Abstract:
Studies of tenofovir disoproxil fumarate (TDF)-emtricitabine (FTC)–based preexposure prophylaxis (PrEP) have not focused on transgendered women who are at disproportionate risk of HIV acquisition. Concerns exist for drug interactions between cross-sex therapy (estradiol, progestins, and spironolactone) with tenofovir disoproxil fumarate–emtricitabine. This review assessed the experimental and theoretical risk for such drug interactions. It was found that none of these medications are implicated as major perpetrators of drug interactions, and the classes use different metabolic pathways for clearance, suggesting a low likelihood for interactions in either direction. Subanalyses of transgender women in Preexposure Prophylaxis Initiative suggested PrEP efficacy if adherence was high. Nevertheless, several research gaps were identified, particularly the need for controlled interaction studies in transgendered women, including effects on renal clearance, intracellular tenofovir diphosphate and emtricitabine triphosphate in target cells, as well as hormone effects on HIV susceptibility and immunity. PrEP should continue to be offered to transgender women while additional research is planned or pending.
Key Words: pharmacology, PrEP, transgender
INTRODUCTION
Transgender women (ie, male-to-female) have one of the highest incidence and prevalence of HIV infection in the United States and around the world.1–3 Preexposure prophylaxis (PrEP) with tenofovir disoproxil fumarate (TDF)–emtricitabine (FTC) is a promising modality to curb HIV incidence in this population, but PrEP studies have thus far focused on men who have sex with men (MSM),4,5 heterosexual men and women,6,7 person who inject drugs,8 and cis-gender women (ie, born female).9,10 Inclusion of transgender women has been limited, underscoring an urgent need to focus PrEP research on these individuals to increase uptake, facilitate access, and ensure safe and effective PrEP use.
A significant question for the transgender community is whether PrEP interacts with transgender hormonal therapy, as no studies have assessed interactions to date.11 The medications used to achieve feminization fall into 3 broad categories: estrogens, antiandrogens, and the possible use of a progestin. The preferred delivery of estrogen is 17-β estradiol (estradiol) or ester conjugates (eg, estradiol valerate), given sublingually, orally, transdermally, or intramuscularly. Antiandrogenic therapy is often achieved with spironolactone, a mineralocorticoid with antiandrogenic activity. The use of progestins is not universally accepted. The Endocrine Society clinical practice guidelines omit their use in their recommendations.12 The World Professional Association for Transgender Health Standards of Care13 calls their use “controversial,” acknowledging that some clinicians consider that breast development is enhanced, but they cite a lack of data to support this claim.
The following review will evaluate experimental and theoretical risk for drug interactions between TDF–FTC with estradiol, progestins, and spironolactone.
ANALYSIS OF TRANSGENDER WOMEN IN RECENT PrEP STUDIES
The most important information for potential drug interactions influencing PrEP efficacy in transgendered women comes from trials. The Preexposure Prophylaxis Initiative (iPrEx), also known as the iPrEx trial, and its open-label extension (iPrEx-OLE) have specifically reported enrollment and subanalysis of transgender women, although neither were designed to evaluate efficacy in this population. Other trials excluded transgender women or did not provide any specific information on transgender enrollment or efficacy.4–10,14–16
iPrEx was a multinational (Brazil, Ecuador, Peru, Thailand, South Africa, and the United States), randomized controlled trial, in which 2499 HIV-negative MSM or transgender women were assigned to daily coformulated oral TDF/FTC or placebo.4 There was a 44% reduction in the incidence of HIV in the TDF/FTC arm, but a subanalysis based on drug concentrations estimated ≥96% efficacy for high-adherers (at least 4 or more doses per week).17 Gender identity and the use of feminizing hormones in iPrEx were determined by self-report. The overall number of transgender women was 339 (14%), with 296 (12%) reporting being transgender women, 29 (1%) identifying as women, and 14 (1%) identified as men but used feminizing hormones.18 Compared with MSM, transgender women had significant vulnerabilities. They were younger, less educated, had more sexual partners and transactional sex, had higher incidence of sexually transmitted infections, and reported less frequent use of condoms for receptive anal intercourse. Twenty percent of the transgender women reported any use of feminizing hormonal regimens, which included progestins (74%), synthetic or natural estrogens (72%), and antiandrogens (23%). Regardless of hormone use, tenofovir diphosphate (TFV-DP) in viably cryopreserved peripheral blood mononuclear cells (PBMC) was detected less consistently in transgender women vs MSM, suggesting less consistent adherence. Importantly, drug detection was less consistent in transgender women who reported receptive anal intercourse without a condom. In contrast, drug detection was more consistent in MSM who reported receptive anal intercourse without a condom. This difference was reflected in the efficacy results. HIV seroconversion was no different in transgender women randomized to the TDF–FTC arm vs the placebo group (11 vs 10 seroconversions) with a hazard ratio (HR) of 1.1 (95% CI: 0.5 to 2.7). In contrast, the HR in MSM was 0.5 (95% CI: 0.34 to 0.75); this efficacy difference did not reach significance; P = 0.09. No study drugs were detected in any of the 11 transgender women at the time seroconversion was documented.18
iPrEx-OLE was also a multinational study conducted between 2011 and 2013 in which the uptake and the adherence to TDF/FTC–based PrEP were evaluated in 1603 HIV-negative MSM and transgender women who had previously participated in PrEP trials.5 In this study, 1225 (76%) participants received PrEP during any portion of the study, and the incidence of HIV infection was 1.8 vs 2.6 infections per 100 person-years in those receiving PrEP vs those who declined PrEP (HR 0.51, 95% CI: 0.26 to 1.01).5 The study population included 192 transgender women, of whom 151 (79%) elected to take PrEP.18 The study used TFV-DP in red blood cells measured with dried blood spots (DBS) as a marker of adherence. This moiety exhibits a 17-day half-life, providing information about cumulative dosing.19 The study showed that protective DBS concentrations (ie, TFV-DP of 700 fmol/punch, commensurate with 4 or more doses per week) were less frequently observed in transgendered women compared with MSM, particularly in those reporting hormone use.18 In total, there were 3 seroconversions among transgender women, 2 in those who received PrEP compared with 1 in the group who declined PrEP. No infections were documented in transgender individuals with DBS reflective of 4 or more TDF/FTC doses per week on average.18 Taken together, these iPrEx subanalyses suggest that PrEP use may be lower in transgender vs MSM (possibly because of drug interaction concerns),18 but when used, it seems to be effective.
PHARMACOLOGY OF TDF–FTC FOR PrEP
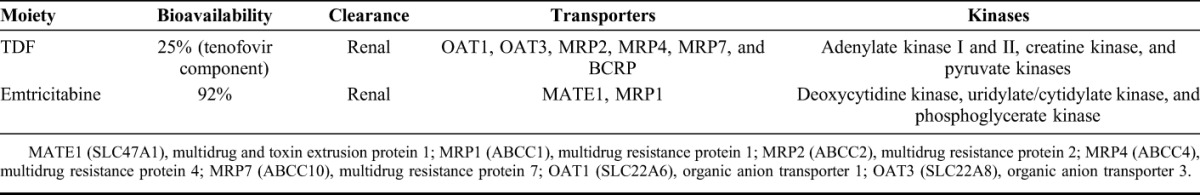
The pharmacokinetic (PK)–pharmacodynamic continuum for TDF–FTC for PrEP is complex, as illustrated in Figure 1. In addition to traditional plasma pharmacokinetics, TDF–FTC requires adequate distribution to genital and lymph tissues, cellular uptake by target cells, phosphorylation and accumulation to effective intracellular TFV-DP/emtricitabine triphosphate (FTC-TP) concentrations, successful competition against endogenous deoxynucleoside triphosphates (dNTPs) for reverse transcriptase, potential immune contributions, followed by pharmacologic effect.20 Each step in the continuum is governed by factors that could be influenced by hormones such as kinase or transporter expression/function, dNTP levels, or immunity. The main kinases and transporters that influence TDF and FTC dispositions are shown in Table 1.21–25 It should be noted that the pharmacologic relevance of transporters can be difficult to interpret, as transporters have overlapping activities, can be broadly distributed anatomically, and can influence multiple PK processes (absorption, clearance, and distribution).26
FIGURE 1.
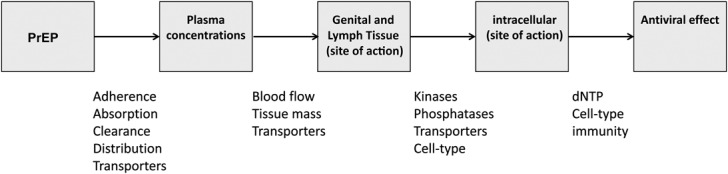
The pharmacologic continuum for TDF-FTC–based PrEP. Potential factors governing this continuum are noted at each step.
TABLE 1.
Summary of Enzymes Influencing TDF–FTC Disposition
In vitro studies suggested that estrogens or progestins can increase or decrease TFV-DP and FTC-TP (or lamivudine triphosphate) depending on the dose and the cell type (genital immune cells, genital epithelial cells, PBMC, or cell lines).27–29 Other studies show that transporter expression is differentially expressed in rectal vs female genital tissues,30 raising possibilities that hormones could influence transporter distribution. However, these kinds of in vitro findings do not reliably translate to clinical relevance.31 Further studies in vivo are needed to explore hormone effects on intracellular TFV-DP and FTC-TP including transporter expression in tissues of relevance for HIV infection. Given the difficulty in studying these issues in vivo, this is a well-suited setting for simulations and physiologically based pharmacokinetic modeling.32,33
DRUG INTERACTION CONSIDERATIONS
TDF and FTC have low potential for major drug interactions.34–36 TDF was studied with contraceptive ethinyl estradiol and norgestimate (a progestin) in women. The 90% CI for area of the concentration time curve AUC, Cmax, and Ctrough ratios (with and without TDF) for ethinyl estradiol and deacetyl norgestimate (the active metabolite measured in the study) were well within the prespecified boundaries of 0.8–1.25, suggesting no clinically relevant interaction. The mean tenofovir Cmax and AUC were 340 ng/mL and 2970 ng·h·mL−1, which were consistent with historical data.34,37 Although the metabolism of ethinyl estradiol differs from estradiol, this study supports a low likelihood for plasma interactions between these medication classes. It is important to note that FTC has not been studied individually with hormone therapy to our knowledge. Given the low interaction profile of FTC,34–36 and its renal clearance, there is also a low likelihood for plasma interactions between these medication classes. Nevertheless, transgendered women are a different population than women using contraception, and estradiol, spironolactone and other progestins such as medroxyprogesterone are different medications (described below). Controlled studies are needed to evaluate plasma and intracellular interactions for these specific medications in the transgender population.
Considerations for Estradiol
Men normally produce low levels of estradiol in the testes and peripheral tissues, resulting in plasma estradiol concentrations of 20–30 pg/mL.38 During transgender therapy, the proposed goal for estradiol concentrations is 100–200 pg/mL (similar to estradiol concentrations during the midluteal phase in women).12,39,40 Importantly, this concentration goal enables therapeutic drug monitoring to maintain target concentrations when faced with drug interaction concerns (commercial assays are readily available).41
Estradiol metabolism is complex, occurring in intestinal mucosa, liver, kidney, and steroid-producing tissues.39 When taken orally, estradiol is significantly metabolized in the intestinal mucosa to estrone (a less active estrogen) by 17β-hydroxysteroid dehydrogenase (17β-HSD). Further metabolism occurs on the first pass through the liver, resulting in numerous metabolites (as many as 100 have been identified), predominately sulfated and glucuronidated conjugates.39 The bioavailability of oral estradiol is less than 5%. Similar bioavailability is observed for estradiol valerate, an ester conjugate of estradiol, because it undergoes rapid ester hydrolysis upon absorption and first pass in the liver, and simultaneously the same metabolism of estradiol occurs.42 When given intramuscularly or transdermally, the drug releases slowly, avoiding the first-pass effect of the liver and providing a more prolonged concentration time profile. Nevertheless, the same metabolic pathways are involved in estradiol disposition. To our knowledge, no major transporter involvement has been reported for estradiol disposition, although multidrug resistance protein 2 (ABCC2, MRP2) is involved with estradiol glucuronide clearance, and estradiol and estrone were reported as breast cancer resistance protein (ABCG2, BCRP) inhibitors.39,43,44 The implication of BCRP inhibition on TFV disposition is uncertain, but unlikely to cause major pharmacokinetic changes given the numerous other transporters involved in its disposition (Table 1). Generally, estradiol has not been implicated as a major perpetrator of drug interactions.35,36
Considerations for Progestins
Although controversial (and beyond the scope of this review), medroxyprogesterone has been implicated as increasing risk of HIV transmission in women, owing to thinning of vaginal mucus and the epithelial barrier, immunosuppression, and/or increased target cells in the endocervix.45–49 It is not evident whether these effects may extend systemically or into penile or rectal mucosa for transgender individuals, but clearly this is an area in need of study. Importantly, no loss of PrEP effectiveness was identified for TDF or TDF–FTC among medroxyprogesterone-treated humans (including women or their male partners)50 or a macaque model.51
Like estradiol, progesterone and synthetic progestins such as medroxyprogesterone are highly metabolized in the gut and liver with approximately 5% bioavailability. CYP3A4 seems to be the principal enzyme for medroxyprogesterone clearance.52 Progestins such as medroxyprogesterone are not implicated as major perpetrators of drug interactions.35,36 In vitro studies suggest MRP2 and P-glycoprotein (Pgp) (ABCB1, Pgp) inhibition, which might raise TDF bioavailability and slow TFV renal clearance, but in vivo studies are needed for confirmation.53 In contrast to these effects, the MTN001 study reported lower (∼20%) TFV plasma concentrations and TFV-DP in PBMC among women receiving injectable or oral contraception, but adherence or other variables may have confounded this finding and follow-up PK modeling of the same study did not report the same finding.54,55
Considerations for Spironolactone
Like estrogens and progestins, spironolactone undergoes extensive hepatic metabolism including deacetylation by esterases followed by glucuronidation.56,57 Several metabolites are pharmacologically active (eg, 7-alpha-thiomethyl spironolactone and canrenone).57 Animal and in vitro studies suggested that spironolactone was an inducer of metabolism, possibly acting through Pregnane X Receptor, which would upregulate metabolic enzymes and transporters such as Pgp and others.23,58 However, spironolactone is not implicated as a major perpetrator of drug interactions in vivo, suggesting a disconnect between in vitro/animal studies and the human profile.35,36 Spironolactone does not influence furosemide (an organic anion transporter 1/3 substrate) pharmacokinetics in vivo, which is relevant for TFV, also an organic anion transporter 1/3 substrate (Table 1).26,59 The product information for Aldactone (spironolactone) lists drug interactions mainly involving hyperkalemia risk, (eg, concomitant Angiotensin Converting Enzyme ACE inhibitors), and a potential increase in digoxin concentrations (a Pgp substrate).57 This profile is not consistent with major Pregnane X Receptor activation and enzyme/transporter induction in vivo, but human volunteer studies are needed to better define spironolactone drug interactions.
CONCLUSIONS
This review did not identify conclusive experimental or theoretical evidence for drug interactions between TDF–FTC with transgender hormones including estradiol, progestins, or spironolactone. However, none of these medications are implicated as major perpetrators of drug interactions, and the classes use different metabolic pathways for clearance, suggesting a low theoretical likelihood for interactions in either direction (ie, effects on hormones or TDF–FTC). Importantly, iPrEx subanalyses of transgender individuals suggested PrEP efficacy if adherence is high. Thus, PrEP should continue to be offered to transgender women, even if additional research is planned or pending.
Nevertheless, several important research gaps were identified including the need for controlled drug interaction studies for these medications in transgendered women, including effects on renal clearances, intracellular TFV-DP and FTC-TP (and dNTP) systemically or in relevant tissues, as well as hormone effects on HIV susceptibility and immunity. Some of these are challenging questions, which could benefit from innovative strategies such as quantitative systems pharmacology modeling.
In conclusion, despite low theoretical concerns for major interactions between TDF–FTC and hormones, research is needed to provide informed guidance for PrEP use in transgendered women who are disproportionately impacted by HIV.
Footnotes
Supported by Grants from the NIH: K23 AI104315 (J.C.-M), U01 AI106499 (P.A.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health.
P.A. receives study drug, research funding, and contract work from Gilead Sciences, paid to his institution. The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Baral SD, Poteat T, Strömdahl S, et al. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:214–222. [DOI] [PubMed] [Google Scholar]
- 2.Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12:1–17. [DOI] [PubMed] [Google Scholar]
- 3.Clements-Nolle K, Marx R, Guzman R, et al. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: implications for public health intervention. Am J Public Health. 2001;91:915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grant RM, Anderson PL, McMahan V, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14:820–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367:399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367:423–434. [DOI] [PubMed] [Google Scholar]
- 8.Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381:2083–2090. [DOI] [PubMed] [Google Scholar]
- 9.Marrazzo JM, Ramjee G, Richardson BA, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2015;372:509–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Damme L, Corneli A, Ahmed K, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367:411–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Center for Innovative in HIV Care. Transgender Women and Pre-exposure Prophylaxis for HIV Prevention: What We Know and What We Still Need to Know. Available at: https://careacttarget.org/sites/default/files/file-upload/resources/PrEP%20and%20Transgender%20Women%20NCIHC%20Brief.pdf2015. Accessed May 31, 2016. [Google Scholar]
- 12.Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2009;94:3132–3154. [DOI] [PubMed] [Google Scholar]
- 13.The World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People. 7th ed Available at: http://www.wpath.org/uploaded_files/140/files/Standards%20of%20Care,%20V7%20Full%20Book.pdf2012. Accessed May 31, 2016. [Google Scholar]
- 14.Liu AY, Cohen SE, Vittinghoff E, et al. Preexposure prophylaxis for HIV infection integrated with municipal- and community-based sexual health services. JAMA Inter Med. 2016;176:75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237–2246. [DOI] [PubMed] [Google Scholar]
- 16.McCormack S, Dunn DT, Desai M, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387:53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson PL, Glidden DV, Liu A, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4:151ra125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deutsch MB, Glidden DV, Sevelius J, et al. HIV pre-exposure prophylaxis in transgender women: a subgroup analysis of the iPrEx trial. Lancet HIV. 2015;2:e512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Castillo-Mancilla JR, Zheng JH, Rower JE, et al. Tenofovir, emtricitabine, and tenofovir diphosphate in dried blood spots for determining recent and cumulative drug exposure. AIDS Res Hum Retroviruses. 2013;29:384–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson PL, Kiser JJ, Gardner EM, et al. Pharmacological considerations for tenofovir and emtricitabine to prevent HIV infection. J Antimicrob Chemother. 2011;66:240–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lade JM, To EE, Hendrix CW, et al. Discovery of genetic variants of the kinases that activate tenofovir in a compartment-specific manner. EBioMedicine. 2015;2:1145–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reznicek J, Ceckova M, Cerveny L, et al. Emtricitabine is a substrate of MATE1 but not of OCT1, OCT2, P-gp, BCRP or MRP2 transporters. Xenobiotica. 2016:1–9. [DOI] [PubMed] [Google Scholar]
- 23.Alam C, Whyte-Allman SK, Omeragic A, et al. Role and modulation of drug transporters in HIV-1 therapy. Adv Drug Deliv Rev. 2016. [DOI] [PubMed] [Google Scholar]
- 24.Deville-Bonne D, El Amri C, Meyer P, et al. Human and viral nucleoside/nucleotide kinases involved in antiviral drug activation: structural and catalytic properties. Antivir Res. 2010;86:101–120. [DOI] [PubMed] [Google Scholar]
- 25.Pushpakom SP, Liptrott NJ, Rodríguez-Nóvoa S, et al. Genetic variants of ABCC10, a novel tenofovir transporter, are associated with kidney tubular dysfunction. J Infect Dis. 2011;204:145–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tweedie D, Polli JW, Berglund EG, et al. Transporter studies in drug development: experience to date and follow-up on decision trees from the International Transporter Consortium. Clin Pharmacol Ther. 2013;94:113–125. [DOI] [PubMed] [Google Scholar]
- 27.Shen Z, Fahey JV, Bodwell JE, et al. Sex hormones regulate tenofovir-diphosphate in female reproductive tract cells in culture. PLoS One. 2014;9:e100863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.James AM, King JR, Ofotokun I, et al. Uptake of tenofovir and emtricitabine into non-monocytic female genital tract cells with and without hormonal contraceptives. J Exp Pharmacol. 2013;5:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anderson PL, King T, Zheng JH, et al. Cytokine and sex hormone effects on zidovudine- and lamivudine-triphosphate concentrations in vitro. J Antimicrob Chemother. 2008;62:738–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nicol MR, Fedoriw Y, Mathews M, et al. Expression of six drug transporters in vaginal, cervical, and colorectal tissues: implications for drug disposition in HIV prevention. J Clin Pharmacol. 2014;54:574–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anderson PL. Recent developments in the clinical pharmacology of anti-HIV nucleoside analogs. Curr Opin HIV AIDS. 2008;3:258–265. [DOI] [PubMed] [Google Scholar]
- 32.Moss DM, Marzolini C, Rajoli RK, et al. Applications of physiologically based pharmacokinetic modeling for the optimization of anti-infective therapies. Expert Opin Drug Metab Toxicol. 2015;11:1203–1217. [DOI] [PubMed] [Google Scholar]
- 33.Duwal S, Schutte C, von Kleist M. Pharmacokinetics and pharmacodynamics of the reverse transcriptase inhibitor tenofovir and prophylactic efficacy against HIV-1 infection. PLoS ONE. 2012;7:e40382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gilead Sciences. Truvada (tenofovir disoproxil fumarate and emtricitabine), Product Information. Gilead Sciences, Foster City, CA; 2016. [Google Scholar]
- 35.FDA. Drug development and drug interactions: table of substrates, inhibitors and inducers. Available at: http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/DrugInteractionsLabeling/ucm093664.htm. Accessed May 31, 2016.
- 36.Polasek TM, Lin FP, Miners JO, et al. Perpetrators of pharmacokinetic drug-drug interactions arising from altered cytochrome P450 activity: a criteria-based assessment. Br J Clin Pharmacol. 2011;71:727–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kearney BP, Mathias A. Lack of effect of tenofovir disoproxil fumarate on pharmacokinetics of hormonal contraceptives. Pharmacotherapy. 2009;29:924–929. [DOI] [PubMed] [Google Scholar]
- 38.de Ronde W, Pols HA, van Leeuwen JP, et al. The importance of oestrogens in males. Clin Endocrinol (Oxf). 2003;58:529–542. [DOI] [PubMed] [Google Scholar]
- 39.Stanczyk FZ, Archer DF, Bhavnani BR. Ethinyl estradiol and 17beta-estradiol in combined oral contraceptives: pharmacokinetics, pharmacodynamics and risk assessment. Contraception. 2013;87:706–727. [DOI] [PubMed] [Google Scholar]
- 40.Meriggiola MC, Berra M. Safety of hormonal treatment in transgenders. Curr Opin Endocrinol Diabetes Obes. 2013;20:565–569. [DOI] [PubMed] [Google Scholar]
- 41.Quest Diagnostics. Estradiol. Available at: http://www.questdiagnostics.com/testcenter/TestDetail.action?ntc=36169. Accessed May 31, 2016. [Google Scholar]
- 42.Düsterberg B, Nishino Y. Pharmacokinetic and pharmacological features of oestradiol valerate. Maturitas. 1982;4:315–324. [DOI] [PubMed] [Google Scholar]
- 43.Cui Y, Konig J, Buchholz JK, et al. Drug resistance and ATP-dependent conjugate transport mediated by the apical multidrug resistance protein, MRP2, permanently expressed in human and canine cells. Mol Pharmacol. 1999;55:929–937. [PubMed] [Google Scholar]
- 44.The International Transporter Consortium. Membrane transporters in drug development. Nat Rev Drug Discov. 2010;9:215–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morrison CS, Chen PL, Kwok C, et al. Hormonal contraception and the risk of HIV acquisition: an individual participant data meta-analysis. Plos Med. 2015;12:e1001778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vishwanathan SA, Guenthner PC, Lin CY, et al. High susceptibility to repeated, low-dose, vaginal SHIV exposure late in the luteal phase of the menstrual cycle of pigtail macaques. J Acquir Immune Defic Syndr. 2011;57:261–264. [DOI] [PubMed] [Google Scholar]
- 47.Chandra N, Thurman AR, Anderson S, et al. Depot medroxyprogesterone acetate increases immune cell numbers and activation markers in human vaginal mucosal tissues. AIDS Res Hum Retroviruses. 2013;29:592–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goode D, Aravantinou M, Jarl S, et al. Sex hormones selectively impact the endocervical mucosal microenvironment: implications for HIV transmission. PLoS One. 2014;9:e97767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ziegler S, Altfeld M. Sex differences in HIV-1-mediated immunopathology. Curr Opin HIV AIDS. 2016;11:209–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Heffron R, Mugo N, Were E, et al. Preexposure prophylaxis is efficacious for HIV-1 prevention among women using depot medroxyprogesterone acetate for contraception. AIDS. 2014;28:2771–2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Radzio J, Hanley K, Mitchell J, et al. Depot-medroxyprogesterone acetate does not reduce the prophylactic efficacy of emtricitabine and tenofovir disoproxil fumarate in macaques. J Acquir Immune Defic Syndr. 2014;67:365–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kobayashi K, Mimura N, Fujii H, et al. Role of human cytochrome P450 3A4 in metabolism of medroxyprogesterone acetate. Clin Cancer Res. 2000;6:3297–3303. [PubMed] [Google Scholar]
- 53.Lindenmaier H, Becker M, Haefeli WE, et al. Interaction of progestins with the human multidrug resistance-associated protein 2 (MRP2). Drug Metab Dispos. 2005;33:1576–1579. [DOI] [PubMed] [Google Scholar]
- 54.Burns RN, Hendrix CW, Chaturvedula A. Population pharmacokinetics of tenofovir and tenofovir-diphosphate in healthy women. J Clin Pharmacol. 2015;55:629–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Coleman J, Chaturvedula A, Hendrix C. Method of hormonal contraception is associated with lower tenofovir concentration in healthy women (MTN-001): implications for pre-exposure prophylaxis [FRLBC03]. Presented at the XIX International AIDS Conference, July 22–27, 2012, Washington DC.
- 56.Sica DA. Pharmacokinetics and pharmacodynamics of mineralocorticoid blocking agents and their effects on potassium homeostasis. Heart Fail Rev. 2005;10:23–29. [DOI] [PubMed] [Google Scholar]
- 57.G.D. Searle. Aldactone Product Information. New York, NY: G.D. Searle; 2008. [Google Scholar]
- 58.Rigalli JP, Ruiz ML, Perdomo VG, et al. Pregnane X receptor mediates the induction of P-glycoprotein by spironolactone in HepG2 cells. Toxicol. 2011;285:18–24. [DOI] [PubMed] [Google Scholar]
- 59.Homeida M, Roberts C, Branch RA. Influence of probenecid and spironolactone on furosemide kinetics and dynamics in man. Clin Pharmacol Ther. 1977;22:402–409. [DOI] [PubMed] [Google Scholar]


