Abstract
Introduction
Allosensitization has been shown to negatively impact post-heart transplant (HTx) survival even with a negative crossmatch. Whether MCS-related allosensitization is associated with worse post-HTx survival remains controversial.
Materials and Methods
Adult HTx recipients listed in the United Network for Organ Sharing database (7/06–12/12) were identified. Multivariate Cox regression assessed the effect of allosensitization on survival. Propensity matching was performed to compare allosensitized and non-sensitized patients. Kaplan-Meier survival analysis compared matched and unmatched patients in both the MCS and medically managed cohorts.
Results
We identified 11,840 HTx recipients, of whom 4,167 had MCS. MCS was associated with allosensitization in multivariate logistic regression. Each different MCS devices was associated with worse post-HTx survival in multivariate Cox regression. Allosensitization did not predict post-HTx mortality in MCS patients, HR: 1.07 (0.89–1.28), P=0.48. Among patients without MCS, allosensitization was associated with post-HTx mortality, HR: 1.19 (1.03–1.39), P=0.02. Kaplan-Meier analysis revealed equivalent survival in unmatched and matched cohorts when comparing MCS patients who were allosensitized and non-sensitized MCS patients. Among non-MCS patients, allosensitization was associated with worse survival in both unmatched and matched analysis.
Conclusions
MCS was associated with allosensitization. For MCS patients, allosensitization did not independently predict worse post-HTx outcome. Among non-MCS patients, allosensitization was associated with worse post-HTx survival. Allosensitization appears to be a heterogeneous process influenced by presence of MCS.
Keywords: Heart Transplantation, Ventricular Assist Devices, Panel Reactive Antibody, Mechanical Circulatory Support
Background
Circulating anti-human leukocyte antigen (anti-HLA) antibodies in transplant recipients are able to react to donor antigens after heart transplantation (HTx). By mixing recipient serum with lymphocytes of known HLA type, the panel reactive antibody (PRA) screen indirectly determines the proportion of potential donor antigens in the greater population to which the patient’s pre-formed antibodies may react. PRA >10% signifies allosensitization; increasing degree of allosensitization has been associated with worse long-term survival and a higher incidence of rejection.1 Reduction of PRA prior to transplantation has been linked with improved post-transplant survival.2
The introduction of left ventricular assist devices (LVADs) has greatly altered the management of patients awaiting heart transplantation; utilization of mechanical circulatory support (MCS) as a bridge to transplantation has increased from less than 25% in 2006 to 37% in 2011.3 Enthusiasm for MCS has been buoyed by evidence for improved survival compared with medically managed patients.4–6 However, LVAD implantation has been associated with allosensitization.7–9 The effect of MCS-related allosensitization on survival after HTx has not been delineated. We reviewed the United Network for Organ Sharing (UNOS) database to assess the effect of allosensitization with or without MCS implantation on post-transplantation survival.
Methods
Study Population and Primary Endpoint
This was a retrospective review of de-identified data supplied by the United Network for Organ Sharing (UNOS) as the contractor for the Organ Procurement and Transplantation Network. This study was granted an exemption by the Institutional Review Board at our institution because no patient identifiers were included. The study’s primary endpoint was post-transplant survival. Patients were censored at the time of last known follow-up. Analyses were conducted with Stata software (version 13, StataCorp LP, College Station, Texas).
Statistical Analysis
Patients were stratified by the presence of MCS – continuous flow LVAD, pulsatile flow LVAD, biventricular assist device (BiVAD), total artificial heart (TAH), or right ventricular assist device (RVAD) – at the time of transplant due to the large difference noted in PRA levels in patients with and without MCS. The standardized differences approach compared covariates between allosensitized and non-sensitized patients to facilitate comparison with subsequent weighted analyses.10 Means are presented with standard deviations; hazard ratios (HRs) are presented with 95% confidence intervals (CI). All testing was 2-sided; p-values ≤0.05 were considered significant. Because of the exploratory nature of this study, no adjustments were made for multiple comparisons.11 Post-transplant survival distributions were estimated with the nonparametric Kaplan-Meier method.12 The log-rank test was used to compare differences between survival distributions in unadjusted analyses.13 Survival curves were re-generated in a sub-population of matched patients following propensity-score matching, and the stratified log-rank test was used to compare survival curves in matched cohorts.14–15
Center volume was included as a covariate in our analyses. During the 77-month study period, centers performing >200 heart transplants were considered high volume (≥30 transplants/y), and centers performing between 100 and 200 transplants were considered moderate volume (15–29 transplants/y). Cut points were chosen by using a restricted cubic spline analysis.
Missing Data
Multiple imputation was employed for variables with missing values to avoid list-wise deletion in our multivariable analyses.16 This was performed in all non-redundant variables by using a regression switching approach with predictive mean matching for continuous and semi-continuous variables, logistic regression for binary variables, and ordered logistic regression for ordinal variables; the model included the event indicator and the Nelson–Aalen estimator of the hazard of death.17, 18 Twenty imputations were performed given our reasonable sample size and moderate amount of missing data.19 The complete sets of observed values were used as covariates for prediction purposes.
Propensity Score Matching
Differences in characteristics between allosensitized and non-sensitized patients were controlled for with propensity-score matching.14 Multivariable logistic regression models that included all available variables at the time of transplant were employed to develop a propensity score for patients in each of our two propensity-matched comparisons; one in patients without MCS (non-MCS) and the other in patients with MCS.20 To handle missing data, propensity scores were calculated across all imputed datasets (n=20) using the "Across" approach described by Mitra and combined according to Rubin's rules.21, 22 We next carried out a 1:1 nearest-neighbor matching algorithm without replacement (using a caliper of 0.01 of the standard deviation of the linear propensity score); balance was achieved in our model by using the standardized differences approach.10, 15
Cox Proportional Hazards Analysis
A sensitivity analysis was undertaken to corroborate the findings from our propensity score analysis. Cox proportional hazards regression modeling assessed the association of demographic, clinical, transplant center, operative, and donor characteristics with survival after HTx in both the non-MCS and MCS cohorts.23 The proportional hazards assumption was tested by plotting scaled Schoenfeld residuals.24 Purposeful selection of covariates was used to create the models; variables hypothesized or previously shown to be of clinical significance in HTx recipients were included along with novel variables that were plausibly significant (P≤0.20) on bivariable analysis.25 Variables that were not statistically significant (P>0.05) by the Wald test in our multivariable models but that were plausibly associated with graft survival were included in our final models; covariate selection was also guided by optimizing the Akaike information criterion (AIC).26
Panel Reactive Antibody
In the UNOS dataset, Class I and Class II PRA are reported each with “most recent” and “peak” values available. A composite PRA level was created using the highest “most recent” PRA value of either Class I or Class II PRA levels. PRA >10% was considered to be allosensitized.27
Results
There were 11,840 heart transplant recipients identified, of whom 4,167 patients had some form of durable MCS device at the time of transplant, in the study period (7/06–12/12). Data was missing for <1% of patients for the majority of all variables analyzed; four variables had missing data for 1–4% of patients (cardiac index, mean pulmonary artery pressure, organ ischemic time, and donor/recipient CMV match), two variables had missing data for 5–9% of patients (pulmonary capillary wedge pressure, and composite PRA level), and two variables had missing data for ≥10% of patients (college education and HLA mismatch). Multiple imputation was used to account for missing data. In our unmatched and matched Kaplan-Meier survival analyses, patients without composite PRA level data (5.7% of patients) were excluded. However, these patients were included with an imputed PRA level in our Cox proportional hazards regression analysis.
Demographic data for unmatched and propensity matched patients is listed in table 1. There were statistically significant differences in baseline characteristics between allosensitized and non-sensitized patients both with and without MCS; the propensity matching algorithm was able to account for these differences.
Table 1.
Baseline characteristics of patients with and without mechanical circulatory support, before and after propensity score matching
| Patients Without Mechanical Circulatory Support at Transplant | Patients With Mechanical Circulatory Support at Transplant | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unmatched Comparison | Matched Comparison | Unmatched Comparison | Matched Comparison | |||||||||
| PRA ≥10% (n=1226) |
PRA <10% (n=6006) |
Stand Diff |
PRA ≥10% (n=1144) |
PRA <10% (n=1144) |
Stand Diff |
PRA ≥10% (n=976) |
PRA <10% (n=2956) |
Stand Diff |
PRA ≥10% (n=973) |
PRA <10% (n=973) |
Stand Diff |
|
| Baseline characteristics | ||||||||||||
| Age, y | 50.4 | 53.2 | 0.209 | 51.0 | 50.9 | 0.005 | 50.6 | 52.2 | 0.129 | 50.6 | 50.6 | 0.002 |
| Male gender | 50% | 76% | 0.573 | 53% | 51% | 0.023 | 66% | 86% | 0.485 | 66% | 66% | 0.013 |
| Caucasian race | 64% | 70% | 0.144 | 64% | 65% | 0.007 | 63% | 70% | 0.144 | 63% | 62% | 0.028 |
| African-American race | 23% | 17% | 0.155 | 23% | 22% | 0.003 | 27% | 19% | 0.171 | 27% | 25% | 0.031 |
| Hispanic ethnicity | 9.2% | 8.4% | 0.029 | 9.0% | 8.7% | 0.012 | 5.7% | 7.3% | 0.065 | 5.8% | 8.6% | 0.111 |
| College education | 54% | 56% | 0.036 | 53% | 53% | 0.004 | 54% | 51% | 0.045 | 54% | 53% | 0.017 |
| Private insurance | 53% | 54% | 0.027 | 53% | 53% | 0.007 | 50% | 51% | 0.018 | 51% | 50% | 0.004 |
| BMI, kg/m2 | 26.0 | 26.6 | 0.116 | 26.1 | 26.0 | 0.020 | 27.4 | 27.7 | 0.047 | 27.4 | 27.4 | 0.012 |
| BMI ≥ 35 kg/m2 | 3.3% | 4.0% | 0.038 | 3.3% | 2.6% | 0.015 | 7.8% | 7.8% | 0.002 | 7.7% | 6.4% | 0.52 |
| Etiology of heart failure | ||||||||||||
| Ischemic cardiomyopathy/CAD | 28% | 40% | 0.240 | 30% | 29% | 0.015 | 36% | 43% | 0.137 | 36% | 35% | 0.026 |
| Idiopathic cardiomyopathy | 29% | 33% | 0.071 | 31% | 32% | 0.026 | 40% | 50% | 0.006 | 40% | 41% | 0.027 |
| Graft dysfunction (retransplantation) | 12% | 3.3% | 0.317 | 8.7% | 6.9% | 0.068 | 1.6% | 0.8% | 0.075 | 1.3% | 1.7% | 0.033 |
| Congenital heart disease | 6.4% | 3.4% | 0.138 | 5.9% | 6.3% | 0.018 | 1.1% | 0.4% | 0.088 | 1.1% | 0.6% | 0.055 |
| Restrictive cardiomyopathy | 3.5% | 3.3% | 0.009 | 3.6% | 4.2% | 0.032 | 1.2% | 0.7% | 0.049 | 1.2% | 0.8% | 0.041 |
| Hypertrophic cardiomyopathy | 3.3% | 3.0% | 0.017 | 3.6% | 4.7% | 0.057 | 1.7% | 0.9% | 0.069 | 1.7% | 1.3% | 0.033 |
| Functional status, life support | ||||||||||||
| Status 1a | 43% | 40% | 0.063 | 43% | 41% | 0.028 | 71% | 75% | 0.077 | 71% | 73% | 0.034 |
| Status 1a or 1b | 89% | 86% | 0.105 | 89% | 89% | 0.014 | 100% | 100% | 0.000 | 100% | 100% | 0.000 |
| NYHA class IV | 51% | 48% | 0.059 | 51% | 51% | 0.005 | 46% | 38% | 0.162 | 46% | 44% | 0.029 |
| NYHA class III–IV | 82% | 83% | 0.014 | 82% | 82% | 0.001 | 78% | 76% | 0.049 | 78% | 79% | 0.017 |
| Inotrope support | 57% | 55% | 0.039 | 58% | 55% | 0.056 | 13% | 14% | 0.042 | 12% | 14% | 0.051 |
| IABP support | 7.3% | 6.7% | 0.021 | 7.1% | 5.7% | 0.057 | 2.2% | 3.0% | 0.052 | 2.2% | 4.1% | 0.112 |
| Ventilator support | 2.7% | 2.2% | 0.030 | 2.4% | 2.1% | 0.018 | 2.5% | 2.7% | 0.018 | 2.5% | 2.7% | 0.013 |
| ECMO support | 1.1% | 0.8% | 0.022 | 0.9% | 1.1% | 0.026 | 1.5% | 0.7% | 0.082 | 1.5% | 0.9% | 0.056 |
| MCSsupport (any) | 0% | 0% | 0.000 | 0% | 0% | 0.000 | 100% | 100% | 0.000 | 100% | 100% | 0.000 |
| MCS support, continuous flow LVAD |
0% | 0% | 0.000 | 0% | 0% | 0.000 | 64% | 64% | 0.001 | 65% | 67% | 0.041 |
| MCS support, pulsatile flow LVAD | 0% | 0% | 0.000 | 0% | 0% | 0.000 | 18% | 22% | 0.097 | 18% | 16% | 0.035 |
| MCS support, BIVAD | 0% | 0% | 0.000 | 0% | 0% | 0.000 | 13% | 11% | 0.057 | 13% | 12% | 0.016 |
| MCS support, TAH | 0% | 0% | 0.000 | 0% | 0% | 0.000 | 4.8% | 2.5% | 0.123 | 4.6% | 4.5% | 0.005 |
| MCS support, RVAD | 0% | 0% | 0.000 | 0% | 0% | 0.000 | 0.4% | 0.8% | 0.050 | 0.4% | 0.4% | 0.000 |
| Hemodynamic parameters | ||||||||||||
| Cardiac index, L/min/m2 | 2.29 | 2.26 | 0.046 | 2.28 | 2.27 | 0.009 | 2.38 | 2.34 | 0.058 | 2.38 | 2.37 | 0.021 |
| Mean pulmonary artery pressure, mmHg |
28.8 | 29.2 | 0.041 | 29.0 | 28.8 | 0.023 | 27.8 | 27.9 | 0.007 | 27.8 | 28.0 | 0.020 |
| Pulmonary capillary wedge pressure, mmHg |
19.7 | 19.7 | 0.009 | 19.8 | 19.4 | 0.042 | 18.2 | 18.5 | 0.029 | 18.2 | 18.5 | 0.039 |
| Renal/liver function, diabetes | ||||||||||||
| CrCl, mL/min | 77.4 | 80.9 | 0.107 | 77.5 | 78.1 | 0.017 | 90.2 | 92.5 | 0.060 | 90.3 | 89.7 | 0.015 |
| Dialysis | 1.9% | 1.7% | 0.016 | 1.8% | 1.7% | 0.007 | 5.2% | 4.0% | 0.059 | 5.0% | 4.0% | 0.50 |
| CrCl<50 mL/min or dialysis | 21% | 17% | 0.105 | 20% | 20% | 0.002 | 15% | 13% | 0.064 | 15% | 14% | 0.024 |
| Diabetes | 21% | 26% | 0.115 | 22% | 22% | 0.007 | 28% | 30% | 0.062 | 28% | 29% | 0.026 |
| Total bilirubin | 1.11 | 1.21 | 0.068 | 1.13 | 1.21 | 0.063 | 1.16 | 1.21 | 0.018 | 1.16 | 1.06 | 0.052 |
| Panel-reactive antibody data | ||||||||||||
| Composite most recent panel-reactive antibody, % |
42.5 | 0.6 | 2.147 | 41.6 | 0.7 | 2.107 | 44.1 | 0.8 | 2.217 | 44.0 | 0.9 | 2.207 |
| Transplant center characteristics | ||||||||||||
| Year of transplant | 2010 | 2009 | 0.184 | 2009 | 2009 | 0.023 | 2010 | 2010 | 0.073 | 2010 | 2010 | 0.069 |
| High-volume listing institution | 38% | 36% | 0.050 | 37% | 35% | 0.051 | 28% | 23% | 0.100 | 27% | 25% | 0.063 |
| Moderate- or high-volume listing institution |
72% | 71% | 0.026 | 72% | 73% | 0.018 | 68% | 64% | 0.73 | 68% | 67% | 0.022 |
| Operative characteristics | ||||||||||||
| Previous cardiac surgery | 39.4% | 36.9% | 0.051 | 39.8% | 36.0% | 0.078 | 100% | 100% | 0.000 | 100% | 100% | 0.000 |
| Bicaval anastomosis | 76% | 71% | 0.115 | 75% | 75% | 0.016 | 75% | 70% | 0.105 | 75% | 75% | 0.012 |
| Organ ischemic time, h | 3.23 | 3.22 | 0.123 | 3.22 | 3.25 | 0.031 | 3.33 | 3.33 | 0.000 | 3.33 | 3.31 | 0.015 |
| Distance organ transported, mi | 194 | 197 | 0.016 | 195 | 194 | 0.005 | 164 | 178 | 0.069 | 165 | 169 | 0.022 |
| Local organ (non-regional, non- national) |
58% | 55% | 0.058 | 57 | 56 | 0.012 | 63% | 57% | 0.113 | 62% | 62% | 0.017 |
| Donor characteristics | ||||||||||||
| Age, y | 32.0 | 31.8 | 0.014 | 31.9 | 32.0 | 0.006 | 31.5 | 30.9 | 0.051 | 31.5 | 31.4 | 0.003 |
| Smoking history >20 y | 15% | 16% | 0.034 | 15% | 14% | 0.029 | 15% | 15% | 0.004 | 15% | 15% | 0.006 |
| Diabetes | 3.2% | 3.4% | 0.013 | 3.2% | 2.8% | 0.026 | 2.9% | 2.9% | 0.001 | 2.9% | 3.2% | 0.017 |
| Donor/recipient matching | ||||||||||||
| Gender match, n (%) | 66% | 73% | 0.153 | 67% | 66% | 0.026 | 72% | 79% | 0.163 | 72% | 74% | 0.032 |
| Race match, n (%) | 48% | 53% | 0.101 | 49% | 49% | 0.017 | 49% | 53% | 0.076 | 49% | 47% | 0.037 |
| CMV - donor positive, recipient negative |
20% | 23% | 0.082 | 20% | 20% | 0.014 | 22% | 24% | 0.056 | 22% | 21% | 0.017 |
| Non-identical ABO blood group match (only compatible) |
18% | 17% | 0.030 | 18% | 17% | 0.021 | 14% | 13% | 0.017 | 14% | 14% | 0.012 |
| Complete HLA mismatch (all 6 alleles) |
19% | 24% | 0.129 | 20% | 23% | 0.077 | 21% | 24% | 0.060 | 22% | 20% | 0.035 |
Abbreviations: PRA, panel reactive antibody; Stand Diff, standardized difference; BMI, body mass index; CAD, coronary artery disease; NYHA, New York Heart Association; IABP, intra-aortic balloon pump; ECMO, extracorporeal membrane oxygenation; MCS, Mechanical Circulatory Support; LVAD, left ventricular assist device; BIVAD, biventricular assist device; TAH, total artificial heart; RVAD, right ventricular assist device; CrCl, creatinine clearance; CMV, cytomegalovirus; HLA, human leukocyte antigen.
Non-MCS patients were separated into patients with a previous history of cardiac surgery and patients without; patients with a history of cardiac surgery had a higher composite most recent PRA that was statistically significant. Composite most recent PRA was greater with each device – except isolated RVAD – than non-MCS patients without a history of cardiac surgery, table 2. Multivariate logistic regression demonstrated that elevated composite most recent PRA ≥10% was associated with MCS, OR 2.01 (1.79 – 2.27), p <0.001, table 3. Other factors associated with MCS were male gender, BMI ≥35, idiopathic cardiomyopathy, NYHA IV symptoms, ventilator dependence, ECMO support, diabetes, later year of transplantation, donor-to-recipient gender match, and organ ischemic time ≥ 4 hours. Negative predictors of MCS were age ≥60 years old, Hispanic ethnicity, college education, diagnoses other than idiopathic cardiomyopathy with ischemic cardiomyopathy as the reference, inotropic support, IABP support, elevated MPAP, donor ≥50 years old, donor diabetes, and non-identical but compatible ABO type.
Table 2.
Panel reactive antibody data, stratified by mechanical circulatory support class. Mean± standard deviation is reported along with median (interquartile range).
| e | Non- missing Data |
No-MCS without history of cardiac surgery (n = 4533) |
No-MCS with history of previous cardiac surgery (n = 2699) |
P | All MCS (n = 3932) |
p | CF LVAD (n = 2532) |
p | PF LVAD (n = 811) |
p | BiVAD (n = 441) |
p | TAH (n = 121) |
p | RVAD (n = 27) |
P |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Most recent panel- reactive antibody, class I |
11108 (93.8) |
5.0±15.3 0 (0–0) |
6.0±17.2 0 (0–1) |
0.007 |
9.2±21.1 0 (0–5) |
<0.001 |
8.8±20.4 0 (0–4) |
<0.001 |
9.0±21.1 0 (0–4) |
<0.001 |
10.4±22.1 0 (0–8) |
<0.001 |
17.6±29.1 2 (0–21.5) |
<0.001 | 4.6±12.6 0 (0–2) |
0.90 |
| Most recent panel- reactive antibody, class II |
10485 (88.6) |
4.4±15.2 0 (0–0) |
4.8±16.1 0 (0–0) |
0.28 |
5.4±16.6 0 (0–0) |
0.01 | 5.2±16.2 0 (0–0) |
0.04 | 4.2±14.7 0 (0–0) |
0.73 |
6.2±18.5 0 (0–0) |
0.02 |
13.0±25.2 0 (0–15.5) |
<0.001 | 3.4±10.5 0 (0–1) |
0.75 |
| Peak panel- reactive antibody, class I |
2720 (23.0) |
24.2±26.4 14 (5–34) |
29.9±29.6 19 (6–47) |
<0.00 1 |
34.4±31.1 24 (9–56) |
<0.001 |
33.3±30.6 23 (8–52) |
<0.001 |
38.3±32.7 28 (10–64) |
<0.001 |
34.6±30.9 24 (9–59) |
<0.001 |
39.3±32.3 30 (14–65) |
<0.001 | 10.0±12.4 6 (1–21) |
0.15 |
| Peak panel- reactive antibody, class II |
1542 (13.0) |
30.8±30.9 18.5 (3– 57) |
33.5±31.5 23 (6–60) |
0.21 | 34.1±31.1 25 (7–58) |
0.17 | 32.8±30.4 23 (7–56) |
0.32 | 37.3±32.8 30 (4–62) |
0.05 | 36.6±32.1 24 (10–58) |
0.14 | 43.1±35.6 27 (16–78) |
0.06 | 17.4±24.0 6 (4–17) |
0.33 |
| Composite most recent panel- reactive antibody, % |
11164 (94.3) |
7.38±18.8 0 (0–2) |
8.32±20.4 0 (0–3) |
0.046 |
9.1±20.9 0 (0–9) |
<0.001 |
11.2±22.6 0 (0–9) |
<0.001 |
10.4±22.7 0 (0–6) |
<0.001 |
13.0±25.1 0 (0–11) |
<0.001 |
21.4±31.3 4 (0–33) |
<0.001 | 5.7±12.7 0 (0–4) |
0.64 |
Abbreviations: MCS, mechanical circulatory support; LVAD, left ventricular assist device; BiVAD, biventricular assist device; TAH, total artificial heart; RVAD, right ventricular assist device.
P-value compares PRA levels against the baseline: patients without MCS and without prior cardiac surgery
Table 3.
Odds ratio of variables associated with patients with a durable mechanical circulatory support device at transplantation
| Demographics | P | |
| Age ≥60 y | 0.72 (0.65–0.80) | <0.001 |
| Male gender | 2.01 (1.79–2.26) | <0.001 |
| Race/Ethnicity | ||
| Caucasian | Reference | |
| African American | 1.10 (0.96–1.25) | 0.16 |
| Hispanic | 0.82 (0.69–0.98) | 0.03 |
| Other | 0.93 (0.73–1.19) | 0.57 |
| College education | 0.89 (0.81–0.99) | 0.03 |
| Private insurance | 1.00 (0.91–1.10) | 0.98 |
| BMI ≥35 kg/m2 | 1.83 (1.50–2.21) | <0.001 |
| Etiology of heart failure | ||
| Ischemic cardiomyopathy/CAD | Reference | |
| Idiopathic cardiomyopathy | 1.23 (1.10–1.37) | <0.001 |
| Graft dysfunction (retransplantation) | 0.15 (0.10–0.20) | <0.001 |
| Congenital heart disease | 0.24 (0.17–0.35) | <0.001 |
| Restrictive cardiomyopathy | 0.10 (0.06–0.15) | <0.001 |
| Hypertrophic cardiomyopathy | 0.34 (0.24–0.48) | <0.001 |
| Functional status, life support | ||
| NYHA class IV | 1.32 (1.19–1.45) | <0.001 |
| Inotrope support | 0.11 (0.10–0.12) | <0.001 |
| IABP support | 0.40 (0.31–0.51) | <0.001 |
| Ventilator support | 3.92 (2.90–5.31) | <0.001 |
| ECMO support | 1.66 (1.01–2.74) | 0.04 |
| Hemodynamic parameters | ||
| Mean pulmonary artery pressure ≥30 mmHg | 0.89 (0.81–0.98) | 0.02 |
| Renal/liver function, diabetes | ||
| CrCl< 50 mL/min or dialysis | 0.98 (0.86–1.12) | 0.77 |
| Diabetes | 1.12 (1.01–1.24) | 0.03 |
| Bilirubin ≥ 2mg/dL | 0.90 (0.78–1.03) | 0.13 |
| Panel-reactive antibody data | ||
| Composite most recent panel-reactive antibody ≥10% | 2.01 (1.79–2.27) | <0.001 |
| Transplant center characteristics | ||
| Year of transplant | 1.21 (1.18–1.24) | <0.001 |
| Moderate- or high-volume listing institution | 1.03 (0.94–1.13) | 0.56 |
| Operative characteristics | ||
| Bicaval anastomosis | 0.94 (0.85–1.04) | 0.22 |
| Organ ischemic time, ≥4h | 1.26 (1.13–1.40) | <0.001 |
| Donor characteristics | ||
| Age ≥50 y | 0.57 (0.47–0.68) | <0.001 |
| Smoking history >20 y | 1.09 (0.96–1.23) | 0.19 |
| Diabetes | 0.75 (0.58–0.98) | 0.03 |
| Donor/recipient matching | ||
| Gender match, n (%) | 1.15 (1.03–1.28) | 0.01 |
| Race match, n (%) | 1.01 (0.92–1.12) | 0.78 |
| CMV - donor positive, recipient negative | 0.99 (0.88–1.10) | 0.79 |
| Non-identical ABO blood group match (only compatible) | 0.81 (0.71–0.91) | 0.001 |
| Complete HLA mismatch (all 6 alleles) | 1.00 (0.89–1.12) | 0.98 |
Abbreviations: BMI, body mass index; CAD, coronary artery disease; NYHA, New York Heart Association; IABP, intra-aortic balloon pump; ECMO, extracorporeal membrane oxygenation; CrCl, creatinine clearance; CMV, cytomegalovirus; HLA, human leukocyte antigen.
Multivariate Cox regression of variables associated with survival in the entire cohort, the subset of patients without support, and the subset of patients with MCS revealed several variables with heterogeneous effects on survival. Whereas composite most-recent PRA ≥10% was not associated with increased hazard for the entire cohort, HR: 1.12 (CI: 0.99–1.26), P=0.06, allosensitization was associated with worse post-HTx survival in the subset of patients without MCS, HR: 1.18 (CI: 1.02–1.37), p=0.03. For patients with MCS, allosensitization did not predict post-transplant mortality, HR: 1.07 (CI: 0.89–1.28), p = 0.48, Table 4.
Table 4.
Multivariable Cox regression of predictors of post-transplant mortality
| Entire Cohort (n=11,840) |
p | Non-MCS Cohort (n=7673) |
P | MCS (n=4167) |
p | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age ≥60 y | 1.25 (1.13–1.39) | <0.001 | 1.08 (0.95–1.23) | 0.24 | 1.62 (1.37–1.92) | <0.001 |
| Male gender | 0.96 (0.86–1.08) | 0.50 | 0.92 (0.81–1.06) | 0.24 | 1.08 (0.88–1.34) | 0.46 |
| Race/ethnicity | ||||||
| Caucasian | Reference | Reference | Reference | |||
| African American | 1.39 (1.23–1.57) | <0.001 | 1.41 (1.21–1.65) | <0.001 | 1.38 (1.12–1.69) | 0.002 |
| Hispanic | 0.98 (0.82–1.17) | 0.85 | 1.07 (0.87–1.33) | 0.51 | 0.78 (0.56–1.08) | 0.13 |
| Other | 1.05 (0.81–1.35) | 0.72 | 1.18 (0.88–1.59) | 0.27 | 0.80 (0.50–1.29) | 0.36 |
| College education | 0.84 (0.76–0.93) | <0.001 | 0.89 (0.79–1.01) | 0.06 | 0.75 (0.64–0.89) | 0.001 |
| Private insurance | 0.85 (0.78–0.93) | 0.001 | 0.86 (0.76–0.96) | 0.008 | 0.85 (0.73–0.99) | 0.04 |
| BMI ≥35 kg/m2 | 1.27 (1.06–1.53) | 0.01 | 1.34 (1.04–1.73) | 0.03 | 1.25 (0.95–1.63) | 0.11 |
| Etiology of heart failure | ||||||
| Ischemic cardiomyopathy/CAD | Reference | Reference | Reference | |||
| Idiopathic cardiomyopathy | 0.78 (0.70–0.87) | <0.001 | 0.78 (0.67–0.91) | 0.002 | 0.87 (0.73–1.04) | 0.12 |
| Graft dysfunction (retransplantation) | 1.46 (1.18–1.80) | <0.001 | 1.44 (1.13–1.83) | 0.003 | 1.40 (0.81–2.42) | 0.22 |
| Congenital heart disease | 1.33 (1.03–1.72) | 0.03 | 1.32 (0.99–1.75) | 0.06 | 1.74 (0.91–3.31) | 0.09 |
| Restrictive cardiomyopathy | 1.54 (1.18–2.00) | 0.001 | 1.48 (1.13–1.96) | 0.005 | 0.65 (0.20–2.11) | 0.47 |
| Hypertrophic cardiomyopathy | 0.69 (0.48–1.00) | 0.05 | 0.64 (0.42–0.97) | 0.04 | 0.98 (0.46–2.09) | 0.96 |
| Functional status, life support | ||||||
| NYHA class IV | 1.37 (1.24–1.51) | <0.001 | 1.33 (1.18–1.50) | <0.001 | 1.47 (1.26–1.73) | <0.001 |
| Inotrope support | 0.98 (0.89–1.09) | 0.76 | 0.97 (0.86–1.09) | 0.63 | 1.04 (0.84–1.28) | 0.74 |
| IABP support | 0.94 (0.78–1.14) | 0.52 | 0.90 (0.72–1.13) | 0.37 | 1.08 (0.74–1.58) | 0.69 |
| Ventilator support | 1.56 (1.24–1.96) | <0.001 | 1.53 (1.12–2.09) | 0.008 | 1.61 (1.13–2.29) | 0.009 |
| ECMO support | 2.64 (1.93–3.61) | <0.001 | 2.87 (1.91–4.32) | <0.001 | 2.44 (1.44–2.11) | 0.001 |
| Mechanical CirculatorySupport | ||||||
| No MCS support | Reference | |||||
| Continuous flow LVAD support | 1.26 (1.10–1.44) | <0.001 | Reference | |||
| Pulsatile flow LVAD support | 1.24 (1.07–1.45) | 0.006 | 1.01 (0.83–1.23) | 0.91 | ||
| BIVAD support | 1.46 (1.19–1.80) | <0.001 | 1.20 (0.95–1.53) | 0.13 | ||
| TAH support | 1.71 (1.20–2.45) | 0.003 | 1.31 (0.90–1.92) | 0.16 | ||
| RVAD (only) support | 2.10 (1.11–3.96) | 0.02 | 1.94 (1.00–3.74) | 0.05 | ||
| Hemodynamic parameters | ||||||
| Mean pulmonary artery pressure ≥30 mmHg | 1.10 (1.00–1.20) | 0.05 | 1.08 (0.96–1.21) | 0.21 | 1.13 (0.97–1.32) | 0.12 |
| Renal/liver function, diabetes | ||||||
| CrCl< 50 mL/min or dialysis | 1.38 (1.24–1.54) | <0.001 | 1.33 (1.16–1.52) | <0.001 | 1.50 (1.24–1.82) | <0.001 |
| Diabetes | 1.06 (0.96–1.17) | 0.27 | 1.04 (0.92–1.18) | 0.54 | 1.09 (0.93–1.28) | 0.30 |
| Bilirubin ≥ 2mg/dL | 1.28 (1.12–1.45) | <0.001 | 1.21 (1.04–1.42) | 0.02 | 1.40 (1.13–1.73) | 0.002 |
| Panel-reactive antibody data | ||||||
| Composite most recent panel-reactive antibody ≥10% | 1.12 (0.99–1.26) | 0.06 | 1.18 (1.02–1.37) | 0.03 | 1.07 (0.89–1.28) | 0.48 |
| Transplant center characteristics | ||||||
| Year of transplant | 0.99 (0.96–1.02) | 0.52 | 0.99 (0.96–1.03) | 0.70 | 0.99 (0.94–1.04) | 0.68 |
| Moderate- or high-volume listing institution | 0.85 (0.78–0.94) | 0.001 | 0.82 (0.73–0.93) | 0.001 | 0.90 (0.77–1.06) | 0.21 |
| Operative characteristics | ||||||
| Bicaval anastomosis | 0.96 (0.87–1.06) | 0.43 | 0.97 (0.86–1.09) | 0.62 | 0.92 (0.79–1.08) | 0.32 |
| Previous cardiac surgery | N/A | 1.16 (1.02–1.31) | 0.02 | N/A | ||
| Organ ischemic time, ≥4h | 1.26 (1.14–1.39) | <0.001 | 1.27 (1.12–1.45) | <0.001 | 1.23 (1.05–1.46) | 0.01 |
| Donor characteristics | ||||||
| Age ≥50 y | 1.37 (1.18–1.59) | <0.001 | 1.43 (1.20–1.70) | <0.001 | 1.24 (0.91–1.67) | 0.17 |
| Smoking history >20 y | 1.21 (1.08–1.35) | 0.001 | 1.29 (1.12–1.48) | <0.001 | 1.08 (0.89–1.31) | 0.43 |
| Diabetes | 1.36 (1.08–1.70) | 0.008 | 1.46 (1.12–1.91) | 0.006 | 1.23 (0.81–1.86) | 0.33 |
| Donor/recipient matching | ||||||
| Gender match, n (%) | 0.86 (0.77–0.95) | 0.002 | 0.89 (0.79–1.01) | 0.07 | 0.78 (0.65–0.93) | 0.006 |
| Race match, n (%) | 0.95 (0.86–1.05) | 0.34 | 0.94 (0.83–1.06) | 0.31 | 0.97 (0.82–1.15) | 0.73 |
| CMV - donor positive, recipient negative | 1.09 (0.98–1.21) | 0.13 | 1.06 (0.92–1.21) | 0.42 | 1.11 (0.93–1.32) | 0.25 |
| Non-identical ABO blood group match (only compatible) | 0.99 (0.88–1.12) | 0.92 | 1.08 (0.93–1.24) | 0.32 | 0.84 (0.68–1.05) | 0.12 |
| Complete HLA mismatch (all 6 alleles) | 1.03 (0.92–1.15) | 0.64 | 1.02 (0.89–1.17) | 0.76 | 1.04 (0.86–1.25) | 0.68 |
Abbreviations: MCS, mechanical circulatory support; BMI, body mass index; CAD, coronary artery disease; NYHA, New York Heart Association; IABP, intra-aortic balloon pump; ECMO, extracorporeal membrane oxygenation; VAD, ventricular assist device; BIVAD, biventricular assist device; TAH, total artificial heart; RVAD, right ventricular assist device; CrCl, creatinine clearance; CMV, cytomegalovirus; HLA, human leukocyte antigen.
Other variables that appeared to have an inconsistent effect between patients with and without MCS were age ≥ 60, college education, BMI ≥35, recipient diagnosis, center volume, donor age, donor smoking history, donor diabetes, and gender match. Recipient diagnosis was an independent predictor of post-transplantation survival in patients without MCS support with the exception of congenital heart disease but failed to become statistically significant in patients with MCS using ischemic cardiomyopathy as the reference. Additionally, patients who underwent transplantation at a moderate-to-high volume institution had a lower hazard of death than patients who underwent transplantation at an institution with less experience both in the entire cohort and in the subgroup of patients without MCS; however, this did not hold for the subgroup of patients with MCS. Among patients with MCS, age ≥60 had an adverse effect on long term outcomes while college education and gender match were predictors of improved survival; these were not significant in the non-MCS cohort. BMI ≥35, donor age, donor smoking history, donor diabetes, and previous cardiac surgery each were predictors of worse post-transplantation survival for patients without MCS but did not affect survival in patients with MCS; previous cardiac surgery was not evaluated in patients with MCS as all patients were considered to have had previous cardiac surgery. Consistent predictors of post-transplantation mortality were African American race, NYHA IV, ECMO, ventilator-dependence, renal insufficiency, bilirubin ≥2, and organ ischemic time >4 hours. Private insurance was a consistent predictor of post-transplantation survival.
Multivariate cox regression utilizing the entire cohort revealed increased hazard with each of the different MCS devices when compared with patients without MCS: continuous flow LVAD support, HR: 1.26 (CI 1.10–1.44), P<0.001; pulsatile flow LVAD, HR: 1.24 (CI: 1.07–1.45), P=0.006; BiVAD, HR: 1.46 (CI: 1.19–1.80), P<0.001; TAH, HR 1.71 (CI: 1.20–2.45), P=0.003; and isolated RVAD, HR 2.10 (CI: 1.11–3.96), P=0.02, table 4. Restricted to the cohort of patients with MCS, the only device associated with increased hazard compared to the other devices was isolated RVAD, HR: 1.94 (CI: 1.00–3.74), P=0.05.
Kaplan-Meier survival analysis of post-transplant survival was performed separately in patients with and without MCS at the time of transplant, both before and after propensity matching. Unmatched analyses of patients without MCS comparing allosensitized and non-sensitized patients revealed that survival was worse in allosensitized patients compared with non-sensitized patients: 87% vs. 91% at 1-year, 73% vs. 76% at 5-years, P<0.001, figure 1A. However, post-transplantation survival was equivalent between allosensitized and non-sensitized patients who had a durable MCS device implanted: 87% vs. 87% at 1-year, 68% vs. 74% at 5-years, P=0.31, figure 1B. In matched analysis, allosensitized patients without MCS had worse survival compared with non-sensitized patients without MCS: 87% vs. 91% at 1-year, 73% vs. 76% at 5-years, P=0.006, figure 1C. Again in matched analysis, there was no difference in survival between allosensitized patients with MCS compared with non-sensitized patients: 87% vs 87% at 1-year, 71% vs. 68% at 5-years, P=0.59, figure 1D.
Figure 1.
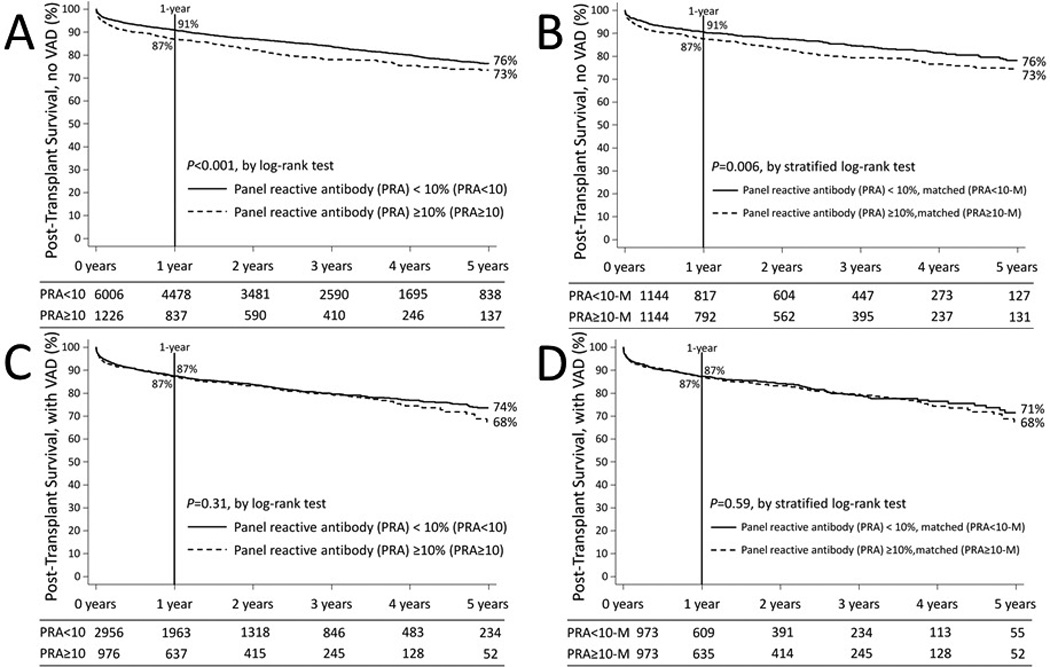
Kaplan Meier Survival Analysis of Post-transplant survival, comparing patients with and without elevated most recent composite panel reactive antibody level; A. Unmatched analysis of patients without MCS, B. Unmatched analysis of patients with MCS implanted, C. Matched analysis of patients without MCS, D. Matched analysis of patients with MCS implanted.
Discussion
MCS is increasingly being employed prior to HTx. Patients receiving MCS at transplantation were more likely to be allosensitized than patients without MCS, but allosensitization was not associated with increased risk of post-HTx mortality in patients with MCS. However, MCS itself was an independent predictor of mortality. In non-MCS patients, allosensitization was associated with an increased hazard for mortality after heart transplantation. Among the subgroup of patients receiving MCS, isolated RVAD implantation was associated with the greatest risk of post-transplant mortality.
Allosensitization
The results of our analysis are consistent with prior studies showing that LVAD implantation is associated with allosensitization.8, 28 In spite of the consistent finding of an association between mechanical circulatory support and allosensitization, the mechanism of sensitization has not been completely delineated. Transfusion of blood products has previously been associated with allosensitization,29, 30 but avoidance of transfusing leukofiltered cellular blood products has not been shown to prevent it.31 Differences in the immunogenicity of the various devices may play a role with more contemporary devices potentially posing a lower risk for allosensitization than earlier iterations of VADs.7, 9 The current analysis demonstrated that each form of MCS except for RVAD had a continued association with increased risk for allosensitization in a contemporary cohort.
The difference in risk associated with allosensitization between MCS and non-MCS patients is not novel per se. A retrospective review of patients bridged-to-transplantation with either a Heartmate XVE (Thoratec corp., Pleasanton, Calif.) or a Heartmate II (Thoratec corp., Pleasanton, Calif.) did not reveal differences in post-transplantation survival comparing patients with PRA >25% and PRA = 0%.32 The current analysis confirms this finding, and it goes further by broadening the cohort to compare patients with a variety of support devices.
The reason for the difference between device-supported and medically managed patients may be related to the immunogenicity of the device. LVAD-related PRA elevation has been observed to peak early and then decline over the course of support; this has been hypothesized to be a result of the initial interaction between patient blood and the device followed by mitigation of the immunogenicity of the device secondary to pseudointima formation.7, 33 With this in mind, explantation of the device would significantly reduce the inflammatory milieu contributing to PRA elevation thus making it a finite process. In contrast, medically treated patients may not have a well-defined reason for PRA elevation potentially suggesting a durable adverse immunologic response to a transplanted organ. Schaffer et al. demonstrated that on the one hand reduction in PRA of allosensitized patients prior to heart transplantation was associated with improved post-transplantation survival in patients without VADs; on the other hand, irreducible PRA was an indicator of poor post-transplantation survival.2 As such, allosensitization appears to be a heterogeneous process, the reversibility of which may be more important than its mere existence.
Durable MCS device implantation and post-transplantation survival
Nativi et al. found in an analysis of the International Society for Heart and Lung Transplantation (ISHLT) registry from 2000 to 2008 that the difference in post-transplantation mortality between medically managed and VAD-supported patients was era-dependent.34 Wozniak et al. further determined that among Status 1A patients the presence of an isolated LVAD implantation was associated with worse post-transplantation survival prior to 2008, though survival was similar in the post-2008 era when the medically managed cohort included patients with intra-aortic balloon pump (IABP).6 These reports suggest the presence of an era effect on the relationship between LVAD and mortality after HTx. Our analysis was limited to a contemporary era (7/12/2006–12/31/2012), and was unable to demonstrate an era effect in the entire cohort or each of the subgroups, i.e. with and without MCS. Additionally, this analysis identified each class of MCS as an independent predictor of post-transplantation mortality suggesting that equivalence has not yet been reached.
This presents a complicated picture. On the one hand, our analysis identified MCS as predictive of post-transplantation mortality. On the other hand, LVAD implantation appears to confer a beneficial effect on waitlist survival when compared with medically managed patients.5,6 Indeed, given the excellent performance of uncomplicated LVAD patients on the waiting list, Dardas et al. suggested that they not be afforded elective status 1A time and even be downgraded from mandatory Status 1B.5 However, an analysis of waitlist data cannot capture the upfront risk associated with the LVAD operation, i.e. not all patients who underwent the initial LVAD operation were eventually waitlisted. Moreover, analyses of waitlist data and data at transplantation are unable to include clinical status at the time of MCS implantation unless the device was implanted while on the waitlist. In this way, the decision to implant an LVAD or any other MCS device must be made while considering the risk associated with the operation, the potential waitlist benefit, and the potential effect on post-transplantation survival. In many cases, patients may not survive to transplantation without implantation of a durable MCS device. Overall, there appears to be a net benefit with appropriate MCS implantation, though further studies must be performed in order to optimize the timing of implantation and the selection of patients.
Limitations
This was a retrospective review of patients undergoing transplantation using registry data. It is limited by potential inconsistencies in reporting data and completeness. Using statistical methods, the effect of missing data in collected variables was mitigated without increasing the likelihood of introducing spurious positive results. However, this does not account for variables that were not collected. As a result, in depth analyses of either the changes to the immunosuppressive regimen as a result of being allosensitized or the effects of allosensitization on cardiac allograft vasculopathy (CAV) were not possible; that information was not available in sufficient detail and quality in the UNOS dataset. Unfortunately, rejection data was also insufficient to produce a satisfactory analysis of the impact of PRA on various forms of rejection, and specific HLA-antibody data was not available and could not be correlated with either survival or CAV. Each of these may be worthy of study in a separate analysis. Finally, this analysis does not include patients who died on the waitlist.
The existence of several methods to screen for PRA introduces variability to the measurement of PRA. Use of different tests by different laboratories can produce substantially different PRA level resulting in labelling one patient as allosensitized by one laboratory and the same patient as not allosensitized at another laboratory.35
Conclusion
Allosensitization is a heterogeneous process that is affected by the presence of MCS. While PRA screening remains beneficial in order to screen for patients who may require a prospective crossmatch, allosensitization was not an independent predictor of mortality in patients with MCS. MCS was an independent predictor of post-HTx mortality, but this result must be taken cautiously as patients being considered for MCS may otherwise not survive to transplantation. As such, MCS should continue to be utilized as a bridge-to-transplantation in appropriately selected patients.
Acknowledgments
Acknowledgments, funding sources, and relevant disclosures
This work was conducted with support from a KL2 Mentored Career Development Award of the Stanford Clinical and Translational Science Award to Spectrum (NIH KL2 TR 001083).
References
- 1.Nwakanma LU, Williams JA, Weiss ES, Russell SD, Baumgartner WA, Conte JV. Influence of pretransplant panel-reactive antibody on outcomes in 8,160 heart transplant recipients in recent era. The Annals of thoracic surgery. 2007;84:1556–1562. doi: 10.1016/j.athoracsur.2007.05.095. discussion 1562–1553. [DOI] [PubMed] [Google Scholar]
- 2.Schaffer JM, Singh SK, Reitz BA, Oyer PE, Robbins RC, Mallidi HR. Heart transplant graft survival is improved after a reduction in panel reactive antibody activity. The Journal of thoracic and cardiovascular surgery. 2013;145:555–564. doi: 10.1016/j.jtcvs.2012.10.025. discussion 564–555. [DOI] [PubMed] [Google Scholar]
- 3.Lund LH, Edwards LB, Kucheryavaya AY, Dipchand AI, Benden C, Christie JD, Dobbels F, Kirk R, Rahmel AO, Yusen RD, Stehlik J, International Society for H, Lung T The registry of the international society for heart and lung transplantation: Thirtieth official adult heart transplant report--2013; focus theme: Age. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2013;32:951–964. doi: 10.1016/j.healun.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Aaronson KD, Eppinger MJ, Dyke DB, Wright S, Pagani FD. Left ventricular assist device therapy improves utilization of donor hearts. J Am Coll Cardiol. 2002;39:1247–1254. doi: 10.1016/s0735-1097(02)01751-5. [DOI] [PubMed] [Google Scholar]
- 5.Dardas T, Mokadam NA, Pagani F, Aaronson K, Levy WC. Transplant registrants with implanted left ventricular assist devices have insufficient risk to justify elective organ procurement and transplantation network status 1a time. Journal of the American College of Cardiology. 2012;60:36–43. doi: 10.1016/j.jacc.2012.02.031. [DOI] [PubMed] [Google Scholar]
- 6.Wozniak CJ, Stehlik J, Baird BC, McKellar SH, Song HK, Drakos SG, Selzman CH. Ventricular assist devices or inotropic agents in status 1a patients? Survival analysis of the united network of organ sharing database. The Annals of thoracic surgery. 2014;97:1364–1371. doi: 10.1016/j.athoracsur.2013.10.077. discussion 1371–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.George I, Colley P, Russo MJ, Martens TP, Burke E, Oz MC, Deng MC, Mancini DM, Naka Y. Association of device surface and biomaterials with immunologic sensitization after mechanical support. J Thorac Cardiovasc Surg. 2008;135:1372–1379. doi: 10.1016/j.jtcvs.2007.11.049. [DOI] [PubMed] [Google Scholar]
- 8.Bull DA, Reid BB, Selzman CH, Mesley R, Drakos S, Clayson S, Stoddard G, Gilbert E, Stehlik J, Bader F, Kfoury A, Budge D, Eckels DD, Fuller A, Renlund D, Patel AN. The impact of bridge-to-transplant ventricular assist device support on survival after cardiac transplantation. The Journal of thoracic and cardiovascular surgery. 2010;140:169–173. doi: 10.1016/j.jtcvs.2010.03.026. [DOI] [PubMed] [Google Scholar]
- 9.Drakos SG, Kfoury AG, Kotter JR, Reid BB, Clayson SE, Selzman CH, Stehlik J, Fisher PW, Merida M, 3rd, Eckels DD, Brunisholz K, Horne BD, Stoker S, Li DY, Renlund DG. Prior human leukocyte antigen-allosensitization and left ventricular assist device type affect degree of post-implantation human leukocyte antigen-allosensitization. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2009;28:838–842. doi: 10.1016/j.healun.2009.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Statistics in medicine. 2009;28:3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1:43–46. [PubMed] [Google Scholar]
- 12.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. Journal of the American Statistical Association. 1958;53:457–481. [Google Scholar]
- 13.Bland JM, Altman DG. The logrank test. Bmj. 2004;328:1073. doi: 10.1136/bmj.328.7447.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 15.Austin PC. The use of propensity score methods with survival or time-to-event outcomes: Reporting measures of effect similar to those used in randomized experiments. Statistics in medicine. 2014;33:1242–1258. doi: 10.1002/sim.5984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Statistics in medicine. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 17.Marshall A, Altman DG, Royston P, Holder RL. Comparison of techniques for handling missing covariate data within prognostic modelling studies: A simulation study. BMC medical research methodology. 2010;10:7. doi: 10.1186/1471-2288-10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White IR, Royston P. Imputing missing covariate values for the cox model. Statistics in medicine. 2009;28:1982–1998. doi: 10.1002/sim.3618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prevention science : the official journal of the Society for Prevention Research. 2007;8:206–213. doi: 10.1007/s11121-007-0070-9. [DOI] [PubMed] [Google Scholar]
- 20.Stuart EA. Matching methods for causal inference: A review and a look forward. Statistical science : a review journal of the Institute of Mathematical Statistics. 2010;25:1–21. doi: 10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mitra R, Reiter JP. A comparison of two methods of estimating propensity scores after multiple imputation. Statistical methods in medical research. 2012 doi: 10.1177/0962280212445945. [DOI] [PubMed] [Google Scholar]
- 22.Rubin D. Multiple imputation for nonresponse in surveys. New York, NY: Wiley; 1987. [Google Scholar]
- 23.Cox DR. Regression models and life-tables. J R Stat Soc Series B Stat Methodol. 1972;34:187–220. [Google Scholar]
- 24.Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–526. [Google Scholar]
- 25.Hosmer DW, Lemeshow S, May S. Applied survival analysis: Regression modeling of time-to-event data. Hoboken, NJ: Wiley-Interscience; 2008. [Google Scholar]
- 26.Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr. 1974;19:716–723. [Google Scholar]
- 27.Costanzo MR, Dipchand A, Starling R, Anderson A, Chan M, Desai S, Fedson S, Fisher P, Gonzales-Stawinski G, Martinelli L, McGiffin D, Smith J, Taylor D, Meiser B, Webber S, Baran D, Carboni M, Dengler T, Feldman D, Frigerio M, Kfoury A, Kim D, Kobashigawa J, Shullo M, Stehlik J, Teuteberg J, Uber P, Zuckermann A, Hunt S, Burch M, Bhat G, Canter C, Chinnock R, Crespo-Leiro M, Delgado R, Dobbels F, Grady K, Kao W, Lamour J, Parry G, Patel J, Pini D, Towbin J, Wolfel G, Delgado D, Eisen H, Goldberg L, Hosenpud J, Johnson M, Keogh A, Lewis C, O'Connell J, Rogers J, Ross H, Russell S, Vanhaecke J, International Society of H Lung Transplantation G The international society of heart and lung transplantation guidelines for the care of heart transplant recipients. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2010;29:914–956. doi: 10.1016/j.healun.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 28.Pagani FD, Dyke DB, Wright S, Cody R, Aaronson KD. Development of anti-major histocompatibility complex class i or ii antibodies following left ventricular assist device implantation: Effects on subsequent allograft rejection and survival. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2001;20:646–653. doi: 10.1016/s1053-2498(01)00232-7. [DOI] [PubMed] [Google Scholar]
- 29.Moazami N, Itescu S, Williams MR, Argenziano M, Weinberg A, Oz MC. Platelet transfusions are associated with the development of anti-major histocompatibility complex class i antibodies in patients with left ventricular assist support. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 1998;17:876–880. [PubMed] [Google Scholar]
- 30.Leffell MS, Kim D, Vega RM, Zachary AA, Petersen J, Hart JM, Rossert J, Bradbury BD. Red blood cell transfusions and the risk of allosensitization in patients awaiting primary kidney transplantation. Transplantation. 2014;97:525–533. doi: 10.1097/01.tp.0000437435.19980.8f. [DOI] [PubMed] [Google Scholar]
- 31.Drakos SG, Stringham JC, Long JW, Gilbert EM, Fuller TC, Campbell BK, Horne BD, Hagan ME, Nelson KE, Lindblom JM, Meldrum PA, Carlson JF, Moore SA, Kfoury AG, Renlund DG. Prevalence and risks of allosensitization in heartmate left ventricular assist device recipients: The impact of leukofiltered cellular blood product transfusions. J Thorac Cardiovasc Surg. 2007;133:1612–1619. doi: 10.1016/j.jtcvs.2006.11.062. [DOI] [PubMed] [Google Scholar]
- 32.Arnaoutakis GJ, George TJ, Kilic A, Weiss ES, Russell SD, Conte JV, Shah AS. Effect of sensitization in us heart transplant recipients bridged with a ventricular assist device: Update in a modern cohort. The Journal of thoracic and cardiovascular surgery. 2011;142:1236–1245. 1245, e1231. doi: 10.1016/j.jtcvs.2011.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kumpati GS, Cook DJ, Blackstone EH, Rajeswaran J, Abdo AS, Young JB, Starling RC, Smedira NG, McCarthy PM. Hla sensitization in ventricular assist device recipients: Does type of device make a difference? The Journal of thoracic and cardiovascular surgery. 2004;127:1800–1807. doi: 10.1016/j.jtcvs.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 34.Nativi JN, Drakos SG, Kucheryavaya AY, Edwards LB, Selzman CH, Taylor DO, Hertz MI, Kfoury AG, Stehlik J. Changing outcomes in patients bridged to heart transplantation with continuous- versus pulsatile-flow ventricular assist devices: An analysis of the registry of the international society for heart and lung transplantation. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2011;30:854–861. doi: 10.1016/j.healun.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 35.Shankar N, Daly R, Geske J, Kushwaha SK, Timmons M, Joyce L, Stulak J, Gandhi M, Kremers W, Park S, Pereira NL. Lvad implant as a bridge to heart transplantation is associated with allosensitization as measured by single antigen bead assay. Transplantation. 2013;96:324–330. doi: 10.1097/TP.0b013e3182985371. [DOI] [PMC free article] [PubMed] [Google Scholar]


