Abstract
Background
Extreme heat (EH) is a growing concern with climate change, and protecting human health requires knowledge of vulnerability factors. We evaluated whether associations between EH (maximum temperature > 97th percentile) and hospitalization for renal, heat and respiratory diseases among people ≥ 65 years differed by individual and area-level characteristics.
Methods
We used Medicare billing records, airport weather data, U.S. Census data and satellite land cover imagery in 109 US cities, May-September, 1992–2006, in a time-stratified case-crossover design. Interaction terms between EH and individual (> 78 years, black race, sex) and home ZIP-code (percentages of non-green space, high school education, housing built before 1940) characteristics were incorporated in a single model. Next, we pooled city-specific effect estimates or regressed them on quartiles of air conditioning prevalence (ACP) in a multivariate random effects meta-analysis.
Results
EH and combined renal/heat/respiratory hospitalization associations were stronger among blacks, the very old, in ZIP codes with lower educational attainment or older housing and in cities with lower ACP. For example, for EH versus non-heat days, we found a 15% (95% CI 11%–19%) increase in renal/heat/respiratory hospitalizations among individuals in ZIP codes with higher percent of older homes in contrast to a 9% (95% CI 6%–12%) increase in hospitalizations in ZIP codes with lower percent older homes.
Conclusion
Vulnerability to EH-associated hospitalization may be influenced by age, educational attainment, housing age and ACP.
Keywords: climate change, heat waves, hospital admissions, morbidity, temperature
1. Introduction
Over the 21st century, extreme heat (EH) episodes are very likely to increase (IPCC 2013). To adapt to climate change, community leaders, public health officials and emergency preparedness officials are interested in extreme-heat vulnerability assessments and in understanding which populations are most vulnerable to the health consequences of EH (Bierbaum et al. 2013, White-Newsome et al. 2014). Furthermore, estimates of the present and future burden of disease due to climate change can be informed by estimates of heat-health associations within subgroups of the population, which vary geographically and over time. Characteristics of vulnerability include personal characteristics, community attributes, and housing factors. These characteristics can enhance vulnerability to EH-related health outcomes, including deaths and hospitalizations, ambulance dispatches or emergency room visits for heat stroke, heat exhaustion, fluid and electrolyte abnormalities, renal failure, cardiovascular disease and respiratory disease. Research estimating increased vulnerability by each of these characteristics can inform these efforts across multiple groups of stakeholders.
The association between heat and mortality is well studied across a wide variety of climates (Anderson et al. 2009, Gosling et al. 2009, Hajat et al. 2010). Several studies have examined associations between heat and morbidity, but with mixed results (Bhaskaran 2009, Turner et al. 2012, Ye et al. 2012). A meta-analysis suggested an association between heat and hospitalization for respiratory but not cardiovascular causes (Turner et al. 2012). More recently, our study of 114 cities across the U.S. found 15% and 4% cumulative increases in hospitalizations for renal and respiratory diseases, respectively, over the eight days following EH. In contrast, we did not find an EH associated increase in hospitalizations for cardiovascular diseases. Furthermore, we observed significant heterogeneity within and between climate zones, suggesting that personal and area characteristics may modify the associations between EH and hospitalization for renal and respiratory diseases (Gronlund et al. 2014).
Individual-level or area-level characteristics which increase vulnerability to heat-associated morbidity have also been evaluated in previous studies, with widely varying results. Age has been found to modify the association between EH and mortality, with EH effects greater among individuals at least 65 years old (Basu 2009). Some U.S. studies have suggested increased vulnerability by racial and ethnic characteristics, with increased vulnerability among non-whites or blacks (Fletcher et al. 2012, Lin et al. 2009, Medina-Ramon et al. 2006, Noe et al. 2012, O’Neill et al. 2003, Schwartz 2005, Ye et al. 2012, Zanobetti et al. 2013) and decreased vulnerability among Asians (Noe et al. 2012), while other studies have not found increased vulnerability by racial and ethnic characteristics (Green et al. 2010, Pillai et al. 2014). Beyond individual racial effects, there may be neighborhood-level effects of living in a community of racial minorities(Morenoff and Lynch 2004), where resources and information for coping with EH may be further limited as a result of present and historical racial segregation.
Some studies have found increased vulnerability to heat-associated morbidity by surrounding imperviousness or lack of vegetation (Harlan et al. 2013, Smargiassi et al. 2009, Uejio et al. 2011, Xu et al. 2013, Zanobetti et al. 2013), while other studies have not (Madrigano et al. 2013, Uejio et al. 2011). In the U.S., individual or area-level low educational level has been associated with increased heat-associated mortality in some studies (O’Neill et al. 2003, Zanobetti et al. 2013) but not others (Basu et al. 2008, Medina-Ramon et al. 2006). However, U.S. studies have been more consistent in their findings of increased vulnerability to heat in low-income neighborhoods or communities (Anderson et al. 2009, Fletcher et al. 2012, Madrigano et al. 2013, Zanobetti et al. 2013).
Housing characteristics, including community-level air conditioning prevalence (ACP) and individual AC usage, have also been identified as largely protective factors during periods of EH (Gronlund et al. 2014). In Barcelona, census-tract housing age was protective against heat-wave mortality (Xu et al. 2013). Case-control studies of heat waves, including the 1995 Chicago heat wave and the 2003 French heat wave, found housing characteristics such as working air conditioners (Semenza et al. 1996) and good home insulation (Vandentorren et al. 2006) to be protective against heat-wave mortality. Research using qualitative or quantitative interview techniques has also identified air-conditioning use as highly protective against heat morbidity and mortality (Sampson et al. 2013).
Multiple individual and community characteristics have been assessed as potential vulnerability factors in the literature. However, several of these factors, such as abundance of vegetation and income in a neighborhood (Harlan et al. 2013), can be correlated with one another, both be associated with the outcome and thus confound, or be confused with, one another (Rothman et al. 2008). This limits the investigator’s ability to assess which factors are likely to be the primary influence on vulnerability and thus are priority targets for intervention.
In this study, we used methods that addressed confounding among the characteristics of age, race, sex, neighborhood racial composition, neighborhood non-green space, neighborhood educational attainment and neighborhood housing age. We applied these methods to a large U.S.-based dataset of hospital admissions among people aged 65 and older. Previous research has indicated that although hospitalization rates for causes coded as heat-related are low, hospitalizations for renal, heat and respiratory causes are associated with EH (Gronlund et al. 2014, Ye et al. 2012). Therefore, to study vulnerability to EH, we treated the potential vulnerability characteristics as “effect modifiers,” or we examined how the hospitalization-EH association varied across different levels of each vulnerability characteristic (Greenland et al. 2008). We addressed issues of confounding among the vulnerability characteristics by including them simultaneously in a regression model. We also assessed whether the potential effects of each of these characteristics were evident only in cities with low ACP.
Our specific objective was to examine vulnerability to the effect of EH in elderly US adults on hospitalizations for renal, heat and respiratory causes. Within categories of regional ACP prevalence and overall, we determined how EH effects increased with increasing age, black race, and male sex. We also determined how EH effects increased with increasing ZIP-code (postal code) percentages of non-green space, low educational attainment, black race, poverty and housing age.
2. Methods
2.1. Study cities and temperature
The 200 counties in the continental U.S. with the largest number of hospitalizations among the elderly were collapsed into 135 study cities and were assigned daily temperature values, as previously described (Gronlund et al. 2014, Zanobetti et al. 2013). For each study city, daily maximum temperatures were obtained via the National Climatic Data Center from the nearest monitor, often an airport, with the most complete time series. The months of May-September were chosen because these are the months of the warm season in the U.S. and virtually all EH events occurred in these months. Of the 135 cities, we obtained information on air conditioning prevalence in 109 cities as described further below, thereby reducing our sample to 109 cities.
2.2. Health outcomes data
We obtained emergency hospitalizations for individuals 65 years and older during 1992–2006 from the U.S. Centers for Medicare and Medicaid Services MedPAR billing records. We created indicator variables for male sex (Male), black race (Black), and aged 78 years and older vs. 65–78 years (Aged 78+). The age cut point of 78 years was the median age in the study sample. We categorized hospitalizations with the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) admission codes of 580–589 (renal, primary admission code only), 992 (effects of heat and light, primary and secondary) and E900.0 (excessive heat due to weather conditions, primary and secondary) as “renal/heat.” In addition to analyzing a combination of these three categories (renal/heat/respiratory), we combined renal and heat admissions into a single category because each category individually comprised too few daily admissions to provide sufficient power to assess effect modification (Gronlund et al. 2014). Additionally, in previous analyses (Gronlund et al. 2014), associations between EH and respiratory, but not renal, hospitalizations differed by climate zone. Furthermore, we might expect certain potential effect modifiers, such as housing age and non-green space, to act differently on respiratory vs. renal/heat hospitalizations given the potential independent effects on respiratory health of poor housing conditions and tree and grass pollen. Therefore, among the causes for which we previously found an association with EH, we analyzed respiratory (ICD-9-CM codes 480–487, 490–492 and 494–496, primary) separately from non-respiratory (i.e., renal/heat) hospitalizations.
2.3. Area-level data
We obtained the following ZIP-code characteristics from Decennial Census Long Form data in 2000 ZIP Code Tabulation Areas (ZCTAs, polygons constructed by the U.S. Census Bureau approximating ZIP codes), for 1990 and 2000 (Geolytics, Inc. 2006): percentages of residents of black race (% Black), residents without a high school degree (% No HS), households below the poverty level (% Poverty) and households in structures built before 1940 (% Built < 1940). We chose 1939 or earlier as our oldest housing category because the U.S. Census has previously used this as a definition of “old” housing (Bennefield and Bonnette 2003). Additionally, in an analysis of the 1999 American Housing Survey data obtained for this study, 80% of homes built before 1940 did not have central AC while only 40% of homes built in 1940 or later lacked central AC (U.S. Census Bureau 2008). Although we also tested for individual effects of black race, we included the ZIP-code level measure of race, as well, to distinguish area-level, or neighborhood effects, from individual effects.
Land cover classifications at a resolution of 30 × 30 m were obtained from the Multi-Resolution Land Characteristics Consortium for 1992 and 2001, and percent area non-green space in each ZIP code (% Non-Green) was calculated as the percentage of 30 × 30 m pixels that were not classified as open water, developed open space (mostly lawn grasses), forest, shrubland, scrub, agricultural, grasses or wetlands.
We obtained annual ACP for 109 of the study cities from 1985–2005 from the American Housing Survey (U.S. Census Bureau 2008). We assigned the corresponding Metropolitan Statistical Area ACP when the county ACP was not available, and we averaged the county values to obtain a citywide value. We used the ACP in 1999 as our measure of ACP, and when missing, ACP in 1999 was linearly interpolated from the preceding and following annual values for that city. We tested the sensitivity of our results to using ACP in only 1999 by modeling ACP as the mean of the available annual ACPs within each city.
We estimated annual values for land cover and socio-demographic characteristics for each ZIP code as the value from the nearest year of available data, 1992 or 2006 for the land cover data or 1990 or 2000 for the Census socio-demographic data.
2.4. Statistical analysis
We used a time-stratified case-crossover design as previously described (Medina-Ramon et al. 2007) to evaluate the association between heat and hospitalizations in each city for May-September. In a time-stratified case-crossover design, cases serve as their own controls on days other than the day on which the hospitalization occurred (case day) but within the same “time strata,” which were defined here as the same month and day-of-week as the case day. In this study design, appropriate for short-term health effects and short-term exposures, characteristics that are non- or slowly-time varying are automatically controlled for. We applied conditional logistic regression using the coxph function in the survival package in R.
In previous work, we extensively studied the functional relationship between EH and hospitalizations up to 7 days following the EH in this sample of elderly individuals. In general, associations between renal and respiratory hospitalizations increased at a nonlinear, progressively increasing rate between the 90th and 99th percentiles of city-specific daily temperature, with little difference in results depending on whether we used minimum, mean, maximum or apparent temperature (Gronlund et al. 2014). Therefore, we modeled temperature as a step function, or three binary categories, with steps at the city-specific 0–90th percentiles of daily maximum temperature, 90th–97th percentiles (moderate heat, MH) and above the 97th percentiles (EH). Temperature percentiles were calculated from each city’s distribution from 1992–2006. We modeled temperature as a step instead of continuous function to restrict our analyses to “discordant sets,” or instances where any exposures differed between the matched case and controls, making analysis of the largest cities computationally feasible by minimizing the size of the analysis dataset while still allowing for a nonlinear dose-response relationship. Note that in matched designs, only discordant sets contribute information. We modeled temperature exposure as means of daily temperature lags to reduce collinearity between lags. Specifically, we used the following lags for MH and EH: 0–1 (the day of and prior to hospital admission) and 2–5 (2 to 5 days before hospital admission). We chose these lags based on the significant positive EH effects seen through lag day 5 in previous research (Gronlund et al. 2014). Collinearity was thus reduced given that, for example, EH01 and EH25 are less correlated as compared to the independent EH on lag days 0, 1 and 2, which are highly correlated. This lag structure also allowed the strengths and directions of effects to vary between the short term (mean of lags 0–1) and a slightly longer time period (mean of lags 2–5) with a small enough number of terms to perform a multivariate meta-analysis on 109 cities.
First, we examined effect modification by individual (Male, Black, Aged 78+) and area-level characteristics (% Black, % No HS, % Poverty and % Built < 1940). We examined effect modification by including interaction terms between each of the two EH lags (EH01 and EH25) and each potential effect modifier. Effect modifiers can confound other effect modifiers (see Section 1 for definitions of confounding and effect modification), and given our large sample size, we were able to control for confounding among these potential effect modifiers by including multiple interaction terms together in the same model. We included interactions between each of the potential modifiers and both of the EH time lags to provide for either potential differences in vulnerability by lag or potential short-term declines in hospitalizations in the 2–5 days following EH within each category of modifier. In addition to parameters for each matched set of case and controls which were conditioned out of the likelihood function, we modeled:
| [1] |
where EM1–EM3 were indicator variables Male, Black and Aged 78+, respectively, and EM4–EM8 were ZIP-code “% Non-Green,” “% No HS,” “% Black” and “% Built < 1940,” respectively, modeled simultaneously (Gronlund et al. 2015). We also considered models with “% Poverty” instead of “% No HS” as the measure of socioeconomic status.
To estimate pooled effects across cities and evaluate how city-level ACP modified the effects of individual- and ZIP-code characteristics, we regressed city-specific model coefficients against quartiles of citywide percent ACP in 1999 in a second-stage multivariate random effect meta-analysis using the method of moments, which is a simple extension of Dersimonian and Laird’s inverse-weighted random effects meta analysis to the multivariate setting (Jackson et al. 2010, Gasparrini et al. 2012). Meta-analyses were performed using the mvmeta package in R 2.15. From the meta-analyses, for each cause of admission for each ACP quartile, we presented the effect of EH over two days (the main EH01 effect) pooled across cities and the cumulative effect of EH over six days in total (the sum of the EH01 and EH25 effects) pooled as well as by ACP quartile, holding all the modifiers at their respective study-wide median values. We also estimated the effects for high and low values (1 and 0 for the individual-level or 75th and 25th study-wide percentiles for the ZIP-code-level characteristics) holding remaining modifiers at their median values. Variances were estimated using the delta method on the within-city covariance matrix resulting from the meta analysis, and covariances were specified for each ACP level. The hospitalization events were rare, so the estimated odds ratios (ORs) were assumed to approximate risk ratios, and percent increase in risk was estimated as (OR – 1) * 100%.
We also assessed multicollinearity, or whether the terms in our model were highly correlated such that any term was well predicted by the remaining terms in the model. In this undesirable circumstance, the effect estimates are highly sensitive to minor changes in the model or data. Variance inflation factors (VIFs, 1/1 – R2) were calculated among each city’s cases by regressing each term in equation 1 on the other terms. VIFs were below 10, except for black or “% Black” in 22 cities (Figure S1). These two characteristics were excluded from the models for these 22 cities, and the variances and covariances for these terms were replaced with very high within-study variances to minimize their contribution to the meta-analysis (Jackson et al. 2010, Gasparrini et al. 2012).
In previous research of the associations between EH and hospitalizations in this case series of Medicare recipients, we did not find confounding of the EH-hospitalization association by ozone or holidays (Gronlund et al. 2014). In the present analysis, to test for potential spatial autocorrelation, we examined the sensitivity of our results in five large cities representing a wide range of ACPs, New York City, NY, Chicago, IL, Houston, TX, Los Angeles, CA and Minneapolis, MN, to estimating robust standard errors clustered on ZIP code.
3. Results
3.1. Individual, ZIP code and city characteristics
The 109 study cities were distributed widely across the U.S. (Figure S1). Among the cities, the mean daily number of hospitalizations for renal or heat-related causes ranged from 0.1 to 6.8 hospitalizations and 1.0–49.0 for respiratory causes (Table 1). The percentage of hospitalizations among individuals aged 78+ years ranged widely (38%–60%), and the percentage of hospitalizations among black individuals ranged even more widely (5.2%–66.2%). City-specific thresholds for EH also differed greatly, from, e.g., 28.6 °C (San Diego, CA) to 44.4 °C (Phoenix, AZ) for the 97th percentile of temperature. Among the study ZIP codes, the full range of percentages (0–100%) of each characteristic was represented. ACP ranged widely and was evenly distributed among the study cities. The 90th percentile of daily maximum temperature and ACP were moderately correlated (r = 0.70).
Table 1.
Characteristics of patients 65 years and older admitted to the hospital, temperature, and ZIP code characteristics in 109 U.S. cities and 8,200 ZIP codes, May–September, 1992–2006.
| Minimum | 25th percentile | Median | 75th percentile | Maximum | |
|---|---|---|---|---|---|
| Citywide mean daily number of hospitalizationsa | |||||
|
| |||||
| Renal/heat | 0.1 | 0.4 | 0.6 | 1.2 | 6.8 |
| Respiratory | 1.0 | 2.5 | 4.2 | 7.0 | 49.0 |
|
| |||||
| Patient characteristics (citywide percent of respiratory, renal and heat cases) | |||||
|
| |||||
| Aged > 78 years | 38.1 | 46.2 | 49.5 | 51.2 | 60.0 |
| Male | 39.2 | 43.8 | 45.5 | 47.4 | 55.0 |
| Black race | 5.2 | 11.5 | 16.1 | 28.5 | 66.2 |
|
| |||||
| Daily citywide exposures, °C | |||||
|
| |||||
| 90th percentile of maximum daily temperature | 25.8 | 30.6 | 32.9 | 34.7 | 43.1 |
| 97th percentile of maximum daily temperature | 28.6 | 33.1 | 34.7 | 36.1 | 44.4 |
|
| |||||
| ZIP code characteristics | |||||
|
| |||||
| Percent non-green space (% Non-Green) | 0.0 | 10.0 | 38.6 | 73.9 | 100.0 |
| Percent of residents without a high school degree (% No HS) | 0.0 | 9.8 | 16.4 | 26.1 | 100.0 |
| Percent of residents of black race (% Black) | 0.0 | 0.7 | 2.8 | 10.4 | 100.0 |
| Percent of residents below poverty level (%Poverty) | 0.0 | 4.2 | 7.5 | 14.4 | 100.0 |
| Percent of households in structures built before 1940 (% Built < 1940) | 0.0 | 2.7 | 11.4 | 27.4 | 100.0 |
|
| |||||
| Citywide percent of households with central air conditioning in 1999 (ACP) | 4.9 | 33.1 | 63.6 | 81.0 | 96.4 |
ICD-9-CM primary admission codes: renal/heat: 580–589, 992 or E900.0; respiratory: 480–487, 490–492, 494–496. Counts of hospitalizations for heat causes also include hospitalizations with any contributing causes coded as heat-related.
The ZIP code characteristics were weakly to moderately correlated with each other (r = 0–0.58, Table S1), with the exception of “% Poverty” and “% No HS,” which were more strongly correlated (r = 0.72).
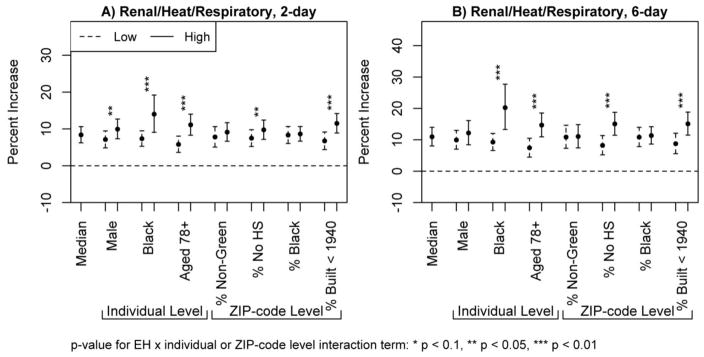
3.2. Main EH effects
For the two-day EH effects vs. non-heat, EH was associated with an 8% (95% CI 6%-11%) increase in hospitalizations for renal/heat/respiratory causes (Median effect, Figure 1A). For the six-day cumulative EH effects vs. non-heat, associations between EH and renal/heat/respiratory hospitalizations were even stronger than for two-day EH effects, with a 11% (95% CI 8%–14%) increase in hospitalizations (Median effect, Figure 1B).
Figure 1.
Percent increases and 95% confidence intervals for admission to the hospital for renal, heat or respiratory causes among individuals aged 65 years and older for the two-day (A) or six-day (B) cumulative effects of extreme heat (EH, temperature > 97th percentile) vs. non-heat (temperature < 90th percentile) among individuals with (high) or without (low) the characteristic (individual level) or among individuals residing in ZIP codes in the 75th percentile (high) or 25th percentile (low) of the characteristic (ZIP-code level), holding the other characteristics at the study-wide median values, May–September, 1992–2006.
3.3 Effect modification by individual and ZIP-code characteristics
3.3.1 Two-day effects
The associations between EH on lag days 0–1 with renal/heat/respiratory hospitalizations were significantly greater among men, blacks, individuals aged 78+ years and in ZIP codes with high “% Built < 1940” (Figure 1A). For example, among blacks, EH was associated with a 14% (95% CI 9%–19%) increase in hospitalizations for renal/heat/respiratory causes, while among non-blacks, EH was associated with a 7% (95% CI 5%–9%) increase in renal/heat/respiratory hospitalizations.
3.3.2. Six-day cumulative effects
The modification seen for two-day EH effects by sex did not persist when we considered the cumulative effects of EH over six days (Figure 1B). However, individual age, black race and ZIP code “% Built < 1940” continued to significantly modify the associations between renal/heat/respiratory hospitalizations over the six days following EH. Specifically, we observed a 20% (95% CI 13–28%) increase in renal/heat/respiratory hospitalizations among blacks, a 15% (95% CI 11%–19%) increase in renal/heat/respiratory hospitalizations among individuals aged 78+ years, a 15% (95% CI 11%–19%) increase in ZIP codes with high “% No HS” and a 15% (95% CI 11%–19%) increase in ZIP codes with high “% Built < 1940” for EH vs. non-heat. In contrast, among non-black individuals, individuals aged 65–77 years or residents of ZIP codes with low “% no HS” or low “% Built < 1940,” the increases in renal/heat hospitalizations during EH vs. non-heat were each lower at 9% (95% CI 7%–12%), 7% (95% CI 4%–10%), 8% (95% CI 5%–11%) and 9% (95% CI 6–12%), respectively. Nevertheless, the effects were still significantly greater than 0.
When examining socioeconomic status modification using “% Poverty” instead of “% No HS,” results were similar (Figure S3). Results in five large cities were virtually identical when using robust standard errors clustered on ZIP code (results not shown).
3.3.3 Specific causes: Renal/heat and respiratory hospitalization
Generally, the directions of the modifying effects of each of the individual and ZIP-code characteristics on the associations between renal/heat and respiratory hospitalizations and EH were the same as when the three categories were grouped together (Figure S2). However, these effects were sometimes not significant in the more specific groupings of hospitalization causes, for which sample sizes were reduced. As an exception, for renal/heat and respiratory hospitalizations, “% Built < 1940” still significantly modified the association between EH and hospitalization (Figure S2). Additionally, the increased association between hospitalization and EH among men was strongly significant (p < 0.01) for respiratory hospitalizations only. However, the odds of respiratory hospitalization for EH vs. non-EH were 0.9% greater for women vs. men over lag days 2–5, offsetting the male-female difference observed at lag days 0–1 (Figure S2). Therefore, for the six-day cumulative effects, male sex did not modify associations between EH and hospitalizations for either respiratory or renal/heat causes.
3.4. Effect modification by ACP
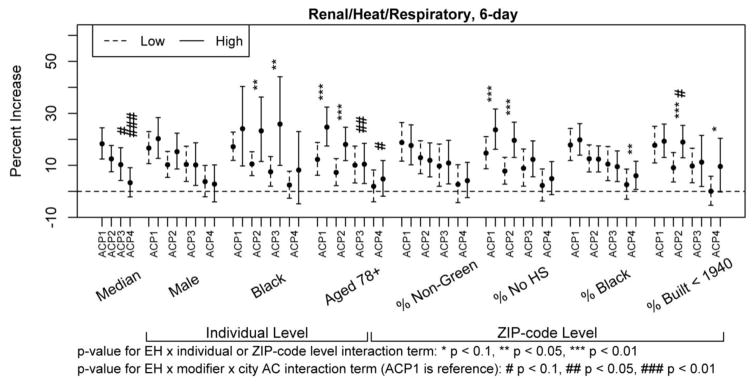
3.4.1 Overall modifying effects of ACP
For the six-day cumulative EH effects on renal/heat/respiratory hospitalizations, associations between EH and hospitalization decreased as ACP increased, even when accounting for the other modifying characteristics (Figure 2). For example, in the fourth quartile of ACP, the association between hospitalization with EH was null (3%, 95% CI = −2%–9%) while in the first quartile of ACP, EH vs. non-heat was associated with an 18% (95% CI 12%–24%) increased risk of hospitalization for renal/heat/respiratory causes.
Figure 2.
Percent increases and 95% confidence intervals for admission to the hospital for renal, heat or respiratory causes among individuals aged 65 years and older for the six-day cumulative effects of extreme heat (EH, temperature > 97th percentile) vs. non-heat (temperature < 90th percentile) among individuals with (high) or without (low) the characteristic (individual level) or among individuals residing in ZIP codes in the 75th percentile (high) or 25th percentile (low) of the characteristic (ZIP-code level), holding the other characteristics at the study-wide median values, by quartiles of citywide air conditioning prevalence (ACP), May–September, 1992–2006. (See Table S2 for corresponding values.)
3.4.2 Modifying effects of ACP on individual and ZIP-code effects
The modifying effects of the individual and ZIP code characteristics did not differ by quartile of ACP, for the most part (Figure 2). The exception was for age. The modifying effects by age of the EH-hospitalizations association were stronger in ACP quartiles 1 and 2 as compared to ACP quartiles 3 and 4. For example, in ACP quartile 1, among individuals aged 78+ years, EH vs. non-heat was associated with a 24% (95% CI 17%–32%) increase in renal/heat/respiratory hospitalizations as compared to a 12% (95% CI 6%–19%) increase among individuals aged 65–77 years, while in ACP quartile 4, the associations between EH and hospitalization were null in both age groups. These results were not sensitive to assigning quartiles of ACP according to the mean of the annual ACPs instead of according to the 1999 ACP value (Figure S4).
4. Discussion
Associations between EH and hospitalizations in the U.S. differed by individual- and ZIP-code-level characteristics, city-level ACP, and lag time since EH exposure.
4.1. Vulnerability by ACP and housing
Both ZIP-code-level housing age and city-level ACP modified associations between EH and renal/heat/respiratory hospitalizations in models accounting for multiple individual and ZIP code characteristics. We were limited in our lack of information on individual- or ZIP-code-level AC ownership and use. However, in addition to city ACP, the individual and ZIP code characteristics, particularly housing age, may have proxied AC ownership. In prior studies, vulnerability to heat was greater in cities with lower ACP (Gronlund 2014) or in California ZIP codes with lower AC ownership and use (Ostro et al. 2010). Additionally, as described above, in the American Housing Survey data obtained for this study, central AC ownership was much higher in houses built in or after 1940 than in those built before 1940. Therefore, the pronounced vulnerability to EH-associated renal/heat/respiratory hospitalizations among residents of ZIP codes with high “% Built < 1940” may be related to an absence of central AC in older homes.
Our results were not sensitive to whether we assigned ACP as the value from 1999 or the average of the available annual values. However, due to our analytic methods, we were limited to modeling ACP as a time-invariant characteristic. In fact, ACP has been increasing over time in the U.S., and a previous study of mortality and heat in the U.S. did not find greater declines in the risk of heat-related mortality among cities with larger increases in ACP (Bobb et al. 2014). This suggests that ACP may currently play a less important role in heat adaptation than our results suggest. However, the potentially greater limitation is our lack of individual- or neighborhood-level AC exposure information.
4.2. Vulnerability among the very old and men
Consistent with other studies of heat and health (Basu 2009), we observed an increased association between EH and hospitalization among the very old. Older age may represent diminished cardiovascular capacity and thermoregulatory responses to EH among the individuals whose hospitalizations were for renal/heat and for respiratory causes.
Care-seeking behaviors may differ between men and women, but it is not clear why we observed differences in the increase in respiratory hospitalizations between men and women at only the shortest lag and why we did not observe a similar pattern for renal/heat hospitalizations. Nevertheless, disparities in EH-associated hospitalization rates that persist for only two days are potentially of less policy relevance than disparities that persist for months or years. Therefore, these results suggest that future studies of EH vulnerability should consider cumulative multi-day vulnerability, as we did. We did not consider lag periods longer than 6 days in this study, but future research should examine a longer time course of EH-associated morbidity.
4.3. Vulnerability by area-level socioeconomic status and race
Many prior studies have explored vulnerability to heat by socioeconomic status, race and/or ethnicity, and results for vulnerability according to race or ethnicity in the U.S. have been inconsistent across studies (Gronlund 2014). In particular, in California, the differences in the excess risk of emergency room visit according to whether the patient was white, Hispanic, black or Asian differed in magnitude and direction according to the cause of admission. For example, fewer heat-associated respiratory but more heat-associated ischemic stroke visits occurred among Hispanics vs. whites (Basu et al. 2012).
One strength of our study was our simultaneous control of multiple individual and area confounders, and with this control, we did not find significant effects of an area measure of race. However, we did find significantly greater effects of EH on hospitalization for renal, heat or respiratory causes among blacks. Presumably, EH-associated hospitalizations for particular causes reflect increased vulnerability to EH among individuals with that pre-existing health condition rather than a new onset of renal or respiratory disease. Therefore, one explanation for the increased association between EH and renal/heat/respiratory hospitalizations among blacks may be poorer general health among blacks than non-blacks, even among individuals with pre-existing renal or respiratory conditions. For example, race was predictive of lower functional level among 520 individuals with advanced chronic obstructive pulmonary disease (Rambod et al. 2012). In turn, poorer health may be related to lower health care utilization and less treatment among blacks than whites (Shaya et al. 2009, Kirkpatrick et al. 2009).
Individuals of low socioeconomic status, as measured by education, income or a latent construct, are often found to be more vulnerable to EH (Anderson et al. 2009, Fletcher et al. 2012, Madrigano et al. 2013, O’Neill et al. 2003, Zanobetti et al. 2013). Vulnerability by education or poverty was present in our study despite control for area housing age and imperviousness, suggesting pathways of socioeconomic vulnerability beyond built environment characteristics. However, our ZIP-code level measures of socioeconomic status and built environment characteristics were coarse, and future research should use more finely spatially resolved health and exposure information.
4.4. Lack of vulnerability by non-green space
We expected non-green space to strongly predict heat-related health effects given that canopy cover, vegetation, imperviousness and land development predict much intra-regional temperature variation (Hart et al. 2009, Kloog et al. 2012, Oswald et al. 2012, Zhou et al. 2014). However, non-green space was not a modifier in any model at any lag in our study. This is inconsistent with other studies which found differential vulnerability to heat-associated mortality in Michigan, Phoenix, Arizona and Barcelona, Spain by perception of green space, vegetation or imperviousness, even with control for other socioeconomic characteristics (Gronlund et al. 2015, Harlan et al. 2013, Xu et al. 2013), although in Barcelona, the measured, as opposed to perceived, tree cover in a census tract was not a significant modifier. Uejio and colleagues (2011) also found imperviousness in a census block group (smaller than a ZIP code) to predict heat distress ambulance calls in Phoenix, Arizona but not heat-related mortality in Philadelphia, Pennsylvania. This absence of effect modification may reflect true absence of increased vulnerability with higher non-green space. However, this may also simply reflect exposure misclassification in our use of spatially coarse land cover information, which is a substantial limitation of our study.
4.6. Additional Limitations
Additional limitations included potential misclassification of our main EH effect, given our use of temperatures from the nearest airport instead of finely-spatially resolved EH exposure. Our main EH exposure may also have been temporally misclassified, considering we didn’t know the date or time of the onset of the condition which eventually led to each individual’s hospitalization. Additionally, the ICD codes used for classifying hospitalizations as due to renal, heat or respiratory disease could have been inaccurate, although we chose broad categories to minimize this potential misclassification.
4.5 Conclusion
In conclusion, we observed increased vulnerability among the elderly to EH-associated hospitalization for renal and heat and/or respiratory causes among the very old; among blacks; among individuals in ZIP codes with high percentages of residents of low socioeconomic status and housing built before 1940; and in cities with lower ACP. For several characteristics, information was only available at a level of ZIP code or city, and analyses using more finely resolved spatial information are important to better understand individual and neighborhood level characteristics of vulnerability. Given our nationwide sample of elderly Medicare beneficiaries, our results are highly generalizable across the U.S. Our findings may be helpful to communities in adapting to climate change.
Supplementary Material
Acknowledgments
This research was supported by the following grants: U.S. Environmental Protection Agency Science to Achieve Results Program R832752010; a National Occupational Research Agenda Pre-Doctoral Scholarship from the University of Michigan Center for Occupational Health and Safety Engineering (a National Institute for Occupational Safety and Health-funded Education and Research Center 2T42OH008455); the National Institute on Aging Interdisciplinary Research Training in Health and Aging T32AG027708; the U.S. Centers for Disease Control and Prevention EH000348, the National Institute of Environmental Health Sciences ES015774, ES024012, R21-ES020156 and R21-ES020695 and a Dow Sustainability Fellowship from the University of Michigan Graham Environmental Sustainability Institute.
Footnotes
Author Attributions
Each author contributed to the study design; acquisition or processing of the health and/or exposure data; analysis and manuscript preparation and editing.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Compliance with Ethical Standards: The research was approved by the Institutional Review Boards at Harvard University and University of Michigan. Informed consent of subjects was waived.
References
- Anderson GB, Bell ML. Weather-related mortality: A study of how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009:205–213. doi: 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R. High ambient temperature and mortality: a review of epidemiological studies from 2001 to 2008. Environ Health. 2009:40. doi: 10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R, Ostro BD. A multicounty analysis identifying the populations vulnerable to mortality associated with high ambient temperature in California. Am J Epidemiol. 2008:632–7. doi: 10.1093/aje/kwn170. [DOI] [PubMed] [Google Scholar]
- Basu R, Pearson D, Malig B, Broadwin R, Green R. The effect of high ambient temperature on emergency room visits. Epidemiology. 2012:813–20. doi: 10.1097/EDE.0b013e31826b7f97. [DOI] [PubMed] [Google Scholar]
- Bennefield R, Bonnette R. Census 2000 Brief. U.S. Department of Commerce, Economics and Statistics Administration,, U.S. Census Bureau; 2003. Structural and Occupancy Characteristics of Housing: 2000. [Google Scholar]
- Bhaskaran K. The effects of ambient temperature on the incidence of myocardial infarction - A systematic review. Heart. 2009:1760–9. doi: 10.1136/hrt.2009.175000. [DOI] [PubMed] [Google Scholar]
- Bierbaum R, Smith J, Lee A, et al. A comprehensive review of climate adaptation in the United States: more than before, but less than needed. Mitig Adapt Strateg Glob Change. 2013:361–406. doi: 10.1007/s11027-012-9423-1. [DOI] [Google Scholar]
- Bobb JF, Peng RD, Bell ML, Dominici F. Heat-related mortality and adaptation to heat in the United States. Environ Health Perspect. 2014:811–6. doi: 10.1289/ehp.1307392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher BA, Lin S, Fitzgerald EF, Hwang SA. Association of Summer Temperatures With Hospital Admissions for Renal Diseases in New York State: A Case-Crossover Study. Am J Epidemiol. 2012:907–16. doi: 10.1093/aje/kwr417. [DOI] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward MG. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat Med. 2012:3821–3839. doi: 10.1002/sim.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geolytics, Inc. Planners Package: Census 2000 Long Form (SF3) and 1990 Form in 2000 Boundaries. Geolytics, Inc; East Brunswick, NJ: 2006. [Google Scholar]
- Gosling S, Lowe J, McGregor G, Pelling M, Malamud B. Associations between elevated atmospheric temperature and human mortality: a critical review of the literature. Clim Change. 2009:299–341. [Google Scholar]
- Green R, Basu R, Malig B, et al. The effect of temperature on hospital admissions in nine California counties. Int J Public Health. 2010:113–121. doi: 10.1007/s00038-009-0076-0. [DOI] [PubMed] [Google Scholar]
- Greenland S, Rothman KJ, Lash TL. Ch 4: Measures of Effect and Measures of Association. In: Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology: Third Edition. Lippincott Williams & Wilkins; Philadelphia, PA: 2008. pp. 51–70. [Google Scholar]
- Gronlund CJ. Racial and socioeconomic disparities in heat-related health effects and their mechanisms: a review. Curr Epidemiol Rep. 2014 doi: 10.1007/s40471-014-0014-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronlund CJ, Zanobetti A, Schwartz JD, Wellenius GA, O’Neill MS. Heat, heat waves and hospital admissions among the elderly in the United States, 1992–2006. Environ Health Perspect. 2014:1187–1192. doi: 10.1289/ehp.1206132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronlund CJ, Berrocal VJ, White-Newsome JL, Conlon KC, O’Neill MS. Vulnerability to extreme heat by socio-demographic characteristics and area green space among the elderly in Michigan, 1990–2007. Environ Res. 2015:449–461. doi: 10.1016/j.envres.2014.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat S, Kosatsky T. Heat-related mortality: a review and exploration of heterogeneity. J Epidemiol Community Health. 2010:753–60. doi: 10.1136/jech.2009.087999. [DOI] [PubMed] [Google Scholar]
- Harlan SL, Declet-Barreto JH, Stefanov WL, Petitti DB. Neighborhood Effects on Heat Deaths: Social and Environmental Predictors of Vulnerability in Maricopa County, Arizona. Environ Health Perspect. 2013:197–204. doi: 10.1289/ehp.1104625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart M, Sailor D. Quantifying the influence of land-use and surface characteristics on spatial variability in the urban heat island. Theor Appl Climatol. 2009:397–406. doi: 10.1007/s00704-008-0017-5. [DOI] [Google Scholar]
- IPCC. Summary for Policymakers. In: Stocker TF, Qin D, Plattner G-K, et al., editors. Climate Change 2013: The Physical Science Basis Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press; United Kingdom and New York, NY: 2013. [Google Scholar]
- Jackson D, White IR, Thompson SG. Extending DerSimonian and Laird’s methodology to perform multivariate random effects meta-analyses. Stat Med. 2010:1282–97. doi: 10.1002/sim.3602. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick dP, Dransfield MT. Racial and sex differences in chronic obstructive pulmonary disease susceptibility, diagnosis, and treatment. Curr Opin Pulm Med. 2009:100–4. doi: 10.1097/MCP.0b013e3283232825. [DOI] [PubMed] [Google Scholar]
- Kloog I, Chudnovsky A, Koutrakis P, Schwartz J. Temporal and spatial assessments of minimum air temperature using satellite surface temperature measurements in Massachusetts, USA. Sci Total Environ. 2012:85–92. doi: 10.1016/j.scitotenv.2012.05.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S, Luo M, Walker RJ, Liu X, Hwang SA, Chinery R. Extreme High Temperatures and Hospital Admissions for Respiratory and Cardiovascular Diseases. Epidemiology. 2009:738–746. doi: 10.1097/EDE.0b013e3181ad5522. [DOI] [PubMed] [Google Scholar]
- Madrigano J, Mittleman MA, Baccarelli A, et al. Temperature, myocardial infarction, and mortality: effect modification by individual- and area-level characteristics. Epidemiology. 2013:439–46. doi: 10.1097/EDE.0b013e3182878397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina-Ramon M, Zanobetti A, Cavanagh DP, Schwartz J. Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect. 2006:1331–1336. doi: 10.1289/ehp.9074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina-Ramon M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatization and effect modification in 50 United States cities. Occup Environ Med. 2007:827–833. doi: 10.1136/oem.2007.033175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morenoff JD, Lynch JW. National Research Council (US) Panel on Race, Ethnicity, and Health in Later Life, editor. Chapter 11: What Makes a Place Healthy? Neighborhood Influences on Racial/ Ethnic Disparities in Health over the Life Course. In: Anderson N, Bulatao R, Cohen B, editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. National Academies Press (US); Washington DC: 2004. [PubMed] [Google Scholar]
- Noe RS, Jin JO, Wolkin AF. Exposure to natural cold and heat: hypothermia and hyperthermia Medicare claims, United States, 2004–2005. Am J Public Health. 2012:e11–8. doi: 10.2105/AJPH.2011.300557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill MS, Zanobetti A, Schwartz J. Modifiers of the temperature and mortality association in seven US cities. Am J Epidemiol. 2003:1074–1082. doi: 10.1093/aje/kwg096. [DOI] [PubMed] [Google Scholar]
- Ostro B, Rauch S, Green R, Malig B, Basu R. The effects of temperature and use of air conditioning on hospitalizations. Am J Epidemiol. 2010:1053–61. doi: 10.1093/aje/kwq231. [DOI] [PubMed] [Google Scholar]
- Oswald EM, Rood RB, Zhang K, et al. An investigation into the spatial variability of near-surface air temperatures in the Detroit, MI metropolitan region. J Appl Meteorol Climatol. 2012:1290–1304. doi: 10.1175/JAMC-D-11-0127.1. [DOI] [Google Scholar]
- Pillai SK, Noe RS, Murphy MW, et al. Heat Illness: Predictors of Hospital Admissions Among Emergency Department Visits-Georgia, 2002–2008. J Community Health. 2014 doi: 10.1007/s10900-013-9743-4. [DOI] [PubMed] [Google Scholar]
- Rambod M, Porszasz J, Make BJ, Crapo JD, Casaburi R. Six-minute walk distance predictors, including CT scan measures, in the COPDGene cohort. Chest. 2012:867–75. doi: 10.1378/chest.11-0870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Lash TL. Ch 9: Validity in Epidemiology Studies. In: Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology: Third Edition. Lippincott Williams & Wilkins; Philadelphia, PA: 2008. pp. 128–147. [Google Scholar]
- Sampson N, Gronlund CJ, Buxton MA, et al. Staying cool in a changing climate: Reaching vulnerable populations during heat events. Global Environ Chang. 2013:475–484. doi: 10.1016/j.gloenvcha.2012.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J. Who is sensitive to extremes of temperature?: A case-only analysis. Epidemiology. 2005:67–72. doi: 10.1097/01.ede.0000147114.25957.71. [DOI] [PubMed] [Google Scholar]
- Semenza JC, Rubin CH, Falter KH, et al. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med. 1996:84–90. doi: 10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- Shaya FT, Maneval MS, Gbarayor CM, et al. Burden of COPD, asthma, and concomitant COPD and asthma among adults: racial disparities in a Medicaid population. Chest. 2009:405–11. doi: 10.1378/chest.08-2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smargiassi A, Goldberg MS, Plante C, Fournier M, Baudouin Y, Kosatsky T. Variation of daily warm season mortality as a function of micro-urban heat islands. J Epidemiol Commun H. 2009:659–64. doi: 10.1136/jech.2008.078147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner LR, Barnett AG, Connell D, Tong S. Ambient Temperature and Cardiorespiratory Morbidity: A Systematic Review and Meta-analysis. Epidemiology. 2012:594–606. doi: 10.1097/EDE.0b013e3182572795. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau, Housing and Household Economic Statistics Division. American Housing Survey (AHS) 2008. [Google Scholar]
- Uejio CK, Wilhelmi OV, Golden JS, Mills DM, Gulino SP, Samenow JP. Intra-urban societal vulnerability to extreme heat: The role of heat exposure and the built environment, socioeconomics, and neighborhood stability. Health Place. 2011:498–507. doi: 10.1016/j.healthplace.2010.12.005. [DOI] [PubMed] [Google Scholar]
- Vandentorren S, Croisier A, Declercq B, et al. August 2003 heat wave in France: risk factors for death of elderly people living at home. Eur J Public Health. 2006:583–91. doi: 10.1093/eurpub/ckl063. [DOI] [PubMed] [Google Scholar]
- White-Newsome JL, McCormick S, Sampson N, et al. Strategies to reduce the harmful effects of extreme heat events: a four-city study. Int J Environ Res Public Health. 2014:1960–88. doi: 10.3390/ijerph110201960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y, Dadvand P, Barrera-Gomez J, et al. Differences on the effect of heat waves on mortality by sociodemographic and urban landscape characteristics. J Epidemiol Commun H. 2013:519–25. doi: 10.1136/jech-2012-201899. [DOI] [PubMed] [Google Scholar]
- Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S. Ambient Temperature and Morbidity: A Review of Epidemiological Evidence. Environ Health Perspect. 2012:19–28. doi: 10.1289/ehp.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanobetti A, O’Neill MS, Gronlund CJ, Schwartz JD. Susceptibility to mortality in weather extremes: Assessing effect modification by zipcode area level characteristic, personal characteristics and specific cause of admission in a multi-city case-only analysis. Epidemiology. 2013:809–19. doi: 10.1097/01.ede.0000434432.06765.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou W, Ji S, Chen TH, Hou Y, Zhang K. The 2011 heat wave in Greater Houston: Effects of land use on temperature. Environ Res. 2014:81–87. doi: 10.1016/j.envres.2014.08.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.