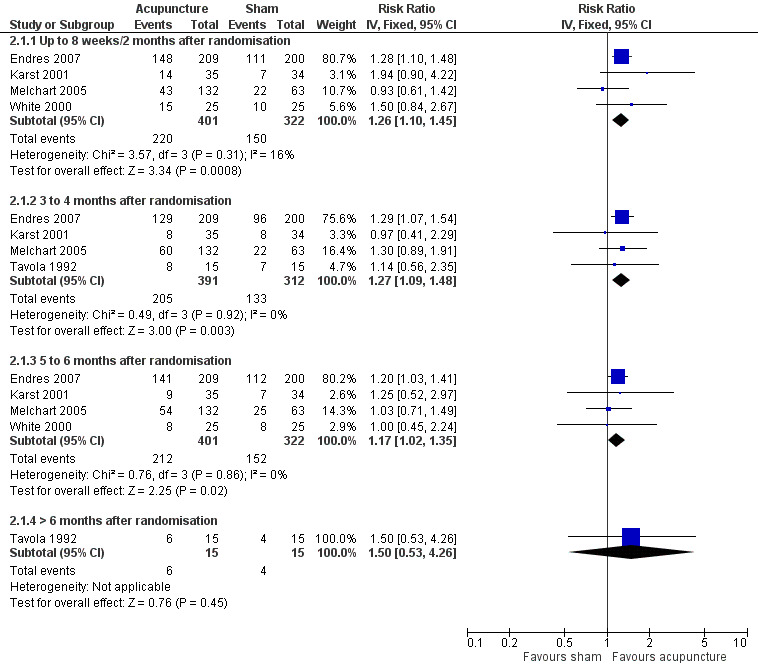
Forest plot of comparison: 2 Acupuncture versus sham interventions, outcome: 2.1 Response.
The same five trials also reported data on the number of headache days per month for at least one time window. After treatment (time window three to four months) the pooled estimate indicated 1.62 fewer headache days in the acupuncture groups (95% CI 0.54 to 2.69 days; I² = 0%; four trials with 653 participants; number of headache days in sham groups varying between 9 and 16 days per month; moderate quality evidence; Analysis 2.2; Figure 5). We downgraded the quality of the evidence to moderate for the same reasons as for the outcome at least 50% reduction. The findings are very similar in the time windows up to two months after randomisation (mean difference 1.49 days; 95% CI 0.39 to 2.58 days) and up to six months after randomisation (1.51 days; 95% CI 0.43 to 2.59 days; Figure 5). Data for the time window more than six months after randomisation were not available. It should be noted that the by far largest trial (409 participants) dominated the meta‐analyses (75% to 80% weight) (Endres 2007). There was no indication of relevant statistical heterogeneity in any of the analyses; however, these analyses have limited power.
2.2. Analysis.
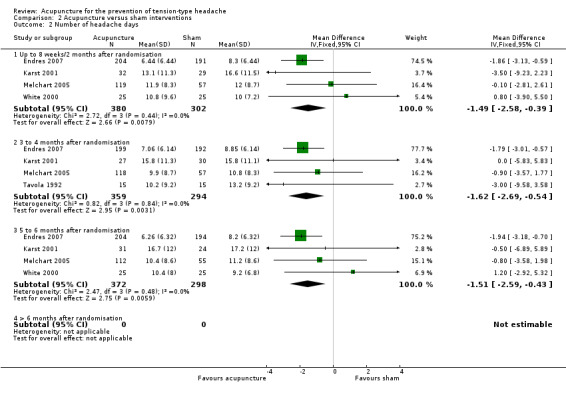
Comparison 2 Acupuncture versus sham interventions, Outcome 2 Number of headache days.
5.
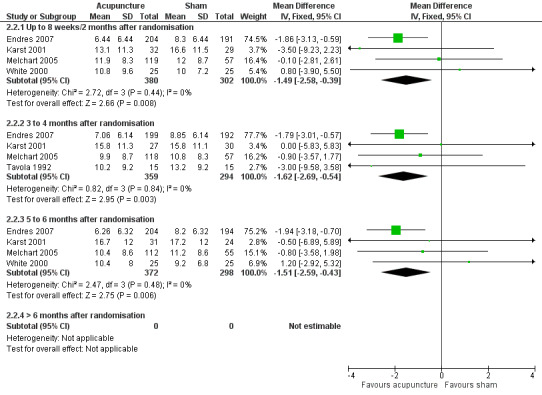
Forest plot of comparison: 2 Acupuncture versus sham interventions, outcome: 2.2 Number of headache days.
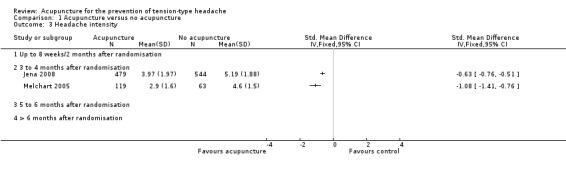
Regarding headache intensity, a small, statistically significant difference was found at five to six months (standardised mean difference (SMD) ‐0.20; four trials with 670 participants) but not at up to two months (SMD ‐0.12; three trials with 143 participants) or three to four months (SMD ‐0.10; four trials with 655 participants) after randomisation (see Analysis 2.3).
2.3. Analysis.
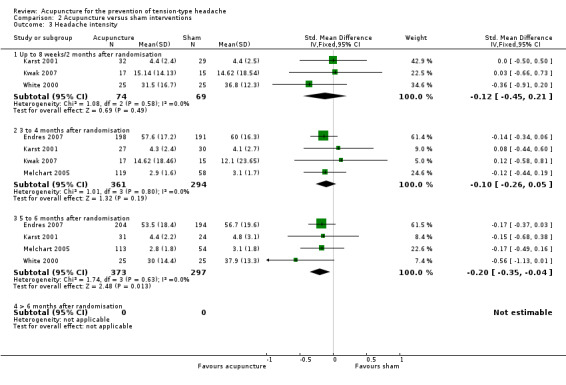
Comparison 2 Acupuncture versus sham interventions, Outcome 3 Headache intensity.
Three trials reported data on the frequency of analgesic use for the first two time windows (266 and 261 participants, respectively; see Analysis 2.4). When we pooled these trials, there was a small, significant effect of acupuncture over sham controls (standardised mean differences 0.31 and 0.30, respectively).
2.4. Analysis.
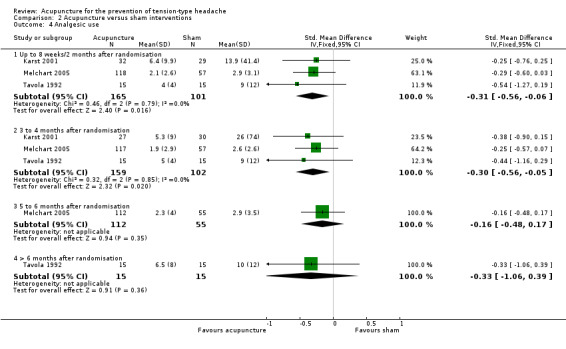
Comparison 2 Acupuncture versus sham interventions, Outcome 4 Analgesic use.
Headache score data were measured in only two small trials, but they did not provide usable data for effect size calculation.
One of 420 participants receiving acupuncture dropped out due to adverse effects compared to none of 343 receiving sham (odds ratio (OR) 1.45; 95% CI 0.06 to 36.06; six trials; low quality evidence). The number of participants reporting adverse effects in the three trials reporting this outcome was 29 of 174 (17%) versus 12 of 103 (12%; OR 1.26; 95% CI 0.60 to 2.65; low quality evidence). We downgraded the quality of the evidence to low due to the very low precision of the estimates and the somewhat unclear methods for assessing adverse effects in the trials.
Comparisons with other treatments
The four trials comparing acupuncture with physiotherapy (Ahonen 1984; Carlsson 1990; Söderberg 2006), relaxation (Söderberg 2006), or a combination of massage and relaxation (Wylie 1997), provide almost no data for effect size estimation and must be interpreted with great caution. There is high risk of bias in the three older trials (Ahonen 1984; Carlsson 1990; Wylie 1997, see Characteristics of included studies), and the reporting of results is insufficient. The most recent trial has somewhat better quality and reported means (but no standard deviations) for a large number of outcomes measured (Söderberg 2006).
Ahonen 1984 reported slightly higher response rates in the acupuncture group, Carlsson 1990 reported better results in the physiotherapy group, Söderberg 2006 found significantly fewer headache days per four weeks in the relaxation group immediately after treatment but no other significant differences, and Wylie 1997 found no significant differences.
None of the trials reported the number of participants dropping out due to adverse effects or the number of participants reporting adverse effects.
Effect size estimates for response, intensity, frequency of analgesic use and headache scores could not be calculated due to insufficient reporting.
Discussion
Summary of main results
Since the publication of the previous version of our review (Linde 2009), only one new small, sham‐controlled trial has become available. Therefore, our findings remain largely unchanged. Two unblinded, but otherwise adequately performed, large studies show that adding acupuncture to routine care or treatment of acute headaches reduces the frequency of headaches in the short term (three months). Long‐term effects were not investigated. Seven trials compared various acupuncture strategies with various sham interventions. Pooled analyses of the trials found a small but significant reduction of headache frequency over sham over a period of six months. None of the four trials comparing acupuncture with physiotherapy, massage or exercise found a superiority of acupuncture, and for some outcomes better results were observed with a comparison therapy. However, these mostly small and older trials of limited quality are difficult to interpret.
Overall completeness and applicability of evidence
Acupuncture is a therapy that is applied in a variable manner in different countries and settings. For example, in Germany, where the three largest trials included in this review were performed, acupuncture is mainly provided by general practitioners and other physicians. Their approach to acupuncture is based on the theories of traditional Chinese medicine, although the amount of training they receive in traditional Chinese medicine is limited (Weidenhammer 2007). In the UK, the providers are likely to be non‐medical acupuncturists with a comparatively intense traditional training, physiotherapists or medical doctors with a more 'Western' approach (Dale 1997). The trials included in this review come from a variety of countries and used a variety of study approaches. However, as with other therapies for tension‐type headache (McCrory 2000), the evidence base available is far from complete. Despite its frequency, tension‐type headache is investigated much less often than migraine. For the German setting, the two large studies available clearly show clinically relevant short‐term benefits of adding acupuncture to no treatment or routine care (Jena 2008; Melchart 2005). However, it is unclear whether these findings can be extrapolated to other settings. It is also unclear whether patients with episodic and chronic tension‐type headache respond in a different manner to acupuncture.
The findings of our review are consistent with the increasing evidence that true acupuncture has a small effect over sham acupuncture interventions for a variety of chronic pain (Lam 2013; Linde 2016; Manheimer 2010; Vickers 2012). If the reduction of headache days over sham is expressed as a standardised mean difference to make it comparable with the findings of trials in other chronic pain conditions, the estimates (between 0.20 and 0.22 for the three time windows with available data) are very similar to those in the cited reviews. If the true effects are of that size this has a number of implications. First, all available trials ‐ even the largest trial in our review (Endres 2007) ‐ have been underpowered. To achieve 80% power a trial would have to include around 400 participants per group (Linde 2010b). Second, as it is almost impossible to blind acupuncturists and to rule out some degree of unblinding of participants in acupuncture trials (as in trials of many other non‐pharmacological interventions) this small effect might even be overestimated due to performance and detection bias. Traditional theories underlying acupuncture are scientifically questionable; therefore, many sceptics consider acupuncture a placebo only (e.g. McGeeney 2015). On the other hand, there are both physiological concepts and experimental evidence that acupuncture has 'specific' effects beyond the traditional concepts (e.g. Kong 2009; Yang 2012). There is also increasing evidence that sham acupuncture is either more potent than other placebos, not an inert placebo, or both (Corbett 2013; Kaptchuk 2006; Linde 2010a; Linde 2010b; Meissner 2013), that acupuncture has clinically relevant effects over usual care controls (Lam 2013; Linde 2016; Manheimer 2010; Vickers 2012), and that acupuncture compares well with a number of active interventions (Corbett 2013; Linde 2016).
We did not find any comparisons of acupuncture with prophylactic drug treatment. The trial by Endres 2007 was originally designed to include a third arm of participants randomised to amitriptyline, the currently most widely accepted therapy (Diener 2004). However, as participants were unwilling to participate in a trial with the possibility of being randomised to amitriptyline, this arm was dropped after one year of very poor accrual. This suggests that participants ready to accept treatment with acupuncture and amitriptyline differ. Apart from the trial by Söderberg 2006, the trials comparing acupuncture with physiotherapy, relaxation and massage are reported insufficiently or have relevant methodological shortcomings. The question of how acupuncture compares to other non‐pharmacological treatments cannot be answered at present.
Overall, the evidence on the effects of acupuncture for tension‐type headache far is from complete. For the comparison with no treatment (beyond treating acute pain) or non‐structured routine care it is not possible to reliably estimate the size of the effects. In the two trials short‐term effects are large (standardised mean differences 0.73 and 1.02), but without further large studies the confidence in these estimates is low. Long‐term effects have not been investigated. Findings on the effects over sham seem to be consistent but the number of trials in our analyses is limited. Future trials might lead to important changes in our effect estimates (although our findings are consistent with those in other conditions). The available evidence is insufficient to assess how acupuncture compares with other treatment options.
Quality of the evidence
While some new trials have acceptable quality, overall there are relevant methodological problems or uncertainties in about half of the studies (high risks of bias). Designing and performing clinical trials of acupuncture is a challenge, particularly with respect to blinding and selection of control interventions. As all relevant headache outcomes have to be assessed by the participants themselves, reporting bias is possible in all trials comparing acupuncture to no treatment, routine, care, drug treatment or other therapies.
Using GRADE, we considered the overall quality of the evidence that acupuncture reduces headache frequency over usual care/treatment of acute headaches only and sham to be moderate. Reasons for not considering the quality of evidence to be high were the lack of blinding of participants (for the comparison with usual care/treatment of acute headaches only), the unblinded treatment providers (both comparisons), and the variable effect sizes in clinically diverse trials (comparison with acupuncture usual care/treatment of acute headaches only). We did not further downgrade our rating for the comparison of acupuncture with usual care/treatment of acute headaches only because the findings consistently showed clinically relevant effects in spite of the variable effect sizes.
Our safety outcomes (the number of participants dropping out due to adverse effects and the number of participants with adverse effects) were only reported in trials with sham controls. As these events were rare both in the acupuncture and sham groups these estimates are very imprecise (low quality evidence).
Potential biases in the review process
We are confident that we have identified the existing large clinical trials relevant to our question, but we cannot rule out the possibility that there are additional small trials that are unpublished or published in sources not accessible by our search. We have not systematically searched Chinese or Korean databases for this version of the review, but trials meeting our selection criteria beyond the one included Korean trial, Kwak 2007, might exist. The few Chinese and Korean trials identified through our literature search did not meet the inclusion criteria. There is considerable skepticism toward clinical trials from China because results that have been reported in the past have been almost exclusively positive (Vickers 1998). However, the quality and number of randomised trials published in Chinese and other Asian languages have improved over recent years (Wang 2007), and it seems inadequate to neglect this evidence without examining it critically. Reviewers from China (YF) and Korea (BCF) have been included in the team to overcome this shortcoming in future updates.
Three members of the review team were involved in at least one of the included trials. These trials were assessed by other members of the review team. All review authors are or were affiliated to a CAM (complementary and alternative medicine) research centre and six (GA, BB, YF, MM, BCS, AW) of the review authors use acupuncture regularly in their patients.
Agreements and disagreements with other studies or reviews
There are two other sufficiently up‐to‐date relevant systematic reviews that summarise randomised trials of acupuncture for tension‐type headache. The review by Davis 2008 was restricted to sham‐controlled trials, but included cross‐over trials with observation periods shorter than eight weeks per phase, which we excluded in our review. The main outcome measure was the number of headache days per month during treatment (broadly comparable to our first time window) and at long‐term follow‐up (20 to 25 weeks). Eight trials met the inclusion criteria for the review and five provided sufficient data for meta‐analysis. Interestingly, although the authors' meta‐analytic calculations for the effect during treatment yielded a larger group difference than ours for the first time window (2.93 days compared to 1.56 days), their findings were statistically not significant, while ours are statistically significant. This is due to the fact that Davis 2008 includes the extremely positive cross‐over trial by Xue 2004 (using electro‐acupuncture), excluded by us, which leads to heterogeneity, and uses earlier, slightly more negative data for the White 2000 trial. Together with the use of a random‐effects model for meta‐analysis these factors result in much wider confidence intervals (‐7.49 to 1.64 in Davis 2008 compared to ‐3.02 to ‐0.10 in our review). Findings for the long‐term outcomes are very similar to ours (a small but significant benefit of acupuncture over sham). Davis 2008 concludes that acupuncture has limited efficacy for the reduction of headache frequency compared to sham treatment. The meta‐analysis by Hao 2013 includes the same five trials also analysed by Davis 2008. The authors performed several subgroup analyses to explore sources of heterogeneity. Due to the small number of trials these are hypothesis‐generating at best. The authors conclude that stimulation mode, needle retention and treatment frequency might influence trial outcomes in a relevant manner.
Authors' conclusions
Implications for practice.
The available results suggest that acupuncture may be considered for treating frequent episodic or chronic tension‐type headaches.
Implications for research.
There is clearly a need for large, high quality trials comparing acupuncture to other effective (pharmacological and non‐pharmacological) treatments for frequent or chronic tension‐type headache. Further trials investigating the long‐term effects of adding acupuncture to routine care or treating acute headaches only are also desirable as both available trials originate from Germany and have short observation periods. We do not consider sham‐controlled trials a priority for the future. The cumulative evidence suggests that acupuncture is effective in various chronic pain conditions, that correct point selection plays a role, but a less important role than acupuncturists have thought, and that a relevant part of the clinical benefit might be due to needling effects not dependent on the selection of traditional points or powerful placebo effects, or both. If researchers decide to perform a sham‐controlled trial, they should seriously consider including a third group receiving another treatment or no treatment beyond treatment of acute headaches. Furthermore, they should be aware that the way the treatment is delivered might have an important impact on outcomes (Kaptchuk 2008), and that large sample sizes might be needed to identify any small point‐specific effects.
Feedback
Feedback submitted, 26 May 2016
Summary
Name: Caroline Struthers
Email Address: caroline.struthers@csm.ox.ac.uk
Affiliation: EQUATOR Network
Role: Education and Training Manager
Comment: NICE has recently issued guidance about not using acupuncture for lower back pain because of lack of robust evidence of effectiveness http://www.csp.org.uk/news/2016/03/24/no‐more‐acupuncture‐low‐back‐pain‐say‐nice‐draft‐proposals
At the same time, this review is being suggested as an example of a review with *positive* results to be used to teach students about Cochrane.
http://community.cochrane.org/news/speaking‐to‐students‐about‐cochrane
I realise the condition is different, but it concerns me that most or all of the authors of this review practice and teach acupuncture.
Reply
Response prepared by the author team, Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Shin BC, Vickers A, White AR.
The comment refers to a website commenting on a draft document on low back pain by NICE. We do not think that we as authors of a review on tension‐type headache should discuss in detail a draft of a guideline for a quite different condition, particularly, as serious concerns regarding the evidence summary underlying the draft and the conclusions drawn have been raised (http://blogs.bmj.com/aim/).
If the editors of the Cochrane Library choose our review as an example for teaching we are pleased, but we neither had any influence on this decision nor do we think we should justify or comment on it. We tried our best to summarize the available data and carefully discuss our findings including the limitations of the evidence.
Caroline Struthers is concerned “that most or all of the authors of this review practice and teach acupuncture”. First, at least two of the authors (A Vickers, a statistician, and K Linde, a clinical epidemiologist) have never practiced acupuncture. Second, only one of the authors (G Allais) actually teaches the practice of acupuncture, but he is also a headache specialist and head of a University Headache Center in which all types of pharmacological approaches to headache treatment are regularly used. Third, reporting the results of research at acupuncture meetings is not “teaching acupuncture”. Systematic reviews of any treatment involve both methodologists and context experts. We think it is a distinct strength that we included epidemiologists, a trial statistician, acupuncture experts who published high‐quality acupuncture trials, and acupuncturists using this treatment clinically. Our review is no different from a review of surgery, where there might be some statisticians and some surgeons.
Editor note, added 10 August 2016: Please note that author ‘employment in a clinical speciality relevant to the Cochrane Review should be declared in the interests of transparency, but this does not prevent an individual from being a review author, including taking on the role of lead (first) author.’ (see http://community.cochrane.org/editorial‐and‐publishing‐policy‐resource/ethical‐considerations/conflicts‐interest‐and‐cochrane‐reviews).
Contributors
Feedback Editor Kate Seers, Managing Editor Anna Erskine, and Co‐ordinating Editor Christopher Eccleston.
Feedback submitted, 19 July 2016
Summary
Date of Submission: 19‐Jul‐2016
Name: Christopher Labos
Email Address: christopher.labos@mail.mcgill.ca
Affiliation: not stated
Role: not stated
I read with interest the recent review by Linde et al. entitled "Acupuncture for the prevention of tension ‐ type headache." However I number of concerns regarding the data as it is presented in the paper.
Having manually re‐read the paper by Endres et al. that is cited in the paper I notice some discrepancies between the published data and the data included in this meta‐analysis.
In the original paper Endres provides the following data for >50% reduction in headache days.
At 6 weeks 138/204 vs. 106/191, at 3 months 119/199 vs. 91/192, 135/204 vs. 106/194.
This data is different than the data provided by Linde et al. in their paper and may serve to conflate the effect size.
On another matter, I do not believe it is appropriate to perform a fixed effects meta‐analysis in this setting. Regardless of what the I‐square statistic is, given the differences in study designs and patient populations, a random effects meta‐analysis would have been more appropriate and I believe it should included in the analysis.
Reply
Christopher Labos is correct in noting that the response data in the Endres et al. [1] paper are slightly different from those used in our meta‐analyses. There are two reasons for this:
As described in our method section (page 7) we use as response criterion ≥ 50 reduction of headache frequency as recommended in the guidelines of International Headache Society for controlled trials in tension‐type headache ([2], page 11). Endres et al. used the slightly different criterion of >50% for their original analyses. As we had access to the individual patient data of the Endres trial through the Acupuncture Trialists’ Collaboration (see page 6 in our review) we re‐calculated response data to keep the analysis approach across trials as similar as possible. We believe this is more than reasonable;
Throughout the review we used the number of patients randomized to a group as denominator to calculate the percentage of responders counting patients with missing data as non‐responders.
Using the data originally reported by Endres et al. for meta‐analysis for calculating pooled risk ratios results in similar effects sizes (1.22 at up to 8 weeks, 1.20 at up to 4 months and 1.18 at up to 6 months) as in our calculations (1.26, 1.27 and 1.17, respectively).
There is debate among statisticians whether fixed or random effect models should be preferred. Clearly, the fixed effect meta‐analysis is a valid test of the null hypothesis of no effect. Furthermore, in five of six meta‐analyses presented in our review I² was 0. In these cases point estimates and confidence intervals are identical in random and fixed effects models. Only in the meta‐analysis of response up to 8 week I² was 16%. Using a random effects model results in the same point estimate as in the4 fixed effects model with slightly wider confidence intervals (1.26 [1.10, 1.45]).
Klaus Linde and Andrew Vickers
1. Endres HG, Böwing G, Diener HC, Lange S, Maier C, Molsberger A, Zenz M, Vickers AJ, Tegenthoff M. Acupuncture for tension‐type headache: a multicentre, sham‐controlled, patient‐and observer‐blinded, randomised trial. J Headache Pain. 2007;8:306‐14.
2. Bendtsen L, Bigal ME, Cerbo R, Diener HC, Holroyd K, Lampl C, Mitsikostas DD, Steiner TJ, Tfelt‐Hansen P; International Headache Society Clinical Trials Subcommittee. Guidelines for controlled trials of drugs in tension‐type headache: second edition. Cephalalgia. 2010 Jan;30(1):1‐16.
Contributors
Feedback Editor Kate Seers, Managing Editor Anna Erskine, and Co‐ordinating Editor Christopher Eccleston.
What's new
| Date | Event | Description |
|---|---|---|
| 10 August 2016 | Feedback has been incorporated | See Feedback 2. |
History
Protocol first published: Issue 3, 1998 Review first published: Issue 1, 2009
| Date | Event | Description |
|---|---|---|
| 12 July 2016 | Feedback has been incorporated | See Feedback. |
| 5 April 2016 | Review declared as stable | See Published notes. |
| 19 January 2016 | New citation required but conclusions have not changed | I. Compared to the previous version we have updated the search; slightly modified the selection criteria; included a new trial; modified the wording of the conclusions; and added GRADE assessments of the evidence. II. We updated the main search on 19 January 2016 (with further update searches in PubMed and the WHO Clinical Trials Platform on 10 February 2016). III. We identified and included one new eligible trial (Kwak 2007). IV. The 12 trials reviewed include 2349 participants; the 11 trials in the previous version included 2317 participants. V: We performed no new analyses. VI. We have slightly modified the wording of the conclusions, mainly reflecting the change in the general knowledge base on acupuncture. |
| 19 January 2016 | New search has been performed | We have updated this review to include the results of a new search; slightly modified the selection criteria; included a new trial; and modified the wording of the conclusions. |
| 10 August 2009 | Amended | Contact details updated. |
| 29 January 2009 | Amended | Contact details updated. |
| 7 November 2008 | New citation required and conclusions have changed | 1) A previously published Cochrane review on 'Acupuncture for idiopathic headache' has been split into two reviews: the present review on 'Acupuncture for tension‐type headache' and a separate review on 'Acupuncture for migraine prophylaxis'. 2) Six new trials of acupuncture for tension‐type headache are included in the present review (Endres 2007; Jena 2008; Karst 2001; Melchart 2005; Söderberg 2006; White 2000). 3) Conclusions have changed as follows: In the previous version of this review, the evidence in support of acupuncture for tension‐type headache was considered insufficient. Now the authors conclude that acupuncture might be considered as a treatment option for frequent episodic or chronic tension‐type headache, although the selection of specific acupuncture points may not be as important as has been thought by providers. 4) The list of review authors has been slightly amended vis‐à‐vis the earlier review (D Melchart and B Berman no longer authors; E Manheimer added as new author). |
| 9 May 2008 | Amended | Converted to new review format. |
| 9 January 2008 | New search has been performed | All searches updated. |
Notes
A new search is not likely to identify any potentially relevant studies likely to change the conclusions. Therefore, this review has now been stabilised following discussion with the authors and editors. The review will be re‐assessed for updating in ten years.
Acknowledgements
We would like to thank the following individuals: the study authors who provided additional information on their trials; Emily Vertosick who provided data from the Acupuncture Trialists Collaboration for our analyses (she re‐analysed individual patient data trial included in the database in a manner that allowed us to enter means, standard deviations, numbers of responders and numbers of observations); Joanne Abbott for performing update searches; Anna Erskine for answering many questions during the update process; and the peer reviewers Janet Wale, Remy Coeytaux and Elliot Shevel for their feedback on the draft of our update.
We acknowledge the institutional support from Cancer Center Support Grant P30 CA008748 (PI: Craig B. Thompson) for Andrew Vickers.
Eric Manheimer, Dieter Melchart, Patricia Fischer and Brian Berman were involved in previous versions of the review.
Cochrane Review Group funding acknowledgement: The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane PaPaS Group. Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, National Health Service (NHS) or the Department of Health.
Appendices
Appendix 1. Search strategy
CENTRAL (The Cochrane Library)
#1 MeSH descriptor: [Acupuncture Therapy] explode all trees
#2 (acupunct* or electroacupunct* or electro‐acupunct*):ti,ab,kw (Word variations have been searched)
#3 #1 or #2
#4 MeSH descriptor: [Headache Disorders] explode all trees
#5 MeSH descriptor: [Headache] this term only
#6 (headache* or migrain* or cephalgi* or cephalalgi*):ti,ab,kw (Word variations have been searched)
#7 #4 or #5 or #6
MEDLINE (OVID)
1. exp Acupuncture Therapy/
2. (acupunct$ or electroacupunct$ or electro‐acupunct$).mp.
3. 1 or 2
4. exp HEADACHE DISORDERS/
5. HEADACHE/
6. (headache$ or migrain$ or cephalgi$ or cephalalgi$).mp.
7. 4 or 5 or 6
8. 3 and 7
9. randomized controlled trial.pt.
10. controlled clinical trial.pt.
11. randomized.ab.
12. placebo.ab.
13. drug therapy.fs.
14. randomly.ab.
15. trial.ab.
16. groups.ab.
17. 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16
18. exp animals/ not humans.sh.
19. 17 not 18
20. 8 and 19
EMBASE (OVID)
1. exp acupuncture/
2. (acupunct$ or electroacupunct$ or electro‐acupunct$).mp.
3. 1 or 2
4. headache/
5. (headache$ or migrain$ or cephalgi$ or cephalalgi$).mp.
6. 4 or 5
7. 3 and 6
8. random$.tw.
9. factorial$.tw.
10. crossover$.tw.
11. cross over$.tw.
12. cross‐over$.tw.
13. placebo$.tw.
14. (doubl$ adj blind$).tw.
15. (singl$ adj blind$).tw.
16. assign$.tw.
17. allocat$.tw.
18. volunteer$.tw.
19. Crossover Procedure/
20. double‐blind procedure.tw.
21. Randomized Controlled Trial/
22. Single Blind Procedure/
23. or/8‐22
24. (animal/ or nonhuman/) not human/
25. 23 not 24
26. 7 and 25
AMED (OVID)
1. exp acupuncture therapy/
2. (acupunct$ or electroacupunct$ or electro‐acupunct$).mp. [mp=abstract, heading words, title]
3. 1 or 2
4. exp headache/
5. (headache$ or migrain$ or cephalgi$ or cephalalgi$).mp. [mp=abstract, heading words, title]
6. 4 or 5
7. 3 and 6
8. exp clinical trials/
9. (random* or trial*).mp. [mp=abstract, heading words, title]
10. placebo.mp.
11. 8 or 9 or 10
12. 7 and 11
Data and analyses
Comparison 1. Acupuncture versus no acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 2 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Up to 8 weeks/2 months after randomisation | 1 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 3 to 4 months after randomisation | 2 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 5 to 6 months after randomisation | 0 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 > 6 months after randomisation | 0 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of headache days | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Up to 8 weeks/2 months after randomisation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 3 to 4 months after randomisation | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 5 to 6 months after randomisation | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 > 6 months after randomisation | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Headache intensity | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Up to 8 weeks/2 months after randomisation | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 3 to 4 months after randomisation | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 5 to 6 months after randomisation | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 > 6 months after randomisation | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Safety/acceptability | 1 | Odds Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Number of participants dropping out due to adverse effects | 1 | 207 | Odds Ratio (IV, Fixed, 95% CI) | 1.72 [0.07, 42.81] |
| 4.2 Number of participants reporting adverse effects | 0 | 0 | Odds Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.4. Analysis.
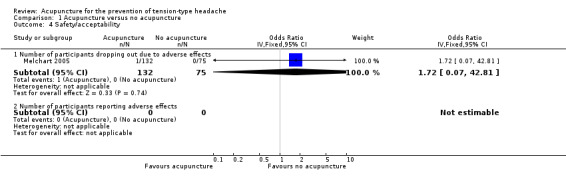
Comparison 1 Acupuncture versus no acupuncture, Outcome 4 Safety/acceptability.
Comparison 2. Acupuncture versus sham interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 5 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Up to 8 weeks/2 months after randomisation | 4 | 723 | Risk Ratio (IV, Fixed, 95% CI) | 1.26 [1.10, 1.45] |
| 1.2 3 to 4 months after randomisation | 4 | 703 | Risk Ratio (IV, Fixed, 95% CI) | 1.27 [1.09, 1.48] |
| 1.3 5 to 6 months after randomisation | 4 | 723 | Risk Ratio (IV, Fixed, 95% CI) | 1.17 [1.02, 1.35] |
| 1.4 > 6 months after randomisation | 1 | 30 | Risk Ratio (IV, Fixed, 95% CI) | 1.5 [0.53, 4.26] |
| 2 Number of headache days | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Up to 8 weeks/2 months after randomisation | 4 | 682 | Mean Difference (IV, Fixed, 95% CI) | ‐1.49 [‐2.58, ‐0.39] |
| 2.2 3 to 4 months after randomisation | 4 | 653 | Mean Difference (IV, Fixed, 95% CI) | ‐1.62 [‐2.69, ‐0.54] |
| 2.3 5 to 6 months after randomisation | 4 | 670 | Mean Difference (IV, Fixed, 95% CI) | ‐1.51 [‐2.59, ‐0.43] |
| 2.4 > 6 months after randomisation | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Headache intensity | 5 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Up to 8 weeks/2 months after randomisation | 3 | 143 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.45, 0.21] |
| 3.2 3 to 4 months after randomisation | 4 | 655 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.26, 0.05] |
| 3.3 5 to 6 months after randomisation | 4 | 670 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.35, ‐0.04] |
| 3.4 > 6 months after randomisation | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Analgesic use | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Up to 8 weeks/2 months after randomisation | 3 | 266 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.56, ‐0.06] |
| 4.2 3 to 4 months after randomisation | 3 | 261 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.56, ‐0.05] |
| 4.3 5 to 6 months after randomisation | 1 | 167 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.48, 0.17] |
| 4.4 > 6 months after randomisation | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐1.06, 0.39] |
| 5 Safety/acceptability | 7 | Odds Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Number of participants dropping out due to adverse effects | 6 | 763 | Odds Ratio (IV, Fixed, 95% CI) | 1.45 [0.06, 36.06] |
| 5.2 Number of participants reporting adverse effects | 3 | 277 | Odds Ratio (IV, Fixed, 95% CI) | 1.26 [0.60, 2.65] |
2.5. Analysis.
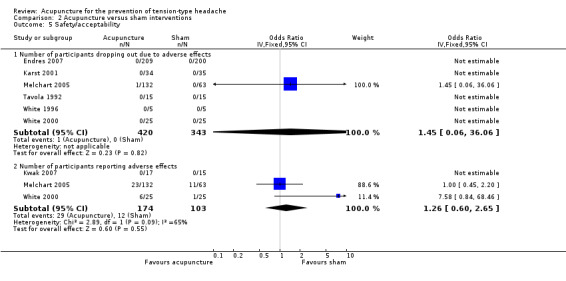
Comparison 2 Acupuncture versus sham interventions, Outcome 5 Safety/acceptability.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ahonen 1984.
| Methods | Blinding: none Dropouts/withdrawals: unclear Observation period: baseline 2 months; treatment unclear, no follow‐up Assessment of acupunctures: GA differently/60% ‐ BB differently/30% | |
| Participants | Number of participants included/analysed: unclear/22 Condition: myogenic headache Demographics: mean age 46 years (acupuncture) and 37 (control); 82% female Setting: neurological outpatient department of university hospital in Finland Time since onset of headaches: 5.7 years | |
| Interventions | Acupuncture points: GB8, GB20, BL10, BL12, BL15, Chuanxi and pressure points on the neck No information on acupuncturist(s) DeChi achieved?: no information Number of treatment sessions: unclear (10 minutes each) Frequency of treatment sessions: no information Control intervention: physiotherapy (parafango, massage, ultrasound) | |
| Outcomes | Method for outcome measurement: point measurement (no diaries); pain intensity (visual analogue scale) and muscle tension (EMG) were measured Only data for follow‐up and number of participants with global response, response regarding frequency and medication were presented | |
| Notes | Insufficient reporting; unclear whether there were dropouts/withdrawals, poor outcome measurement; sample size too small to assess equivalence of the 2 therapies | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No mention of attrition |
| Incomplete follow‐up outcome data addressed? | Unclear risk | No mention of attrition |
| Selective reporting (reporting bias) | High risk | Visual analogue scales have been used but only global responder measures are reported |
Carlsson 1990.
| Methods | Blinding: not blinded Dropout/withdrawals: bias possible (8/31 dropouts in acupuncture group, 2/31 in physiotherapy group) Observation period: baseline 3 to 8 weeks; treatment 2 to 8 weeks; follow‐up 7 to 12 months Assessment of acupuncture: GA completely differently/10% ‐ BB completely different/20% | |
| Participants | Number of participants included/analysed: 62/52 Condition: chronic tension headache (ad hoc) Demographics: mean age 34 years; all female Setting: hospital/outpatient department, Sweden Time since onset of headaches: mean 9 years | |
| Interventions | Acupuncture points: local points: GB 20, GB 21; distal points: LI 4 Information on acupuncturists: n = 2; no further information DeChi achieved?: yes Number of treatment sessions: 4 to 10 sessions of 20 minutes each Frequency of treatment sessions: 1 to 2/week Control intervention: individualised physiotherapy (10 to 12 sessions of 30 to 45 minutes each, including relaxation, auto‐massage, TENS, cryotherapy, coping techniques) | |
| Outcomes | Method for outcome measurement: point measurement (no diary) Outcomes: visual analogue scales, Likert scales for intensity and frequency, Sickness Impact Profile, Mood Adjective Check List | |
| Notes | Multiple publication; dropouts different between groups; control group got more therapy than acupuncture group Data for effect size estimation re‐calculated from data presented in the publication Pain Clinic 1990 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | Information from author: "The randomisation was done in blocks of 4. In an envelope there were 4 pieces of paper which were folded two times and signed with A for acupuncture and R for relaxation (two of each). For each patient one piece of paper was drawn 'blinded' until all were taken." |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2 participants randomised to acupuncture did not enter the treatment phase. A further 6 acupuncture and 2 physiotherapy participants dropped out (reasons not related to efficacy). 23 of 31 randomised to acupuncture and 29 of 31 randomised to physiotherapy participants in analysis. Dropouts seem to have been excluded from all analyses. |
| Incomplete follow‐up outcome data addressed? | Unclear risk | See above |
| Selective reporting (reporting bias) | Unclear risk | No predefined outcome measure; a number of relevant measures presented in figures, others summarised in text; no indication that there was a major selection |
Endres 2007.
| Methods | Blinding: participants, telephone interviewers; blinding tested and successful Dropouts/withdrawals: only a very small number of participants, bias unlikely Observation period: 4 weeks baseline; 6 weeks treatment; 20 weeks follow‐up Assessment of acupuncture: GA similarly/40% ‐ BB similarly/75% | |
| Participants | Number of participants included/analysed: 409/409 Condition: episodic or chronic tension‐type headache (IHS) Demographics: median age 38 years (range 29 to 48 years); 78% female Setting: 122 primary care practices in Germany Time since onset of headaches: median 7.3 (acupuncture) and 8.7 (sham) years (range 3.1 to 18.3 years) | |
| Interventions | Acupuncture points: semi‐standardised ‐ depending on Chinese syndrome diagnosis, predefined collections of obligatory and flexible points Information on acupuncturists: 122 primary care physicians; at least 140 hours of acupuncture training, average experience 8.5 years (range 2 to 36 years) DeChi achieved?: yes Number of treatment sessions: 10 (if moderate response further 5 sessions possible) Frequency of treatment sessions: 2/week Control intervention: sham acupuncture (superficial needling at distant non‐acupuncture points) | |
| Outcomes | Method for outcome measurement: diary and interviews Main outcome measure: at least 50% frequency reduction and no protocol violations Other outcomes: number of headache days per 4 weeks, at least 50% frequency reduction (regardless of protocol violations), quality of life (SF‐12), von Korff chronic pain grading scale, global patient rating | |
| Notes | Large, rigorous trial with unusual main outcome measure (responders were re‐classified to non‐responders for various reasons, for example if there were minor changes in acute medication (participants were allowed to use only one of their pre‐baseline oral headache analgesics)). The trial initially included a third arm with amitriptyline, which had to be close as no one was willing to be randomised to this arm(therefore this arm was closed). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer program |
| Allocation concealment (selection bias) | Low risk | Central telephone randomisation procedure |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and telephone interviewers were blinded. Test of blinding suggests successful blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate and intention‐to‐treat analyses |
| Incomplete follow‐up outcome data addressed? | Low risk | Low attrition rate and intention‐to‐treat analyses |
| Selective reporting (reporting bias) | Low risk | Primary outcome predefined, good presentation of relevant secondary outcomes |
Jena 2008.
| Methods | Sequence generation: computer program (information from author) Concealment: central telephone randomisation (information from author) Blinding: none Dropouts/withdrawals: 1479 of 1613 included in the acupuncture group with 3‐month data versus 1456 of 1569 in the control group; sensitivity analyses with missing values replaced confirm main analysis based on available data Observation period: no baseline period; treatment 3 months; no follow‐up (for randomised comparison) Assessment of acupuncture: GA insufficient information for an assessment ‐ BB ? | |
| Participants | Number of participants included/analysed: 3182/2935 with migraine or TTH (of those included 1265 with TTH, no information on numbers of TTH participants analysed) Condition: migraine and/or tension‐type headache (IHS) Demographics: mean age 44 years, 77% female (for total group) Setting: several thousand practices in Germany Time since onset of headaches: 10.8 years (for total group) | |
| Interventions | Acupuncture points: individualised selection Information on acupuncturists: multiple physicians with at least 140 hours of acupuncture training DeChi achieved?: no information Number of treatment sessions: up to a maximum of 15 Frequency of treatment sessions: individualised Control intervention: waiting list receiving "usual care" | |
| Outcomes | Method for outcome measurement: questionnaires, no diary Primary outcome: headache days in the third month Other outcomes: intensity, quality of life | |
| Notes | Large, very pragmatic study including both participants with migraine and tension‐type headache reporting some outcomes for headache subgroups; treating physicians were completely free to choose points, number of sessions (upper limit allowed 15) etc. Unclear what usual care consisted of. Some diagnostic misclassification likely. Authors provided raw means, standard deviations and number of observations for headache days and headache intensity. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer program |
| Allocation concealment (selection bias) | Low risk | Central telephone randomisation |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate and sensitivity analyses with replacing missing values confirming main analyses |
| Incomplete follow‐up outcome data addressed? | Unclear risk | No randomised comparison after 3 months |
| Selective reporting (reporting bias) | Low risk | Limited outcome measurement. Data on relevant outcomes for the subgroup of participants suffering from tension‐type headache provided by authors. |
Karst 2001.
| Methods | Blinding: participants (blinding tested), examiner, statistician Dropouts/withdrawals: 61 (32 versus 29) of 69 (34 versus 35) completed treatment, 55 (27 versus 24) included in the long‐term follow‐up (information from author) Observation period: 4 weeks baseline; 10 weeks treatment; 5 months follow‐up Assessment of acupuncture: GA differently/25% ‐ BB differently/40% | |
| Participants | Number of participants included/analysed: 69/61 Condition: episodic (22) or chronic (39) tension‐type headache (IHS) Demographics: mean age 48 years, 55% female Setting: academic physical medicine outpatient department, Hannover, Germany Time since onset of headaches: not reported in publication; first author confirms that > 6 months was an inclusion criterion | |
| Interventions | Acupuncture points: GB20, LI4, LR3 in all participants + selection of points to be chosen individually according to symptoms Information on acupuncturists: n = 5 (3 highly experienced, 2 with limited experience) (information from author) DeChi achieved?: achieved in majority of participants (information from author) Number of treatment sessions: 10 Frequency of treatment sessions: 2/week Control intervention: non‐penetrating placebo needle treatment at true acupuncture points | |
| Outcomes | Method for outcome measurement: diary and questionnaires Outcomes: number of headache days per month, analgesic use, pain intensity, site and duration of headache attacks, overall rating on a visual analogue scale and Clinical Global Impression Index, Nottingham Health Profile, Everyday Life Questionnaire, Freiburg Questionnaire of Coping with Illness, and von Zerssen Depression Scale | |
| Notes | Sham needles fixed at true acupuncture points; additional information from authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer program (information from author) |
| Allocation concealment (selection bias) | Unclear risk | Allocation after inclusion of a patient checked in a random number list by independent secretary (information from author) |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Non‐penetrating (Streitberger) needle at true points used as sham treatment. Test of blinding suggests successful blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Incomplete description in the publication but the author provided copies of an unpublished report with relevant information. Analyses were performed based on the available data. Completion of treatment 32/34 (acupuncture) versus 29/35 (sham), 6‐week follow‐up available for 27/34 versus 30/35. |
| Incomplete follow‐up outcome data addressed? | Unclear risk | 5 month follow‐up data available for 31/34 versus 24/35 participants |
| Selective reporting (reporting bias) | Low risk | No primary outcome reported, but table provides a good summary of the most relevant outcome measures |
Kwak 2007.
| Methods | Blinding: participants (blinding tested) Dropouts/withdrawals: unclear (only number of participants analysed reported) Observation period: unclear baseline; 4 weeks treatment; 12 weeks follow‐up Assessment of acupuncture: BCS ‐ similarly/70% | |
| Participants | Number of participants included/analysed: unclear/32 Condition: chronic tension‐type headache (IHS second edition) Demographics: mean age 45 versus 49 years, 81% female Setting: Daejon University Hospital (for traditional Korean medicine) Time since onset of headaches: mean 73 versus 69 months | |
| Interventions | Acupuncture points: tailored selection of acupoints following participants symptoms:
Posterior or superior headache: LI1(T), BL67(T), BL40(S), ST36(S) + GB20, GV20, Intang (extra)
Anterior headache: GB41(T), ST43(T), LI1(S), ST45(S) + Intang (extra)
Sphenoidal headache: LI1(T), GB44(T), SI5(S), GB38(S) + Taiyang (extra
With shoulder pain: +GB43(T), BL66(T), GB44(S), LI1(S) Information on acupuncturists: not reported DeChi achieved?: unclear Number of treatment sessions: 8 Frequency of treatment sessions: 2/week Control intervention: sham acupuncture (non‐acupoints, 20 mm lateral side, total 6 points) |
|
| Outcomes | Method for outcome measurement: diary and questionnaires Outcomes: primary outcome VAS, HDI (Henry Ford Headache Disability Inventory), Likert scale, algometer score | |
| Notes | Additional information from first author sought but no response received | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Balanced block randomisation (random number table) |
| Allocation concealment (selection bias) | Unclear risk | Blinded physician included participants; information to treatment providers by phone or email (but by whom?) |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants blinded, minimised communication between acupuncturists and participants; allocation guesses does not suggest unblinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of participants randomised and attrition not reported |
| Incomplete follow‐up outcome data addressed? | Unclear risk | No long‐term follow‐up |
| Selective reporting (reporting bias) | Low risk | Results for measured outcomes reported |
Melchart 2005.
| Methods | Blinding: participants, diary evaluators Dropouts/withdrawals: major bias unlikely Observation period: baseline 4 weeks; treatment 8 weeks; follow‐up 12 weeks Assessment of acupuncture: AW similarly/60% ‐ GA exactly as in the study/95% | |
| Participants | Number of participants included/analysed: 270/234 Condition: episodic and chronic tension‐type headache (IHS) Demographics: mean age 43 years, 74% female Setting: 28 primary care practices in Germany Time since onset of headaches: mean 14.5 years | |
| Interventions | Acupuncture points: in all participants GB20, GB21 and LIV3, additional optional points recommended according to symptoms Information on acupuncturists: n = 42, at least 160 hours of training DeChi achieved?: yes Number of treatment sessions: 12 Frequency of treatment sessions: 2/week for 4 weeks, then 1/week for 4 weeks Control intervention 1: minimal acupuncture (superficial needling at non‐acupuncture points) Control 2: no acupuncture waiting list group (participants only treated acute headaches with analgesics and received acupuncture 12 weeks after randomisation) | |
| Outcomes | Method for outcome measurement: diary and pain questionnaires Main outcome measure: difference in the number of headache days between baseline and weeks 9 to 12 Other outcomes: headache days, intensity, analgesic use, duration, headache score, global intensity rating, quality of life (SF‐36), depressive symptoms (CES‐D), emotional aspects of pain (SES), disability (PDI) | |
| Notes | Additional information for effect size calculation taken from unpublished study report (response, number of headache days, analgesic use and headache score in weeks 5 to 8) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer program |
| Allocation concealment (selection bias) | Low risk | Central telephone randomisation |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and diary evaluators were blinded for comparison with sham. Participants were informed that two different types of acupuncture were compared. Early tests of blinding indicate successful blinding, but at follow‐up guesses about allocation status were different between groups (P value = 0.08). Comparison with no treatment not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate and intention‐to‐treat analyses |
| Incomplete follow‐up outcome data addressed? | Low risk | Low attrition rate and intention‐to‐treat analyses |
| Selective reporting (reporting bias) | Low risk | Detailed presentation of main results |
Söderberg 2006.
| Methods | Blinding: no blinding Dropouts/withdrawals: no dropouts until treatment completion, 11 participants with missing data at 3 months follow‐up and 34 at 6 months could not be analysed (main reasons lacking headache diaries) Observation period: 4 weeks baseline; 2.5 to 3 months treatment; 7 months follow‐up Assessment of acupuncture: GA differently/65% ‐ BB differently/50% | |
| Participants | Number of participants included/analysed: 90/90 Condition: chronic tension‐type headache (IHS) Demographics: mean age 37.5 years, 81% female Setting: 3 physiotherapy clinics in Sweden Time since onset of headaches: median duration 7.5 years | |
| Interventions | Acupuncture points: mandatory GB20, GB14, LI4, ST44, optional PC6, PC7, SP6, BG34, ST8, EX1 and EX2 Information on acupuncturists: 5 experienced physiotherapists DeChi achieved?: yes Number of treatment sessions: 12 Frequency of treatment sessions: 1/week Control intervention 1: physical training (10 sessions at the clinic + 15 home training sessions; exercises focusing on neck and shoulder muscles) Control intervention 2: relaxation (progressive muscle relaxation and autogenic relaxation techniques, breathing, stress coping) | |
| Outcomes | Method for outcome measurement: diary, pain rating Outcomes: headache intensity, headache‐free days, headache‐free periods | |
| Notes | Some additional information received from first author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sealed, opaque envelopes were prepared and mixed in a box. After inclusion of a patient, an envelope was taken from the box. |
| Allocation concealment (selection bias) | Unclear risk | See above |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate and intention‐to‐treat analysis |
| Incomplete follow‐up outcome data addressed? | Unclear risk | More than a third of participants were lost to follow‐up (dropout rates similar in all 3 groups and intention‐to‐treat analysis) |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported |
Tavola 1992.
| Methods | Blinding: participants and data‐collecting physician Dropouts/withdrawals: none (all participants completed the follow‐up) Observation period: baseline 4 weeks; treatment 8 weeks; follow‐up 12 months Assessment of acupuncture: GA (probably) exactly the same way/80% ‐ BB exactly the same way/90% | |
| Participants | Number of participants included/analysed: 30/30 Condition: tension‐type headache (ad hoc criteria) Demographics: mean age 33 years; 87% female Setting: headache outpatient department of a university hospital in Italy Time since onset of headaches: mean 8 years | |
| Interventions | Acupuncture points: individualised according to traditional Chinese medicine, possibility of changing points Information on acupuncturist: n = 1 DeChi achieved?: yes Number of treatment sessions: 8 (20 minutes each) Frequency of treatment sessions: 1/week Control intervention: sham (non‐acupuncture points in the same regions) | |
| Outcomes | Method for outcome measurement: diary Outcomes: headache score, duration, frequency, intensity, analgesic use, response | |
| Notes | Rigorous trial; acupuncture seems to be clearly better in all outcomes, but most differences are not statistically significant; surprisingly negative conclusions Number of headache days at 3 months recalculated from baseline values and percentage reduction. As no standard deviation was available, the pooled baseline standard deviation was used. Data for headache index and analgesic use extrapolated from figures. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and physician collecting the diaries were blinded. Description of the procedure suggests adequate blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Explicit statement that there were no losses to follow‐up |
| Incomplete follow‐up outcome data addressed? | Low risk | Explicit statement that there were no losses to follow‐up |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported in figures or text |
White 1996.
| Methods | Blinding: participants and evaluator Dropouts/withdrawals: bias unlikely Observation period: 3 weeks baseline; 6 weeks treatment; 3 weeks follow‐up Assessment of acupuncture: GA similarly/25% ‐ BB similarly/65% | |
| Participants | Number of participants included/analysed: 10/9 Condition: tension‐type headache (IHS) Demographics: mean age 57 years; 8 women Setting: unclear, UK Time since onset of headaches: 32 and 36 years on average | |
| Interventions | Acupuncture points: 2 to 6 local points, LI4 Information on acupuncturist: n = 1, GP "who recently attended a basic acupuncture course" DeChi achieved?: probably in most cases Number of treatment sessions: 6 (brief needling) Frequency of treatment sessions: 1/week Control intervention: sham procedure (plastic guide tube and cocktail stick on 4 body regions without known acupuncture points) | |
| Outcomes | Method for outcome measurement: diary with intensity, duration and medication. Questions on blinding. | |
| Notes | This methodologically rigorous pilot study is uninterpretable due to relevant baseline differences; more pain‐free weeks in true acupuncture group; only brief needling | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer program |
| Allocation concealment (selection bias) | Low risk | Central telephone randomisation |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants blinded (procedure mimicking needle insertion). Credibility testing suggests successful blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 of 5 participants (20%) in the acupuncture group dropped out |
| Incomplete follow‐up outcome data addressed? | Unclear risk | No follow‐up performed |
| Selective reporting (reporting bias) | Low risk | Relevant outcome reported |
White 2000.
| Methods | Blinding: participants (blinding tested), study nurse Dropouts/withdrawals: bias unlikely for early follow‐up (8 weeks after randomisation), but possible for follow‐up 3 months after treatment Observation period: 3 weeks baseline; 5 weeks treatment; 3 months follow‐up Assessment of acupuncture: GA differently/25% ‐ BB differently/45% | |
| Participants | Number of participants included/analysed: 50/50 Condition: episodic tension‐type headache (although during baseline several participants had headaches on more than half of all days) Demographics: mean age 49 years, 76% female Setting: 4 primary care practices and 1 university institute in the UK Time since onset of headaches: mean 20 years | |
| Interventions | Acupuncture points: obligatory GB20 and LI4 + 4 optional, individualised points Information on acupuncturists: members of the British Medical Acupuncture Society DeChi achieved?: yes Number of treatment sessions: 8 Frequency of treatment sessions: first 6 treatments weekly, then 1/month for 2 months Control intervention: sham treatment (tapping a blunted cocktail stick in a guide tube against bony prominences) | |
| Outcomes | Method for outcome measurement: diary and questionnaires Main outcome measure: number of headache days Other outcomes: intensity, duration, analgesic use, General Health Questionnaire, global assessments | |
| Notes | Non‐traditional acupuncture technique (brief needling without needle retention) For analyses of headache frequency the data reported for headache days per week were multiplied by 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer program |
| Allocation concealment (selection bias) | Low risk | Central telephone randomisation |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and assisting nurses were blinded. Test of blinding suggests successful blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate and intention‐to‐treat analysis |
| Incomplete follow‐up outcome data addressed? | Unclear risk | 10 of 25 (acupuncture group) and 6 of 25 (sham group) participants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes presented |
Wylie 1997.
| Methods | Blinding: post‐treatment care Dropouts/withdrawals: unclear Observation period: baseline 4 weeks; treatment/follow‐up unclear Assessment of acupuncture: GA insufficient information for an assessment ‐ BB similarly/70% | |
| Participants | Number of participants included/analysed: 67/? Condition: 27 migraine or migraine + tension‐type headache, 40 tension‐type headache (IHS) Demographics: mean age 38 years; 67% female Setting: headache outpatient department, UK Time since onset of headaches: mean 10 years | |
| Interventions | Acupuncture points: chosen individually according to traditional Chinese medicine No information on acupuncturist(s) DeChi achieved?: no information Number of treatment sessions: 6 Frequency of treatment sessions: unclear Control intervention: massage and relaxation | |
| Outcomes | Method for outcome measurement: diary Outcomes: pain index, headache index (psychological variables only at baseline) | |
| Notes | Insufficiently reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants unblinded. Follow‐up assessments carried out by blinded clinician. Most outcome measures patient‐rated. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 82 participants agreed to enter study; 67 started treatment and seemed to have completed the study |
| Incomplete follow‐up outcome data addressed? | Unclear risk | No follow‐up performed |
| Selective reporting (reporting bias) | Unclear risk | Insufficient presentation of results |
Assessment of acupuncture: Raters: GA=Gianni Allais, BB=Benno Brinkhaus, YF=Yutong Fei, BCS=Byung‐Cheul Shin, AW=Adrian White (further details see section 'Assessment of the adequacy of the acupuncture intervention') DeChi: irradiating sensation said to indicate effective needling EMG: electromyography IHS: International Headache Society TENS: transcutaneous electrical nerve stimulation TTH: tension‐type headache VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Borglum‐Jensen 1979 | Methods: random allocation unlikely |
| Chassot 2015 | Cross‐over trial with 2 x 5 weeks of treatment (acupuncture or sham) with 2 weeks washout in between. Unclear whether outcomes were measured for 2 x 5 weeks only (no follow‐up after phase 2); in any case duration of observation was < 8 weeks per phase |
| Coeytaux 2005 | RCT in participants with chronic daily headache |
| Ebneshahidi 2005 | RCT on laser acupuncture (no needling) in participants with chronic tension‐type headache |
| Gottschling 2008 | Intervention: laser acupuncture without skin penetration Participants: both children with migraine and tension‐type headache included ‐ no results for tension‐type headache patients alone presented |
| Guerreiro da Silva 2012 | Trial included only pregnant women in whom headache started during pregnancy |
| Hamp 1999 | Randomised trial of relaxation and acupuncture in children with tension‐type headache |
| Hansen 1985 | Cross‐over study with less than 8 weeks observation (3 weeks treatment + 3 weeks follow‐up) per period in participants with chronic tension‐type headache |
| Hong 2007 | Only 2 weeks treatment and 1 week observation; possibly participants with recent onset of headaches |
| Karakurum 2001 | RCT comparing dry needling with subcutaneous needle insertion in 30 participants with tension‐type headache. Reason for exclusion: only 4 weeks post‐randomisation observation period. |
| Lavies 1998 | Small randomised trial of laser acupuncture (no skin penetration) versus sham laser in participants with migraine or tension‐type headache |
| Loh 1984 | Participants: both participants with migraine and tension‐type headache included. No separate results for participants with tension‐type headache presented. |
| Shi 2000 | RCT of acupuncture versus inactivated laser in participants with "therapy‐resistant headache" (exact headache diagnoses not reported). Insufficiently reported. |
| Sozen 2013 | Trial in participants with chronic daily headache (chronic migraine or chronic tension‐type headache without presenting results for subgroups) |
| Tekeoglu 1995 | Intervention: electroacupuncture versus music sound electroacupuncture |
| Turk 1990 | Methods/intervention/outcomes: unclear method of allocation/acupuncture versus laser acupuncture/follow‐up < 4 weeks |
| Vickers 2004 | Participants: most (95%) of participants with migraine |
| Vincent 1990 | Methods/outcomes: multiple single case cross‐over trials in which 4 true and 4 sham acupuncture treatments were randomly given in an 8‐week observation period (therefore, no constant follow‐up > 4 weeks) |
| Wang 2003 | RCT of electrical stimulation at acupuncture points (no skin penetration) versus sham intervention in participants with tension‐type headache |
| Xue 2004 | Randomised cross‐over study of electro‐acupuncture versus sham electro‐acupuncture in participants with tension‐type headache. Observation period before cross‐over < 8 weeks (6 weeks) |
RCT: randomised controlled trial
Differences between protocol and review
For this 2016 update we made a number of changes to the protocol/previous versions.
To make it more clear that this review does not address the treatment of acute headaches we changed the title from 'Acupuncture for tension‐type headache' to 'Acupuncture for the prevention of tension‐type headache'.
We defined the selection criteria in more detail: we have added the criterion regarding disease duration to the description of the participants section to better comply with common diagnostic standards.
Changes to the 'Types of interventions' section: 1) we added a minimum number of six acupuncture sessions, given at least once per week, for inclusion to warrant that participants received an adequate minimum dose of treatment; and 2) we limited eligible other active treatments to pharmacological treatment, cognitive and physical treatment to sharpen the focus of the review.
Acceptable outcome measures are now more explicitly defined and we also assessed adverse events in line with current Cochrane policy.
Based on the recommendation of the statistician in our team (AV), we now use fixed‐effect models for calculating pooled estimates. This is primarily because the fixed‐effect analysis constitutes a valid test of the null hypothesis.
We have added judgements of the overall quality of evidence according to the GRADE approach for key outcomes.
Contributions of authors
All review authors participated in the development of the protocol, the selection, extraction or assessment of the primary studies (or both) and review of drafts of the manuscript. All authors approved the final version. Klaus Linde co‐ordinated the review, wrote the draft of the manuscript and is responsible for updating.
Sources of support
Internal sources
No sources of support supplied
External sources
-
NIH grant R01AT006794, USA.
The participation of Andrew Vickers was supported by grant to Dr Vickers.
-
Cancer Center Support Grant P30 CA008748 (PI: Craig B. Thompson), USA.
Institutional support from Cancer Center Support Grant for Andrew Vickers.
Declarations of interest
This review includes trials in which some of the review authors were involved: Jena 2008 ‐ Benno Brinkhaus; Melchart 2005 ‐ Benno Brinkhaus and Klaus Linde; White 1996 and White 2000 ‐ Adrian White. These trials were reviewed by at least two other members of the review team.
Gianni Allais, Benno Brinkhaus, Yutong Fei, Byung‐Cheul Shin, Michael Mehring and Adrian White use acupuncture in their clinical work.
Within the last three years (January 2013 to December 2015): Gianni Allais received fees for teaching acupuncture in private schools; Klaus Linde once received a fee from the German Medical Acupuncture Society for speaking about research at a conference; Benno Brinkhaus has received fees for presenting research findings at meetings of acupuncture societies in various countries; Adrian White is employed by the British Medical Acupuncture Society as a journal editor and has received fees for lecturing on acupuncture on several occasions.
Andrew Vickers' contribution to this review was supported by the NIH grant R01AT006794 (see Sources of support).
We believe that none of the statements above constitute a potential conflict of interest in relation to this review.
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Ahonen 1984 {published data only}
- Ahonen E, Hakumäki M, Mahlamäki S, Partanen J, Riekkinen P, Sivenius J. Acupuncture and physiotherapy in the treatment of myogenic headache patients: pain relief and EMG activity. In: Bonica JJ, Lindblom U, Iggo A editor(s). Advances in Pain research and Therapy. Vol. 5. New York: Raven Press, 1983:571‐6. [Google Scholar]
- Ahonen E, Hakumäki M, Mahlamäki S, Partanen J, Riekkinen P, Sivenius J. Effectiveness of acupuncture and physiotherapy on myogenic headache: a comparative study. Acupuncture and Electro‐Therapeutics Research 1984;9(3):141‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Carlsson 1990 {published data only}
- Carlsson J, Augustinsson LE, Blomstrand C, Sullivan M. Health status in patients with tension headache treated with acupuncture or physiotherapy. Headache 1990;30(9):593‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Carlsson J, Fahlcrantz A, Augustinsson LE. Muscle tenderness in tension headache treated with acupuncture or physiotherapy. Cephalalgia 1990;10(3):131‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Carlsson J, Rosenhall U. Oculomotor disturbances in patients with tension headache treated with acupuncture or physiotherapy. Cephalalgia 1990;10(3):123‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Carlsson J, Wedel A, Carlsson GE, Blomstrand C. Tension headache and signs and symptoms of craniomandibular disorders treated with acupuncture or physiotherapy. Pain Clinic 1990;3:229‐38. [Google Scholar]
Endres 2007 {published and unpublished data}
- Endres HG, Böwing G, Diener HC, Lange S, Maier C, Molsberger A, et al. Acupuncture for tension‐type headache: a multicentre, sham‐controlled, patient‐ and observer‐blinded, randomised trial. Journal of Headache and Pain 2007;8(5):306‐14. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molsberger AF, Boewing G, Diener HC, Endres HG, Kraehmer N, Kronfeld K, et al. Designing an acupuncture study: the nationwide, randomized, controlled German Acupuncture Trials on migraine and tension‐type headache. Journal of Alternative and Complementary Medicine 2006;12(3):237‐45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Jena 2008 {published and unpublished data}
- Jena S, Becker‐Witt C, Brinkhaus B, Selim D, Willich S. Effectiveness of acupuncture treatment for headache ‐ the Acupuncture in Routine Care Study (ARC‐Headache). Focus on Alternative and Complementary Therapies 2004;9 Suppl:17. [Google Scholar]
- Jena S, Witt CM, Brinkhaus B, Wegscheider K, Willich SN. Acupuncture in patients with headache. Cephalalgia 2008;28(9):969‐79. [DOI] [PubMed] [Google Scholar]
- Witt CM, Reinhold T, Jena S, Brinkhaus B, Willich SN. Cost‐effectiveness of acupuncture treatment in patients with headache. Cephalalgia 2008;28(4):334‐45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Karst 2001 {published and unpublished data}
- Fink M, Gutenbrunner C, Rollnik J, Karst M. Credibility of a newly designed placebo needle for clinical trials in acupuncture research. Forschende Komplementärmedizin und Klassische Naturheilkunde 2001;8(6):368‐72. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Karst M, Reinhard M, Thum P, Wiese B, Rollnik J, Fink M. Needle acupuncture in tension‐type headache: a randomized, placebo‐controlled study. Cephalalgia 2001;21(6):637‐42. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Karst M, Rollnik JD, Fink M, Reinhard M, Piepenbrock S. Pressure pain threshold and needle acupuncture in chronic tension‐type headache ‐ a double‐blind placebo‐controlled study. Pain 2000;88(2):199‐203. [DOI] [PubMed] [Google Scholar]
Kwak 2007 {published data only (unpublished sought but not used)}
- Kwak BM, Kim MJ, Kim YM, Lee JM, Park YC, Jo JH. Persisting effects of acupuncture method for chronic tension‐type headache; a randomized controlled trial. Journal of Korean Acupuncture & Moxibustion Society [taehan chimgu hakhoe chi] 2008;25:165‐77. [Google Scholar]
Melchart 2005 {published and unpublished data}
- Melchart D, Linde K, Streng A, Reitmayr S, Hoppe A, Brinkhaus B, et al. Acupuncture Randomized Trials (ART) in patients with migraine or tension‐type headache ‐ design and protocols. Forschende Komplementärmedizin und Klassische Naturheilkunde 2003;10(4):179‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Melchart D, Streng A, Hoppe A, Brinkhaus B, Becker‐Witt C, Hammes M, et al. The Acupuncture Randomised Trial (ART) for tension‐type headache ‐ details of the treatment. Acupuncture in Medicine 2005;23(4):157‐65. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Melchart D, Streng A, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, et al. Acupuncture in patients with tension‐type headache ‐ randomised controlled trial. BMJ 2005;331(7513):376‐82. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Söderberg 2006 {published data only}
- Söderberg E, Carlsson J, Stener‐Victorin E. Chronic tension‐type headache treated with acupuncture, physical training and relaxation training. Between‐group differences. Cephalalgia 2006;26(11):1320‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Söderberg EI, Carlsson JY, Stener‐Victorin E, Dahlöf C. Subjective well‐being in patients with chronic tension‐type headache: effect of acupuncture, physical training, and relaxation training. Clinical Journal of Pain 2011;27:448‐56. [DOI] [PubMed] [Google Scholar]
Tavola 1992 {published data only}
- Tavola T, Gala C, Conte G, Invernizzi G. Traditional Chinese acupuncture in tension‐type headache: a controlled study. Pain 1992;48(3):325‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
White 1996 {published data only}
- White AR, Resch KL, Ernst E, Eddleston C, Hardie R. A pilot study of acupuncture for tension headache, using a novel placebo. Acupuncture in Medicine 1996;14:11‐5. [Google Scholar]
White 2000 {published data only}
- White AR, Resch KL, Chan JC, Norris CD, Modi SK, Patel JN, et al. Acupuncture for episodic tension‐type headache: a multicentre randomized controlled trial. Cephalalgia 2000;20(7):632‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wylie 1997 {published data only}
- Wylie KR, Jackson C, Crawford PM. Does psychological testing help to predict the response to acupuncture or massage/relaxation therapy in patients presenting to a general neurology clinic with headache?. Journal of Traditional Chinese Medicine 1997;17(2):130‐9. [MEDLINE: ] [PubMed] [Google Scholar]
References to studies excluded from this review
Borglum‐Jensen 1979 {published data only}
- Borglum‐Jensen L, Melsen B, Borglum‐Jensen S. Effect of acupuncture on headache measured by reduction in number of attacks and use of drugs. Scandinavian Journal of Dental Research 1979;87(5):373‐80. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Chassot 2015 {published data only}
- Chassot M, Dussan‐Sarria JA, Sehn FC, Deitos A, Souza A, Vercelino R, et al. Electroacupuncture analgesia is associated with increased serum brain‐derived neurotrophic factor in chronic tension‐type headache: a randomized, sham controlled, crossover trial. BMC Complementary and Alternative Medicine 2015;15:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coeytaux 2005 {published data only}
- Coeytaux RR, Kaufman JS, Kaptchuk TJ, Chen W, Miller WC, Callahan LF, et al. A randomized controlled trial of acupuncture for chronic daily headache. Headache 2005;45(9):1113‐23. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ebneshahidi 2005 {published data only}
- Ebneshahidi NS, Heshmatipour M, Moghaddami A, Eghtesadi‐Araghi P. The effect of laser acupuncture on chronic tension headache ‐ a randomised controlled trial. Acupuncture in Medicine 2005;23(1):13‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gottschling 2008 {published data only}
- Gottschling S, Meyer S, Gribova I, Distler L, Berrang J, Gortner L, et al. Laser acupuncture in children with headache: a double‐blind, randomized, bicenter, placebo‐controlled trial. Pain 2008;137(2):405‐12. [DOI] [PubMed] [Google Scholar]
Guerreiro da Silva 2012 {published and unpublished data}
- Guerreiro da Silva JB, Nakamura MU, Cordeiro JA, Kulay L. Acupuncture for tension‐type headache in pregnancy: a prospective, randomized, controlled study. European Journal of Integrative Medicine 2012;4:e366‐e70. [Google Scholar]
- Guerreiro da Silva JB, Nakamura MU, Cordeiro JA, Kulay L. Corrigendum to Acupuncture for tension‐type headache in pregnancy: a prospective, randomized, controlled study [European Journal of Integrative Medicine 4, 4 (2012) e366‐e370]. European Journal of Integrative Medicine 2013;5:189. [Google Scholar]
- Silva JBG, Nakamura MU, Cordeiro JA, Kulay Jr L. Acupuncture for tension‐type headache in pregnancy: a prospective, randomized, controlled study. Journal of Alternative and Complementary Medicine 2013;19(7):A20. [Google Scholar]
Hamp 1999 {published data only}
- Hamp C, Karlsson A, List T. Effect of acupuncture and relaxation training in children and adolescents with tension‐type headache ‐ a pilot study [Effekten av akupunktur och avspääning vid behandling av barn och ungdomar med huvudvärk av spänningstyp ‐ en pilostudie]. Nordisk Fysioterapi 1999;3:13‐9. [Google Scholar]
Hansen 1985 {published data only}
- Hansen PE, Hansen JH. Acupuncture treatment of chronic tension headache ‐ a controlled cross‐over trial. Cephalalgia 1985;5(3):137‐42. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hong 2007 {published data only}
- Hong KE, Park YC, Jo JH, C JI, Kang WC, Lee SB, et al. Effect of Sa‐am acupuncture method for chronic tension‐type headache: a randomized controlled trial. Journal of Korean Acupuncture & Moxibustion Society [taehan chimgu hakhoe chi] 2007;24(1):13‐28. [Google Scholar]
Karakurum 2001 {published data only}
- Karakurum B, Karaalin O, Coskun Ö, Dora B, Ücler S, Inan L. The 'dry needling technique': intramuscular stimulation in tension‐type headache. Cephalalgia 2001;21(8):813‐7. [DOI] [PubMed] [Google Scholar]
Lavies 1998 {published data only}
- Lavies NG. Laser acupuncture for migraine and muscle tension headache: a double‐blind controlled trial. Acupuncture in Medicine 1998;16:73‐6. [Google Scholar]
Loh 1984 {published data only}
- Loh L, Nathan PW, Schott GD, Zilkha KJ. Acupuncture versus medical treatment for migraine and muscle tension headaches. Journal of Neurology, Neurosurgery and Psychiatry 1984;47(4):333‐7. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shi 2000 {published data only}
- Shi J, Flemming M, Stehr‐Zirngibl S, Taeger K. Treating chronic headache by means of acupuncture. A clinical trial [Schmerztherapie mit Akupunktur bei chronischen Kopfschmerzen. Eine klinische Studie]. Chinesische Medizin 2000;15:14‐25. [Google Scholar]
Sozen 2013 {published data only}
- Sozen A, Yilmaz M, Koyuncuoglu HR, Yurekli V, Uzar E, Kutluhan S. Effectiveness of acupuncture for the treatment of chronic daily headache: a sham‐controlled clinical trial. Acta Medica Mediterranea 2013;29:167‐72. [Google Scholar]
Tekeoglu 1995 {published data only}
- Tekeoglu I. Introduction of a new therapy method: music sound electroacupuncture stimulation. Acupuncture in Medicine 1995;13:71‐3. [Google Scholar]
Turk 1990 {published data only}
- Turk Z, Moser I. Curing chronic headache with acupuncture [Heilung des chronischen Kopfschmerzes durch Akupunktur]. Erfahrungsheilkunde 1990;11:724‐6. [Google Scholar]
Vickers 2004 {published data only}
- Vickers A, Rees R, Zollman C, Smith C, Ellis N. Acupuncture for migraine and headache in primary care: a protocol for a pragmatic, randomized trial. Complementary Therapies in Medicine 1999;7(1):3‐18. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al. Acupuncture for chronic headache in primary care: large, pragmatic, randomised trial. BMJ 2004;328(7442):744‐7. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al. Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis. Health Technology Assessment 2004;8(48):1‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Wonderling D, Vickers AJ, Grieve R, McCarney R. Cost effectiveness analysis of a randomised trial of acupuncture for chronic headache in primary care. BMJ 2004;328(7442):747‐51. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vincent 1990 {published data only}
- Vincent CA. The treatment of tension headache by acupuncture: a controlled single case design with time series analysis. Journal of Psychosomatic Research 1990;34(5):553‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wang 2003 {published data only}
- Wang K, Svensson P, Arendt‐Nielsen L. Effect of acupuncture‐like electrical stimulation on chronic tension‐type headache: a randomized, double‐blinded, placebo‐controlled trial. Clinical Journal of Pain 2007;23(4):316‐22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Xue 2004 {published data only}
- Xue CC, Dong L, Polus B, English RA, Zheng Z, Costa C, et al. Electroacupuncture for tension‐type headache on distal acupoints only: a randomized, controlled, crossover trial. Headache 2004;44(4):333‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Additional references
Bodeker 2005
- Bodeker G, Ong CK, Grundy C, Burford G, Shein K. WHO Global Atlas of Traditional, Complementary and Alternative Medicine. Kobe, Japan: WHO Center for Health Development, 2005. [Google Scholar]
Burke 2006
- Burke A, Upchurch DM, Dye C, Chyu L. Acupuncture use in the United States: findings from the National Health Interview Study. Journal of Alternative and Complementary Medicine 2006;12(7):639‐48. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bäcker 2004
- Bäcker M, Gareus IK, Knoblauch NTM, Michalsen A, Dobos G. Acupuncture in the treatment of pain ‐ hypothesis to adaptive effects [Akupunktur in der Schmerztherapie ‐ Hypothese zu adaptiven Prozessen]. Forschende Komplementärmedizin und Klassische Naturheilkunde 2004;11(6):335‐45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Carlsson 2002
- Carlsson C. Acupuncture mechanisms for clinically relevant long‐term effects ‐ reconsideration and a hypothesis. Acupuncture in Medicine 2002;20(2‐3):82‐99. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Corbett 2013
- Corbett MS, Rice SJ, Madurasinghe V, Slack R, Fayter DA, Harden M, et al. Acupuncture and other physical treatments for the relief of pain due to osteoarthritis of the knee: network meta‐analysis. Osteoarthritis Cartilage 2013;9:1290‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dale 1997
- Dale J. Acupuncture practice in the UK. Part I: report of a survey. Complementary Therapies in Medicine 1997;5:215‐20. [Google Scholar]
Davis 2008
- Davis MA, Kononowech RW, Rolin SA, Spierings EL. Acupuncture for tension‐type headache: a meta‐analysis of randomized, controlled trials. Journal of Pain 2008;9(8):667‐77. [DOI] [PubMed] [Google Scholar]
Diener 2004
- Diener HC. Advances in the field of headache 2003/2004. Current Opinion in Neurology 2004;17(3):271‐3. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Endres 2007a
- Endres HG, Diener HC, Molsberger A. Role of acupuncture in the treatment of migraine. Expert Review of Neurotherapeutics 2007;7(9):1121‐34. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ernst 1998
- Ernst E, White A. Acupuncture for back pain. A meta‐analysis of randomized controlled trials. Archives of Internal Medicine 1998;158(20):2235‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- GRADEpro GDT 2015. GRADEpro Guideline Development Tool. McMaster University, 2015 (developed by Evidence Prime, Inc.), 2015.
Hao 2013
- Hao XA, Xue CC, Dong L, Zheng Z. Factors associated with conflicting findings on acupuncture for tension‐type headache: qualitative and quantitative analyses. Journal of Alternative and Complementary Medicine 2013;19:285‐97. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Härtel 2004
- Härtel U, Volger E. Use and acceptance of classical and alternative medicine in Germany ‐ findings of a representative population‐based survey [Inanspruchnahme und Akzeptanz klassischer Naturheilverfahren und alternativer Heilmethoden in Deutschland ‐ Ergebnisse einer repräsentativen Bevölkerungsstudie]. Forschende Komplementärmedizin und Klassische Naturheilkunde 2004;11(6):327‐34. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
IHS 2004
- Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia 2004;24 Suppl 1:1‐160. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
IHS 2013
- Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629‐808. [DOI] [PubMed] [Google Scholar]
IHS Clinical Trials Subcommittee 2009
- Bendtsen L, Bigal ME, Cerbo R, Diener HC, Holroyd K, Lampl C, et al. on behalf of the International Headache Society Clinical Trials Subcommittee. Guidelines for controlled trials of drugs intension‐type headache: Second edition. Cephalagia 2009;30:1‐16. [DOI] [PubMed] [Google Scholar]
Kaptchuk 2002
- Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Annals of Internal Medicine 2002;136(5):374‐83. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kaptchuk 2006
- Kaptchuk TJ, Stason WB, Davis RB, Legezda ATR, Schnyer RN, Kerr CE, et al. Sham device v inert pill: randomised controlled trial of two placebo treatments. BMJ 2006;332(7538):391‐7. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaptchuk 2008
- Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE, et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 2008;336(7651):999‐1003. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kong 2009
- Kong J, Kaptchuk TJ, Webb JM, Kong JT, Sasaki Y, Polich GR, et al. Functional neuroanatomical investigation of vision‐related acupuncture point specificity‐‐a multisession fMRI study. Human Brain Mapping 2009;30:38‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lam 2013
- Lam M, Galvin R, Curry P. Effectiveness of acupuncture for nonspecific chronic low back pain: a systematic review and meta‐analysis. Spine 2013;38:2124‐38. [DOI] [PubMed] [Google Scholar]
Linde 2010a
- Linde K, Niemann K, Meissner K. Are sham acupuncture interventions more effective than (other) placebos? A re‐analysis of data from the Cochrane review on placebo effects. Forschende Komplementarmedizin 2010;17:259‐64. [DOI] [PubMed] [Google Scholar]
Linde 2010b
- Linde K, Niemann K, Schneider A, Meissner K. How large are the nonspecific effects of acupuncture? A meta‐analysis of randomized controlled trials. BMC Medicine 2010;8:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Linde 2016
- Linde K, Allais G, Brinkhaus B, Manheimer W, Vickers A, White A. Acupuncture for the prophylaxis of episodic migraine. Cochrane Database of Systematic Reviews 2016, Issue [in press]. [Google Scholar]
Manheimer 2010
- Manheimer E, Cheng K, Linde K, Lao L, Yoo J, Wieland S, et al. Acupuncture for peripheral joint osteoarthritis. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD001977.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
McCrory 2000
- McCrory DC, Penzien DB, Gray RN, Hasselblad V. Behavioral and physical treatments for tension‐type and cervicogenic headache. October 2000. Prepared for the Foundation for Chiropractic Education and Research, Grant No. 99‐05‐01. Available in 2001 from: www.fcer.org. Executive Summary still available (2 July 2008) at www.fcer.org/html/Research/DukeEvidenceReport.htm 2000.
McGeeney 2015
- McGeeney BE. Acupuncture is all placebo and here is why. Headache 2015;55:465‐9. [DOI] [PubMed] [Google Scholar]
Meissner 2013
- Meissner K, Fässler M, Rücker G, Kleijnen J, Hróbjartsson A, Schneider A, et al. Differential effectiveness of placebo treatments: a systematic review of migraine prophylaxis. JAMA Internal Medicine 2013;173:1941‐51. [DOI] [PubMed] [Google Scholar]
Pfaffenrath 1998
- Pfaffenrath V, Brune K, Diener HC, Gerber WD, Göbel H. Treatment of tension‐type headache. Recommendations of the German Migraine and Headache Society [Behandlung des Kopfschmerzes vom Spannungstyp. Therapieempfehlungen der Deutschen Migräne‐ und Kopfschmerzgesellschaft]. Schmerz 1998;12(2):156‐70. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre; The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre; The Cochrane Collaboration, 2014.
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Stovner 2007
- Stovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton RB, Scher A, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 2007;27(3):193‐210. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Vickers 1998
- Vickers A, Goyal N, Harland R, Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Controlled Clinical Trials 1998;19(2):159‐66. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Vickers 2010
- Vickers AJ, Cronin AM, Maschino AC, Lewith G, Macpherson H, Victor N, et al. Acupuncture Trialists' Collaboration. Individual patient data meta‐analysis of acupuncture for chronic pain: protocol of the Acupuncture Trialists' Collaboration. Trials 2010;11:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vickers 2012
- Vickers AJ, Cronin AM, Maschino AC, Lewith G, MacPherson H, Foster NE, et al. Acupuncture Trialists' Collaboration. Acupuncture for chronic pain: individual patient data meta‐analysis. Archives of Internal Medicine 2012;172:1444‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2007
- Wang G, Mao B, Xiong ZY, Fan T, Chen XD, Wang L, et al. CONSORT Group for Traditional Chinese Medicine. The quality of reporting of randomized controlled trials of traditional Chinese medicine: a survey of 13 randomly selected journals from mainland China. Clinical Therapeutics 2007;29(7):1456‐67. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Weidenhammer 2007
- Weidenhammer W, Streng A, Linde K, Hoppe A, Melchart D. Acupuncture for chronic pain within the research program of 10 German Health Insurance Funds ‐ basic results from an observational study. Complementary Therapies in Medicine 2007;15(4):238‐46. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Yang 2012
- Yang J, Zeng F, Feng Y, Fang L, Qin W, Liu X, et al. A PET‐CT study on the specificity of acupoints through acupuncture treatment in migraine patients. BMC Complementary and Alternative Medicine 2012;12:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Linde 2009
- Linde K, Allais G, Brinkhaus B, Manheimer W, Vickers A, White A. Acupuncture for tension‐type headache. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD007578] [DOI] [PMC free article] [PubMed] [Google Scholar]


