Abstract
PURPOSE
We aimed to assess the safety and effectiveness of transcatheter arterial embolization (TAE) for mesenteric bleeding following trauma.
METHODS
From 2001 to 2015, 12 patients were referred to our interventional unit for mesenteric bleeding following trauma, based on clinical decisions and computed tomography (CT) images. After excluding one patient with no bleeding focus and one patient who underwent emergency surgery, a total of 10 patients (male:female ratio, 9:1; mean age, 52.1 years) who underwent super selective TAE of visceral arteries were included in this study. Technical and clinical success, complications, and 30-day mortality rate were analyzed.
RESULTS
In 10 patients who underwent TAE, the types of trauma were motor vehicle collision (n=6), fall (n=2), assault (n=1), and penetrating injury (n=1), and the bleeding arteries were in the pancreaticoduodenal arterial arcade (n=4), jejunal artery (n=3), colic artery (n=2), and sigmoid artery (n=1). N-butyl-2-cyanoacrylate (NBCA) (n=2), microcoils (n=2), and combinations of NBCA, microcoils, or gelatin sponge particles (n=6) were used as embolic agents. Technical success was achieved in all 10 patients, with immediate cessation of bleeding. Clinical success rate was 90% (9/10), and all patients were discharged with no further treatment required for mesenteric bleeding. However, one patient showed rebleeding 10 days later and underwent repeated TAE with successful result. There were no TAE-related ischemic complications such as bowel infarction. The 30-day mortality rate was 0%.
CONCLUSION
Our clinical experience suggests that TAE used to control mesenteric bleeding following trauma is safe and effective as a minimally invasive alternative to surgery.
Mesenteric injury following trauma is relatively rare. However, it is clinically important because it can be associated with intraperitoneal, gastrointestinal, or retroperitoneal bleeding, intestinal ischemia, stenosis, and/or perforation (1). Surgical treatment has been the standard treatment of choice for mesenteric injuries, especially active mesenteric bleeding, mesenteric disruption, and associated bowel ischemia (2–4). The effectiveness of transcatheter arterial embolization (TAE) for traumatic liver, splenic, and renal injuries has been well established (5); however, TAE for traumatic mesenteric injury has received less attention than surgical managements.
There have been few case reports of TAE for mesenteric bleeding following trauma (1, 2, 6–8). The purpose of our study was to retrospectively evaluate the safety and effectiveness of TAE for traumatic mesenteric bleeding.
Methods
Patients
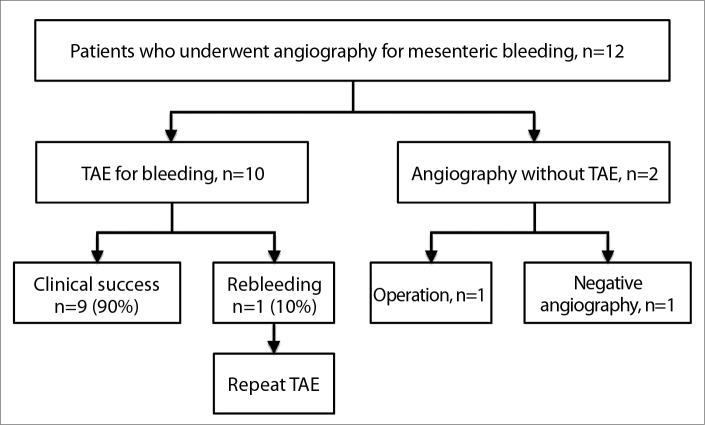
This retrospective study was approved by our institutional review board. From January 2001 to June 2015, 12 patients were referred to our interventional unit for TAE of traumatic mesenteric bleeding, based on clinical decisions and computed tomography (CT) images. Among these 12 patients, 10 patients who underwent selective TAE to control mesenteric bleeding were included in this study (Fig. 1). The patient characteristics are presented in the Table.
Figure 1.
Clinical course of 12 patients who underwent angiography with or without transcatheter arterial embolization (TAE) for mesenteric bleeding following trauma.
Table.
Patient characteristics and clinical outcomes
| No./Sex/Age (y) | Trauma type | Interval* (hrs) | CE/PSA on CT scans | Bleeding artery | Angio. findings | Embolic materials | Hb (Pre/Post) | Technical success | Clinical success | Remark |
|---|---|---|---|---|---|---|---|---|---|---|
| 1/M/50 | Fall | 55 | CE, PSA | Jejunal | CE, PSA | Coils | 8.6/10.2 | Yes | Yes | |
| 2/M/26 | MVC | 4 | CE | PD arcade | CE | Coils, GSP | 12.7/11.2 | Yes | Yes | |
| 3/M/52 | MVC | 8 | CE | PD arcade | CE | Coils, GSP | 9.6/11.5 | Yes | Yes | |
| 4/M/58 | MVC | 5 | CE, PSA | Jejunal | CE, PSA | NBCA | 12.1/12.7 | Yes | Yes | |
| 5/M/31 | MVC | 136 | NA unenhanced CT) | Left colic | PSA | Coil | 9.2/11.6 | Yes | No | Rebleeding → 2nd embolization |
| 6/M/75 | Fall | 3 | CE | PD arcade | CE | NBCA | 7.9/9.8 | Yes | Yes | Left renal artery embolization |
| 7/F/44 | Assault | 12 | CE, PSA | PD arcade | CE, PSA | NBCA, Coils | 8.2/11.0 | Yes | Yes | |
| 8/M/61 | MVC | 2 | CE | Jejunal | CE | NBCA, GSP | 9.3/10.5 | Yes | Yes | |
| 9/M/58 | MVC | 86 | PSA | Mid colic | PSA | NBCA, Coils | 12.3/13.2 | Yes | Yes | |
| 10/M/66 | Penetrating injury | 4 | CE | Sigmoid | CE | NBCA, Coils | 9.1/12.8 | Yes | Yes | PSA of puncture site →thrombin |
CE, contrast extravasation; PSA, pseudoaneurysm; CT, computed tomography; Angio., angiographic; Hb, hemoglobin; M, male; MVC, motor vehicle collision; PD, pancreaticoduodenal artery; GSP, gelatin sponge particle; NBCA, n-butyl-2-cyanoacrylate; NA, not available; F, female;.
Interval means time interval between trauma and angiography.
Traumatic mesenteric bleeding was defined as contrast extravasation, mesenteric hematoma and hemoperitoneum seen on CT scans after trauma (9, 10). Vital signs, including systolic and diastolic blood pressure and heart rate, and coagulation study results such as hemoglobin, platelet count, prothrombin time, activated partial thromboplastin time, and the international normalized ratio (INR), were also obtained at the patient’s initial presentation.
The interval between the trauma and angiography, type of trauma, clinical presentations, CT findings, details of the embolization procedure, such as the angiographic findings and embolic materials used, procedure-related complications, and outcomes after TAE, including technical and clinical success and the 30-day mortality rate, were analyzed.
Angiography and the embolization procedure
Angiography and embolization were performed by four interventional radiologists with 6–27 years of clinical experience performing endovascular treatment. After local anesthesia with lidocaine, the right common femoral artery was routinely accessed. Celiac, superior mesenteric, and/or inferior mesenteric angiograms were performed to determine the focus of mesenteric injury using a 5F catheter (RH or C2 catheter, Cook Medical) and a 0.035-inch, hydrophilic guidewire (Radifocus, Terumo Inc.). Super selection of bleeding arteries was performed using a 2.0F–2.4F microcatheter (Progreat, Terumo Inc.; Renegade, Boston Scientific).
Embolization was performed under fluoroscopic monitoring using microcoils (MicroNester or Tornado; Cook Medical), n-butyl-2-cyanoacrylate (NBCA; Histoacryl, B. Braun) or gelatin sponge particles (Spongostan, Johnson & Johnson) depending on the manifestation of bleeding signs or the operator’s preference. Complete angiograms were performed in order to confirm that bleeding has been successfully controlled.
Definitions and study end-points
In patients with active bleeding, technical success of TAE was defined as occlusion of the bleeding site without extravasation seen on post-TAE angiography. Clinical success was defined as the cessation of bleeding following TAE without need for repeat embolization or additional surgery due to mesenteric bleeding.
Complications were classified as major or minor according to the guidelines of the Society of Interventional Radiology Standards of Practice Committee (11). Major complications were defined as those requiring major therapy, an unplanned increase in the level of care or prolonged hospitalization, permanent adverse sequelae or death. Minor complications were defined as those requiring no nominal therapy, including overnight admission for observation only (11).
Results
The characteristics and outcomes of the 10 patients who underwent embolization are summarized in the Table. The median interval between the trauma and angiography was five hours (range, two hours to 6 days). Short interval of less than 24 hours was noted in seven patients (range, 2–12 hours), while long interval of more than 24 hours in three patients (range, 55–136 hours). The most common type of trauma was a motor vehicle collision (n=6), followed by fall (n=2), assault (n=1), and penetrating injury (n=1). Hematemesis was noted in one patient (Patient 2). In the remaining nine patients, there were no signs of gastrointestinal bleeding, such as hematemesis, hematochezia, or melena.
Five patients had further injury to other intra-abdominal organs: pancreas (n=4), liver (n=2), kidney (n=1), and mesentery (n=1). Eight patients sustained further injury to other systems: musculoskeletal (n=7), thorax (n=2), head and neck (n=1), and cardiovascular (n=1). In one patient (Patient 6) with concomitant left renal traumatic injury, left renal angiogram showed two foci of active bleeding at the anterior segmental branch of the left renal artery, and both of which were successfully embolized with microcoils and gelatin sponge particles.
Three patients (30%, 3/10) showed blood pressure drop to less than 90/60 mmHg. Coagulopathy was not noted in any patients. The median INR of all patients was 1.1 (range, 0.9–1.3), and the median number of the platelet count was 171000/μL (range, 137000–259000).
All 10 patients showed mesenteric hematoma and hemoperitoneum on CT images. Contrast extravasation or pseudoaneurysm was noted in nine patients. In one patient (Patient 5), contrast extravasation or pseudoaneurysm could not be evaluated, because the patient was evaluated by unenhanced CT scans due to high level of creatinine.
In 12 patients referred for angiography, there were positive signs of bleeding in 11 patients, and there was no bleeding focus in one patient. One of the 11 patients underwent surgery immediately following angiography without TAE by surgeon’s decision because of large amount of hemoperitoneum. Therefore, a total of 10 patients (male:female ratio, 9:1; mean age, 52.1 years) underwent super selective TAE of visceral arteries in order to control mesenteric bleeding (Fig. 1). For the one patient with no bleeding focus, prophylactic embolization was not performed, and he became stabilized with conservative treatment.
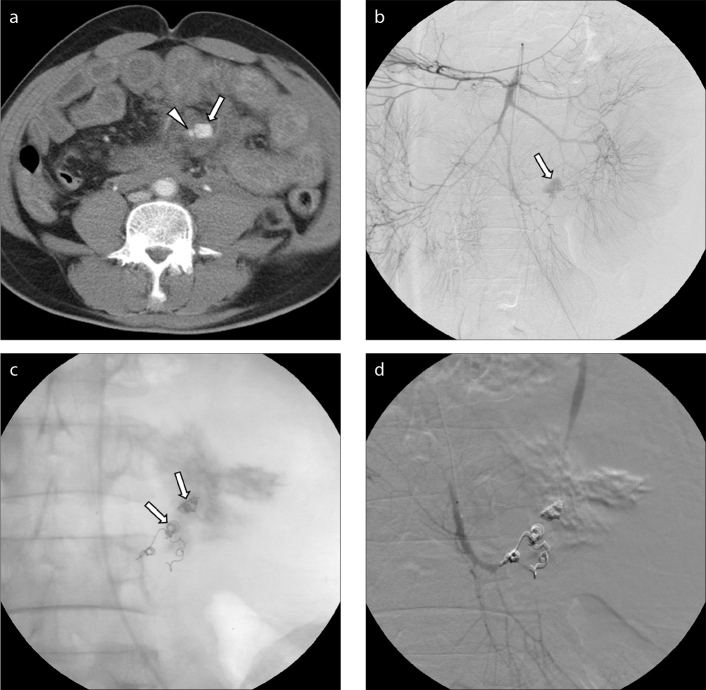
On angiography, bleeding artery was most commonly found in the pancreaticoduodenal arterial arcade (n=4, Fig. 2), followed by the jejunal artery (n=3, Fig. 3), colic artery (n=2), and sigmoid artery (n=1). Contrast extravasation was noted in eight patients, pseudoaneurysm in five patients, and both in three patients.
Figure 2.
a–d. A 44-year-old woman (Patient 7) with abdominal pain after an assault one day previously. An enhanced, axial CT scan image (a) shows a pseudoaneurysm (arrow) with contrast extravasation (arrowhead) at a branch of the gastroduodenal artery with hemoperitoneum. Common hepatic arteriogram (b) shows a pseudoaneurysm (arrow) with contrast extravasation (arrowhead) from the branch of the gastroduodenal artery. Distal pancreaticoduodenal arteries were embolized using two microcoils (arrows), and the pseudoaneurysm was then embolized with NBCA (arrowheads) (c). Completion common hepatic arteriogram (d) shows no further bleeding. The superior mesenteric arteriogram also shows no bleeding focus (not shown).
Figure 3.
a–d. A 50-year-old man (Patient 1) who had a motor vehicle collision two days previously. An enhanced, axial CT scan image (a) shows a pseudoaneurysm (arrow) with contrast extravasation (arrowhead) at a branch of the jejunal artery with hemoperitoneum. Superior mesenteric arteriogram (b) shows a pseudoaneurysm (arrow) at a branch of the jejunal artery of the superior mesenteric artery. After superselection of the bleeding arterial branch, the bleeding focus was embolized using seven microcoils (arrows) (c). The extravasated contrast agent is also noted (c). Completion selective superior mesenteric arteriogram (d) shows no further bleeding.
Single embolic agents were used in four patients: NBCA (n=2) and microcoils (n=2). Combined embolic agents were used in six patients: microcoils with NBCA (n=3), microcoils with gelatin sponge particles (n=2), and NBCA with gelatin sponge particles (n=1).
Technical success was achieved in all 10 patients, with immediate cessation of bleeding. Among the patients who underwent technically successful embolization, clinical success was achieved in nine patients, all of whom were discharged with no further treatment for the mesenteric bleeding, resulting in a clinical success rate of 90%.
One patient (Patient 5) with clinical failure showed a drop of blood pressure and an increased amount of hemoperitoneum on a CT scan performed 10 days following TAE of the left colic artery with a microcoil. The patient then underwent repeat angiography. On the second angiography, a pseudoaneurysm with extravasation at another branch of the left colic artery was observed and TAE was performed using microcoils. Successful bleeding control was achieved after the second embolization. The patient was discharged with no further treatment for the mesenteric bleeding.
There was no TAE-related ischemic complication such as bowel ischemia or infarction. One patient (Patient 10) complained for pulsatile palpable mass in right inguinal region after procedure. Ultrasonography (US) showed a pseudoaneurysm at right common femoral artery, and the lesion was successfully treated by US-guided thrombin injection.
Three patients with drop in blood pressure showed stabilization of their blood pressure after TAE. In all patients, the median amount of the transfusion was 4 units of packed red blood cells (range, 2–8 packs). The 30-day mortality rate of these patients was 0%.
Discussion
In this study, angiography showed a high detection rate of the bleeding focus in patients with mesenteric bleeding following trauma. TAE was successfully used in all 10 patients to control mesenteric bleeding following trauma.
Mesentery and bowel injury develops in an estimated 1%–5% of cases after blunt abdominal trauma and in up to 17% of cases following penetrating injury (12, 13). Mesenteric injuries may cause significant blood loss or lead to bowel ischemia and necrosis with eventual delayed rupture or ischemic strictures (14). Traumatic mesenteric injuries are traditionally treated surgically (6, 8). However, if the mesenteric injuries are isolated and not associated with gastrointestinal perforation, angiography and TAE may be considered (6, 8).
Nonsurgical management of abdominal trauma has gained increasing acceptance in mild trauma patients, and this approach has been expanded for use in severe patients previously considered as candidates for surgery (15). Angiography and TAE may have an important role in the diagnosis and treatment of mesenteric bleeding. Angiography can detect and localize the bleeding focus, and TAE can effectively stop acute bleeding (16). Skilled interventional radiologists and improved interventional devices including embolic materials have increased the utility of TAE in various conditions (17).
Among 12 patients with suspected mesenteric bleeding on CT images following trauma, there were positive signs of bleeding in 11 patients. The rate of positive angiographic findings was 92% (11/12) in our study. In 10 patients who underwent TAE, the angiographic findings were very similar with pre-procedural CT findings except one patient (Patient 5) who underwent unenhanced CT because of decreased renal function. Nowadays multidetector CT is recognized as a primary tool in the diagnosis of traumatic injuries to the bowel and mesentery in stable and semi-stable patients (10). Previous reports indicate that multidetector CT has a high negative predictive value, but there is variability in the sensitivity and accuracy of CT for the diagnosis of bowel and mesenteric injuries requiring surgery (13, 14, 18).
A few cases of successful treatment of traumatic mesenteric bleeding by TAE have been reported (1, 2, 6–8). In our study, technical success was achieved in all 10 patients and clinical success was achieved in 90% (9/10). Furthermore, in one case of rebleed (Patient 5), the rebleeding focus was successfully treated by repeat TAE and differed from the bleeding focus at the first TAE.
One more advantage of the TAE for mesenteric bleeding is that bleeding of other intra-abdominal organs, such as the liver, spleen or kidney, or bleeding from major pelvic fractures can be simultaneously controlled by TAE. In our study, renal artery embolization was performed to control renal bleeding in one patient (Patient 6). TAE for traumatic hepatic, splenic, and renal injury and pelvic fracture was reported to be a safe and effective treatment (15, 19, 20).
The choice of the embolic materials is based on vascular anatomy, angiographic findings, achievable catheter position, and preference of the operator. Embolization of the feeding artery was achieved using different combinations of embolic materials. In our study, NBCA and microcoils were commonly used embolic materials, and gelatin sponge particle was additionally used in three patients. Gelatin sponge particles cause temporary occlusion of the embolized arteries, with most vessels recanalizing in several weeks (21). In our study, gelatin sponge particles and NBCA were used to embolize more distal parts of the bleeding arteries, whereas microcoils were primarily used to embolize more proximal parts of the bleeding arteries.
The use of NBCA has recently gained acceptance (22). NBCA is widely used for controlling active bleeding, including mesenteric arterial bleeding (23). It is highly penetrable due to its liquid nature, and should be mixed with lipiodol for radiopacity and control of viscosity. Deeper penetration of NBCA to distal vessel can be achieved at more diluted concentrations (22). It rapidly polymerizes with blood; therefore, it is advantageous for massive bleeding that urgently requires hemostasis, especially in patients with coagulopathy (24). NBCA can be used alone or in combination with other embolic materials for successful bleeding control.
Various major and minor complications of TAE for mesenteric arteries have been reported in previous studies (17, 22, 25, 26). In our study, pseudoaneurysm developed at the vascular access site in one patient (Patient 10). The lesion was successfully treated by US-guided thrombin injection. US-guided thrombin injection is a safe treatment method for iatrogenic femoral pseudoaneurysm with good results (27). TAE for the mesenteric artery can increase the risk of bowel ischemia by reducing blood flow to the bowel segment (25), and nontarget embolization can also occur (26). However, advanced super selective catheterization technique has helped to decrease this risk during the past decade (25). In our study, there were no TAE-related ischemic complications and there was no patient mortality.
Our study has several limitations. First, this is a nonrandomized, retrospective study where all data were collected through a review of the medical records. Second, the number of patients in our study was relatively small. However, traumatic mesenteric bleeding is uncommon and the data collection time was 15 years. Third, various interventional devices and embolic materials were used over a long study period. And the number of operators also adds to the variability that may potentially influence the results.
In conclusion, patients with mesenteric bleeding following trauma require prompt clinical and imaging evaluation and, if clinically necessary, should be considered for endovascular intervention. Angiography can determine and localize the bleeding focus, and embolization can be performed subsequently. Our clinical experience suggests that TAE is a safe and effective minimally invasive alternative to surgery for control of mesenteric bleeding following trauma.
Main points.
Angiography and transcatheter arterial embolization (TAE) may be considered in patients presenting with isolated mesenteric injuries that are not associated with gastrointestinal perforation.
TAE for mesenteric bleeding following trauma is technically feasible and shows a high clinical success rate.
TAE for the control of mesenteric bleeding following trauma is safe and effective as a minimally invasive alternative to surgery.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Asayama Y, Matsumoto S, Isoda T, Kunitake N, Nakashima H. A case of traumatic mesenteric bleeding controlled by only transcatheter arterial embolization. Cardiovasc Intervent Radiol. 2005;28:256–258. doi: 10.1007/s00270-003-9108-y. http://dx.doi.org/10.1007/s00270-003-9108-y. [DOI] [PubMed] [Google Scholar]
- 2.Kakizawa H, Toyota N, Hieda M, et al. Traumatic mesenteric bleeding managed solely with transcatheter embolization. Radiat Med. 2007;25:295–298. doi: 10.1007/s11604-007-0135-5. http://dx.doi.org/10.1007/s11604-007-0135-5. [DOI] [PubMed] [Google Scholar]
- 3.Brofman N, Atri M, Hanson JM, Grinblat L, Chughtai T, Brenneman F. Evaluation of bowel and mesenteric blunt trauma with multidetector CT. Radiographics. 2006;26:1119–1131. doi: 10.1148/rg.264055144. http://dx.doi.org/10.1148/rg.264055144. [DOI] [PubMed] [Google Scholar]
- 4.Fang JF, Wong YC, Lin BC, Hsu YP, Chen MF. Usefulness of multidetector computed tomography for the initial assessment of blunt abdominal trauma patients. World J Surg. 2006;30:176–182. doi: 10.1007/s00268-005-0194-7. http://dx.doi.org/10.1007/s00268-005-0194-7. [DOI] [PubMed] [Google Scholar]
- 5.Velmahos GC, Chahwan S, Falabella A, Hanks SE, Demetriades D. Angiographic embolization for intraperitoneal and retroperitoneal injuries. World J Surg. 2000;24:539–545. doi: 10.1007/s002689910087. http://dx.doi.org/10.1007/s002689910087. [DOI] [PubMed] [Google Scholar]
- 6.Gabata T, Matsui O, Nakamura Y, Kimura M, Tsuchiyama T, Takashima T. Transcatheter embolization of traumatic mesenteric hemorrhage. J Vasc Interv Radiol. 1994;5:891–894. doi: 10.1016/s1051-0443(94)71632-8. http://dx.doi.org/10.1016/S1051-0443(94)71632-8. [DOI] [PubMed] [Google Scholar]
- 7.Rundback JH, Chughtai S, Rozenblit G, Panageas E, Poplausky M. Traumatic ileocolic pseudoaneurysm: diagnosis and transcatheter treatment. Catheter Cardiovasc Interv. 1999;48:217–219. doi: 10.1002/(sici)1522-726x(199910)48:2<217::aid-ccd22>3.0.co;2-j. http://dx.doi.org/10.1002/(SICI)1522-726X(199910)48:2<217::AID-CCD22>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 8.Hagiwara A, Takasu A. Transcatheter arterial embolization is effective for mesenteric arterial hemorrhage in trauma. Emerg Radiol. 2009;16:403–406. doi: 10.1007/s10140-008-0761-y. http://dx.doi.org/10.1007/s10140-008-0761-y. [DOI] [PubMed] [Google Scholar]
- 9.Virmani V, George U, MacDonald B, Sheikh A. Small bowel and mesenteric injuries in blunt trauma of the abdomen. Can Assoc Radiol J. 2013;64:140–147. doi: 10.1016/j.carj.2012.10.001. http://dx.doi.org/10.1016/j.carj.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Iaselli F, Mazzei MA, Firetto C, et al. Bowel and mesenteric injuries from blunt abdominal trauma: a review. Radiol Med. 2015;120:21–32. doi: 10.1007/s11547-014-0487-8. http://dx.doi.org/10.1007/s11547-014-0487-8. [DOI] [PubMed] [Google Scholar]
- 11.Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003;14:S199–S202. doi: 10.1097/01.rvi.0000094584.83406.3e. http://dx.doi.org/10.1097/01.RVI.0000094584.83406.3e. [DOI] [PubMed] [Google Scholar]
- 12.Watts DD, Fakhry SM. Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the East multi-institutional trial. EAST Multi-Institutional Hollow Viscus Injury Research Group. J Trauma. 2003;54:289–294. doi: 10.1097/01.TA.0000046261.06976.6A. http://dx.doi.org/10.1097/01.TA.0000046261.06976.6A. [DOI] [PubMed] [Google Scholar]
- 13.Butela ST, Federle MP, Chang PJ, et al. Performance of CT in detection of bowel injury. AJR Am J Roentgenol. 2001;176:129–135. doi: 10.2214/ajr.176.1.1760129. http://dx.doi.org/10.2214/ajr.176.1.1760129. [DOI] [PubMed] [Google Scholar]
- 14.Khan I, Bew D, Elias DA, Lewis D, Meacock LM. Mechanisms of injury and CT findings in bowel and mesenteric trauma. Clin Radiol. 2014;69:639–647. doi: 10.1016/j.crad.2014.01.021. http://dx.doi.org/10.1016/j.crad.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Goffette PP, Laterre PF. Traumatic injuries: imaging and intervention in post-traumatic complications (delayed intervention) Eur Radiol. 2002;12:994–1021. doi: 10.1007/s00330-002-1396-0. http://dx.doi.org/10.1007/s00330-002-1396-0. [DOI] [PubMed] [Google Scholar]
- 16.Hastings GS. Angiographic localization and transcatheter treatment of gastrointestinal bleeding. Radiographics. 2000;20:1160–1168. doi: 10.1148/radiographics.20.4.g00jl361160. http://dx.doi.org/10.1148/radiographics.20.4.g00jl361160. [DOI] [PubMed] [Google Scholar]
- 17.Shin JH. Recent update of embolization of upper gastrointestinal tract bleeding. Korean J Radiol. 2012;13:S31–S39. doi: 10.3348/kjr.2012.13.S1.S31. http://dx.doi.org/10.3348/kjr.2012.13.S1.S31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atri M, Hanson JM, Grinblat L, et al. Surgically important bowel and/or mesenteric injury in blunt trauma: accuracy of multidetector CT for evaluation. Radiology. 2008;249:524–533. doi: 10.1148/radiol.2492072055. http://dx.doi.org/10.1148/radiol.2492072055. [DOI] [PubMed] [Google Scholar]
- 19.Gould JE, Vedantham S. The role of interventional radiology in Trauma. Semin Intervent Radiol. 2006;23:270–278. doi: 10.1055/s-2006-948766. http://dx.doi.org/10.1055/s-2006-948766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choe J, Shin JH, Yoon HK, et al. Safety and efficacy of transarterial nephrectomy as an alternative to surgical nephrectomy. Korean J Radiol. 2014;15:472–480. doi: 10.3348/kjr.2014.15.4.472. http://dx.doi.org/10.3348/kjr.2014.15.4.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lubarsky M, Ray C, Funaki B. Embolization agents-which one should be used when? Part 2: small-vessel embolization. Semin Intervent Radiol. 2010;27:99–104. doi: 10.1055/s-0030-1247891. http://dx.doi.org/10.1055/s-0030-1247891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shin JH. Refractory gastrointestinal bleeding: role of angiographic intervention. Clin Endosc. 2013;46:486–491. doi: 10.5946/ce.2013.46.5.486. http://dx.doi.org/10.5946/ce.2013.46.5.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koo HJ, Shin JH, Kim HJ, et al. Clinical outcome of transcatheter arterial embolization with N-butyl-2-cyanoacrylate for control of acute gastrointestinal tract bleeding. AJR Am J Roentgenol. 2015;204:662–668. doi: 10.2214/AJR.14.12683. http://dx.doi.org/10.2214/AJR.14.12683. [DOI] [PubMed] [Google Scholar]
- 24.Toyoda H, Nakano S, Kumada T, et al. Estimation of usefulness of N-butyl-2-cyanoacrylate-lipiodol mixture in transcatheter arterial embolization for urgent control of life-threatening massive bleeding from gastric or duodenal ulcer. J Gastroenterol Hepatol. 1996;11:252–258. doi: 10.1111/j.1440-1746.1996.tb00071.x. http://dx.doi.org/10.1111/j.1440-1746.1996.tb00071.x. [DOI] [PubMed] [Google Scholar]
- 25.Ramaswamy RS, Choi HW, Mouser HC, et al. Role of interventional radiology in the management of acute gastrointestinal bleeding. World J Radiol. 2014;6:82–92. doi: 10.4329/wjr.v6.i4.82. http://dx.doi.org/10.4329/wjr.v6.i4.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yap FY, Omene BO, Patel MN, et al. Transcatheter embolotherapy for gastrointestinal bleeding: a single center review of safety, efficacy, and clinical outcomes. Dig Dis Sci. 2013;58:1976–1984. doi: 10.1007/s10620-012-2547-z. http://dx.doi.org/10.1007/s10620-012-2547-z. [DOI] [PubMed] [Google Scholar]
- 27.Olsen DM, Rodriguez JA, Vranic M, Ramaiah V, Ravi R, Diethrich EB. A prospective study of ultrasound scan-guided thrombin injection of femoral pseudoaneurysm: a trend toward minimal medication. J Vasc Surg. 2002;36:779–782. http://dx.doi.org/10.1016/S0741-5214(02)00133-7. [PubMed] [Google Scholar]