Abstract
The nuclear factor-κB protein c-Rel plays a critical role in controlling autoimmunity. c-Rel–deficient mice are resistant to streptozotocin-induced diabetes, a drug-induced model of autoimmune diabetes. We generated c-Rel–deficient NOD mice to examine the role of c-Rel in the development of spontaneous autoimmune diabetes. We found that both CD4+ and CD8+ T cells from c-Rel–deficient NOD mice showed significantly decreased T-cell receptor–induced IL-2, IFN-γ, and GM-CSF expression. Despite compromised T-cell function, c-Rel deficiency dramatically accelerated insulitis and hyperglycemia in NOD mice along with a substantial reduction in T-regulatory (Treg) cell numbers. Supplementation of isogenic c-Rel–competent Treg cells from prediabetic NOD mice reversed the accelerated diabetes development in c-Rel–deficient NOD mice. The results suggest that c-Rel–dependent Treg cell function is critical in suppressing early-onset autoimmune diabetogenesis in NOD mice. This study provides a novel natural system to study autoimmune diabetes pathogenesis and reveals a previously unknown c-Rel–dependent mechanistic difference between chemically induced and spontaneous diabetogenesis. The study also reveals a unique protective role of c-Rel in autoimmune diabetes, which is distinct from other T-cell–dependent autoimmune diseases such as arthritis and experimental autoimmune encephalomyelitis, where c-Rel promotes autoimmunity.
Introduction
Type 1 diabetes is an autoimmune disorder in which the immune system is self-reactive and destroys the insulin-producing β-cells in the pancreas (1,2). It leads to hyperglycemia and severe secondary complications from chronic inflammation that lead to blindness, renal failure, nerve damage, and cardiovascular dysfunction (3). Although high blood glucose can be controlled by pharmacologic administration of insulin, there is no cure for type 1 diabetes (1). T lymphocytes play key roles in autoimmune diabetes pathogenesis in humans and rodent models. CD4+ T cells produce cytokines such as interleukin-2 (IL-2), interferon-γ (IFN-γ), and granulocyte macrophage colony-stimulating factor (GM-CSF) as well as promote the cytotoxic activity of CD8+ T cells, whereas T-regulatory (Treg) cells suppress autoimmunity (2,4–6). The balance between T cells and Treg cells with opposing functions controls the outcome of self-reactivity (7). Many functions of T lymphocytes are controlled by transcription factors such as nuclear factor-κB (NF-κB) and nuclear factor of activated T cells (NFAT) (8–10). However, the specific roles of various components of these transcription factors in autoimmunity are not well understood.
NF-κB is an evolutionarily conserved, dimeric transcription factor family comprising five members (RelA, RelB, c-Rel, p105/p50, and p100/p52) (11). Diverse extracellular and intracellular stimuli activate NF-κB–dependent transcription and expression of gene products (11), which play a central role in regulating several autoimmune and inflammatory disorders, including autoimmune type 1 diabetes, type 2 diabetes, obesity, lupus, arthritis, and celiac disease (12–16). Although NF-κB function has been implicated in autoimmunity and type 1 diabetes, a physiologically relevant mouse model to study the roles of NF-κB subunits in autoimmune diabetes has not yet been described.
NF-κB REL gene and c-Rel protein function is important in several autoimmune diseases, such as arthritis, celiac disease, psoriasis, and autoimmune encephalomyelitis (16). c-Rel is critical for T-helper 1 (Th1) cell differentiation in a model of autoimmune encephalomyelitis (17), and c-Rel deficiency causes resistance in an experimental model of this disease (18). Deficiency of c-Rel also confers resistance to autoimmunity resulting from mutations in Fas ligand (19) as well as collagen-induced arthritis (20). Furthermore, loss of c-Rel results in resistance to streptozotocin-induced diabetes, a mouse model of autoimmune diabetes (21). On the other hand, c-Rel is critical for the development of FOXP3-positive Treg cells, which suppress the activity of self-reactive T cells and autoimmunity (22,23).
The NOD mouse is a well-recognized model of human type 1 diabetes and has provided valuable insights into the pathogenesis and molecular mechanisms involved in autoimmune diabetes (24). These animals spontaneously develop lymphocytic infiltrates in pancreatic β-cells (insulitis) as early as 4 weeks of age, which can lead to destruction of insulin-producing β-cells and overt hyperglycemia starting as early as 12 weeks of age. NOD mice develop many aberrant immunophenotypes, such as functionally defective T cells, impaired development of Treg cells, poor antigen-presenting cell function, and defective cytokine production, all of which could be associated with NF-κB c-Rel functions (7,16). c-Rel is the major regulator of T-cell function that mediates autoimmunity and development of Treg cells that suppress autoimmunity. We tested the role of c-Rel in a spontaneous model of autoimmune diabetes by its deletion from NOD mice. Because c-Rel deficiency confers resistance to autoimmunity (16,17,20,21), we hypothesized that c-Rel deletion from NOD mice will 1) ameliorate autoimmune complications and 2) shed light onto some critical regulatory mechanisms associated with autoimmunity in NOD mice. We report that the absence of c-Rel, counter to expectation, accelerates diabetogenesis in NOD mice. We also found that the accelerated incidence of diabetes was attributable to the loss of Treg cell–mediated immunosuppression.
Research Design and Methods
Western Blotting
Thymus, spleen, and lungs were isolated from C57BL/6, B6.c-Rel−/−, NOD, and NOD.c-Rel−/− mice at 6–8 weeks of age. Red blood cells were lysed, and whole-cell lysates were prepared and analyzed by Western blotting as previously described (25).
Quantitative Real-Time PCR
Cells were stimulated at various time points with plate-bound anti-CD3 and anti-CD28 (2 μg/mL each) antibodies. Quantitative real-time PCR using TaqMan Gene Expression Assays (Applied Biosystems, Foster City, CA) was performed as previously described (26). The results obtained for individual genes were normalized to the expression of UBE2D2.
Treg Cell Supplementation
Congenic FOXP3-IRES-GFP NOD mice expressing green fluorescent protein (GFP) in their Treg cells were sacrificed at 6–10 weeks of age. Spleen and lymph nodes were harvested, red blood cells were lysed, and GFP-positive Treg cells were isolated by FACS using a MoFlo XDP cell sorter with a 488-nm laser and detected using a 530/40 fluorescein isothiocyanate filter. Cells were washed and suspended at 200,000 cells in 150 μL PBS and injected into c-Rel–deficient NOD mice.
Statistical Analysis
Differences in gene expression were analyzed using two-tailed unpaired Student t test with Prism software (GraphPad, La Jolla, CA). Data are presented as mean ± SEM. P < 0.05 was considered significant unless otherwise indicated. The percentage of diabetes in mice was statistically analyzed by a log-rank test in Prism.
Results
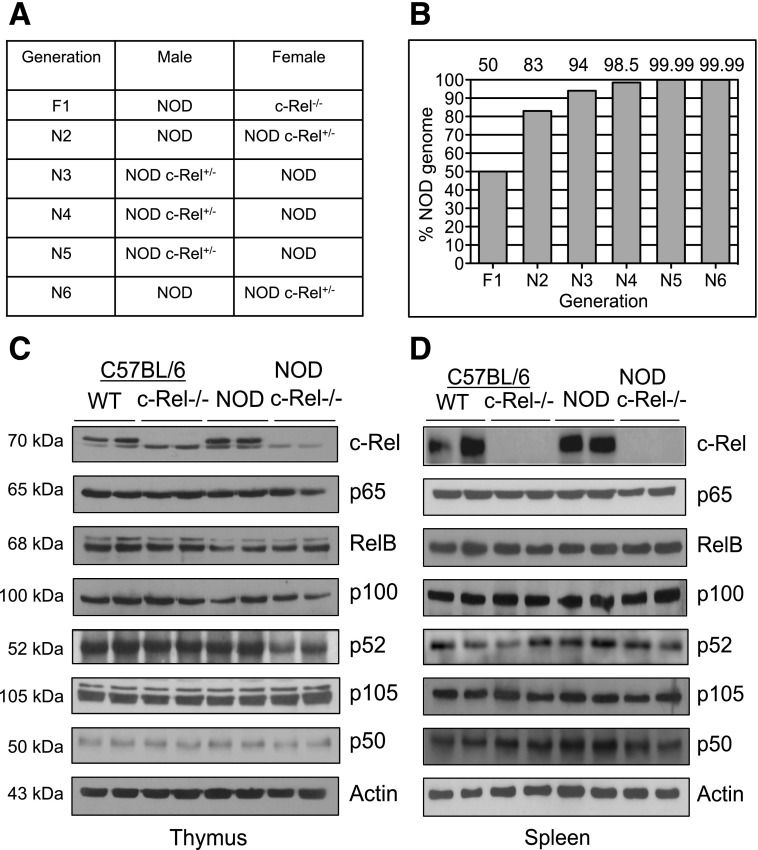
Expression of NF-κB Proteins in c-Rel–Deficient NOD Mice
To study the role of c-Rel in spontaneous diabetogenesis in NOD mice, we generated c-Rel knockout mice on the NOD background by using a marker-assisted speed congenic approach (Fig. 1A and B) (27). We analyzed the expression of NF-κB protein subunits by Western blotting in wild-type and c-Rel–deficient C57BL/6 mice and NOD mice to 1) confirm the absence of c-Rel and 2) examine whether c-Rel deficiency affects the expression of other NF-κB subunits. We analyzed cells from two lymphoid compartments, thymus (Fig. 1C) and spleen (Fig. 1D), as well as a nonlymphoid compartment, lungs (Supplementary Fig. 1A). As expected, c-Rel was absent in c-Rel–deficient mice, whereas the expression of other NF-κB subunits, p65, RelB, p105/p50, and p100/p52, were comparable in spleen and lungs of control and c-Rel–deficient NOD mice. Analysis of thymic NF-κB proteins showed a modest decrease in the p52 subunit levels in c-Rel–deficient NOD mice, whereas no change in the level of its precursor, p100, was observed (Fig. 1C and Supplementary Fig. 1B).
Figure 1.
Generation of c-Rel–deficient NOD mice. A: c-Rel knockout mice in C57BL/6 background were mated with NOD mice, and the heterozygotes obtained were mated with NOD mice in six successive generations as indicated in the table. B: Up to 15 mice from each generation were assessed by genome scanning to identify the percent incorporation of NOD genome. Shown is the highest percentage of NOD genome obtained in each generation. C and D: Expression of NF-κB family members in thymus and spleen of c-Rel–deficient C57BL/6 and NOD mice. Total cell lysates of thymus (C) and spleen (D) of 6–8-week-old mice were prepared and 20–30 μg of protein probed as indicated. Two representative samples for each strain are shown from four or more mice per strain. Normalized protein levels were confirmed by β-actin staining.
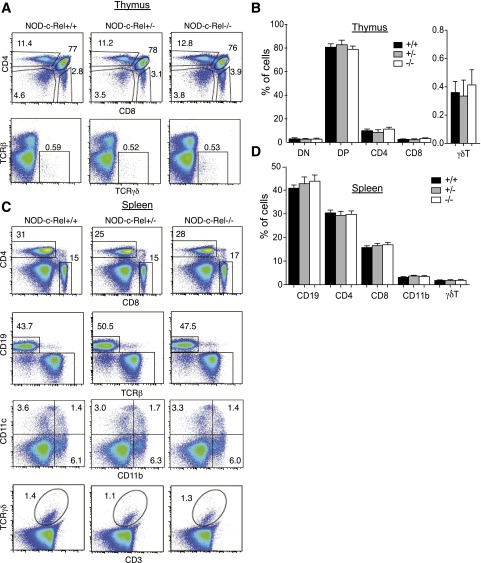
c-Rel Deficiency Does Not Affect the Development of Major Hematopoietic Cells in NOD Mice
To examine whether c-Rel deficiency affects development or survival of major cell populations of hematopoietic origin, we analyzed lymphoid and myeloid cells from 6–8-week-old prediabetic, normoglycemic, NOD c-Rel+/+, NOD c-Rel+/−, and NOD c-Rel−/− mice. We did not observe significant differences in the numbers (Fig. 2A) or proportions (Fig. 2B) of CD4+ CD8+ double-positive, CD4− CD8− double-negative, CD4+ or CD8+ single-positive, or T-cell receptor (TCR) (γδ)–positive T-cell populations in the thymus. Furthermore, no differences were found in the numbers (Fig. 2C) or percentages (Fig. 2D) of CD4+, CD8+ αβT cells; CD19+ B cells; CD11b+ and/or CD11c+ myeloid/dendritic cells; or γδTCR-positive T cells in the spleen. These results show that the development of these major hematopoietic subsets is not altered on the c-Rel–deficient NOD background.
Figure 2.
Major hematopoietic cell populations in NOD mice are not affected by c-Rel deficiency. Flow cytometric analysis of hematopoietic populations in thymus (A and B) and spleen (C and D) comparing NOD c-Rel+/+, heterozygous NOD c-Rel+/−, and homozygous NOD c-Rel−/− mice. A: Representative plots of CD4 vs. CD8 and TCRβ vs. TCRγδ from three independent experiments for thymocytes. B. Histogram summary of three experiments with percentages (mean ± SEM) for double-negative (DN), double-positive (DP), CD4, and CD8 single-positive subsets as well as γδT cells, showing normal distributions of thymocytes in all three mouse genotypes. C: Representative plots of CD4 vs. CD8, CD19 vs. TCRβ, CD11c vs. CD11b (gated on CD19− cells), and TCRγδ vs. CD3, for splenocytes. D: Histogram summary of three experiments with percentages (mean ± SEM) for CD19+ B cells, CD4+, CD8+, and γδT cells as well as CD11b+ myeloid cells, showing normal distributions of cells in all three mouse genotypes. FACS plots are representative of three experiments, and bar graphs represent the average of three mice per genotype.
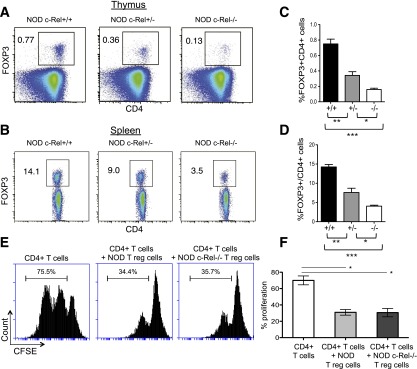
c-Rel Deficiency Selectively Decreases Treg Cell Numbers in NOD Mice
c-Rel is crucial for the expression of Treg cell–specific transcription factor FOXP3 and the development of Treg cells in C57BL/6 mice (22,23,28). Consistent with this, the present c-Rel–deficient NOD mice showed >80% and >75% reduction in FOXP3-positive CD4+ Treg cells in the thymus (Fig. 3A) and spleen (Fig. 3B), respectively, with the heterozygote showing intermediate percentages of FOXP3-positive cells in both cases. The differences in proportion of FOXP3-positive cells in NOD mice compared with that in c-Rel–deficient NOD mice for both thymus (Fig. 3C) and spleen (Fig. 3D) were found to be highly significant (P < 0.0001). We also found that CD4+ CD25+ Treg cells isolated from c-Rel–competent NOD and c-Rel–deficient NOD mice exhibited similar suppressive ability on the proliferation of CD4+ T cells isolated from NOD mice (Fig. 3E and F). The data suggest that c-Rel deficiency does not compromise the suppressive function of Treg cells and that the residual Treg cells in NOD c-Rel−/− mice are fully functional.
Figure 3.
A and B: FOXP3 cells are differentially affected by the loss of one or two copies of c-Rel on the NOD background. Representative plots of surface CD4 vs. intracellular FOXP3 for thymocytes (A) and splenocytes (B). C and D: Histogram summary of four experiments showing the percentage of FOXP3+ CD4+ cells (mean ± SEM) in thymus (C) and the percentage of FOXP3+ cells among CD4+ cells in spleen (D) for each genotype. Results from t tests comparing each pair of genotypes for four mice from each group are as shown. E and F: c-Rel–deficient Treg cells are functionally competent in suppressing CD4+ T-cell proliferation in vitro. E: Flow cytometric analysis of carboxyfluorescein succinimidyl ester (CFSE) dilution in CD4+ T cells alone, with NOD Treg cells, and with NOD c-Rel−/− Treg cells. Histograms are representative of three mice per genotype from three experiments (F). Percentage of proliferating CD4+ T cells based on CFSE assay data. Bar graphs represent mean of duplicates from three mice per group. *P < 0.05, **P < 0.005, ***P < 0.0001.
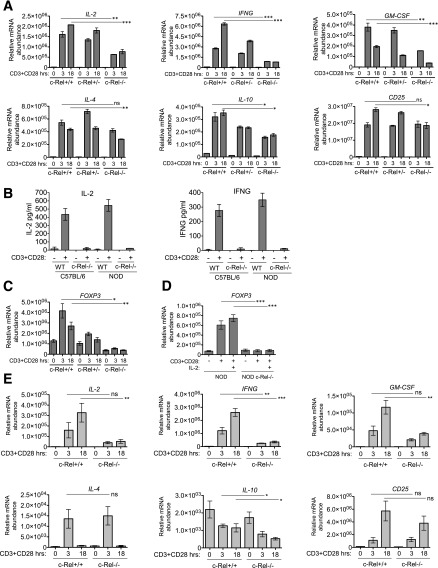
c-Rel Is Required for the Expression of Selected Cytokines and FOXP3 in T Cells of NOD Mice
c-Rel has been previously shown to be important for T-cell function and expression of several TCR-induced genes (16,29,30). We isolated CD4+ T cells from NOD c-Rel+/+, NOD c-Rel+/−, and NOD c-Rel−/− mice and studied TCR-induced gene expression following anti-CD3/CD28 costimulation. We found that T cells from NOD c-Rel−/− mice showed greatly decreased anti-CD3/CD28–induced expression of proautoimmune Th1 cytokines IL-2, IFN-γ, and GM-CSF (Fig. 4A). Genes such as IL-4 that are suggested to have a c-Rel binding site in their promoter regions (31), and IL-10, the expression of which was previously shown to be diminished in the absence of c-Rel (32), showed only a moderate decrease, suggesting that they only partially depend on c-Rel for their expression (Fig. 4A). As expected, expression of these genes in c-Rel heterozygote mice was intermediate between c-Rel wild-type and c-Rel–deficient T cells. c-Rel deficiency was found to have only minimal effects on the expression of other NF-κB–dependent genes, such as CD25 (Fig. 4A). We also analyzed the expression of IL-2 and IFN-γ by ELISA and found that the protein levels of both these cytokines were dramatically decreased in c-Rel–deficient C57BL/6 and NOD mice (Fig. 4B). Because the total CD4+ T-cell pool also contains CD4+ CD25+ Treg cells, we separated Treg cells from total CD4+ T cells and studied TCR-induced gene expression, exclusively in CD4+ CD25− T cells. We found that removal of Treg cells showed some differences, such as decreased early induction of IL-2, decreased sustained IL-4 production, and decreased basal level of CD25 in CD4+ CD25− T cells compared with that in total CD4+ T cells (Supplementary Fig. 2A).
Figure 4.
c-Rel deficiency decreases cytokine and FOXP3 expression in NOD mice. A: CD4+ T cells were purified from c-Rel+/+, c-Rel+/− and c-Rel−/− NOD mice by magnetic-activated cell sorting. Cells were stimulated with plate-bound anti-CD3 and anti-CD28 antibodies (2 μg/mL each) for the indicated time points. Gene expression was analyzed by real-time PCR from at least three mice per genotype in triplicate. B: Analysis of the expression of IL-2 and IFN-γ in culture supernatant by ELISA. CD4+ T cells from C57BL/6 and NOD mice were treated as in A for 18 h. Data are the mean of triplicates from three mice per group. C: Expression of FOXP3 was analyzed as in A in triplicate from three mice per group. D: CD4+ T cells were treated as in A, and the effect of exogenous IL-2 (50 units/mL) on FOXP3 expression was analyzed. Data are the mean of triplicates from three mice per genotype. E: CD8+ T cells were purified from c-Rel+/+ and c-Rel−/− NOD mice by magnetic-activated cell sorting. Cells were stimulated and gene expression analyzed by real-time PCR as in A from at least three mice in triplicate. Expression of indicated genes was normalized to UBE2D2. Data are mean ± SEM. Unpaired Student t test comparing gene expression in c-Rel+/+ and c-Rel−/− T cells. *P < 0.05, **P < 0.01, ***P < 0.001. IFNG, interferon-γ; ns, nonsignificant; WT, wild type.
Consistent with the decreased FOXP3 expression observed by intracellular staining (Fig. 3A and B), mRNA expression of FOXP3 was also greatly decreased in c-Rel–deficient CD4+ T cells (Fig. 4C). As previously shown, the function of c-Rel is critical for both IL-2 and FOXP3 expression (16). IL-2 has also been suggested to be required for the expression of FOXP3 as well as the development and survival of Treg cells (9,28,33). Therefore, we asked whether the decreased FOXP3 expression and Treg cell numbers in c-Rel–deficient mice result from decreased IL-2 production. We examined the TCR-induced FOXP3 expression in CD4+ T cells isolated from wild-type and c-Rel knockout C57BL/6 mice (Supplementary Fig. 2B) and parental NOD and c-Rel–deficient NOD mice (Fig. 4D) in the presence of exogenous IL-2. The addition of IL-2 did not increase the FOXP3 transcription in CD4+ T cells isolated from either strain, suggesting that the defect is indeed due to the absence of c-Rel and not due to the insufficiency of IL-2. Consistent with this, c-Rel has been shown to induce FOXP3 transcription directly by binding to the enhancer region of FOXP3 gene (22).
Because CD8+ T cells are the major cytotoxic force behind diabetogenic β-cell destruction, we also performed anti-CD3/CD28–induced gene expression studies by using CD8+ T cells. Similar to CD4+ T cells, c-Rel deficiency also compromised TCR-induced expression of IL-2, IFN-γ, and GM-CSF in CD8+ T cells (Fig. 4E, top panels). TCR-induced IL-4 and CD25 expression in CD8+ T cells did not show significant dependence on c-Rel. IL-10 was not induced by TCR activation in either NOD or NOD c-Rel−/− CD8 T cells, and its expression showed a decrease from basal levels after TCR activation (Fig. 4E, bottom panels).
c-Rel Deficiency Exacerbates Autoimmunity in NOD Mice
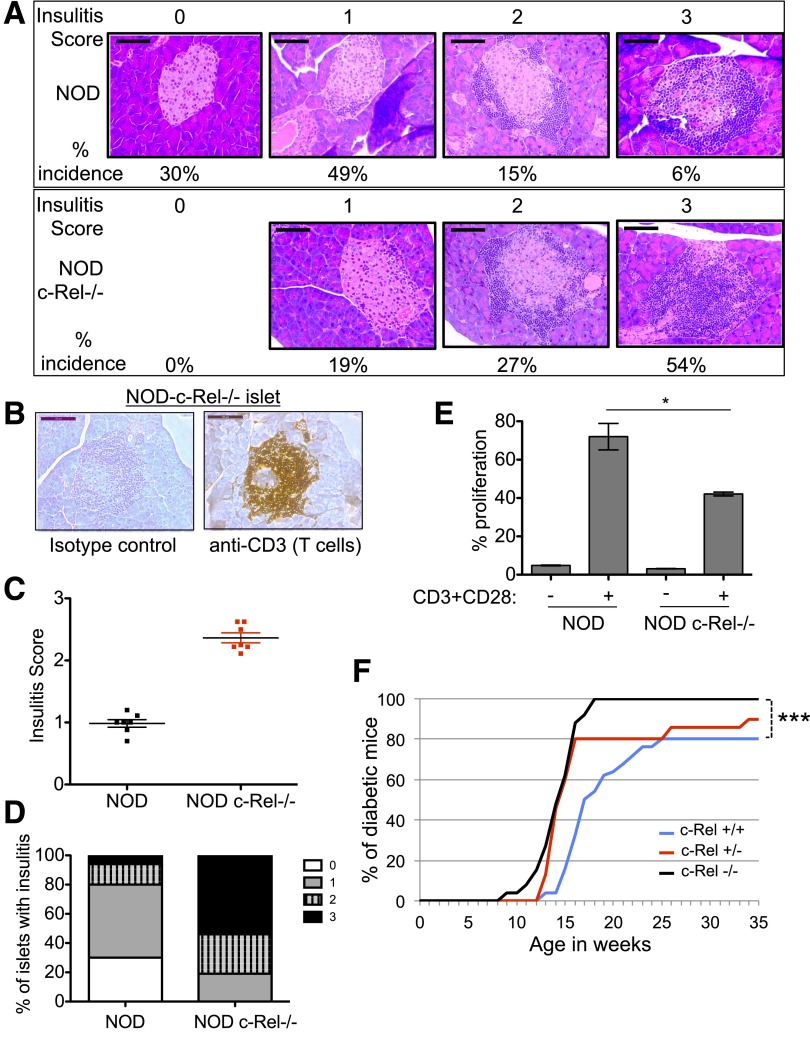
Overt hyperglycemia in NOD mice is preceded by infiltration of immune cells in the pancreas (insulitis) that mediates autoimmune destruction of the islets. We analyzed the pancreas of control and c-Rel–deficient prediabetic NOD mice of 8–9 weeks of age with a blood glucose level in the range of 80–120 mg/dL by hematoxylin and eosin staining. We found that the absence of c-Rel led to a dramatic increase in insulitis, suggesting a critical role of c-Rel in suppressing autoimmunity (Fig. 5A, percentages of insulitis score under respective images). The islets from c-Rel–deficient NOD pancreas were strongly stained with an anti-CD3 antibody, confirming that the infiltrating cells are predominantly T cells (Fig. 5B). We performed the scoring of insulitis as previously described (34), and the average insulitis score (Fig. 5C) and the percentage of islets showing infiltration (Fig. 5D) were calculated. Because c-Rel deficiency enhanced the T-cell infiltration in the islets, we studied whether these cells are hyperresponsive to T-cell activation. We found that CD4+ T cells from the spleens of c-Rel−/− NOD mice showed significantly decreased proliferative response in vitro compared with NOD mice after TCR costimulation (Fig. 5E).
Figure 5.
c-Rel deficiency accelerates insulitis and diabetes in NOD mice. A: Pancreata were isolated from 8–9-week-old prediabetic female NOD c-Rel+/+ (top) and c-Rel−/− (bottom) mice and analyzed by hematoxylin and eosin staining for insulitis. The histology shows islets representing insulitis scores of 0–3 and their percentage of incidence from NOD and NOD c-Rel−/− mice from >10 animals analyzed per group. B: T-cell infiltrates in the islets. Pancreas sections of NOD c-Rel−/− mice were stained using an anti-CD3 or isotype control antibodies. Scale bar = 100 μm. Data represent staining performed on pancreatic tissue sections from four mice for each genotype. C and D: Insulitis score and the percentage of islets with each grade of insulitis in NOD and c-Rel−/− NOD mice. C: Insulitis was scored from seven mice per genotype, and the mean score of individual mice was plotted. Scale: no infiltration = 0; peri-islet infiltration of <25% of islet = 1; invasive infiltration of 25–50% of the islet = 2; high infiltration of >50% of the islet = 3. The insulitis score was analyzed using ANOVA; P < 0.0001 (Prism). D: Percentage of islets with each grade of insulitis calculated from 63 c-Rel+/+ and 59 c-Rel−/− islets from 36 independent sections for each mouse, with a total of seven mice per group. E: TCR-induced proliferation of CD4+ T cells isolated from spleen of NOD and c-Rel−/− NOD mice. Data are mean of triplicates from two mice per genotype. *P < 0.05. F: c-Rel+/+ (n = 26), c-Rel+/− (n = 16), and c-Rel−/− (n = 27) NOD mice were analyzed weekly for blood glucose levels. Once the glucose level reached 250 mg/dL, the mice were monitored twice a week. Mice showing three consecutive readings of 250 mg/dL were marked as diabetic. Significant differences by log-rank test were seen between c-Rel+/+ and c-Rel−/− mice (***P < 0.001) and c-Rel+/+ and c-Rel+/− mice (*P < 0.05).
We then followed the development of diabetes in c-Rel−/− NOD mice compared with the c-Rel+/− heterozygote and c-Rel+/+ NOD mice. Consistent with the increase in prediabetes insulitis, we found that diabetogenesis was also accelerated in c-Rel–deficient NOD mice. Unlike the NOD female mice, which showed ∼80% diabetes occurrence by 25 weeks of age, 100% of c-Rel–deficient and 80% of the c-Rel+/− NOD female mice were diabetic by 17 weeks of age (Fig. 5F).
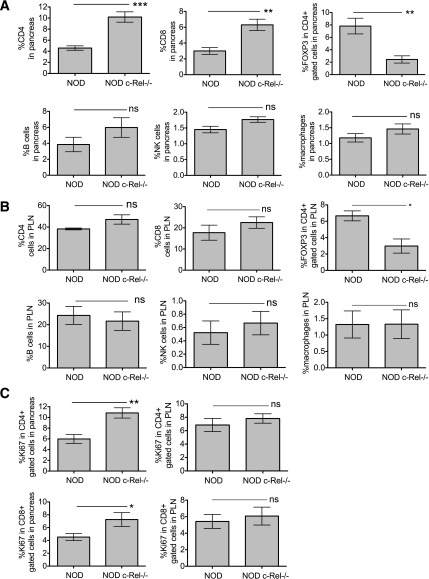
c-Rel Deficiency Increases CD4+ T-Cell Proliferation in the Pancreas
To further understand the mechanistic basis of accelerated diabetes development in NOD c-Rel−/− mice, we examined the extent of immune cell infiltration and proliferation of T cells among total cells in the pancreas and pancreatic lymph nodes of NOD and NOD c-Rel−/− mice. We found that the percentages of CD4+ and CD8+ T cells were significantly increased by 2.5- and 2.0-fold, whereas the percentage of Treg cells was found to be decreased by 75% in the pancreas of NOD c-Rel−/− mice (Fig. 6A, top panels). Their percentages of B cells, natural killer (NK) cells, and macrophages showed only a modest increase and were statistically not significant (Fig. 6A, bottom panels). Thus, similar to the increased insulitis and T-cell infiltration observed in histological analyses in 8–9-week-old mice (Fig. 5A and B), flow cytometry analyses using 6–8-week-old mice showed a trend of increased infiltration of T cells in the pancreas (Fig. 6A). We also examined the pancreatic lymph nodes of NOD and NOD c-Rel−/− mice and found no significant differences in the percentages of CD4+ and CD8+ T cells, B cells, NK cells, or macrophages, whereas the number of Treg cells was decreased by 70% (Fig. 6B). Next, we studied the proliferation of CD4+ and CD8+ T cells by Ki67 staining and found that the percentage of proliferating CD4+ T cells was significantly higher in the pancreas but not in the pancreatic lymph nodes (Fig. 6C, top panels). We also found an increase in proliferating CD8+ T cells but to a lesser extent than that of CD4+ T cells (Fig. 6C, bottom panels). Although the TCR-induced in vitro proliferative capacity of c-Rel–deficient CD4+ T cells was reduced (Fig. 5E), the in vivo proliferation within the pancreas was significantly increased, suggesting that the paucity of Treg cells in both pancreas and pancreatic lymph nodes allows enhanced proliferation of CD4+ T cells in the pancreas.
Figure 6.
A and B: c-Rel deficiency significantly increases the number of CD4+ and CD8+ T cells and decreases Treg cells in the pancreas. Pancreata (A) and pancreatic lymph nodes (PLNs) (B) were isolated from 6–8-week-old prediabetic female NOD and NOD c-Rel−/− mice. Single-cell suspensions were analyzed by flow cytometry for CD4+ and CD8+ T cells, FOXP3+ Treg cells, B cells, NK cells, and macrophages. For the entire staining, single-cell isolates from pancreas and PLNs were prepared as described in the Supplementary Data. Live cells were gated first, and percentage of cell populations of interest among the total cells in the pancreas and PLNs were determined. C: c-Rel deficiency increases proliferation of CD4+ T cells in the pancreas as assessed by the costaining of surface CD4 and intracellular staining of the proliferation marker Ki67. Data are mean ± SEM of seven mice for pancreas and five mice for PLN per group. *P < 0.05, **P < 0.01, ***P < 0.001. ns, nonsignificant.
Supplementation of c-Rel–Competent Treg Cells Reverts the Accelerated Diabetes in c-Rel–Deficient NOD Mice
Because the paucity of Treg cells in pancreas and pancreatic lymph nodes (Fig. 6A and B) might prove to be the underlying reason for the enhanced CD4+ T-cell proliferation and accelerated diabetogenesis in NOD c-Rel−/− mice, our next aim was to address whether supplementation with c-Rel–competent Treg cells could reverse their aggravated autoimmunity. To accomplish this, we used congenic FOXP3-IRES-GFP NOD mice that express GFP in Treg cells. Analysis of spleen (Supplementary Fig. 3A) and lymph nodes (Supplementary Fig. 3B) from these mice showed 2.1% and 5.6% of GFP-positive Treg cells, respectively. We isolated these GFP-positive Treg cells by FACS and retro-orbitally injected 6–8-week-old NOD c-Rel−/− mice with 2 × 105 GFP-positive cells/mouse in PBS. We found that supplemented GFP-positive Treg cells were present in the pancreata (Fig. 7A, left) and pancreatic lymph nodes (Fig. 7A, right) in NOD c-Rel−/− mice 5 weeks postreconstitution. We scored the pancreata for insulitis (Fig. 5C and D) and calculated the average insulitis score (Fig. 7B) and the percentage of islets showing infiltration (Fig. 7C). We found that supplemented Treg cells reversed the severity of insulitis in NOD c-Rel−/− mice. Next, we reconstituted 12 NOD c-Rel−/− recipient mice and confirmed the presence of circulating GFP-positive Treg cells in their blood (Fig. 7D). While all the c-Rel–deficient NOD mice showed hyperglycemia by 18 weeks of age, only 50% of animals supplemented with the GFP-positive Treg cells developed hyperglycemia at this stage. We continued to collect the data to 35 weeks and found that Treg cell supplementation reversed the enhanced pathology of diabetes caused by c-Rel deficiency, although it did not protect the mice from developing diabetes (Fig. 7E).
Figure 7.
Supplementation of c-Rel–competent Treg cells reverts exacerbated diabetes in c-Rel−/− NOD mice. A: Presence of transplanted Treg cells in pancreas (left) and pancreatic lymph node (right). FACS plot represents the flow cytometry performed using the organs from three mice each per group, 5 weeks postsupplementation of GFP-positive Treg cells. B: Insulitis scores at 5 weeks postsupplementation of GFP-positive Treg cells from four individual mice per group and the mean score ± SEM are plotted. C: Percentage of islets with each grade of insulitis calculated from 38 c-Rel−/− and 35 GFP-positive Treg-supplemented c-Rel−/− islets from 15 independent sections for each mouse from four mice per group (P < 0.001). D: Presence of transplanted Treg cells examined by tail vein bleeding and flow cytometry for GFP-positive cells in blood 10 weeks postsupplementation in 11 NOD and 12 NOD c-Rel−/− mice. E: c-Rel+/+ (n = 11), c-Rel−/− (n = 12), and c-Rel−/− + GFP-positive Treg (n = 12) NOD mice were analyzed for blood glucose levels as described in Fig. 5F. Significant differences by log-rank test were seen between c-Rel+/+ and c-Rel−/− mice (***P < 0.001) as well as between c-Rel+/+ and c-Rel−/− + GFP-positive Treg reconstituted mice (***P < 0.001). SSC-A, side-scatter area.
Discussion
Autoimmunity results from a combined action of genetic, environmental, and immunological factors that lead to impaired central and/or peripheral immune tolerance. The etiology of type 1 diabetes is also associated with a shortfall of immune tolerance in which the immune system recognizes pancreatic islet cells as foreign and destroys them (35). However, the root cause that ignites the autoimmune response in diabetes remains enigmatic (1). NF-κB family members play substantial roles in regulating multiple aspects of immune responses and autoimmunity. Deficiency of RelB and NF-κB2 (p100/p52) results in enhanced autoimmunity (36,37), whereas the absence of c-Rel has been suggested to confer resistance to autoimmunity (16,17). Several abnormal immunophenotypes of NOD mice, such as autoreactivity of T cells, autoantibody production by B cells, defective antigen presentation, and abnormal proautoimmune and inflammatory cytokine production, could be associated with deregulated c-Rel function. c-Rel is critical for the function of Th1 cells, including induction of genes such as IL-2, IFN-γ and GM-CSF (29,30). c-Rel is also required for the induction of FOXP3 and the development of Treg cells (22,28). These Th1 and Treg cell functions play major and possibly opposing roles in autoimmune diabetes. In this study, we developed the novel c-Rel–deficient NOD mouse, which is a natural system to study how total loss of c-Rel affects diabetogenesis. Because c-Rel knockout mice are resistant to autoimmunity in general (16), we speculated that c-Rel deficiency might delay or prevent the autoimmune diabetogenesis in NOD mice. However, against expectation, the results show that the absence of c-Rel on the autoimmune NOD background did not prevent or delay autoimmunity. Rather, it resulted in an acceleration of insulitis and frequency of occurrence of type 1 diabetes associated with a paucity of immunosuppressive FOXP3-positive Treg cells.
c-Rel is a critical component of the IL-2 promoter–activating complex (38). However, IL-2 is induced by multiple pathways in T cells (39), and a minimal amount of IL-2 is produced even in the absence of c-Rel (30) (Fig. 4A). IL-2 has been implicated as a critical factor in autoimmunity (40), including type 1 diabetes in humans and NOD mice, playing complex roles in the balance between diabetes pathogenesis and protection by Treg cells (41), with Treg cells being particularly sensitive to reductions in IL-2 levels (42,43). However, the addition of exogenous IL-2 did not increase TCR-induced FOXP3 expression in c-Rel–deficient T cells, suggesting the requirement of c-Rel in transcriptional regulation of FOXP3.
Acceleration of disease despite a decrease in IL-2, IFN-γ, and GM-CSF production, both by CD4+ and CD8+ T cells, emphasizes the critical importance of Treg cells in suppressing autoimmunity in NOD mice. In agreement with this, Treg cells have been previously shown to play a critical role in suppressing the onset of autoimmune diabetes in NOD mice (44,45). Furthermore, restoration of diabetes progression in c-Rel–deficient NOD mice to a level similar to that in NOD mice after injection of c-Rel–competent NOD Treg cells shows that the absence of Treg cells are indeed responsible for the observed acceleration of disease.
Of note, in the current reconstitution studies with FOXP3-positive cells (Fig. 7), although the c-Rel–deficient NOD mice recovered from accelerated diabetes development, Treg cell supplementation was not sufficient to decrease diabetes beyond that seen in the c-Rel–competent NOD mice. Although it is possible that the number of Treg cells we injected was not sufficient to fully suppress the autoimmune response, restoration of normal disease kinetics is not necessarily surprising because wild-type NOD Treg cells are normally unable to prevent the development of type 1 diabetes in NOD mice. In addition, Treg cells appear to be less effective at regulating pathogenic T cells in later stages (46–48). Restoration of wild-type NOD disease progression with the injection of labeled wild-type NOD Treg cells also suggests that either the observed decrease in cytokine production and proliferation by c-Rel–deficient T cells observed in vitro has no effect on disease progression or alternative mechanisms that promote the disease are present within the T cells or other cells present in the NOD mice. In line with this possibility, the data show that T cells in the pancreas have enhanced proliferative capacity. The paucity of Treg cells in both pancreas and pancreatic lymph nodes may account for diminished suppression of autoreactive T cells in these compartments and enhanced proliferation of CD4+ and CD8+ T cells in the pancreas.
Because c-Rel is present in all hematopoietic cells and in pancreatic β-cells (16,23), altered NF-κB functions in those cells may play additional roles. The current detailed analysis of immune cells in pancreas and pancreatic lymph nodes suggests that c-Rel deficiency has only a modest effect on infiltration of B cells, NK cells, and macrophages into the pancreas. However, the overall modest increase in infiltrating immune cells suggests increased trafficking of immune cells into the pancreas of NOD c-Rel−/− mice. c-Rel and NF-κB, in general, play an antiapoptotic role in several cell types, including pancreatic β-cells (13,49). The absence of c-Rel may render β-cells of NOD mice prone to apoptosis by compromising expression of antiapoptotic molecules, such as Bcl-XL, Bcl-2, and A1 (16), which may contribute to the high incidence of diabetes in c-Rel−/− NOD mice. Concurring with this possibility, inhibition of NF-κB in pancreatic β-cells of NOD mice has been shown to accelerate autoimmune diabetes (50). We examined the serum insulin levels in prediabetic NOD and NOD c-Rel−/− mice to confirm that their β-cell function is intact. We found no significant difference in insulin secretion (Supplementary Fig. 3B), which suggests that c-Rel deficiency does not cause inherent defects in β-cells. Moreover, in our experiments, supplementation of Treg cells rescues the NOD c-Rel−/− animals from accelerated development of diabetes, and the blood glucose level becomes comparable to that in NOD mice, further suggesting that β-cells in c-Rel–deficient NOD mice do not have intrinsic defects that lead to their death and they behave similarly to those in NOD mice.
In a previous study of c-Rel and NF-κB1 (p105) knockout mice on the C57BL/6 background, these NF-κB subunits were suggested to play a role in susceptibility to diabetes (21). Both these knockout mice showed reduced levels of inflammatory cytokines and some degree of resistance to diabetes development after injection with the chemical streptozotocin. In contrast, c-Rel–deficient NOD mice, which may be a better model of the human disease, showed accelerated diabetes development, suggesting a difference in NF-κB c-Rel involvement in chemical-induced and spontaneous diabetogenesis.
In humans, the incidence of autoimmune diabetes is constantly rising, and the secondary complications of hyperglycemia are increasing. Because of its polygenic and varied nature, knowledge of the molecular mechanisms involved in the complications of type 1 diabetes is limited. We showed previously that hyperglycemia-induced O-GlcNAcylation activates c-Rel–dependent transcription. This results in enhanced production of Th1 cytokines that may culminate in exacerbation of autoimmunity in diabetes (26). The current novel c-Rel–deficient NOD mouse model can be used to 1) dissect the roles of c-Rel in various components of type 1 diabetes pathogenesis in the NOD mouse in both the prediabetic and the hyperglycemic state and 2) generate transgenic mice expressing non–O-GlcNAcylatable or other mutants of c-Rel to study the role of posttranslational modifications regulating c-Rel function in autoimmune diabetes. This is especially important because the current results suggest that inhibition of global c-Rel function may not prove to be a desirable strategy to treat autoimmune diabetes.
Article Information
Acknowledgments. The authors thank Hsiou-Chi Liou, Cornell University, for providing c-Rel knockout mice; Diane Mathis and Christophe Benoist, Harvard Medical School, for providing FOXP3-IRES-GFP mice; the California Institute of Technology and Case Western Reserve University animal facilities; Ni Feng, California Institute of Technology, for flow cytometry; and Daniel Kahn and Jevgenij Raskatov, California Institute of Technology, and Timothy Kern, Case Western Reserve University, for insightful discussions.
Funding. This work was initially supported by National Institute of General Medical Sciences grant 2R01-GM-039458 to D.B. and later by Mizutani Foundation for Glycoscience grant 120022, the Clinical and Translational Science Collaborative of Cleveland, grant CTSC UL1-TR-000439 from the National Center for Advancing Translational Sciences, and National Institute of Allergy and Infectious Diseases grant 1R01-AI-116730-01A1 to P.R. M.A.Y. was supported by National Institutes of Health grant AI-64590. J.A.T. was supported by an American Association of Immunologists (AAI) Careers in Immunology Fellowship to P.R.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. P.R. contributed to the study conception and design, data research, and writing of the manuscript. M.A.Y. contributed to the data research, discussion, and editing of the manuscript. J.A.T., D.M., and R.P. contributed to the data research. D.B. contributed to the data interpretation, discussion, and review and editing of the manuscript. P.R. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db15-1607/-/DC1.
References
- 1.Atkinson MA, Eisenbarth GS, Michels AW. Type 1 diabetes. Lancet 2014;383:69–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Castaño L, Eisenbarth GS. Type-I diabetes: a chronic autoimmune disease of human, mouse, and rat. Annu Rev Immunol 1990;8:647–679 [DOI] [PubMed] [Google Scholar]
- 3.Melendez-Ramirez LY, Richards RJ, Cefalu WT. Complications of type 1 diabetes. Endocrinol Metab Clin North Am 2010;39:625–640 [DOI] [PubMed] [Google Scholar]
- 4.Tsai S, Shameli A, Santamaria P. CD8+ T cells in type 1 diabetes. Adv Immunol 2008;100:79–124 [DOI] [PubMed] [Google Scholar]
- 5.Mallone R, van Endert P. T cells in the pathogenesis of type 1 diabetes. Curr Diab Rep 2008;8:101–106 [DOI] [PubMed] [Google Scholar]
- 6.Phillips JM, Parish NM, Raine T, et al. Type 1 diabetes development requires both CD4+ and CD8+ T cells and can be reversed by non-depleting antibodies targeting both T cell populations. Rev Diabet Stud 2009;6:97–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wållberg M, Cooke A. Immune mechanisms in type 1 diabetes. Trends Immunol 2013;34:583–591 [DOI] [PubMed] [Google Scholar]
- 8.Oh H, Ghosh S. NF-κB: roles and regulation in different CD4(+) T-cell subsets. Immunol Rev 2013;252:41–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hori S. c-Rel: a pioneer in directing regulatory T-cell lineage commitment? Eur J Immunol 2010;40:664–667 [DOI] [PubMed] [Google Scholar]
- 10.Macian F. NFAT proteins: key regulators of T-cell development and function. Nat Rev Immunol 2005;5:472–484 [DOI] [PubMed]
- 11.Baltimore D. NF-κB is 25. Nat Immunol 2011;12:683–685 [DOI] [PubMed] [Google Scholar]
- 12.Baker RG, Hayden MS, Ghosh S. NF-κB, inflammation, and metabolic disease. Cell Metab 2011;13:11–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao Y, Krishnamurthy B, Mollah ZU, Kay TW, Thomas HE. NF-κB in type 1 diabetes. Inflamm Allergy Drug Targets 2011;10:208–217 [DOI] [PubMed] [Google Scholar]
- 14.Ramakrishnan P, Kahn DA, Baltimore D. Anti-apoptotic effect of hyperglycemia can allow survival of potentially autoreactive T cells. Cell Death Differ 2011;18:690–699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol 2011;11:98–107 [DOI] [PubMed]
- 16.Gilmore TD, Gerondakis S. The c-Rel transcription factor in development and disease. Genes Cancer 2011;2:695–711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hilliard BA, Mason N, Xu L, et al. Critical roles of c-Rel in autoimmune inflammation and helper T cell differentiation. J Clin Invest 2002;110:843–850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen G, Hardy K, Bunting K, Daley S, Ma L, Shannon MF. Regulation of the IL-21 gene by the NF-κB transcription factor c-Rel. J Immunol 2010;185:2350–2359 [DOI] [PubMed] [Google Scholar]
- 19.O’Reilly LA, Hughes P, Lin A, et al. Loss of c-REL but not NF-κB2 prevents autoimmune disease driven by FasL mutation. Cell Death Differ 2015;22:767–778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campbell IK, Gerondakis S, O’Donnell K, Wicks IP. Distinct roles for the NF-kappaB1 (p50) and c-Rel transcription factors in inflammatory arthritis. J Clin Invest 2000;105:1799–1806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lamhamedi-Cherradi SE, Zheng S, Hilliard BA, et al. Transcriptional regulation of type I diabetes by NF-kappa B. J Immunol 2003;171:4886–4892 [DOI] [PubMed] [Google Scholar]
- 22.Long M, Park SG, Strickland I, Hayden MS, Ghosh S. Nuclear factor-kappaB modulates regulatory T cell development by directly regulating expression of Foxp3 transcription factor. Immunity 2009;31:921–931 [DOI] [PubMed] [Google Scholar]
- 23.Ruan Q, Kameswaran V, Tone Y, et al. Development of Foxp3(+) regulatory T cells is driven by the c-Rel enhanceosome. Immunity 2009;31:932–940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anderson MS, Bluestone JA. The NOD mouse: a model of immune dysregulation. Annu Rev Immunol 2005;23:447–485 [DOI] [PubMed] [Google Scholar]
- 25.Ramakrishnan P, Baltimore D. Sam68 is required for both NF-κB activation and apoptosis signaling by the TNF receptor. Mol Cell 2011;43:167–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramakrishnan P, Clark PM, Mason DE, Peters EC, Hsieh-Wilson LC, Baltimore D. Activation of the transcriptional function of the NF-κB protein c-Rel by O-GlcNAc glycosylation. Sci Signal 2013;6:ra75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wakeland E, Morel L, Achey K, Yui M, Longmate J. Speed congenics: a classic technique in the fast lane (relatively speaking). Immunol Today 1997;18:472–477 [DOI] [PubMed] [Google Scholar]
- 28.Isomura I, Palmer S, Grumont RJ, et al. c-Rel is required for the development of thymic Foxp3+ CD4 regulatory T cells [published correction appears in J Exp Med 2010;207:899]. J Exp Med 2009;206:3001–3014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Köntgen F, Grumont RJ, Strasser A, et al. Mice lacking the c-rel proto-oncogene exhibit defects in lymphocyte proliferation, humoral immunity, and interleukin-2 expression. Genes Dev 1995;9:1965–1977 [DOI] [PubMed] [Google Scholar]
- 30.Liou HC, Jin Z, Tumang J, Andjelic S, Smith KA, Liou ML. c-Rel is crucial for lymphocyte proliferation but dispensable for T cell effector function. Int Immunol 1999;11:361–371 [DOI] [PubMed] [Google Scholar]
- 31.Bunting K, Rao S, Hardy K, et al. Genome-wide analysis of gene expression in T cells to identify targets of the NF-kappa B transcription factor c-Rel. J Immunol 2007;178:7097–7109 [DOI] [PubMed] [Google Scholar]
- 32.Tumang JR, Hsia CY, Tian W, Bromberg JF, Liou HC. IL-6 rescues the hyporesponsiveness of c-Rel deficient B cells independent of Bcl-xL, Mcl-1, and Bcl-2. Cell Immunol 2002;217:47–57 [DOI] [PubMed] [Google Scholar]
- 33.Visekruna A, Huber M, Hellhund A, et al. c-Rel is crucial for the induction of Foxp3(+) regulatory CD4(+) T cells but not T(H)17 cells. Eur J Immunol 2010;40:671–676 [DOI] [PubMed] [Google Scholar]
- 34.Emamaullee JA, Davis J, Merani S, et al. Inhibition of Th17 cells regulates autoimmune diabetes in NOD mice. Diabetes 2009;58:1302–1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jeker LT, Bour-Jordan H, Bluestone JA. Breakdown in peripheral tolerance in type 1 diabetes in mice and humans. Cold Spring Harb Perspect Med 2012;2:a007807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Valéro R, Baron ML, Guérin S, et al. A defective NF-kappa B/RelB pathway in autoimmune-prone New Zealand black mice is associated with inefficient expansion of thymocyte and dendritic cells. J Immunol 2002;169:185–192 [DOI] [PubMed] [Google Scholar]
- 37.Zhu M, Chin RK, Christiansen PA, et al. NF-kappaB2 is required for the establishment of central tolerance through an Aire-dependent pathway. J Clin Invest 2006;116:2964–2971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang DB, Chen YQ, Ruetsche M, Phelps CB, Ghosh G. X-ray crystal structure of proto-oncogene product c-Rel bound to the CD28 response element of IL-2. Structure 2001;9:669–678 [DOI] [PubMed] [Google Scholar]
- 39.Bunting K, Wang J, Shannon MF. Control of interleukin-2 gene transcription: a paradigm for inducible, tissue-specific gene expression. Vitam Horm 2006;74:105–145 [DOI] [PubMed] [Google Scholar]
- 40.Sharma R, Fu SM, Ju ST. IL-2: a two-faced master regulator of autoimmunity. J Autoimmun 2011;36:91–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rosenzwajg M, Churlaud G, Hartemann A, Klatzmann D. Interleukin 2 in the pathogenesis and therapy of type 1 diabetes. Curr Diab Rep 2014;14:553. [DOI] [PubMed] [Google Scholar]
- 42.Wang J, Wicker LS, Santamaria P. IL-2 and its high-affinity receptor: genetic control of immunoregulation and autoimmunity. Semin Immunol 2009;21:363–371 [DOI] [PubMed] [Google Scholar]
- 43.Cheng G, Yu A, Dee MJ, Malek TR. IL-2R signaling is essential for functional maturation of regulatory T cells during thymic development. J Immunol 2013;190:1567–1575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen Z, Herman AE, Matos M, Mathis D, Benoist C. Where CD4+CD25+ T reg cells impinge on autoimmune diabetes. J Exp Med 2005;202:1387–1397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Feuerer M, Shen Y, Littman DR, Benoist C, Mathis D. How punctual ablation of regulatory T cells unleashes an autoimmune lesion within the pancreatic islets. Immunity 2009;31:654–664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.You S, Belghith M, Cobbold S, et al. Autoimmune diabetes onset results from qualitative rather than quantitative age-dependent changes in pathogenic T-cells. Diabetes 2005;54:1415–1422 [DOI] [PubMed] [Google Scholar]
- 47.D’Alise AM, Auyeung V, Feuerer M, et al. The defect in T-cell regulation in NOD mice is an effect on the T-cell effectors. Proc Natl Acad Sci U S A 2008;105:19857–19862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tritt M, Sgouroudis E, d’Hennezel E, Albanese A, Piccirillo CA. Functional waning of naturally occurring CD4+ regulatory T-cells contributes to the onset of autoimmune diabetes. Diabetes 2008;57:113–123 [DOI] [PubMed] [Google Scholar]
- 49.Mokhtari D, Barbu A, Mehmeti I, Vercamer C, Welsh N. Overexpression of the nuclear factor-κB subunit c-Rel protects against human islet cell death in vitro. Am J Physiol Endocrinol Metab 2009;297:E1067–E1077 [DOI] [PubMed] [Google Scholar]
- 50.Kim S, Millet I, Kim HS, et al. NF-kappa B prevents beta cell death and autoimmune diabetes in NOD mice. Proc Natl Acad Sci U S A 2007;104:1913–1918 [DOI] [PMC free article] [PubMed] [Google Scholar]