Summary
Langerhans cells (LC) are the resident antigen-presenting cells in human epithelium, and are therefore responsible for initiating immune responses against human papillomaviruses (HPV) entering the epithelial and mucosal layers in vivo. Upon proper pathogenic stimulation, LC become activated causing an internal signaling cascade that results in the up-regulation of co-stimulatory molecules and the release of inflammatory cytokines. Activated LC then migrate to lymph nodes where they interact with antigen specific T cells and initiate an adaptive T-cell response. However, HPV manipulates LC in a suppressive manner that alters these normal maturation responses. Here, in vitro LC activation assays for the detection of phosphorylated signaling intermediates, the up-regulation of activation-associated surface markers, and the release of inflammatory cytokines in response to HPV particles are described.
Keywords: Human papillomavirus, HPV16, Langerhans cells, PI3K/AKT pathway
1. Introduction
High-risk human papillomaviruses (HPV) are sexually transmitted viruses that cause several cancers including cervical cancer [1]. Of the different cancer-causing HPV genotypes, HPV type 16 (HPV16) is by far the most common, leading to more than 50% of all cervical cancers [2]. During its natural life cycle, HPV16 infects the basal cells of the epithelium in vivo where it interacts with Langerhans cells (LC), the resident antigen presenting cells (APC) of the epithelium [3]. Due to their location, LC are responsible for initiating immune responses against pathogens entering the epithelial layer [4].
The expression of HPV16 viral genes and the production of new infectious virions is dependent on the differentiation of basal epithelial cells into mature keratinocytes [5]. This has led much of the papillomavirus research field to utilize virus-like particles (VLP) to study specific aspects of viral internalization and HPV-induced immune responses. 360 copies of the major capsid protein L1 can self-assemble into L1-only VLP when expressed alone, which possess an icosahedral structure composed of 72 L1 pentamers [6]. If L1 is expressed with the minor capsid protein L2, there are between 12 and 72 L2 proteins incorporated per capsid [6,7].
Initial HPV-LC immune responses are mediated through the interaction between HPV capsid proteins and LC surface receptors making VLP a valuable tool for studying HPV capsid protein-mediated immune responses in vitro. Although L1 is sufficient to form a VLP, L1L2 VLP more closely resemble wild type infectious virions. Furthermore, we have recently demonstrated that LC exposed to the L2 protein in HPV16 L1L2 VLP do not become activated whereas L1 VLP are capable of activating LC [8]. Moreover, it has been shown that epithelial LC respond differently to HPV16 VLP when compared to dermal dendritic cells (DC) [8], which suggests that HPV16 has evolved in a specific mechanism to manipulate this unique epithelial APC.
Proper antigenic stimulation leads to a unique signaling cascade within LC shortly after initial contact. Specifically, activation of the PI3K/AKT signaling cascade has been observed in activated LC, and this pathway is manipulated by the HPV16 L2 minor capsid protein [8,9,10,11]. The PI3K/AKT signaling cascade is activated within minutes in response to certain stimuli, and is therefore the first detectable sign of LC activation. The downstream consequences of activation-associated signal cascades within LC include the upregulation of genes associated with T cell stimulation and inflammation as well as the translocation of molecules to the extracellular surface. For example, non-activated LC have low surface expression of MHC class II molecules, while large amounts remain intracellular. However LC that experience an activating or maturating stimulus translocate MHC-II molecules to the cell surface (reviewed in [12]). Additionally, PI3K signaling leads to the transcription of genes controlled by the transcription factor NFkB such as interleukins (i.e. IL6, IL8, and IL12) and TNFα [8,13], which are inflammatory cytokines released by activated LC.
Here, three different techniques for analyzing the activation of LC exposed to HPV16 VLP in vitro are described in detail. Though unique, each assay employs antibodies for immuno-detection of molecules associated with different aspects of LC activation from the initial signal-cascade to the up-regulation of activation-associated surface markers and the release of inflammatory cytokines. Likewise, while the initial steps for the activation of LC are constant for each experiment, each assay differs in the methods necessary for detection and analysis. For instance, the detection of LC activation-associated phosphorylated signaling intermediates is performed via immuno-blotting. The up-regulation of surface markers associated with LC activation is analyzed by flow cytometry. Lastly, supernatants are analyzed for the release of inflammatory cytokines using a multiplex bead array system.
2. Materials
-
Langerhans Cells:
LC can be directly purified from epithelial tissue via separation techniques or can be derived in vitro from CD34+ progenitor cells or peripheral blood monocytes (PBMC) as previously described [13,14,15]. However, the activation assays described herein have been consistently performed on LC derived from PBMC (Section 3.1). In brief, PBMC from healthy donors are obtained by leukapheresis. Leukocytes are purified by Ficoll gradient centrifugation (Nycomed, Oslo, Norway) and stored in liquid nitrogen prior to differentiation (∼150 × 106 PBMC/cryovial; see Note 1).
-
Dendritic Cells:
Dendritic cells (DC) can be used as a control cell-type for activation experiments because it has been previously shown that they differentially respond to HPV16 VLP [8]. Like LC, DC can be isolated from tissue or derived from precursor cells as mentioned above. For use as a control with PBMC derived LC, and to reduce possible confounding variables, DC can be derived from the same PBMC donor used for the generation of LC as previously described (Section 3.2) [15].
-
Virus-Like Particles:
HPV16L1 VLP and HPV16L1L2 VLP can be produced using a recombinant baculovirus expression system in insect cells as previously described [16]. Western blot analyses confirm the presence of L1 and L2 while an ELISA and transmission electron microscopy can be used to confirm the presence of intact particles. An E-toxate kit (Sigma-Aldrich) is used to semi-quantitate endotoxin. Baculovirus DNA used in VLP production procedure has been shown not to activate LC [9], however, endotoxin levels in preparations need to be shown to not activate LC; levels of less than 0.06 in our own preparations do not activate LC [9]. VLP are stored at -80°C until needed. (see Note 2)
-
Commercial antibodies used are as follows:
Immuno-blot antibodies:
PI3K Rb-α-Hn (Cat. no. 4292S; Cell Signaling)
pPI3K Rb-α-Hn (Cat. no. 4228S; Cell Signaling)
AKT Rb-α-Hn (Cat. no. 4685S; Cell Signaling)
pAKT Rb-α-Hn (Cat. no. 9271S; Cell Signaling)
GAPDH Ms-α-Hn (Cat. no. MAB374; Millipore)
Gt-α-Rb IgG-Alexa Fluor 680 (Cat. no. A21109; Life Technologies)
Gt-α-Ms IgG-IRDye800 (Cat. no. 610-132-121; Rockland)
Flow Cytometry Antibodies
-
H
CD80 (B7-1)-FITC Ms-α-Hn (mouse IgM; Cat. no. 305206; Biolegend)
-
I
CD86 (B7-2)-FITC Ms-α-Hn (mouse IgG1; Cat. no. 555657; BD Biosciences)
-
J
HLA DP, DQ, DR (MHC II)-FITC Ms-α-Hn (mouse IgG2a; Cat. no. 555558; BD Biosciences)
-
K
FITC-conjugated isotype controls (IC) (mouse IgM, IgG1, and IgG2a; BD Biosciences)
-
Solutions:
LC/DC complete medium: RPMI 1640 containing 10 mM sodium pyruvate, 10 mM non-essential amino acids (NEAA; Life Technologies), 100 μg/ml penicillin-streptomycin, 55 μM 2-mercaptoethanol and 10% fetal bovine serum (FBS).
Phosphate buffered saline (PBS).
-
Cytokines:
GM-CSF: granulocyte macrophage colony stimulating factor (Genzyme) reconstituted in complete medium at 1 × 105 units/mL (∼ 18 μg/mL).
rhIL-4: recombinant human interleukin 4 (Invitrogen) reconstituted in PBS at 2 × 105 U/mL (∼40 μg/mL).
TGF-β: Transforming growth factor-beta (BioSource International) reconstituted in PBS at 5 μg/mL.
Store reconstituted cytokines following the manufacturer's instructions.
Lipopolysaccharide (LPS; Sigma). Reconstitute LPS in PBS at 1 mg/mL and store the reagent following manufacturer's instructions.
Lysis buffer: M-PER Mammalian Protein Extraction Reagent (Thermo) with 1X Halt Proteinase and Phosphatase Inhibitor Cocktail (Thermo) and 1X EDTA (Thermo). Proteinase and phosphatase inhibitors should be added just prior to use. Alternative lysis buffers may be used at the investigators discretion (ex. RIPA buffer), as long as they solubilize cytoplasmic proteins, are compatible with Immuno-blotting, and contain buffer appropriate protease and phosphatase inhibitors.
Loading buffer: 4X LDS NuPage Sample Buffer (Invitrogen).
Reducing agent: 10X NuPage Sample Reducing Agent (Invitrogen).
Tris buffered saline with 0.5% Tween 20 (TBS/T): Add 100 mL 10X TBS/T to 900 mL deionized H2O. 1X formulation contains 50 mM Tris, 150 mM NaCl, and 0.05% Tween 20 with a pH of 7.6.
Tris-acetate (TA) buffer: 20X Tris-acetate sodium dodecyl sulfate (SDS) running buffer (Invitrogen) diluted with deionized H20 for use with TA SDS-polyacrylamide gel electrophoresis (SDS-PAGE).
MES buffer: 20X MES SDS running buffer (Invitrogen) diluted with deionized H20 for use with Bis-Tris (BT) SDS-PAGE gels.
Blocking buffer: StartingBlock (TBS) Blocking Buffer (Thermo) or other comparable buffer.
10% SDS solution (Thermo).
FACS buffer: PBS (Sigma) complemented with 2% FBS (Omega) and 0.01% sodium azide (Sigma).
4% Paraformaldehyde: Follow the guideline regarding use and disposal of hazardous chemicals and waste. Measure paraformaldehyde and add PBS in a chemical hood to avoid contact with harmful aerosols. For a stock solution, weigh 20 g paraformaldehyde (Sigma) and add it to a 500 mL glass Erlenmeyer flask. Add PBS to a final volume of 500 mL. In a fume hood, stir the solution using a stirring hotplate with heat on and a magnetic stirring bar covered overnight (O/N) until clear. Sterilize the 4% w/v mixture by filtering it with a 0.22 μm filter unit. Aliquot 50 mL into 50 mL tubes and store at -20°C.
-
Flasks, plates, and tubes:
T-175 treated polystyrene tissue culture flasks.
T-75 treated polystyrene tissue culture flasks.
50 mL polypropylene conical tubes.
96-well U-bottom plates with lids.
Microcentrifuge tubes (1.5 and 2.0 mL)
-
Multiplex Human Cytokine/Chemokine Kit and Plate Reader:
The scientific concepts behind the Milliplex Human Cyokine/Chemokine MAP assay (Millipore), or the Bio-Plex Multiplex Cytokine Assay (BioRad) are not unlike those in a capture sandwich enzyme linked immuno-sorbent assay (ELISA). An antibody specific to the target cytokine is coupled to an internally-dyed color-coded bead. The supernatants are incubated with the beads, which are then further stained with biotinylated antibodies that are specific to a different epitope on the target protein, and then detected with a streptavidin-conjugated fluorophore. There are a variety of commercially available fully set-up multiplex human cytokine kits (Millipore, BioRad, Life Technologies) available for purchase, each prepared to measure a unique subset of cytokines.
Also available is the option to purchase custom kits, which allow the researcher to choose which cytokines to detect. For instance, our lab uses a custom Milliplex MAP kit (Millipore) that detects for cytokines released by activated LC, which include IFNα2, IL-1β, IL-6, IL-8, IL-10, IL-12 (p70), IP-10, MCP-1, MIP-1α, MIP-1β, and TNFα. Similarly, for convenience, there is a 14-plex Premixed Bead set for human cytokines that measures many of these (IL-6, IL-8, IL-12, MCP-1, and TNFα) as well as other cytokines (GM-CSF, IFNγ, IL-1β, IL-2, IL-4, IL-5, IL-7, and IL-13). These kits require Luminex instruments and vendor-provided software to read and analyze the results. The cytokines should be chosen carefully depending on the cell type (LC and DC), as well as the appropriate kit and instrumentation. Kits should be stored at 4°C until use
3. Methods
The initial activation steps are the same for all three assays (Sections 3.1-3.4). Activation steps are carried out at physiologic temperature (37°C).
3. 1 Generation of Langerhans Cells
As previously mentioned, primary LC can be isolated from tissue or derived from precursor cells. The following steps are used to derive LC from PBMC.
Thaw frozen PBMC and wash once with LC complete medium. To do this, add thawed cells to ≥20 mL warm LC medium, centrifuge at 500 RCF for 5 min, and decant supernatant to wash away dimethyl sulfoxide (DMSO) used for liquid nitrogen storage. Repeat wash step. Resuspend final cell pellet in 10 mL complete medium.
Plate ∼150 × 106 cells (PBMC should be counted before liquid nitrogen storage) in a 175-cm2 tissue culture flask and incubate the flask for 2 hrs in a 37°C, 5% CO2 humidified incubator to select for plastic adherent cells. Do not disturb culture flasks during this time period.
After 2 hrs incubation, pour off medium and gently wash away excess non-adherent cells with ∼10 mL warm PBS two times.
Culture remaining adherent cells for 7 days in 30 mL fresh LC complete medium, and add 1000 U/mL (∼180 ng/mL) GM-CSF, 1000 U/mL (∼200 ng/mL) IL-4, and 10 ng/ml TGF-β; thaw date is day 1.
Replenish 50% GM-CSF and IL-4 on day 3 and 100% on day 5; replenish 100% TGF-β on days 3 and 5 (see Note 3 for feeding details).
At the end of 7 days, optional phenotyping can be performed to test for proper differentiation (see Note 4).
3.2 Generation of Dendritic Cells
DC can be derived from the same PBMC donor as previously described for control experiments. The following steps are used to derive DC from PBMC.
Thaw frozen PBMC and wash once with DC complete medium. To do this, add thawed cells to ≥20 mL warm LC medium, centrifuge at 500 RCF for 5 min at room temperature (RT), and decant supernatant to wash away DMSO used for liquid nitrogen storage. Resuspend cells in 10 mL complete medium.
Plate ∼150 × 106 cells in a 175-cm2 tissue culture flask and incubate the flask for 2 hrs in a 37°C 5% CO2 humidified incubator to select for plastic adherent cells. Do not disturb culture flasks during this time period.
After 2 hrs incubation, pour off medium, and gently wash away excess non-adherent cells with warm PBS (∼10 ml). Repeat wash.
Culture remaining adherent cells for 7 days in 30 mL fresh DC complete medium, and add 1000 U/mL (∼180 ng/mL) GM-CSF, 1000 U/mL (∼200 ng/mL) IL-4; thaw date is day 1.
Replenish 50% GM-CSF and IL4 on day 3 and 100% on day 5. (see Note 3 for feeding details).
At the end of 7 days, optional phenotyping can be performed to test for proper differentiation (see Note 5).
3.3 Harvest and seed cells
Immature or un-activated LC and DC are sensitive to stimuli; see Note 6 for tips on handling.
-
1
Harvest LC or DC from 175-cm2 culture flasks (see 3.1 or 3.2) by collecting medium (monocyte derived LC and DC are non-adherent) into 50 mL conical tubes.
-
2
Wash flasks with an additional 10 mL warm PBS. Pipette PBS over the bottom of the flasks several times to collect all non-adherent cells, and discard flasks
-
3
Spin down cells at 500 RCF for 5 min at RT.
-
4
Decant supernatant and re-suspend cells in 10 mL PBS to wash away excess cytokines from the medium.
-
5
Spin down cells at 500 RCF for 5 min at RT.
-
6
Decant supernatant and re-suspend cells in 10 mL culture medium (complete medium described above without cytokines).
-
7
Count viable cells with trypan blue stain and hemacytometer or automated cell counter.
-
8a
For the detection of phosphorylated intermediates, add 2×106 cells in 2 mL complete media pre-warmed to 37°C to 2 mL microcentrifuge tubes and proceed to activation (section 3.4); dilute cells to 1 × 106/mL after counting and add 2 mL cell suspension per tube. If cells are at a concentration less than 1 × 106/mL, spin cells down and re-suspend in the appropriate volume of medium for this concentration. Add cells to a minimum of three tubes for each LC and DC; negative control, positive control, and VLP treated groups. (see Note 7 for tips on experimental groups).
-
8b
For the detection of surface markers and the cytokine assay (sections 3.6-3.7), seed 2×106 cells in a 75 cm2 culture flask at a concentration of 2 × 105 cells/mL in 10 mL complete medium pre-warmed to 37°C; dilute cells to 1 × 106/mL after counting and add 2 mL cell suspension per flask containing an additional 8 mL pre-warmed complete medium. Seed cells in a minimum of three flasks for each LC and DC; negative control, positive control, and VLP treated groups. (see Note 7 for tips on experimental groups).
3.4 Activate cells
VLP and LPS are added to LC and/or DC to invoke activation.
Thaw and quantify VLP in mg/mL. Though quantification can be done before cold storage, it is recommended to re-quantify after thawing at least once per VLP prep. The quantification of VLP is preferably done with a Coomassie Blue stain of an electrophoresed reducing gel where the protein content of the L1 band is quantified according to a predetermined quantified standard (see Note 8 for tips on Coomassie quantification).
If using different VLP preps (i.e. HPV16 L1 VLP, HPV16 L1L2 VLP, or VLP from different HPV genotypes), bring all VLP to the same concentration of 0.2 mg/mL in PBS.
For the LPS positive control, dilute LPS to 0.2 mg/mL in PBS (dilute 1:5 from 1 mg/mL stocks).
Add 100 μL of VLP dilutions (10 μg/106 cells) per tube/flask for experimental groups.
Add 100 μL LPS dilution (10 μg/106 cells) per tube/flask for positive controls.
Add 100 μL PBS to negative controls.
3.5 Detection of Activation Associated Phosphorylated Intermediates
LC have been shown to have an increase in p-PI3K and p-AKT when treated with LPS and HPV16 L1 VLP, but only an increase in p-PI3K when treated with HPV16 L1L2 VLP demonstrating that L2 contributes to an altered signaling pattern [8]. To measure these differences, proteins are collected from treated and untreated LC/DC shortly after exposure (5-15 min) to VLP, separated by electrophoresis, and then PI3K, p-PI3K, AKT, and p-AKT are detected with immuno-blotting. Due to the collection of cells shortly after VLP exposure, it is most feasible to perform the activation steps in micro-centrifuge tubes rather than culture flasks (see Note 9). Relative quantities of the non-phosphorylated proteins should remain relatively constant between the different groups.
Spin down cells 5-15 min after the addition of VLP in the activation steps in Section 3.4 (see Note 10 for suggestions on timing) at 500 RCF for 5 min at 4°C; centrifuge should be pre-cooled to 4°C.
Pull off supernatant and wash cell pellet with 1 mL ice-cold PBS.
Spin down cells at 500 RCF for 5 min at 4°C.
Use a pipette to carefully remove and discard the supernatant to leave the pellet as dry as possible.
Prepare the lysis buffer by adding 1 μL of 100X protease and phosphatase inhibitors to 100 μL lysis buffer; scale up as needed. Re-suspend cell pellet in 100 μL ice-cold lysis buffer containing protease and phosphatase inhibitors.
Incubate at 4°C for 15 min and vortex tubes for 10 sec every 2.5 min.
Centrifuge at >10,000 RCF for 15 min at 4°C to spin down insoluble lipid complexes.
Transfer the supernatant (soluble protein in lysis buffer) to a clean pre-chilled tube on ice (siliconized tubes are recommended to avoid protein adherence to tubes).
Quantify protein and normalize samples based on the lowest concentration i.e. dilute samples to match the lowest concentration. The sample concentration for detection of phospho-proteins should not be lower than 2 mg/mL (see Note 11). For same-day use maintain on ice, or for long-term storage, quick freeze samples using a dry ice-ethanol bath, then store samples at -80°C.
Make 100 μL normalized running samples (based on protein concentrations) with sample loading buffer and reducing agent.
Heat samples at 70°C for 10 min and prepare for SDS-PAGE.
Set up SDS-PAGE gel boxes for 4 gels; 2 × 7% Tris-acetate (TA) gels in TA buffer for the detection of PI3K and p-PI3K, and 2 × 10% Bis-Tris (BT) gels in MES buffer for the detection of AKT and p-AKT (see Note 12).
-
Load the 100 μL running samples into 4 different gels as follows:
15 μL into 7% TA gel #1 (for PI3K)
30 μL into 7% TA gel #2 (for p-PI3K)
15 μL into 7% BT gel #1 (for AKT)
30 μL into 7% BT gel #2 (for p-AKT)
-
Electrophores gels as follows:
TA gels (#1 and #2) at 150V for 1 hr
BT gels (#1 and #2) at 200V for 50 min
Transfer gels to nitrocellulose or PVDF membranes (optimize for protein size).
Incubate in blocking buffer overnight at 4° C with mixing.
Wash membranes once with TBST.
-
Incubate membranes with ∼10 mL primary antibody mixture overnight at 4° C as follows:
TA gel #1 with α-PI3K diluted 1:1000 in TBST containing 10% blocking buffer
TA gel #2 with α-p-PI3K diluted 1:1000 in TBST containing 10% blocking buffer
BT gel #1 with α-AKT diluted 1:1000 in TBST containing 10% blocking buffer
BT gel #2 with α-p-AKT diluted 1:1000 in TBST containing 10% blocking buffer
Each additionally with α-GAPDH diluted at 1:2000.
Wash membranes 5 × 5 min with ∼10 ml TBST at room temperature (RT) with rocking.
Incubate each membranes with ∼10 mL secondary antibody mixture containing 1:25000 Goat-α-RB Alexa Fluor 680, 1:25000 Goat-α-Ms IRDye800, 10% blocking buffer, and 0.01% SDS (1:1000 dilution of 10% SDS solution) in TBST for 1 hr at RT with rocking.
Wash membranes 4 × 5 min with TBST at RT with rocking.
Wash once with TBS (no Tween-20) for 5 min at RT with rocking. This is done to remove the Tween-20, which can otherwise interfere with the infrared imager.
Visualize membranes with an infrared imager and normalize band intensities of signaling molecules (PI3K/p-PI3K and AKT/p-AKT) to the band intensities of GAPDH for relative quantities (see Note 13 for alternative).
3.6 Detection of Up-regulated Activation-Associated Surface Markers
Similar to the signaling molecules, there has also been reported differences in the up-regulation of surface markers in LC treated with L1 and L1L2 VLP [8]. For this assay, LC/DC are incubated for 48 hrs following activation and then the up-regulation of activation-associated surface markers (i.e. MHC class II, CD86, CD80) is measured via flow cytometry.
-
1
Collect cells into 15 mL polypropylene centrifuge tubes.
-
2
Spin down cells at 500 RCF for 5 min at 4°C (pre-cool centrifuge if necessary as all subsequent steps are performed at 4°C).
-
3
Pull off supernatant and re-suspend cell pellet with 1 mL ice-cold FACS buffer.
-
4
Transfer 100 μL (2×105 cells) cell suspension per well into 7 wells per cell group (i.e. untreated LC/VLP treated LC) across a row in a 96-well U-bottom plate for extracellular staining (see Figure 1 for example set-up). Additional stains may be added with the remaining cells.
-
5
Place plate on ice and prepare the extracellular stains as follows:
MHC II: 40 μL MHC II Ab into 960 μL FACS buffer (1 mL total volume)
CD86: 40 μL CD86 into 960 μL FACS buffer (1 mL total volume).
CD80: 40 μL CD80 into 960 μL FACS buffer (1 mL total volume).
IgG2a IC: 2 μL IgG2a Ab into 998 μL FACS buffer (1 mL total volume).
IgG1 IC: 2 μL IgG1 Ab into 998 μL FACS buffer (1 mL total volume).
IgM IC: 2 μL IgM Ab into 998 μL FACS buffer (1 mL total volume).
-
6
Spin down plate at 500 RCF for 5 min at 4°C (with pre-cooled centrifuge).
-
7
Flick off supernatant and lightly vortex plate to loosen cell pellet.
-
8
Resuspend cells in 100 μL (final concentration is 20 μL/106 cells for MHC II, CD86, and CD80; 1 μg/106 cells for all IC) stain mixtures down the rows of the plate (see Figure 1). For un-stained cells, resuspend in 100 μL FACS buffer.
-
9
Incubate plate for 1 hr at 4°C.
-
10
Wash cells 4 × 5 min with 150 μL FACS buffer. Centrifuge plate at 500 RCF for 5 min at 4°C, flick off supernatant and lightly vortex plate to loosen cell pellet, and resuspend cells in 150 μL FACS buffer.
-
11a
If proceeding directly to flow cytometry, transfer the entire cell suspensions to FACS tubes. Rinse wells with an additional 150 μL FACS buffer and add to the cell suspensions.
-
11b
If flow cytometry will be performed at a later time, transfer the entire cell suspensions to FACS tubes. Rinse wells with an additional 150 μL 4% paraformaldehyde and add to the cell suspensions (2% final paraformaldehyde concentration). Mix well and store at 4°C until analysis.
-
12
Analyze fluorescence with flow cytometry.
Figure 1.
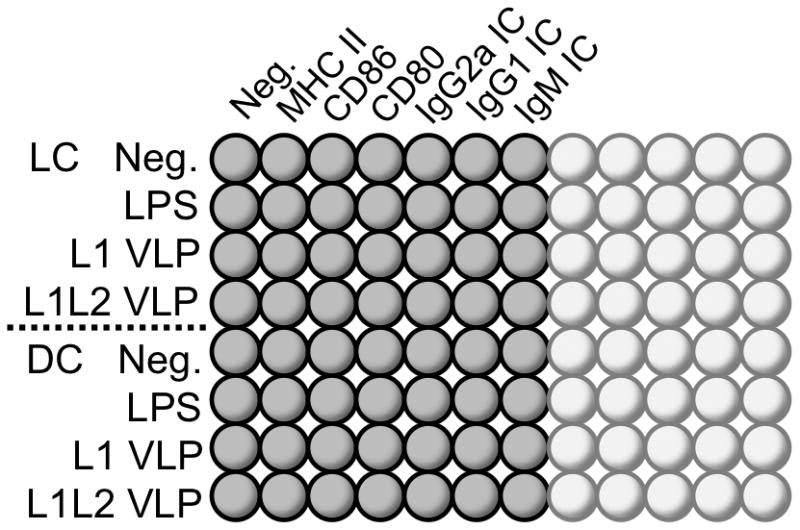
Example plate set-up. The cell groups are listed down the left side and the different extracellular stain groups are listed at top.
3.7 Bio-Plex Cytokine Assay
Cells are incubated for 48 hours following activation and then the supernatants are collected and analyzed for the release of inflammatory cytokines via a multiplexing cytokine assay. Follow the instructions provided by the manufacturers that are specific to the kit.
To prepare samples:
Collect 200 μL of cell supernatants after 48 hours (other time points may be tested as well).
Centrifuge at 1000 RCF for 10 min to remove debris from the samples.
Immediately store samples at -20°C until use and avoid multiple freeze thaws (see Note 14).
4. Notes
PBMC should be stored in liquid nitrogen with freezing medium containing 90% FBS, and 10% DMSO. Experiments call for ∼150 × 106 cells to be cultured per culture flask so ideally freeze this number of PBMC per 1mL freezing medium per cryovial.
When possible, avoid multiple freeze-thaw cycles of VLP preparations.
-
For cytokines reconstituted at concentrations suggested in Section 3.1-3.2, add cytokines as follows:
Day 1: 300 μL GM-CSF (30,000 U), 150 μL IL-4 (30,000 U), and 60 μL TGF-β for LC only.
Day 3: 150 μL GM-CSF (15,000 U), 75 μL IL-4 (15,000 U), and 60 μL TGF-β for LC only.
Day 5: 300 μL GM-CSF (30,000 U), 150 μL IL-4 (30,000 U), and 60 μL TGF-β for LC only.
Properly derived LC express certain surface markers that can be detected with extracellular immuno-staining and flow cytometry. For example, LC express CD207 (Langerin), E-cadherin, and CD1a.
Properly derived DC express certain surface markers that differ from LC that can be detected with extracellular immuno-staining and flow cytometry. DC specific markers include CD1c and CD209 (DC-SIGN).
Gentle handling during the harvesting and seeding steps for LC and DC is necessary because harsh handling may inadvertently activate cells.
A minimum of 3 groups per cell type (i.e. LC or DC) in the seeding step is required; a negative untreated control, a positive TLR agonist control such as LPS, and an HPV16 VLP experimental group. Additional groups could include other TLR agonists, and differential VLP such as L1-only VLP and L1L2 VLP or VLP from other HPV types.
Many protein quantification methods (e.g., Bradford and coomassie) depend on a reagent binding to available primary amine groups on the protein of interest, which causes a change in absorption of the reagent at a pre-determined wavelength. VLP have many of these available amine groups hidden within the stable capsid structure, therefore a method that breaks apart the capsid and linearizes the individual capsid proteins such as separation with SDS-PAGE in reducing conditions followed by a Coomassie blue stain has been most consistent in our own experience, though other methods may also work. For a Coomassie stain of VLP, first prepare VLP running samples for reducing SDS-PAGE (VLP sample with loading buffer and reducing agent). Heat running samples to 95°C for ten minutes to melt VLP into individual components (i.e., monomeric L1 and L2). Load samples and predetermined protein standards (i.e., BSA in increasing concentrations) into a 10% BT gel along with a protein ladder. Electrophorese gel at 160 V for 1 hr. Pre-fix gel with 20 mL fixing solution (43% acetic acid and 7% methanol added to deionized H20) for 15 min. Wash with approx. 100 mL deionized H20 3 × 5 min. Add 20 mL GelCode Blue Stain Reagent (Thermo) until protein bands appear (approx. 10-30 min). Wash gel with 100 mL deionized H20 3 × 5 min. Optimization and modifications can be made per manufacturer's instructions. Scan with infrared scanner and quantify L1 bands (L1 appears as a strong band at ∼55 kDa with 700 nm excitation) according to protein standards.
Instead of seeding 2 × 106 cells into flasks, 2 × 106 LC/DC can be put directly into microcentrifuge tubes as mentioned in Section 3.3, and the activation steps from Section 3.4 can be done within them. This can be done in a smaller volume as well i.e., 2 × 106 in 1 mL complete media. While this high cell concentration could cause LC to activate over a longer time period, the short time frame of the phosphorylation assay prevents LC self-activation, and allows for better control of the time points. Therefore, the HPV VLP or LPS can be added directly to the small volume of cells in the microcentrifuge tubes as directed in Section 3.4. Then the cells can be centrifuged immediately after activation at 500 RCF for 5 min at 4°C at the indicated time point (5-15 min) to stop the activation at that time, and to cease intracellular signaling. Proceed with the detection of phosphorylated intermediates protocol from Section 3.5.
The intracellular signaling cascade within LC happens rapidly after stimulation with an appropriate antigen and proceeds stepwise from early signaling molecules to later signaling molecules. Therefore the detection of early phosphorylated intermediates such as p-PI3K may be optimal closer to 5 min whereas the detection of p-AKT may be optimal closer to 15 min. This must be optimized by the end user.
The sample concentrations should not be lower than 2 mg/mL for the detection of phosphorylated intermediates because of the sensitivity of the phospho-antibodies suggested in Section 2.4. If the concentrations of protein collected from an appropriate lysis buffer are consistently less than 2 mg/mL from 2 × 106 cells, then more cells should be used per group to increase the concentration while using the same volume of lysis buffer.
The commercially available antibodies optimized for these activation-associated target proteins are all of rabbit origin (Cell Signaling), therefore non-phosphorylated and phosphorylated versions of the same protein are not distinguishable on the same gel as they require the same anti-Rb secondary antibody for detection. Additionally, the detection of the phosphorylated intermediates requires more input protein than the detection of their non-phosphorylated partners. Lastly, PI3K and AKT are different sized (85 kDa vs 60 kDa respectively) and require different running voltages for optimal separation. Therefore running 4 separate gels for the detection of each protein as described is recommended for the best detection and resolution of each.
As an alternative to the fluorophore-conjugated secondary antibodies, horseradish peroxidase-(HRP)-conjugated secondary antibodies can be used followed by the addition of an HRP-sensitive chemiluminescent substrate and plain film exposure.
Samples should not be stored in glass; use polypropylene tubes.
References
- 1.Walboomers JMM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12–19. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 2.Bosch F, M M, Munoz N, Sherman M, Jansen A, Peto J, Schiffman M, Moreno V, Kurman R, Shah K. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on servical cancer (IBSCC) Study Group. J Natl Cancer I. 1995;87:796–802. doi: 10.1093/jnci/87.11.796. [DOI] [PubMed] [Google Scholar]
- 3.Stanley MA, P MR, Coleman N. HPV: from infection to cancer. Biochem Soc T. 2007;35:1456–1460. doi: 10.1042/BST0351456. [DOI] [PubMed] [Google Scholar]
- 4.Merad M, Ginhoux F, Collin M. Origin, homeostasis and function of Langerhans cells and other langerin-expressing dendritic cells. Nat Rev Immunol. 2008;8:935–947. doi: 10.1038/nri2455. [DOI] [PubMed] [Google Scholar]
- 5.Cumming S, C-I T, Milligan S, Graham SV. Human Papillomavirus type 16 late gene expression is regulated by cellular RNA processing factors in response to epithelial differentiation. Biochem Soc T. 2008;36:522–524. doi: 10.1042/BST0360522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirnbauer R, Booy F, Cheng N, Lowy DR, Schiller JT. Papillomavirus L1 major capsid protein self-assembles into virus-like particles that are highly immunogenic. Proc Natl Acad Sci U S A. 1992;89:12180–12184. doi: 10.1073/pnas.89.24.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buck CB, Cheng N, Thompson CD, Lowy DR, Steven AC, et al. Arrangement of L2 within the papillomavirus capsid. J Virol. 2008;82:5190–5197. doi: 10.1128/JVI.02726-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fahey LM, Raff AB, Da Silva DM, Kast WM. A major role for the minor capsid protein of human papillomavirus type 16 in immune escape. J Immunol. 2009;183:6151–6156. doi: 10.4049/jimmunol.0902145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fausch SC, Da Silva DM, Rudolf MP, Kast WM. Human papillomavirus virus-like particles do not activate Langerhans cells: a possible immune escape mechanism used by human papillomaviruses. J Immunol. 2002;169:3242–3249. doi: 10.4049/jimmunol.169.6.3242. [DOI] [PubMed] [Google Scholar]
- 10.Fausch SC, DS D, Kast WM. Differential uptake and cross-presentation of human papillomavirus virus-like particles by dendritic cells and Langerhans cells. Cancer Res. 2003;63:3478–3482. [PubMed] [Google Scholar]
- 11.Fausch SC, Fahey LM, Da Silva DM, Kast WM. Human papillomavirus can escape immune recognition through Langerhans cell phosphoinositide 3-kinase activation. J Immunol. 2005;174:7172–7178. doi: 10.4049/jimmunol.174.11.7172. [DOI] [PubMed] [Google Scholar]
- 12.Romani N, Clausen BE, Stoitzner P. Langerhans cells and more: langerin-expressing dendritic cell subsets in the skin. Immunol Rev. 2010;234:120–141. doi: 10.1111/j.0105-2896.2009.00886.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peiser M, Koeck J, Kirschning CJ, Wittig B, Wanner R. Human Langerhans cells selectively activated via Toll-like receptor 2 agonists acquire migratory and CD4+T cell stimulatory capacity. J Leukocyte Biol. 2008;83:1118–1127. doi: 10.1189/jlb.0807567. [DOI] [PubMed] [Google Scholar]
- 14.Renn CN, Sanchez DJ, Ochoa MT, Legaspi AJ, Oh CK, et al. TLR activation of Langerhans cell-like dendritic cells triggers an antiviral immune response. J Immunol. 2006;177:298–305. doi: 10.4049/jimmunol.177.1.298. [DOI] [PubMed] [Google Scholar]
- 15.Fahey LM, Raff AB, Da Silva DM, Kast WM. Reversal of human papillomavirus-specific T cell immune suppression through TLR agonist treatment of Langerhans cells exposed to human papillomavirus type 16. J Immunol. 2009;182:2919–2928. doi: 10.4049/jimmunol.0803645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirnbauer R, B F, Cheng N, Lowy DR, Schiller JT. Papillomavirus L1 major capsid protein self-assembles into virus-like particles that are highly immunogenic. Proc Natl Acad Sci U S A. 1992;89:12180–12184. doi: 10.1073/pnas.89.24.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]


