Abstract
Background
delay in diagnosis and treatment of tuberculosis (TB) may worsen the disease, increase mortality and enhance transmission in the community. This study aimed at assessing the association between total delay and unfavorable treatment outcome among newly diagnosed pulmonary TB (PTB) patients.
Methods
A prospective cohort study was conducted in West Gojjam Zone, Amhara Region of Ethiopia from October 2013 to May 2015. Newly diagnosed PTB patients who were ≥15 years of age were consecutively enrolled in the study from 30 randomly selected public health facilities. Total delay (the time period from onset of TB symptoms to first start of anti-TB treatment) was measured. Median total delay was calculated. Mixed effect logistics regression was used to analyze factors associated with unfavorable treatment outcome.
Results
Seven hundred six patients were enrolled in the study. The median total delay was 60 days. Patients with total delay of > 60 days were more likely to have unfavorable TB treatment outcome than patients with total delay of ≤ 60 days (adjusted odds ratio [AOR], 2.33; 95% confidence interval [CI], 1.04–5.26). Human immunodeficiency virus (HIV) positive TB patients were 8.46 times more likely to experience unfavorable treatment outcome than HIV negative TB patients (AOR, 8.46; 95% CI, 3.14–22.79).
Conclusions
Long total delay and TB/HIV coinfection were associated with unfavorable treatment outcome. Targeted interventions that can reduce delay in diagnosis and treatment of TB, and early comprehensive management of TB/HIV coinfection are needed to reduce increased risk of unfavorable treatment outcome.
Introduction
Tuberculosis (TB) remains a major threat to human beings, with the majority of cases occurring in the developing world. According to a recent World Health Organization (WHO) report, there were 9.6 million new TB cases and 1.5 million deaths from TB worldwide [1]. The 22 high TB burden countries collectively accounted for 80% of all estimated incident cases.
Ethiopia is among the 22 high TB burden countries in the world. The directly observed treatment, short-course (DOTS) strategy has been adopted in the country since 1992 to control the TB epidemic [2]. The prevalence, incidence and mortality from TB in Ethiopia is currently estimated at 200/100,000 population, 207/100,000 population and 33 per 100,000 population, respectively [1]. These indicators show that the TB burden in Ethiopia is still enormous.
Early diagnosis and prompt initiation of treatment is essential for an effective TB control program. Delay in TB diagnosis and treatment plays a major role in increasing the size of the infectious pool of TB. It may worsen the disease, increase the risk of mortality and enhance transmission in the community [3]. Delay in diagnosis and treatment of TB has previously been studied in various parts of the world. A systematic review reported that the median time of delay from onset of cough until treatment initiation varied from 21–136 days [4]. In Ethiopia, a number of studies that assessed the length of time of delay in TB diagnosis and treatment showed long delay time from onset of symptoms till initiation of treatment [5–9]. Various factors such as rural residence [8], lower educational level [7,9], being women, large family size, and stigma [9], being old age [8], first visit to non-formal health providers [7], first visit to clinics/ health posts [6] and form of TB [6,8] were reported as predictors of total delay.
Despite the increasing number of studies on diagnostic and treatment delay however, there is little to no information about the effect of total delay on unfavorable treatment outcome in Ethiopia and elsewhere. Factors such as old age, gender, TB/HIV coinfection, rural residence, low educational level and retreatment were reported to be associated with unfavorable treatment outcome [10–14]. Investigating the consequences of total delay on TB treatment outcome is important to suggest interventions that will improve the treatment success rate. Thus, the aim of this study was to analyze the association of total delay with unfavorable treatment outcome.
Methods
Study Setting
This study was conducted in West Gojjam Zone which is one of the ten zones of Amhara Region, Ethiopia. The total population is estimated at 2 382 497 [15]. More than 90% of the population resides in rural areas. One government hospital, 90 government health centers, 356 health posts and 76 private health institutions were rendering health services to the population during the study period.
A health post is the lowest level health care and is staffed by two female health extension workers (HEWs). HEWs play an important role in identifying and referring TB suspects to the next level of health care i.e. health centers for TB diagnosis and initiation of treatment. Health posts are not equipped with TB diagnostic tools.
TB Diagnosis and Treatment
The national guideline for clinical and programmatic management of TB which is adapted from the WHO TB treatment guidelines was followed to TB diagnosis, TB classification, case definition, TB treatment and evaluate treatment outcome [16]. Smear-positive TB is diagnosed when a patient has at least two initial sputum smear examinations positive for acid-fast bacilli (AFB), or one initial sputum smear examination positive for AFB and culture positive, or one initial sputum smear examination positive for AFB and radiographic abnormalities consistent with active TB. Smear-negative TB is diagnosed when a patient has symptoms suggestive of TB with at least three initial sputum smear examinations negative for AFB, radiographic abnormalities consistent with active TB, no response to a course of broad spectrum antibiotics and a decision by a clinician to treat with a full course of anti-TB chemotherapy. Provider initiated HIV counseling and testing is one of the routine clinical services given to TB patients.
TB treatment for new TB patients is given for six months. The regimen contains an intensive phase of daily chemotherapy with (2RHZE) rifampicin, isoniazid, pyrazinamide and ethambutol for two months, followed by a continuous phase treatment with (4RH) rifampicin and isoniazid for four months [16].
In this study, treatment outcomes are categorized into successful and unfavorable treatment outcomes. Successful treatment outcome includes “cured” and “treatment completed” cases. A patient is defined as “cured” if he/she became smear or culture negative in the last month of treatment and on at least one previous occasion. A patient is labeled as “treatment completed” if he/she completed treatment with resolution of symptoms [16, 17].
Unfavorable treatment outcome includes “treatment failure” cases and patients who “died”. A patient, who becomes smear or culture positive at five months or later during treatment or harbors a multi-drug resistant (MDR) strain at any point of time during the treatment, is referred to as “treatment failure”. A patient who died for any reason during treatment for TB is defined as “died”.
Defaulter: a defaulter is a patient who has been on treatment for at least four weeks and whose treatment was interrupted for eight or more consecutive weeks [16, 17].
Study Design and Population
This is a prospective cohort study conducted from October 2013 to May 2015. All newly diagnosed PTB patients ≥ 15 years of age who were registered for treatment in the selected public health facilities of the study area were consecutively enrolled. Patients were prospectively followed throughout their treatment period (six months). Health workers working in TB clinics of each study site provided treatment, followed patients and recorded treatment outcomes. PTB patients below 15 years of age, extra pulmonary TB (EPTB) patients, and TB patients with a previous history of TB and MDR-TB cases were excluded from the study.
Sample Size and Sampling Technique
The minimum required sample size for this study was determined using the formula for comparison of two proportions. This was done by applying openepi statistical software (version 2.3). The following assumptions were taken into account when calculating sample size. We considered 95% confidence interval, 80% power and exposed to non-exposed ratio of 1.0. The previous national report that showed 11% unsuccessful treatment outcome [18] was used to assign the proportion of exposed and non-exposed study participants with treatment outcome. Accordingly, we assumed that 8.5% of PTB patients exposed to long total delay and 2.5% of PTB patients non-exposed to long total delay would have unfavorable treatment outcome. Based on these assumptions, the sample size was calculated to be 518. We added 20% for non-responses and lost to follow-up cases and the total sample size was estimated at 622. However, we finally included all of the 706 new PTB patients that attended to the study sites during the study period.
Random sampling method was used to select study sites. First, we obtained list of all public health facilities providing TB diagnostic and treatment services in West Gojjam Zone. Accordingly, 73 health centers and one hospital were providing TB diagnostic and treatment services during the study period. Of these, 29 health centers were randomly selected. We also added one hospital which is the only available hospital in the study zone. This makes a total of 30 study sites.
Data Collection
Socio-demographic and clinical data were collected using a pre-tested semi-structured questionnaire. The data among others included: age, sex, symptoms at presentation, knowledge on TB and time period from onset of symptoms to first start of treatment. Trained health officers and nurses at each study site collected the data. To assure quality of the data, frequent supervision was made by the principal investigator and other supervisors throughout the data collection period. The supervisors regularly checked the completeness, consistency and accuracy of the data.
Data Analysis
Data were entered, cleaned and analyzed using Statistical Package for the Social Sciences (SPSS) IBM Version 22 (SPSS Inc. Chicago, IL, USA). The median total delay was used as a cut-off point to dichotomize the sample into delay and non-delay groups [5, 6, 9]. Descriptive statistics such as proportions and medians with interquartile ranges (IQRs) were computed. Mann-Whitney/Kruskal-Wallis tests were used to compare group differences in total delay. Categorical variables were compared using Fishers’ exact test and chi-square test. For each TB knowledge question a score of one was given for the correct answer and a zero score was given for incorrect responses. Then, total knowledge score and median were calculated. Finally, those with a total score of below the median value were classified as having poor knowledge whereas, those equal or above the median value were considered as having good knowledge.
Mixed-effect logistic regression model was used in order to adjust the clustering effects. Health facilities were held as random effect variable and other variables were used as fixed effects. Kaplan-Meier curve was used to estimate the probability of unfavorable treatment outcome of patients by delay status. Univariate and multivariate analysis were performed by using Stata statistical software V.14 (Stata Corporation, College Station, Texas, 77845 USA). Models were fit to analyze independent predictors of total delay, unfavorable treatment outcome and mortality. A two sided p-value of < 0.05 was considered statistically significant.
Operational Definition of Variables
Total delay: the time period from the onset of TB symptoms to first start of anti-TB treatment.
Long total delay: if the time period from the onset of TB symptoms to first start of anti-TB treatment is more than the calculated median total delay period.
A new case of TB: is a patient who has never had treatment for TB or who had taken anti-TB drugs for less than one month.
Ethical Approval
The Regional Committee for Medical Research Ethics (REK Øst) in Oslo, Norway and the National Research Ethics Review Committee (NRERC) in Addis Ababa, Ethiopia approved this study. In addition, letter of support and permissions to conduct the study in the local area were obtained from the local administrations. All participants were fully informed before written consents were taken. Then written informed consent was obtained from each participant who was willing to take part in this study. For those participants under the age of 18 years, written consent was obtained from their parents/legal guardians. The participants were assured about the confidentiality of the data.
Results
Characteristics of the Study Participants
A total of 706 newly diagnosed PTB patients were included in the study. Of these were 423 (59.9%) males and 283 (40.1%) females. The median age of the study participants was 30 years (IQR: 23–47 years). Of the total study participants, 61.6% were rural residents, 46.3% were farmers by occupation and 58.2% had no formal education (Table 1). Majority, 95% of the study participants reported to have taken less than two hours to reach at the nearest health facility (Table 2).
Table 1. Socio-demographic and clinical characteristics of the study participants, October 2013 to May 2015, West Gojjam Zone, Ethiopia.
| Variables | Frequency | Percent (%) |
|---|---|---|
| Age (years) | ||
| 15–24 | 197 | 27.9 |
| 25–44 | 291 | 41.2 |
| ≥45 | 218 | 30.9 |
| Sex | ||
| Male | 423 | 59.9 |
| Female | 283 | 40.1 |
| Place of residence | ||
| Urban | 271 | 38.4 |
| Rural | 435 | 61.6 |
| Educational level | ||
| Not literate | 411 | 58.2 |
| Literate | 295 | 41.8 |
| Marital status | ||
| Married | 386 | 54.7 |
| Single | 205 | 29.0 |
| Divorced | 73 | 10.3 |
| Widowed | 42 | 5.9 |
| Occupation | ||
| Civil servant | 41 | 5.8 |
| Housewife | 39 | 5.5 |
| Student | 76 | 10.8 |
| Farmer | 327 | 46.3 |
| Day laborer | 82 | 11.6 |
| Merchant | 47 | 6.7 |
| Others | 94 | 13.3 |
| Monthly family income (Birr)b | ||
| 1–400 | 109 | 15.4 |
| 401–800 | 84 | 11.9 |
| ≥ 801 | 264 | 37.4 |
| No regular income | 249 | 35.3 |
| HIV sero-status | ||
| Positive | 82 | 11.6 |
| Negative | 616 | 87.3 |
| Not known | 8 | 1.1 |
| Forms of TB | ||
| Smear-positive PTB | 334 | 47.3 |
| Smear -negative PTB | 372 | 52.7 |
b 1 USD = 22.00 Ethiopian Birr
PTB: Pulmonary tuberculosis
Table 2. Knowledge about TB and health seeking of the study participants, October 2013 to May 2015, West Gojjam Zone, Ethiopia.
| Variables | Frequency | Percent (%) |
|---|---|---|
| Knowledge of TB | ||
| Poor | 355 | 50.3 |
| Good | 351 | 49.7 |
| Perceived to be stigmatized | ||
| Yes | 88 | 12.5 |
| No | 618 | 87.5 |
| Time travelled to arrive at the nearest health facility Ѱ | ||
| ≤ 2 hours | 671 | 95.0 |
| > 2 hours | 35 | 5.0 |
| Health facilities first visited | ||
| Private health facilities | 280 | 39.6 |
| Public health centers | 342 | 48.4 |
| Public hospitals | 71 | 10.0 |
| Health posts | 13 | 2.0 |
| First action taken | ||
| Visited formal-health provider | 433 | 61.3 |
| Visited non-formal health provider | 223 | 31.6 |
| Self-treatment with home remedy | 50 | 7.1 |
Ѱ nearest health facility including health post, TB: tuberculosis
Duration of Delay and TB Symptoms
The median total delay was 60 days (IQR: 24–147 days). For 351 (49.8%) patients, the median total delay was > 60 days (Fig 1). Six hundred nineteen (97.9%) patients had persistent cough. High frequencies of fever, chest-pain, loss of appetite and body weight loss were reported among patients with total delay of > 60 days than those patients with total delay of ≤ 60 days (Table 3).
Fig 1. Study participants profile.
Table 3. Baseline signs and symptoms of new PTB patients stratified by median total delay, October 2013 to May 2015, West Gojjam Zone, Ethiopia.
| Variables | Total number (%) | Total delay > 60 days | Total delay ≤ 60 days | P value |
|---|---|---|---|---|
| Cough | 619 (97.9) | 344 (97.7) | 347 (98.0) | 0.78 |
| *Blood in sputum | 167 (23.7) | 94 (40.0) | 73 (33.2) | 0.13 |
| Chest pain | 578 (81.9) | 311 (88.4) | 267 (75.4) | < 0.001 |
| Fever | 513 (72.7) | 296 (84.1) | 217 (61.3) | < 0.001 |
| Loss of appetite | 633 (89.7) | 334 (94.9) | 299 (84.5) | < 0.001 |
| Night sweats | 569 (80.6) | 285 (81.0) | 284 (80.2) | 0.80 |
| Body weight loss | 548 (77.6) | 301 (85.5) | 247 (69.8) | < 0.001 |
PTB: pulmonary tuberculosis
Note: Participants could have more than one symptom
*Calculated among patients who reported productive cough
Factors Associated with Total Delay
In multivariate analysis, poor knowledge of TB (AOR, 2.39; 95% CI, 1.57–3.64), first visit to a non-formal health provider (AOR, 5.27; 95% CI, 3.43–8.08), being sputum smear-negative (AOR, 1.58; 95% CI, 1.09–2.29) and first visit to a health center (AOR, 2.18; 95% CI, 1.45–3.26) were factors associated with long total delay (Table 4).
Table 4. Associations of socio-demographic and clinical factors with total delay of new PTB patients, October 2013 to May 2015, West Gojjam Zone, Ethiopia.
| Variables | Number | Total delay ¶ Delayed (%) | Crude OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Sex | ||||
| Male | 423 | 197 (46.6) | 1.00 | 1.00 |
| Female | 283 | 155 (54.8) | 1.46 (1.06–2.00) | 1.32 (0.88–1.99) |
| Age | ||||
| 15–24 | 197 | 86 (43.7) | 1.00 | 1.00 |
| 25–44 | 291 | 136 (46.7) | 1.13 (0.77–1.65) | 0.86 (0.46–1.58) |
| ≥45 | 218 | 130 (59.6) | 2.03 (1.35–1.07)* | 1.16 (0.57–2.35) |
| Education | ||||
| Literate | 295 | 119 (40.3) | 1.00 | 1.00 |
| Not literate | 411 | 233 (56.7) | 2.17 (1.57–3.01)* | 1.41 (0.84–2.38) |
| Occupation | ||||
| Civil servant | 41 | 11 (26.8) | 1.00 | 1.00 |
| Housewife | 39 | 16 (41.0) | 1.91 (0.71–5.15) | 0.41 (0.09–1.73) |
| Student | 76 | 36 47.4) | 2.58 (1.08–6.19) | 1.25 (0.33–4.73) |
| Farmer | 327 | 179 (54.7) | 3.63 (1.68–7.86)* | 1.29 (0.48–3.49) |
| Day laborer | 82 | 36 (43.9) | 2.22 (0.94–5.27) | 0.65 (0.19–2.28) |
| Merchants | 47 | 21 (44.7) | 2.31 (0.89–6.01) | 1.79 (0.57–5.64) |
| Others | 94 | 53 (56.4) | 3.91 (1.67–9.16)* | 1.21 (0.34–4.33) |
| Marital status | ||||
| Married | 386 | 195 (50.5) | 1.00 | 1.00 |
| Single | 205 | 87 (42.4) | 0.70 (0.49–1.01) | 0.79 (0.44–1.44) |
| Divorced | 73 | 44 (60.3) | 1.44 (0.84–2.44) | 1.22 (0.63–2.34) |
| Widowed | 42 | 26 (61.9) | 1.56 (0.79–3.10) | 1.13 (0.46–2.75) |
| Place of residence | ||||
| Urban | 271 | 121 (44.6) | 1.00 | 1.00 |
| Rural | 435 | 231 (53.1) | 1.48 (1.07–2.07)* | 1.12 (0.71–1.78) |
| Monthly family income (Birr)b | ||||
| 1–400 | 109 | 47 (43.1) | 0.79 (0.49–1.27) | 0.53 (0.22–1.23) |
| 401–800 | 84 | 46 (54.8) | 1.24 (0.74–2.09) | 0.88 (0.34–2.26) |
| ≥ 801 | 264 | 134 (50.8) | 1.02 (0.70–1.48) | 0.79 (0.32–1.94) |
| No regular income | 249 | 125 (50.2) | 1.00 | 1.00 |
| HIV sero-status | ||||
| Positive | 82 | 42 (51.2) | 1.04 (0.64–1.70) | 1.19 (0.64–2.26) |
| Negative | 616 | 304 (49.4) | 1.00 | 1.00 |
| Knowledge of TB | ||||
| Poor | 355 | 222 (62.5) | 3.25 (2.32–4.54)* | 2.39 (1.57–3.64)* |
| Good | 351 | 130 (37.0) | 1.00 | |
| Perceived to be stigmatized | ||||
| Yes | 88 | 42 (47.7) | 0.92 (0.57–1.49) | 0.84 (0.47–1.49) |
| No | 618 | 310 (50.2) | 1.00 | 1.00 |
| Distance to the nearest HF | ||||
| ≤ 2hrs | 671 | 333 (49.6) | 1.00 | 1.00 |
| > 2hrs | 35 | 19 (54.3) | 1.45 (0.71–2.97) | 0.73 (0.32–1.69) |
| Forms of TB | ||||
| Smear -positive PTB | 334 | 150 (44.9) | 1.00 | 1.00 |
| Smear -negative PTB | 372 | 202 (54.3) | 1.55 (1.14–2.13)* | 1.58 (1.09–2.29)* |
| Health facilities first visited | ||||
| Private health facilities | 280 | 122 (43.6) | 1.00 | 1.00 |
| Public health centers | 342 | 187 (54.7) | 1.64 (1.17–2.29)* | 2.18 (1.45–3.26)* |
| Public hospitals | 71 | 36 (50.7) | 1.25 (0.72–2.17) | 1.26 (0.66–2.41) |
| Health posts | 13 | 7 (53.8) | 1.57 (0.49–4.99) | 1.63 (0.41–6.53) |
| First action taken | ||||
| Visited formal-health provider | 433 | 165 (38.1) | 1.00 | 1.00 |
| Visited non -formal health provider | 223 | 161 (72.2) | 5.12 (3.48–7.55)* | 5.27 (3.43–8.08)* |
| Self-treatment with home remedy | 50 | 26 (52.0) | 1.98 (1.06–3.70)* | 1.87 (0.93–3.76) |
*P ≤ 0.05,
¶: > 60 days,
OR: Odds Ratio, CI: confidence interval, PTB: pulmonary tuberculosis HF: health facility,
b 1 USD = 22.00 Ethiopian Birr
Tuberculosis Treatment Outcome
Overall, 656 (93%) patients had a successful treatment outcome (cured and treatment completed). A total of 38 (5.4%) patients had unfavorable treatment outcome (treatment failure and death) (Table 5). The proportion of unfavorable treatment outcome was higher for patients with total delay of > 60 days (7.6%) than for patients with total delay of ≤ 60 days (3.4%) (P = 0.02).
Table 5. Treatment outcomes of the study participants, West Gojjam Zone, Ethiopia.
| Treatment outcome | Number (%) |
|---|---|
| Cured | 310 (44.0) |
| Treatment completed | 346 (49.0) |
| Treatment failure | 10 (1.4) |
| Died | 28 (4.0) |
| Defaulter | 11(1.6) |
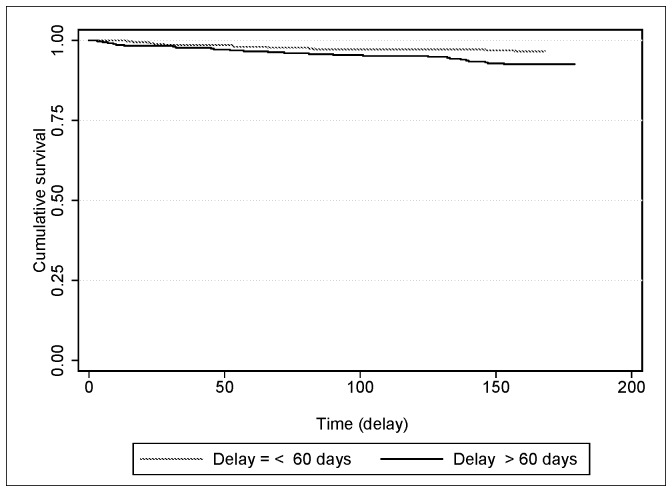
In multivariate analysis, those patients with total delay of > 60 days were more likely to have unfavorable treatment outcome than those patients with total delay of ≤ 60 days (AOR, 2.33; 95% CI, 1.04–5.26) (Table 6) (Fig 2). Being HIV-positive was associated with unfavorable treatment outcome (AOR, 8.46; 95% CI, 3.14–22.79).
Table 6. Associations of socio-demographic and clinical factors with unfavorable treatment outcome of new PTB patients, October 2013 to May 2015, West Gojjam Zone, Ethiopia.
| Variables | Number | Unfavorable treatment outcome (%) | Crude OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Total delay | ||||
| ≤ 60 days | 354 | 12 (3.4) | 1.00 | 1.00 |
| > 60 days | 351 | 26 (7.4) | 2.25 (1.10–4.59)* | 2.33 (1.04–5.26)* |
| Sex | ||||
| Male | 423 | 26 (6.1) | 1.00 | 1.00 |
| Female | 282 | 12 (4.2) | 0.66 (0.33–1.36) | 0.38 (0.14–1.01) |
| Age | ||||
| 15–24 | 197 | 4 (2.0) | 1.00 | 1.00 |
| 25–44 | 291 | 19 (6.5) | 3.39 (1.12–10.22)* | 2.14 (0.51–8.95) |
| ≥45 | 217 | 15 (7.0) | 3.69 (1.19–11.48)* | 2.85 (0.61–13.40) |
| Education | ||||
| Literate | 295 | 12 (4.1) | 1.00 | 1.00 |
| Not literate | 410 | 26 (6.3) | 1.65 (0.80–3.37) | 1.24 (0.42–3.66) |
| Marital status | ||||
| Married | 386 | 23 (6.0) | 1.00 | 1.00 |
| Single | 205 | 7 (3.4) | 0.56 (0.23–1.34) | 1.94 (0.57–6.55) |
| Divorced/ Widowed | 114 | 8 (7.0) | 1.10 (0.47–2.59) | 0.99 (0.34–2.91) |
| HIV sero-status | ||||
| Negative | 615 | 22 (3.6) | 1.00 | 1.00 |
| Positive | 82 | 15 (18.3) | 6.61 (3.10–14.08)* | 8.46 (3.14–22.79)* |
| Knowledge of TB | ||||
| Good | 351 | 15 (4.3) | 1.00 | 1.00 |
| Poor | 354 | 23 (6.5) | 1.59 (0.79–3.15) | 1.27 (0.53–3.08) |
| Perceived to be stigmatized | ||||
| No | 617 | 38 (6.2) | 1.00 | 1.00 |
| Yes | 88 | 0 (0.0) | Undefined | 0 (0.00— —) |
| Place of residence | ||||
| Urban | 271 | 17 (6.3) | 1.00 | 1.00 |
| Rural | 434 | 21 (4.8) | 0.79 (0.39–1.56) | 0.94 (0.35–2.49) |
| Occupation | ||||
| Farmer | 327 | 18 (5.5) | 1.00 | 1.00 |
| Housewife | 39 | 5 (12.8) | 2.30 (0.77–6.88) | 1.90 (0.31–11.72) |
| Day laborer | 81 | 6 (7.4) | 1.32 (0.49–3.55) | 0.37 (0.07–1.97) |
| Others | 258 | 9 (3.5) | 0.58 (0.25–1.34) | 0.31 (0.08–1.24) |
| Monthly family income (Birr)b | ||||
| No regular income | 248 | 16 (6.4) | 1.00 | 1.00 |
| 1–400 | 109 | 6 (5.5) | 0.85 (0.32–2.28) | 0.61 (0.16–2.25) |
| 401–800 | 84 | 5 (5.9) | 0.94 (0.33–2.72) | 0.60 (0.13–2.70) |
| ≥ 801 | 264 | 11 (4.2) | 0.65 (0.29–1.47) | 0.45 (0.12–1.77) |
| Forms of TB | ||||
| Smear-positive PTB | 333 | 18 (5.4) | 1.00 | 1.00 |
| Smear-negative PTB | 372 | 20 (5.4) | 1.04 (0.53–2.03) | 0.75 (0.35–1.59) |
| Distance to the nearest health facility | ||||
| ≤ 2hrs | 670 | 37 (5.5) | 1.00 | 1.00 |
| > 2hrs | 35 | 1 (2.8) | 0.67 (0.08–5.27) | 0.85 (0.09–7.99) |
*P ≤ 0.05, OR: Odds ratio, CI: confidence interval, PTB: pulmonary tuberculosis,
b 1 USD = 22.00 Ethiopian Birr
Fig 2. Kaplan-Meier estimate survival curves showing unfavorable treatment outcome of new PTB patients by total delay status.
Among the 38 patients with unfavorable treatment outcomes, 28 (73.7%) died and 10 (26.3%) had treatment failure. Further analysis was performed to analyze the association between total delay and death of PTB patients. Of the 28 patients who died during TB treatment, 18 (64.3%) patients had a total delay of > 60 days, and 27 patients did know their HIV status of which 13 (48.1%) were coinfected with HIV. Of the 13 HIV coinfected PTB patients who died during treatment, 11(84.6%) had total delay of more than 60 days. Nineteen (67.8%) deaths occurred during the intensive phase treatment (the first two months). Of these, 12 (63.1%) patients had total delay of > 60 days. The multivariate analysis did not show statistically significant association between total delay and death during treatment (AOR, 1.62; 95% CI, 0.64–4.12) (Table 7). HIV-positive TB patients were 21.7 times more likely to die compared to HIV-negatives (AOR 21.74; 95% CI, 6.35–74.42).
Table 7. Factors associated with death of PTB patients, October 2013 to May 2015, West Gojjam Zone, Ethiopia.
| Variables | Number | Death (%) | Crude OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Total delay | ||||
| ≤ 60 days | 354 | 10 (2.8) | 1.00 | 1.00 |
| > 60 days | 351 | 18 (5.1) | 1.84 (0.83–4.08) | 1.62 (0.64–4.12) |
| Sex | ||||
| Male | 423 | 19 (4.5) | 1.00 | 1.00 |
| Female | 282 | 9 (3.2) | 0.69 (0.30–1.56) | 0.35 (0.11–1.11) |
| Age | ||||
| 15–24 | 197 | 3 (1.5) | 1.00 | 1.00 |
| 25–44 | 291 | 12 (4.1) | 2.80 (0.78–10.11) | 1.33 (0.23–7.66) |
| ≥45 | 217 | 13 (5.9) | 4.18 (1.16–15.03)* | 2.97 (0.47–18.82) |
| Place of residence | ||||
| Urban | 271 | 12 (4.4) | 1.00 | 1.00 |
| Rural | 434 | 16 (3.7) | 0.84 (0.39–1.84) | 1.00 (0.31–3.26) |
| Occupation | ||||
| Housewife | 39 | 4 (10.3) | 1.00 | 1.00 |
| Farmer | 327 | 14 (4.3) | 0.39 (0.12–1.30) | 0.45 (0.56–3.51) |
| Day laborer | 81 | 3 (3.7) | 0.33 (0.69–1.58) | 0.05 (0.01–0.46) |
| Others | 258 | 7 (2.7) | 0.24 (0.66–0.89) | 0.11 (0.18–0.69) |
| Education | ||||
| Literate | 295 | 9 (3.0) | 1.00 | 1.00 |
| Not literate | 410 | 19 (4.6) | 1.56 (0.69–3.53) | 1.53 (0.41–5.63) |
| Marital status | ||||
| Married | 386 | 17 (4.4) | 1.00 | 1.00 |
| Single | 205 | 5 (2.4) | 0.54 (0.19–1.51) | 1.94 (0.57–6.55) |
| Divorced/ Widowed | 114 | 6 (5.3) | 1.16 (0.44–3.06) | 0.99 (0.34–2.91) |
| HIV sero-status | ||||
| Positive | 82 | 13 (15.9) | 8.52 (3.71–19.57)* | 21.74 (6.35–74.42)* |
| Negative | 615 | 14 (2.3) | 1.00 | 1.00 |
| Monthly family income (Birr)b | ||||
| No regular income | 248 | 11 (4.4) | 1.00 | 1.00 |
| 1–400 | 109 | 5 (4.6) | 1.01 (0.34–3.03) | 0.74 (0.16–3.44) |
| 401–800 | 84 | 4 (4.8) | 1.07 (0.33–3.51) | 0.63 (0.10–3.80) |
| ≥ 801 | 264 | 8 (3.0) | 0.68 (0.26–1.73) | 0.42 (0.85–2.13) |
| Knowledge of TB | ||||
| Good | 351 | 11 (3.1) | 1.00 | 1.00 |
| Poor | 354 | 17 (4.8) | 1.56 (0.71–3.41) | 1.27 (0.46–3.50) |
| Forms of TB | ||||
| Smear-positive PTB | 333 | 8 (2.4) | 1.00 | |
| Smear-negative PTB | 372 | 20 (5.4) | 2.43 (1.04–5.66)* | 2.24 (0.85–5.92) |
| Distance to the nearest health facility | ||||
| ≤ 2hrs | 670 | 27 (4.0) | 1.00 | 1.00 |
| ˃ 2hrs | 35 | 1 (2.9) | 0.79 (0.09–6.26) | 0.81 (0.85–7.53) |
*P ≤ 0.05, OR: Odds ratio, PTB: pulmonary tuberculosis, CI: confidence interval,
b 1 USD = 22.00 Ethiopian Birr
Discussion
In this study, we found an association between total delay and unfavorable treatment outcome. Patients with total delay of > 60 days were found to be more likely to have unfavorable treatment outcome than patients with total delay of ≤ 60 days. Long delays in diagnosis and treatment start contribute to severity and complications of illness that may result in poor treatment outcomes [19, 20]. It also increases the risk of developing anti-TB drug resistance leading to increased mortality rate, treatment failure and transmission of drug resistant TB strains in the community [21, 22]. This finding underscores the importance of early diagnosis and treatment of TB.
Majority, 18 (64.3%) patients who died during TB treatment had total delay of > 60 days. However, our analysis did not show statistically significant association between long total delay and increased death. This is consistent with the findings of earlier studies conducted in Gunea [23] and Vietnam [20]. In contrast, associations between diagnostic delay and increased mortality were reported from studies in China [24] and Taiwan [25]. These differences in findings among the studies may be related to variations in sample sizes, study populations, study settings and socio-economic backgrounds considered in the respective studies. The lack of significant association between total delay and death in our study may also be linked to the small number of observed deaths included in the sample analysis. Therefore, larger prospective cohort study is warranted to further investigate the effect of total delay on TB mortality.
Early mortality reflects advanced disease and could be attributed to delayed treatment and late diagnosis [26]. In our study, 67.9% of the deaths occurred during the two month (intensive phase) TB treatment period. Of these, 63.2% of patients had total delay of > 60 days. This finding suggests that expediting early diagnosis and treatment may reduce TB mortality.
The proportion of HIV positive TB patients accounted for 12% of the study population. This is somewhat higher than the recent 9.3% HIV prevalence observed in TB patients in Ethiopia [1]. There are variations in HIV prevalence among the different regions of Ethiopia. The Amhara Region where the study zone is located is one of the regions that have the highest HIV prevalence [27].
We found high risk of unfavorable treatment outcomes among HIV coinfected PTB patients. This is in line with findings of former studies [12–14]. Also, being HIV-positive was significantly associated with increased death of TB patients during treatment. This is consistent with the results of previous studies conducted in Ethiopia [28, 29], Cameroon [30], and Uzbekistan [31]. A number of possible explanations including severity of TB due to immune suppression, atypical clinical manifestation of TB, delay in diagnosis and treatment initiation have previously been reported for increased unfavorable treatment outcomes [32]. Immunological studies have also shown that host responses to M. tuberculosis enhance HIV replication which accelerates the natural progression of HIV and further depression of cellular immunity [33]. In addition decreased gut absorption of anti-tuberculous drugs leads to impaired treatment outcomes including death among TB/HIV coinfected patients [34].
In our study, about 80.4% of HIV coinfected PTB patients who died during treatment had total delay of > 60 days. This finding suggests that early comprehensive management of TB and HIV coinfection is required to reduce the risk of increased mortality and improve treatment outcome [35]. Early Antiretroviral treatment initiation improves survival in HIV-positive TB patients [36]. It also enables linkage between HIV and TB treatment programmes and could improve adherence [37]. Moreover, initiation of early antiretroviral treatment decreases incidence of HIV disease progression and has good tolerability [38].
The observed median total delay in our study is lower than that reported from an earlier study conducted in a comparable setting in the Amhara Region of Ethiopia [5], but higher than the study findings reported from other regions of Ethiopia [7,9,19]. It is also higher compared to the studies done in Nepal [21], Angola [39], Zimbabwe [40] and South Africa [41].
Various factors may have contributed to the relatively shorter total delay observed in our study compared to the former study that was conducted in a similar settings in the study region [5]. Improved access to diagnostic and treatment services, and the contribution of health extention workers in identifying and referring suspected TB cases to health facilities (health centers) for smear microscopy may be considered as the possible factors for the observed reduction in total delay. However, given the increased access to TB diagnostic and treatment services, and the integration of TB screening activities with the general health service in health care facilities of the study area, the observed median total delay in the current study is still very long.
In a recent qualitative study, a number of challenges that may have implications for long delay in TB diagnosis and treatment were reported from the study area. Among others, frequent interruptions of laboratory reagents and anti-TB drugs supplies, lack of diagnostic tools for smear-negative TB and lack of laboratory personnel in some health centers were identified [13]. Interventions directed at solving these challenges are essential to reduce long total delay observed in the study.
Majority of the TB patients at presentation had cough however, significantly higher proportion of clinical symptoms such as chest-pain, fever, loss of appetite and body weight loss were observed among patients with total delay of > 60 days than their counterparts. This is not surprising as prolonged delay results in disease progression and worsening of symptoms. The association between delay in TB treatment and clinical severity was reported from a study conducted in Gunea-Bissau [23].
Fifty four percent of patients with total delay of more than 60 days first visited public health centers. This finding is similar with a previous study done in Ethiopia [8]. Smear microscopy is the only TB diagnostic tool used in majority of health centers of the study area. Smear microscopy has very low sensitivity [42] and may show false negative results in many TB patients. The study highlights the need to enhance TB diagnostic capacity of health facilities particularly health centers. Better TB diagnostic tools to complement AFB smear microscopy are needed to early diagnose PTB cases.
Our study has limitations. The study did not include extra pulmonary and retreatment TB cases. In addition, the study was only carried out in government health facilities. Therefore, the findings cannot be generalized to all TB patients in the study area. Patients may not exactly remember the onset of their symptoms and time of first vist to a medical provider. This may be subjected to a recall bias. However, efforts were made to lessen recall bias by using local calendars listing main religious and national days to define the perceived date of onset cough (TB symptoms) and time of first health seeking. We did not collect data about the level of treatment adherence of each patient. In addition, complete sputum smear grading data was lacking due to absence of mycobacterial culture facilities in the study zone. The non-inclusion of these two variables in the analysis may have an effect on our findings.
The study also has strengths. As far as our literature review is concerned, this is the first study in Ethiopia that attempted to investigate the effect of total delay on TB treatment outcome. Therefore, the findings may be used as baseline data for future studies. The study also covered a large geographic area and included patients from urban and rural settings. In addition, the study was prospective cohort study. Participants were properly followed until completion of their treatment and the proportion of lost to follow-up cases was very low.
Conclusions
Long total delay and TB/HIV coinfection were associated with unfavorable treatment outcome. Mortality among HIV infected TB patients was high. Targeted interventions that can reduce delay in diagnosis and treatment of TB are needed to improve treatment outcome. Better TB diagnostic tools to complement AFB smear microscopy are needed at health centers of the study area. In addition, early comprehensive management of TB and HIV coinfection is essential to reduce the risk of increased mortality among HIV infected TB patients.
Acknowledgments
We would like to thank the Amhara Regional State Health Bureau, the West Gojjam Zone Health Department, the Districts and Town Administrations Health Offices for their support. We wish to thank all health professionals who participated in the data collection. Last but not least, we are very much grateful to the study subjects who consented to participate in the study.
Data Availability
Data may be used to identify study participants and may not be publicly shared. Data may be requested from the corresponding author.
Funding Statement
University of Oslo funded the study. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Global tuberculosis report. 2015. Available: http://apps.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf?ua=1. Accessed 17 January 2016.
- 2.Federal Ministry of Health Ethiopia. Tuberculosis, Leprosy and TB/HIV Prevention and Control Program Manual. 4 th ed Addis Ababa, Ethiopia: Ministry of Health of Ethiopia; 2008. [Google Scholar]
- 3.Sreeramareddy CT, Panduru KV, Menten J, Van den Ende J. Time delays in diagnosis of pulmonary tuberculosis: a systematic review of literature. BMC Infect Dis. 2009; 9:91 10.1186/1471-2334-9-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Storla DG, Yimer S and Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. 2008; 8:15 10.1186/1471-2458-8-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yimer S, Bjune G and Alene G. Diagnostic and treatment delay among pulmonary tuberculosis patients in Ethiopia: a cross sectional study. BMC Infect Dis. 2005; 5: 112 10.1186/1471-2334-5-112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belay M, Bjune G, Ameni G, Abebe F. Diagnostic and treatment delay among Tuberculosis patients in Afar Region, Ethiopia: A cross-sectional study. BMC Public Health. 2012; 12:369 10.1186/1471-2458-12-369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hussen A, Biadgilign S, Tessema F, Mohammed S, Deribe K, Deribew A. Treatment delay among pulmonary tuberculosis patients in pastoralist communities in Bale Zone, Southeast Ethiopia. BMC Res Notes. 2012; 5:320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yimer SA, Bjune GA, Holm-Hansen C. Time to first consultation, diagnosis and treatment of TB among patients attending a referral hospital in Northwest, Ethiopia. BMC Infect Dis. 2014; 14: 19 10.1186/1471-2334-14-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asefa A, Teshome W. Total Delay in Treatment among Smear Positive Pulmonary Tuberculosis Patients in Five Primary Health Centers, Southern Ethiopia: A Cross Sectional Study. PLoS ONE. 2014; 9(7): e102884 10.1371/journal.pone.0102884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gebrezgabiher G, Romha G, Ejeta E, Asebe G, Zemene E, Ameni G. Treatment Outcome of Tuberculosis Patients under Directly Observed Treatment Short Course and Factors Affecting Outcome in Southern Ethiopia: A Five-Year Retrospective Study. PLoS ONE.2016; 11(2): e0150560 10.1371/journal.pone.0150560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Munoz-Sellart M, Cuevas LE, Tumato M, Merid Y, Yassin MA. Factors associated with poor tuberculosis treatment outcome in the Southern Region of Ethiopia. Int J Tuberc Lung Dis.2010; 14: 973–979. [PubMed] [Google Scholar]
- 12.Jemal M, Tarekegne D, Atanaw T, Ebabu A, Endris M, Tessema B, et al. Treatment Outcomes of Tuberculosis Patients in Metema Hospital, Northwest Ethiopia: A Four Years Retrospective Study. Mycobact Dis. 2015; 5:190 10.4172/2161-1068.1000190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gebreegziabher SB, Yimer SA, Bjune GA. Qualitative Assessment of Challenges in Tuberculosis Control in West Gojjam Zone, Northwest Ethiopia: Health Workers’ and Tuberculosis Control Program Coordinators’ Perspectives. Tuberc Res Treat. 2016; 2016: 2036234 10.1155/2016/2036234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NNR NM,Mohd NS, WM Z, S D, NR NH. Factor associated with unsuccessful treatment outcome of pulmonary tuberculosis in Koto Bahru, Kelan. Malays J Public Health Medicine. 2011; 11(1): 6–15. [Google Scholar]
- 15.Central Statistics Autority: The 2007 Population and Housing Census of Ethiopia. Addis Ababa, Ethiopia: 2008. [Google Scholar]
- 16.Federal Ministry of Health Ethiopia. Guidelines for clinical and programmatic management of TB, leprosy and TB/HIV in Ethiopia. 5th ed Addis Ababa, Ethiopia: Ministry of Health of Ethiopia; 2012. [Google Scholar]
- 17.World Health Organization. Treatment of tuberculosis: guidelines -4th ed WHO/HTM/TB/2009.420; 2010. [PubMed] [Google Scholar]
- 18.World Health Organization (WHO). Global tuberculosis report. 2013. Available: http://apps.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf. Accessed on 11 November 2016.
- 19.Hamza A, Demissie M, Gare S, Teshome G. Delay in Tuberculosis Diagnosis among Tuberculosis Patients at the Three Hospitals: Asella, Robe and Abomsa of Arsi Zone, Oromia Regional State. Open Access Library Journal. 2015; 2, e1947 10.4236/oalib.1101947. [DOI] [Google Scholar]
- 20.Vree M, Huong NT, Duong BD, Co NV, Sy DN, Cobelens FG, et al. High mortality during tuberculosis treatment does not indicate long diagnostic delays in Vietnam: a cohort study. BMC Public Health. 2007; 7:210 10.1186/1471-2458-7-210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahato RK, Laohasiriwong W, Vaeteewootacharn K, Koju R, Bhattarai R. Major Delays in the Diagnosis and Management of Tuberculosis Patients in Nepal. J Clin Diagn Res. 2015; 9(10):LC05–9. 10.7860/JCDR/2015/16307.6633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kuznetsov VN, Grjibovski AM, Mariandyshev AO, Johansson E and Bjune GA, et al. Two vicious circles contributing to a diagnostic delay for tuberculosis patients in Arkhangelsk. Emerg Health Threats J. 2014; 7:24909 10.3402/ehtj.v7.24909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Virenfeldt J, Rudolf F, Camara C, Furtado A, Gomes V, Aaby P, et al. Treatment delay affects clinical severity of tuberculosis: a longitudinal cohort study. BMJ Open. 2014; 4:e004818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lui G, Wong RYK, Li F, Lee MKP, Lai RWM, Li TCM, et al. High Mortality in Adults Hospitalized for Active Tuberculosis in a Low HIV Prevalence Setting. PLoS ONE. 2014; 9(3): e92077 10.1371/journal.pone.0092077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu YC, Lin HH, Chen YS, Su IJ, Huang TS, Tsai HC, et al. Reduced health provider delay and tuberculosis mortality due to an improved hospital programme. Int J Tuberc Lung Dis. 2010; 14 (1):72–8. [PubMed] [Google Scholar]
- 26.Tolosie K, Sharma MK. Application of Cox Proportional Hazards Model in Case of Tuberculosis Patients in Selected Addis Ababa Health Centers, Ethiopia. Tuberc Res Treat. 2014; 2014:536976 10.1155/2014/536976. 10.1155/2014/536976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Central Statistical Agency of Ethiopia, ICF International Calverton M, USA. Ethiopia Demographic and Health Survey 2011. Central statistical Agency of Ethiopia: 2012. [Google Scholar]
- 28.Birlie A, Tesfaw G, Dejene T, Woldemichael K. Time to Death and Associated Factors among Tuberculosis Patients in Dangila Woreda, Northwest Ethiopia. PLoS ONE. 2015; 10(12): e0144244 10.1371/journal.pone.0144244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Workneh MH, Bjune GA and Yimer SA. Diabetes mellitus is associated with increased mortality during tuberculosis treatment: a prospective cohort study among tuberculosis patients in South- Eastern Amahra Region, Ethiopia. Infect Dis Poverty. 2016; 5:22 10.1186/s40249-016-0115-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Djouma FN, Noubom M, Ngomba AV, Donfack H, Kouomboua PSM, Saah MAF. Determinants of death among tuberculosis patients in a semi urban diagnostic and treatment centre of Bafoussam, West Cameroon: a retrospective case-control study. Pan Afr Med J. 2015; 22: 253 10.11604/pamj.2015.22.253.6576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gadoev J, Asadov D, Tillashaykhov M, Tayler-Smith K, Isaakidis P, Dadu A, et al. Factors Associated with Unfavorable Treatment Outcomes in New and Previously Treated TB Patients in Uzbekistan: A Five Year Countrywide Study. PLoS ONE. 2015; 10(6): e0128907 10.1371/journal.pone.0128907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shastri S, Naik B, Shet A, Rewari B and Costa AD. TB treatment outcomes among TB-HIV Co-infections in Karnataka, India: how do these compare with non-HIV tuberculosis outcomes in the province. BMC Public Health. 2013; 13:838 10.1186/1471-2458-13-838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Falvo JV, Ranjbar S, Jasenosky LD and Goldfeld AE. Arc of a Vicious Circle: Pathways Activated by Mycobacterium tuberculosis That Target the HI.V-1 Long Terminal Repeat. Am J Respir Cell Mol Biol. 2011; 45(6):1116–24. 10.1165/rcmb.2011-0186TR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lazarus JV, Olsen M, Ditiu L and Matic S. Tuberculosis-HIV coinfection: policy and epidemiology in 25 countries in the WHO European region. HIV Medicine. 2008; 9: 406–414. 10.1111/j.1468-1293.2008.00567.x [DOI] [PubMed] [Google Scholar]
- 35.Yan S, Chen L, Wu W, Fu Z, Zhang H, Li Z, et al. Early versus Delayed Antiretroviral Therapy for HIV and Tuberculosis Co-Infected Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS ONE. 2015; 10(5): e0127645 10.1371/journal.pone.0127645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Varma JK, Nateniyom S, Akksilp S, Mankatittham W, Sirinak C, Sattayawuthipong W, et al. HIV care and treatment factors associated with improved survival during TB treatment in Thailand: an observational study. BMC Infect Dis. 2009; 9:42 10.1186/1471-2334-9-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suthar AB, Rutherford GW, Horvath T, Doherty MC, Negussie EK. Improving antiretroviral therapy scale-up and effectiveness through service integration and decentralization. AIDS. 2014; 28 Suppl 2:S175–85. 10.1097/QAD.0000000000000259 [DOI] [PubMed] [Google Scholar]
- 38.Sinha S, Shekha RC, Singh G, Shah N, Ahmad H, Kuma N, et al. Early versus delayed initiation of antiretroviral therapy for Indian HIV-Infected individuals with tuberculosis on antituberculosis treatment. BMC Infect Dis. 2012; 12:168 10.1186/1471-2334-12-168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Segagni Lusignani L, Quaglio G, Atzori A, Nsuka J, Grainger R, Palma Mda C, et al. Factors associated with patient and health care system delay in diagnosis for tuberculosis in the province of Luanda, Angola. BMC Infect Dis. 2013; 13:168 10.1186/1471-2334-13-168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Takarinda KC, Harries AD, Nyathi B, Ngwenya M, Mutasa-Apollo T, Sandy C. Tuberculosis treatment delays and associated factors within the Zimbabwe national tuberculosis programme. BMC Public Health. 2015; 15:29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Van Wyk SS, Enarson DA, Beyers N, Lombard C, Hesseling AC. Consulting private health care providers aggravates treatment delay in urban South African tuberculosis patients. Int J Tuberc Lung Dis. 2011; 15(8):1069–76. 10.5588/ijtld.10.0615 [DOI] [PubMed] [Google Scholar]
- 42.Parsons L.M, Somosko A, Gutierrez C, Lee E, Paramasivan C.N, Abimiku A, et al. Laboratory Diagnosis of Tuberculosis in Resource-Poor Countries: Challenges and Opportunities. Clin Microbiol Rev. 2011; 24 (2): 314–350. 10.1128/CMR.00059-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data may be used to identify study participants and may not be publicly shared. Data may be requested from the corresponding author.