Abstract
Background
Little is known about the impact of hospitalization for an acute myocardial infarction (AMI) on subsequent adherence to statins.
Methods and Results
Using administrative claims from a 5% random sample of Medicare beneficiaries, we identified a cohort of Medicare patients ≥65 years, hospitalized from 2007–2011, taking statins in the year before AMI hospitalization (n=6,618). We then determined the proportion of patients nonadherent to statins (proportion of days covered [PDC] <80%) in the year before AMI hospitalization who became statin adherent (PDC ≥80%) in the year after AMI hospitalization. The proportion of statin adherent patients who became nonadherent was also studied. These proportions were compared with patients hospitalized for pneumonia (n=11,471) and patients not hospitalized (n=158,099) in 2010 and 2011. Among patients nonadherent to statins before AMI hospitalization, 37.7% became adherent after discharge. Patients hospitalized for AMI were more likely to become adherent than patients hospitalized for pneumonia (aRR 1.70, 95%CI 1.57–1.84) or patients not hospitalized (aRR 1.79, 95%CI 1.68–1.90). Among patients adherent to statins before AMI hospitalization, 32.6% became nonadherent after discharge. Those hospitalized for AMI were less likely to become nonadherent than those hospitalized for pneumonia (aRR 0.93, 95%CI 0.88–0.98) but more likely to become nonadherent than patients without hospitalizations (aRR 1.41, 95%CI 1.35–1.48).
Conclusions
Among nonadherent patients, hospitalization for AMI was associated with increased likelihood of becoming adherent to statins compared to hospitalization for pneumonia or no hospitalizations. Among adherent patients, hospitalization for AMI was associated with increased likelihood of becoming nonadherent to statins compared to no hospitalizations.
Keywords: prevention, adherence, statins, myocardial infarction
Introduction
Hospitalization for a health event such as an acute myocardial infarction (AMI) has potential to either positively or negatively impact adherence to cardiovascular medications. Hospitalization for AMI may serve as a teachable moment that motivates patients to adopt positive cardiovascular health behaviors including adherence to medications in an effort to prevent further disease.(1–3) However, life-threatening health events may also induce depression, post-traumatic stress disorder, and other forms of psychological distress that are associated with poor adherence to recommended health behaviors.(4–8) Some patients may additionally experience a “post-hospital syndrome” in which they temporarily develop physical and cognitive disabilities as a consequence of the stressfulness of a hospitalization; this syndrome may impair patients’ ability to adhere to a medical regimen following discharge.(9) Challenges that arise during transitions in care from hospital to home may further impede adherence after hospitalization.(10)
Adherence to cardiovascular medications is one of the most important health behaviors after hospitalization for AMI.(11) Poor adherence to statins has been associated with increased risk for recurrent cardiovascular events and mortality, increased healthcare costs, and preventable readmissions.(12–15) Previous studies have documented substantial nonadherence to statins after hospitalization for AMI,(16–18) but few data have been published on changes in adherence to statins from before to after an AMI hospitalization.(19) Determining the impact of an AMI hospitalization on adherence to statins after discharge can guide clinical expectations of statin adherence and can inform the design of interventions to improve adherence.
To increase the understanding of the impact of an AMI hospitalization on adherence to statins, we examined changes in adherence to statins from the year before to the year after hospitalization for an AMI. First, to determine whether changes in statin adherence from before to after hospitalization for AMI suggest an opportunity for a teachable moment, we compared changes in statin adherence experienced by those hospitalized for AMI with a control group of patients hospitalized for a non-cardiovascular problem unassociated with statin use, pneumonia. To ensure that changes in statin adherence after hospitalization for AMI were not due to regression to the mean, we compared patients hospitalized for AMI with a second control group of patients not hospitalized. Finally, to evaluate whether the experience of being hospitalized, in itself, results in worsening adherence, we compared changes in adherence among patients hospitalized for AMI, hospitalized for pneumonia, and patients not hospitalized.
Methods
Sources of Data
We obtained administrative claims on a 5% random sample of Medicare beneficiaries from the Centers for Medicare and Medicaid Services (CMS) Chronic Condition Data Warehouse. Medicare is a federal program that provides health insurance for adults ≥65 years in the United States. Insurance through Medicare is provided as a fee-for-service program or by contracts with healthcare organizations (Part C or Medicare Advantage). Data for the current analyses included claims from Medicare fee-for-service Parts A (inpatient), B (outpatient), and D (prescription drug). Medicare claims and assessment data from Parts A, B, and D are linked by beneficiary across the continuum of care. Beneficiaries with Part C coverage (Medicare managed care) were not included as their claims are not complete. Institutional review boards at the University of Alabama at Birmingham and CMS approved these analyses. Data for these analyses are stored at the University of Alabama at Birmingham.
Patient Population
We identified three cohorts of patients (Supplemental Figure 1). Our main study population included Medicare beneficiaries who were hospitalized for AMI with an admission date on or after January 1, 2007 and a discharge date on or before December 31, 2011. Our first control population included beneficiaries who were hospitalized for pneumonia during this time period but not hospitalized for AMI from 365 days before the pneumonia hospitalization to 182 days after discharge. AMI was defined by International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) code 410.xx (except 410.x2 which indicates a subsequent episode of care) in the primary discharge diagnosis position in Medicare inpatient files. Pneumonia was defined as a hospitalization with an overnight stay with an ICD-9 diagnosis of 480–488.11 in the primary discharge diagnosis position. For these cohorts, patients were required to be between 65 and 110 years at 365 days prior to the date of hospital admission and have at least one fill for a statin between the 182 and 365 days prior to admission so that statin adherence in the year before hospitalization could be calculated over a minimum of 182 days. Additional eligibility criteria included having a duration of hospitalization less than 31 days; having Parts A, B, and D coverage for each month beginning 365 days before hospital admission through 182 days after discharge; living in the U.S.; being in the 5% Medicare sample; and not receiving hospice care during this period. The third cohort included Medicare beneficiaries who were not hospitalized in 2010 and 2011. These patients had to be between 65 and 110 years on January 1, 2010; have at least one statin fill in the 182 to 365 days before January 1, 2011 (i.e., January 1, 2010 to June 30, 2010); have continuous Medicare Parts A, B, D but not C coverage; live in the U.S.; be in the 5% Medicare sample; and not receiving hospice services from January 1, 2010 through June 30, 2011.
Assessment of Statin Adherence
Statin prescription fills were identified in the Medicare Part D claims using National Drug Codes (NDCs). Statins included atorvastatin, fluvastatin, lovastatin, pravastatin, rosuvastatin, and simvastatin. Adherence to statins was calculated using the interval-based proportion of days covered (PDC).(20,21) To calculate the PDC before the AMI hospitalization and, separately, the pneumonia hospitalization, the denominator was the number of days from the first statin fill between 182 to 365 days before hospital admission until the date of hospital admission. The numerator was the total number of days during this period for which the patient had a statin available; if a prescription was filled earlier than the last day supplied by the previous fill, the overlapping supply was added to the end of the last prescription fill.7 Patients were considered to have statins available regardless of brand, dose, or switching types of statins. Adherence after hospitalization was calculated from the date of discharge to 365 days following discharge, date of death, date of loss of Parts A, B, and D coverage or initiation of Part C coverage using the PDC, and an identical approach was applied to the period before hospitalization. Days of supply at the time of hospital admission for the AMI were carried forward and applied to the calculation of PDC after discharge. For those not hospitalized, PDC was calculated from the first statin fill between January 1 and June 30, 2010 through December 31, 2010 and, separately, between January 1, 2011 and December 31, 2011. Patients were categorized a priori as nonadherent (PDC <80%) or adherent (PDC ≥80%) for the time periods before and after AMI or pneumonia hospitalization or January 1, 2011 for the no hospitalization cohort. The 80% cutpoint was used as this has been associated with increased mortality risk(14) and is the convention for studies of adherence to cardiovascular medications.(11,16,22)
Patient Demographic and Clinical Characteristics
Demographic covariates, identified in the Medicare beneficiary summary file, included age, sex, race/ethnicity, urban versus rural residence based on metropolitan statistical area codes, receipt of a low-income subsidy in at least 1 month prior to AMI or pneumonia hospitalization or prior to January 1, 2011 for the not hospitalized cohort. Medicare claims and validated algorithms were used to identify the presence of comorbidities including coronary heart disease, diabetes, chronic kidney disease, depression, dementia, receipt of home care services, and total number of medication classes filled during the period before AMI or pneumonia hospitalization or before January 2011 for those in the not hospitalized cohort.(23–26) Coronary artery bypass graft surgery (CABG) during the AMI hospitalization was also assessed.
Statistical Analysis
Characteristics for patients hospitalized for AMI were calculated by adherence status (adherent versus nonadherent) prior to their hospitalization. Cross-tabulation of adherence status before and after AMI hospitalization was also calculated. This enabled us to compare the percentages of patients who changed from nonadherent to adherent and from adherent to nonadherent in the year before to the year after AMI hospitalization. For comparison, cross-tabulations of adherence status before and after pneumonia hospitalization and, separately, from 2010 to 2011 for patients not hospitalized, were also calculated. The AMI, pneumonia, and no hospitalization cohorts were also pooled to compare changes in adherence status between cohorts.
Among patients who were nonadherent before hospitalization or January 1, 2011 for those not hospitalized, we calculated the relative risk for becoming adherent after AMI hospitalization versus pneumonia hospitalization, AMI hospitalization versus no hospitalization, and pneumonia hospitalization versus no hospitalization. Among patients who were adherent before hospitalization or January 1, 2011 for those not hospitalized, we calculated the relative risks for becoming nonadherent between the three groups. Relative risks were calculated using Poisson regression models with sandwich estimators and adjustment for age, sex, race, eligibility for low-income subsidy, urban residence, area level income, comorbidities (coronary heart disease, diabetes, chronic kidney disease, depression, dementia), number of medication classes, receipt of home health services, and in the nonadherent to adherent analyses only, PDC<50% versus 50%–79%. Poisson regression was used as it provides a direct estimate of the relative risk.(27–29)
To eliminate the influence of small changes in adherence near the 80% threshold when categorizing adherence, sensitivity analyses were conducted in which an improvement in adherence was defined as a change in PDC from <80% to ≥80% with a 10% or larger increase in PDC. Analogously, in sensitivity analyses, a decline in adherence was defined as a change in PDC from ≥80% to <80% with a 10% or larger decrease in PDC. Increases in PDC with cardiovascular medications after AMI of 4% to 6% have been associated with a reduction in rates of first vascular events, suggesting that the choice of a minimum change in statin adherence of at least 10% represents a clinically significant change.(30)
To quantify the change in mean PDC for statins between the periods before and after the AMI hospitalization, we conducted secondary analyses in which we calculated the change in the PDC between the two time periods as a continuous variable. We used linear regression to compare the change in adherence, modeled as a continuous variable, between the two time periods for the patients in the AMI hospitalization cohort versus patients in the pneumonia hospitalization cohort and patients not hospitalized. We conducted these analyses for patients who were nonadherent and, separately, those who were adherent in the first time period. All analyses were conducted using SAS 9.3 (SAS Institute, Research Triangle Park, NC).
Results
Overall, 6,618 Medicare beneficiaries with an AMI hospitalization, 11,471 beneficiaries with a pneumonia hospitalization, and 158,099 beneficiaries without hospitalizations met the study eligibility criteria (Supplemental Figure 1). Compared to patients who were adherent to statins before AMI hospitalization, those who were nonadherent were more likely to be younger, non-white, live in low-income areas, and receive home health services (Table 1). Prior to AMI hospitalization, 36.4% of patients were nonadherent to statins. In comparison, 31.6% of patients were nonadherent prior to pneumonia hospitalization and 28.3% of patients not hospitalized were nonadherent in 2010 (Supplemental Table 1). After AMI hospitalization, the proportion of patients who were nonadherent to statins increased to 43.4%. In comparison, the proportion of patients who were nonadherent after pneumonia hospitalization increased to 48.9% and the proportion of patients who were nonadherent in 2011 increased to 40.6%.
Table 1.
Sociodemographic and Clinical Characteristics According to Level of Statin Adherence in the Year Before Hospitalization for Acute Myocardial Infarction (N=6,618).
| Adherence before AMI hospitalization | ||
|---|---|---|
| Characteristic | Nonadherent; PDC<80% (N=2,408; 36.4%) | Adherent; PDC ≥80% (N=4,210; 63.6%) |
| Age, in years | ||
| 65–69 | 458 (19.0) | 709 (16.8) |
| 70–74 | 584 (24.3) | 904 (21.5) |
| 75–79 | 532 (22.1) | 915 (21.7) |
| 80–84 | 445 (18.5) | 810 (19.2) |
| 85–110 | 389 (16.2) | 872 (20.7) |
| Female gender | 1,378 (57.2) | 2,324 (55.2) |
| Non-white race/ethnicity | 455 (18.9) | 510 (12.1) |
| Eligible for low-income subsidy | 1,048 (43.5) | 1,803 (42.8) |
| Urban residence | 1,587 (66.8) | 2,821 (68.2) |
| Area-level income, $ | ||
| <30,000 | 648 (27.3) | 1,011 (24.5) |
| 30,000-<75,000 | 1,581 (66.6) | 2,812 (68.2) |
| 75,000+ | 145 (6.1) | 303 (7.3) |
| Comorbidity | ||
| Coronary heart disease | 1,545 (64.2) | 2,739 (65.1) |
| Diabetes mellitus | 1,147 (47.6) | 2,031 (48.2) |
| Chronic kidney disease | 572 (23.8) | 954 (22.7) |
| Depression | 318 (13.2) | 504 (12.0) |
| Dementia | 253 (10.5) | 415 (9.9) |
| Receive home health services | 514 (21.3) | 805 (19.1) |
| Number of medication classes | ||
| <5 | 139 (5.8) | 205 (4.9) |
| 5 – 9 | 658 (27.3) | 1,134 (26.9) |
| ≥10 | 1,611 (66.9) | 2,871 (68.2) |
AMI – Acute myocardial infarction, PDC – proportion of days covered.
Numbers in table are sample size (column percentage)
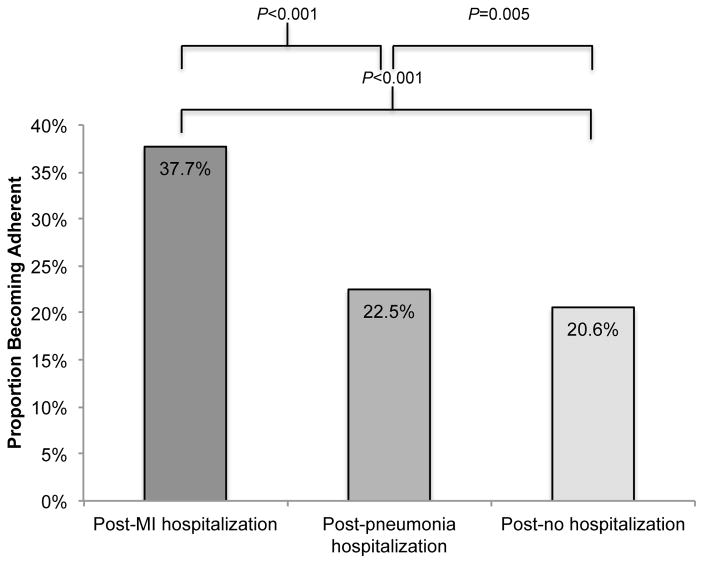
Change from Nonadherent to Adherent
Among 2,408 patients who were nonadherent to statins before AMI hospitalization, 37.7% were adherent in the subsequent year. In comparison, 22.5% of those hospitalized for pneumonia and 20.6% of those not hospitalized became adherent (Figure 1). After multivariable adjustment, patients hospitalized for AMI were more likely to become adherent compared with patients hospitalized for pneumonia [adjusted relative risk (aRR) 1.70, 95%CI, 1.57–1.84)] and those not hospitalized (aRR 1.79, 95% CI, 1.68–1.90). Patients hospitalized for pneumonia were not more likely to become adherent to statins than patients who were not hospitalized (aRR 1.00, 95%CI, 0.94–1.07). Results were similar in sensitivity analyses defining becoming adherent as a change in PDC from <80% to ≥80% with a 10% or larger increase in PDC (Supplemental Table 2).
Figure 1.
Proportion of Nonadherent Patients That Become Adherent to Statins after Acute Myocardial Infarction Hospitalization, Pneumonia Hospitalization, or in 2011 versus 2010 for those without a Hospitalization. Patients were considered adherent if proportion of days covered (PDC) with statins was ≥80% and nonadherent if PDC<80%.
Among patients who were nonadherent before their AMI hospitalization, eligibility for low-income subsidy and living in higher-income areas were associated with greater likelihood of becoming adherent to statins after discharge (Table 2). The presence of pre-existent coronary heart disease, diabetes, and PDC<50% were associated with lower likelihood of becoming adherent after discharge.
Table 2.
Sociodemographic and Clinical Characteristics Associated with Changing from Nonadherent to Statins before Hospitalization for Acute Myocardial Infarction to Adherent to Statins After Hospital Discharge (N=2,408).*
| Characteristic | Unadjusted RR (95% CI) |
Adjusted†
RR (95% CI) |
|---|---|---|
| Age, in years | ||
| 65–74 | 1 (ref) | 1 (ref) |
| 75–84 | 1.07 (0.96 , 1.20 ) | 1.07 (0.96 , 1.20 ) |
| 85+ | 0.97 (0.83 , 1.13 ) | 0.96 (0.82 , 1.13 ) |
| Female gender | 1.00 (0.90 , 1.11 ) | 1.01 (0.90 , 1.12 ) |
| Non-white race/ethnicity | 0.85 (0.74 , 0.98 ) | 0.86 (0.73 , 1.01 ) |
| Eligible for low-income subsidy | 0.99 (0.89 , 1.10 ) | 1.13 (1.01 , 1.27 ) |
| Urban residence | 1.00 (0.90 , 1.12 ) | 1.01 (0.90 , 1.13 ) |
| Area-level income, $ | ||
| <30,000 | 1 (ref) | 1 (ref) |
| 30,000-<75,000 | 1.13 (1.00 , 1.28 ) | 1.09 (0.96 , 1.24 ) |
| 75,000+ | 1.25 (1.00 , 1.55 ) | 1.26 (1.00 , 1.59 ) |
| Comorbidity | ||
| Coronary heart disease | 0.79 (0.72 , 0.88 ) | 0.81 (0.73 , 0.91 ) |
| Diabetes mellitus | 0.82 (0.74 , 0.91 ) | 0.87 (0.78 , 0.97 ) |
| Chronic kidney disease | 0.86 (0.76 , 0.98 ) | 0.91 (0.79 , 1.05 ) |
| Depression | 0.88 (0.75 , 1.04 ) | 0.89 (0.75 , 1.06 ) |
| Dementia | 0.86 (0.71 , 1.03 ) | 0.85 (0.70 , 1.03 ) |
| Number of medication classes before MI | ||
| <5 | 1 (ref) | 1 (ref) |
| 5 – 9 | 0.83 (0.68 , 1.01 ) | 0.88 (0.72 , 1.08 ) |
| ≥10 | 0.75 (0.62 , 0.90 ) | 0.85 (0.69 , 1.04 ) |
| Before hospitalization PDC<50% | 0.72 (0.64 , 0.80 ) | 0.71 (0.63 , 0.79 ) |
| CABG during hospitalization | 1.14 (0.96 , 1.35 ) | 1.02 (0.86 , 1.21 ) |
| Receive home health services | 0.99 (0.87 , 1.12 ) | 1.14 (0.99 , 1.30 ) |
Abbreviations: RR, relative risk; AMI, acute myocardial infarction; PDC, proportion of days covered; CABG, coronary artery bypass graft surgery
Analyses were conducted using the primary definition of adherence in which patients were categorized as adherent if PDC ≥80%.
Adjusted analyses include all the variables listed in the table.
In secondary analyses, among patients who were nonadherent before AMI hospitalization, mean PDC increased from 51% to 61% (Table 3). After multivariable adjustment, patients with an AMI hospitalization had 15.4% and 15.0% larger increases in mean PDC than their counterparts hospitalized for pneumonia and without a hospitalization, respectively (both p<0.001; Supplemental Table 3).
Table 3.
Change in Mean Adherence to Statins from Before to After Acute Myocardial Infarction Hospitalization, Pneumonia Hospitalization, and No Hospitalization in Patients Who Were Nonadherent in the First Time Period, and in Patients Who Were Adherent in the First Time Period*
| Nonadherent to Statins (PDC <80%) in First Time Period | |||
|---|---|---|---|
| AMI hospitalization (N=2,408) | Pneumonia hospitalization (N=3,624) | No hospitalization in 2010 - 2011 (N=44,815) | |
| Pre-hospitalization adherence, mean PDC (SD) | 51.1% (21.0%) | 52% (21%) | 53.3% (20.0%) |
| Post-hospitalization adherence, mean PDC (SD) | 61.1% (32.1%) | 45.6% (34.7%) | 48.0% (31.9%) |
| Change in adherence, [post minus pre- hospitalization PDC (95%CI)]† | 10.0% (8.8%, 11.1%) | −6.0% (−6.9%, −5%) | −5.3% (−5.5%, −5.1%) |
| Adherent to Statins (PDC ≥80%) in First Time Period | |||
|---|---|---|---|
| AMI hospitalization (N=4,210) | Pneumonia hospitalization (N=7,847) | No hospitalization in 2010 - 2011 (N=113,284) | |
| Pre-hospitalization adherence, mean PDC (SD) | 94.4% (5.5%) | 94.6% (5.5%) | 95.0% (5.3% ) |
| Post-hospitalization adherence, mean PDC (SD) | 80.6% (22.2%) | 77.7% (24.7%) | 84.1% (17.4%) |
| Change in adherence [post minus pre- hospitalization PDC (95%CI)]‡ | −13.8% (−14.3%, − 13.2%) | −16.9% (−17.4%, − 16.5%) | −11.0% (−11.1%, − 10.9%) |
Abbreviations: AMI, acute myocardial infarction; PDC, proportion of days covered
Proportion of days covered with statins is presented as a continuous measure in this table. The first time period refers to the one year period before the first hospitalization for AMI or pneumonia among patients with this type of hospitalization between 2007 and 2011 or to the one year period spanning 2010 for patients with no hospitalizations in 2010 and 2011.
P-interaction <0.001 comparing all three groups. P-interaction <0.001 for the pairwise comparison of pneumonia hospitalization with AMI hospitalization, and no hospitalization with AMI hospitalization. P-interaction=0.11 for the pairwise comparison of no hospitalization with pneumonia hospitalization.
P-interaction <0.001 comparing all three groups. P-interaction <0.001 for the pairwise comparison of pneumonia hospitalization with AMI hospitalization, no hospitalization with AMI hospitalization and no hospitalization with pneumonia hospitalization.
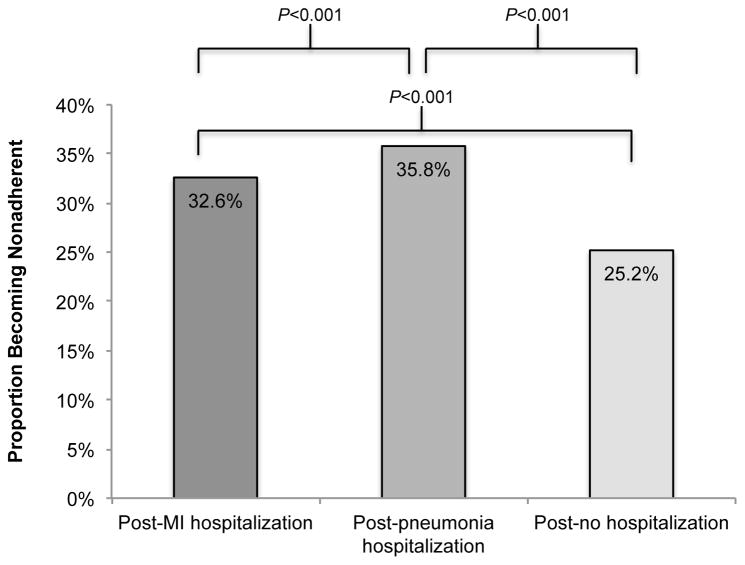
Change from Adherent to Nonadherent
Among 4,210 patients who were adherent to statins before an AMI hospitalization, 32.6% became nonadherent after discharge. In comparison, 35.8% of patients hospitalized for pneumonia and 25.2% of those not hospitalized became nonadherent (Figure 2). After multivariable adjustment, those with an AMI hospitalization were less likely to become nonadherent than those with a pneumonia hospitalization (aRR 0.93, 95% CI, 0.88–0.98). Those with an AMI hospitalization (aRR 1.41, 95% CI, 1.35–1.48) and, separately, those with a pneumonia hospitalization (aRR 1.57, 95%CI, 1.52–1.63) were more likely than those not hospitalized to become nonadherent. Results were similar in sensitivity analyses defining becoming nonadherent as a change in PDC from ≥80% to <80% with a 10% or larger decrease in PDC (Supplemental Table 4).
Figure 2.
Proportion of Adherent Patients That Become Nonadherent After Acute Myocardial Infarction Hospitalization, Pneumonia Hospitalization, or in 2011 versus 2010 for those without a Hospitalization. Patients were considered adherent if proportion of days covered (PDC) with statins was ≥80% and nonadherent if PDC<80%.
Among those who were adherent before their AMI hospitalization, older age, diabetes, depression, and dementia were associated with increased risk of becoming nonadherent after hospital discharge whereas eligibility for low-income subsidy was associated with decreased risk of becoming nonadherent (Table 4).
Table 4.
Sociodemographic and Clinical Characteristics Associated with Changing from Adherent before Hospitalization for Acute Myocardial Infarction to Nonadherent After Hospital Discharge* (N=4,210)
| Characteristic | Unadjusted RR (95% CI) |
Adjusted†
RR (95% CI) |
|---|---|---|
| Age, in years | ||
| 65–74 | 1 (ref) | 1 (ref) |
| 75–84 | 1.17 (1.05 , 1.29 ) | 1.13 (1.02 , 1.25 ) |
| 85+ | 1.31 (1.17 , 1.47 ) | 1.26 (1.11 , 1.43 ) |
| Female gender | 1.07 (0.98 , 1.17 ) | 1.01 (0.92 , 1.11 ) |
| Non-white race/ethnicity | 1.06 (0.93 , 1.21 ) | 1.05 (0.91 , 1.21 ) |
| Eligible for low-income subsidy | 0.96 (0.88 , 1.05 ) | 0.88 (0.80 , 0.98 ) |
| Urban residence | 0.94 (0.85 , 1.03 ) | 0.98 (0.88 , 1.08 ) |
| Area-level income, $ | ||
| <30,000 | 1 (ref) | 1 (ref) |
| 30,000–<75,000 | 1.09 (0.98 , 1.21 ) | 1.07 (0.96 , 1.20 ) |
| 75,000+ | 1.1 (0.91 , 1.32 ) | 1.07 (0.88 , 1.29 ) |
| Comorbidity | ||
| Coronary heart disease | 1.03 (0.94 , 1.13 ) | 1.01 (0.91 , 1.11 ) |
| Diabetes mellitus | 1.12 (1.02 , 1.22 ) | 1.10 (1.00 , 1.21 ) |
| Chronic kidney disease | 1.18 (1.07 , 1.30 ) | 1.09 (0.98 , 1.21 ) |
| Depression | 1.25 (1.11 , 1.41 ) | 1.15 (1.01 , 1.31 ) |
| Dementia | 1.37 (1.22 , 1.55 ) | 1.23 (1.08 , 1.40 ) |
| Number of medication classes before AMI | ||
| <5 | 1 (ref) | 1 (ref) |
| 5 – 9 | 1.01 (0.80 , 1.28 ) | 0.96 (0.75 , 1.21 ) |
| ≥10 | 1.22 (0.97 , 1.52 ) | 1.06 (0.84 , 1.35 ) |
| CABG during hospitalization | 0.93 (0.79 , 1.09 ) | 1.03 (0.87 , 1.22 ) |
| Receive home health services | 1.22 (1.11 , 1.35 ) | 1.10 (0.99 , 1.23 ) |
Abbreviations: RR, relative risk; CI, confidence interval; AMI, acute myocardial infarction; CABG, coronary artery bypass graft surgery
Analyses were conducted using the primary definition of adherence in which patients were categorized as adherent if PDC ≥ 80%.
Adjusted analyses include all the variables listed in the table.
In secondary analyses that examined the change in mean adherence among patients with a PDC ≥80% before AMI hospitalization, mean PDC adherence declined from 94% to 81% (Table 3). After multivariable adjustment, patients with an AMI hospitalization had a 2.7% smaller decline in mean PDC adherence compared with patients with a pneumonia hospitalization (p<0.001; Supplemental Table 3). Compared to patients without hospitalizations, patients with an AMI hospitalization and a pneumonia hospitalization had 3.4% and 6.6% larger declines in mean PDC, respectively, after multivariable adjustment (both p<0.001).
Conclusions
In the current study of statin adherence before and after hospitalization for AMI, more than 40% of Medicare beneficiaries were nonadherent to statins after AMI, and the overall proportion of beneficiaries that was nonadherent increased from before to after the AMI hospitalization. Despite this overall worsening in adherence after AMI hospitalization, patients who were nonadherent to statins before hospitalization for AMI were nearly two times more likely to become adherent after discharge as compared to patients hospitalized for pneumonia or those not hospitalized. This finding supports the hypothesis that a hospitalization for AMI can act as teachable moment that promotes adherence to treatments prescribed to prevent recurrent events. In contrast, patients who were adherent to statins before hospitalization for AMI or pneumonia were more likely to become nonadherent after discharge compared to patients with no hospitalizations. This suggests that a hospitalization, irrespective of the reason, can also have an adverse impact on medication adherence.
The conceptual model underlying teachable moments is that health events transiently increase perceived vulnerability to the disease underlying the health event and trigger a reassessment of the expected risks and benefits of relevant health behaviors.(31,32) These processes, in turn, may promote a tipping point toward positive health behavior change. While several studies have shown that health events, such as cancer diagnosis, pregnancy, or AMI, can increase smoking cessation,(2,33) there are few data showing that health events can positively influence medication adherence.(19) Several small studies show that clinicians can enhance the effect of the teachable moment by drawing clear connections between the health event and preventive health behaviors when counseling patients.(34,35) Thus, our study implies that clinicians can promote statin adherence after AMI by explicitly linking the prevention of recurrent cardiac events to medication adherence.
Hospitalization for either AMI or pneumonia was associated with a modest worsening in adherence to statins in patients who were adherent before hospitalization. The inclusion of a control group of patients with no hospitalizations enabled us to ensure that this worsening in adherence was not simply due to regression to the mean. Patients who were older and those with comorbid depression or dementia represented vulnerable subgroups who were at significantly higher risk of a decline in adherence after hospital discharge. These findings are consistent with evidence showing that disjointed transitions in care from hospital to home can produce medication reconciliation errors that put patients, especially those from vulnerable groups, at risk for medication nonadherence.(36,37) These findings also support the post-hospital syndrome hypothesis that the hospitalization, in itself, impairs patients’ ability to adhere to medications after discharge. To prevent a decline in adherence after hospitalization, there is a need for increased attention to interventions that take place immediately after discharge to help optimize adherence after hospitalization as opposed to solely focusing on the in-hospital discharge process.(38) Furthermore, interventions that reduce the stress of hospitalization by optimizing sleep and keeping patients mentally and physically active during their stay may have a beneficial effect on medication adherence after discharge.(39)
There are a number of strengths to the current study. Medicare claims include data for a large national sample that is highly generalizable to older US adults. Medicare claims also capture continuity of care for patients, thus allowing us to examine adherence before and after hospitalization. Additionally, using Medicare claims facilitates the evaluation of a number of factors that may influence adherence, including demographics, comorbidities, and polypharmacy. Despite these strengths, the current study should be interpreted in the context of certain limitations. Although we required patients to have continuous Medicare Part D coverage, some may have paid for their statins without a Part D claim being submitted.(40) Additionally, patients hospitalized for AMI may have disproportionately received free samples of statins after discharge. Further, some patients may have been advised by their physician to discontinue their statin during the study period, and Medicare claims do not capture this information. These unmeasured factors may have led to the misclassification of adherent patients as nonadherent, and may have led to an overestimate of the adverse impact of hospitalization on nonadherence. Also, the analysis was limited to fee-for-service Medicare beneficiaries, and it is unknown whether the findings extend to younger patients or patients enrolled in a Medicare Advantage program. Finally, the analysis was limited to patients who survived until at least six months after the initial hospitalization, which may have biased the sample toward being more adherent.
In conclusion, a substantial proportion of patients will have an improvement in adherence to statins after AMI hospitalization. Even with this improvement, approximately 40% of patients are likely to be nonadherent after AMI. Efforts to improve adherence to statins after AMI have met with disappointing results in prior studies.(41,42) The results of the current study suggest that an AMI may present a potent opportunity for motivating patients to become adherent to cardiovascular medications, and counseling interventions that emphasize the connection between statin adherence and recurrent AMI prevention may be particularly effective. Also, a hospitalization, regardless of the cause, appears to represent a vulnerable period that is associated with a worsening in adherence in a substantial proportion of patients. Quality improvement initiatives that incorporate adherence monitoring after discharge are needed to prevent a decline in adherence after AMI hospitalization.
Supplementary Material
What is Known
Nonadherence to statins is common after hospitalization for acute myocardial infarction (AMI).
Patients who are nonadherent to statins after AMI are at increased risk for recurrent cardiovascular events and have higher healthcare costs.
What the Study Adds
Medicare beneficiaries who are hospitalized for an AMI are nearly twice as likely to become adherent to statins as compared to beneficiaries hospitalized for a non-cardiac reason.
A hospitalization for an AMI may represent a teachable moment that can be leveraged to motivate patients to improve their adherence to statins.
A hospitalization for an AMI also represents a vulnerable period that can lead to a worsening in statin adherence in about 1 in 3 Medicare beneficiaries.
Acknowledgments
Sources of Funding: Dr. Kronish is supported by the National Institutes of Health (K23 HL-098359, R01 HL123368, and UL1 TR000040). Dr. Ross is supported by the National Institute on Aging (K08 AG032886) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; nor decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: Dr. Ross receives research support through Yale University from Medtronic, Inc. and Johnson & Johnson to develop methods of clinical trial data sharing, from the Centers of Medicare and Medicaid Services (CMS) to develop and maintain performance measures that are used for public reporting, and from the Food and Drug Administration (FDA) to develop methods for post-market surveillance of medical devices. Dr. Muntner receives research support from Amgen Inc. None of the authors has financial relationships with industry.
References
- 1.Lawson PJ, Flocke SA. Teachable moments for health behavior change: a concept analysis. Patient Educ Counsel. 2009;76:25–30. doi: 10.1016/j.pec.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glasgow RE, Stevens VJ, Vogt TM, Mullooly JP, Lichtenstein E. Changes in smoking associated with hospitalization: quit rates, predictive variables, and intervention implications. Am J Public Health. 1991;6:24–29. doi: 10.4278/0890-1171-6.1.24. [DOI] [PubMed] [Google Scholar]
- 3.Fonarow GC. In-hospital initiation of statins: taking advantage of the 'teachable moment'. Cleve Clin J Med. 2003;70:502, 504–6. doi: 10.3949/ccjm.70.6.502. [DOI] [PubMed] [Google Scholar]
- 4.Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS One. 2012;7:e38915. doi: 10.1371/journal.pone.0038915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lane D, Carroll D, Ring C, Beevers DG, Lip GY. The prevalence and persistence of depression and anxiety following myocardial infarction. Br J Health Psychol. 2002;7:11–21. doi: 10.1348/135910702169321. [DOI] [PubMed] [Google Scholar]
- 6.Kronish IM, Edmondson D, Goldfinger JZ, Fei K, Horowitz CR. Posttraumatic stress disorder and adherence to medications in survivors of strokes and transient ischemic attacks. Stroke. 2012;43:2192–7. doi: 10.1161/STROKEAHA.112.655209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rieckmann N, Kronish IM, Haas D, Gerin W, Chaplin WF, Burg MM, Vorchheimer D, Davidson KW. Persistent depressive symptoms lower aspirin adherence after acute coronary syndromes. Am Heart J. 2006;152:922–927. doi: 10.1016/j.ahj.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 8.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 9.Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368:100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia-Caballos M, Ramos-Diaz F, Jimenez-Moleon JJ, Bueno-Cavanillas A. Drug-related problems in older people after hospital discharge and interventions to reduce them. Age Ageing. 2010;39:430–438. doi: 10.1093/ageing/afq045. [DOI] [PubMed] [Google Scholar]
- 11.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028–3035. doi: 10.1161/CIRCULATIONAHA.108.768986. [DOI] [PubMed] [Google Scholar]
- 12.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 13.Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff. 2011;30:91–99. doi: 10.1377/hlthaff.2009.1087. [DOI] [PubMed] [Google Scholar]
- 14.Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA. 2007;297:177–186. doi: 10.1001/jama.297.2.177. [DOI] [PubMed] [Google Scholar]
- 15.Chowdhury R, Khan H, Heydon E, Shroufi A, Fahimi S, Moore C, Stricker B, Mendis S, Hofman A, Mant J, Franco OH. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013;34:2940–2948. doi: 10.1093/eurheartj/eht295. [DOI] [PubMed] [Google Scholar]
- 16.Choudhry NK, Setoguchi S, Levin R, Winkelmayer WC, Shrank WH. Trends in adherence to secondary prevention medications in elderly post-myocardial infarction patients. Pharmacoepidemiol Drug Saf. 2008;17:1189–1196. doi: 10.1002/pds.1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA. 2002;288:462–467. doi: 10.1001/jama.288.4.462. [DOI] [PubMed] [Google Scholar]
- 18.Hirsh BJ, Smilowitz NR, Rosenson RS, Fuster V, Sperling LS. Utilization of and adherence to guideline-recommended lipid-lowering therapy after acute coronary syndrome: Opportunities for improvement. J Am Coll Cardiol. 2015;66:184–192. doi: 10.1016/j.jacc.2015.05.030. [DOI] [PubMed] [Google Scholar]
- 19.de Vries FM, Denig P, Vegter S, Bos HJ, Postma MJ, Hak E. Does a cardiovascular event change adherence to statin treatment in patients with type 2 diabetes? A matched cohort design. Curr Med Res Opin. 2015;31:595–602. doi: 10.1185/03007995.2015.1011780. [DOI] [PubMed] [Google Scholar]
- 20.Nau DP. Proportion of days covered (PDC) as a preferred method of measuring medication adherence. Springfield, VA: Pharmacy Quality Alliance; [Date accessed: April 7, 2016]. http://pqaalliance.org/resources/adherence.asp. [Google Scholar]
- 21.Choudhry NK, Shrank WH, Levin RL, Lee JL, Jan SA, Brookhart MA, Solomon DH. Measuring concurrent adherence to multiple related medications. Am J Manag Care. 2009;15:457–464. [PMC free article] [PubMed] [Google Scholar]
- 22.Fang G, Robinson JG, Lauffenburger J, Roth MT, Brookhart MA. Prevalent but moderate variation across small geographic regions in patient nonadherence to evidence-based preventive therapies in older adults after acute myocardial infarction. Med Care. 2014;52:185–193. doi: 10.1097/MLR.0000000000000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noyes K, Liu H, Lyness JM, Friedman B. Medicare beneficiaries with depression: comparing diagnoses in claims data with the results of screening. Psychiatr Serv. 2011;62:1159–1166. doi: 10.1176/ps.62.10.pss6210_1159. [DOI] [PubMed] [Google Scholar]
- 24.Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(Suppl 2):B10–21. doi: 10.2337/diacare.27.suppl_2.b10. [DOI] [PubMed] [Google Scholar]
- 25.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46:1075–1079. doi: 10.1016/0895-4356(93)90103-8. [DOI] [PubMed] [Google Scholar]
- 26.United States Renal Data System. USRDS 2009 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. Bethesda, MD: 2010. [Google Scholar]
- 27.Behrens T, Taeger D, Wellmann J, Keil U. Different methods to calculate effect estimates in cross-sectional studies. A comparison between prevalence odds ratio and prevalence ratio. Methods Inf Med. 2004;43:505–509. [PubMed] [Google Scholar]
- 28.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 29.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 30.Choudhry NK, Avorn J, Glynn RJ, Antman EM, Schneeweiss S, Toscano M, Reisman L, Fernandes J, Spettell C, Lee JL, Levin R, Brennan T, Shrank WH. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365:2088–2097. doi: 10.1056/NEJMsa1107913. [DOI] [PubMed] [Google Scholar]
- 31.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18:156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 32.Boudreaux ED, Bock B, O'Hea E. When an event sparks behavior change: an introduction to the sentinel event method of dynamic model building and its application to emergency medicine. Acad Emerg Med. 2012;19:329–335. doi: 10.1111/j.1553-2712.2012.01291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rigotti NA, Munafo MR, Stead LF. Smoking cessation interventions for hospitalized smokers: a systematic review. Arch Intern Med. 2008;168:1950–1960. doi: 10.1001/archinte.168.18.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen DJ, Clark EC, Lawson PJ, Casucci BA, Flocke SA. Identifying teachable moments for health behavior counseling in primary care. Patient Educ Couns. 2010;85:e8–15. doi: 10.1016/j.pec.2010.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flocke SA, Step MM, Antognoli E, Lawson PJ, Smith S, Jackson B, Krejci S, Parran T, Marsh S. A randomized trial to evaluate primary care clinician training to use the Teachable Moment Communication Process for smoking cessation counseling. Prev Med. 2014;69:267–273. doi: 10.1016/j.ypmed.2014.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kripalani S, Roumie CL, Dalal AK, Cawthon C, Businger A, Eden SK, Shintani A, Sponsler KC, Harris LJ, Theobald C, Huang RL, Scheurer D, Hunt S, Jacobson TA, Rask KJ, Vaccarino V, Gandhi TK, Bates DW, Williams MV, Schnipper JL. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge: a randomized trial. Ann Intern Med. 2012;157:1–10. doi: 10.7326/0003-4819-157-1-201207030-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kripalani S, Henderson LE, Jacobson TA, Vaccarino V. Medication use among inner-city patients after hospital discharge: patient-reported barriers and solutions. Mayo Clin Proc. 2008;83:529–535. doi: 10.4065/83.5.529. [DOI] [PubMed] [Google Scholar]
- 38.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314–323. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 39.Bartick MC, Thai X, Schmidt T, Altaye A, Solet JM. Decrease in as-needed sedative use by limiting nighttime sleep disruptions from hospital staff. J Hosp Med. 2010;5:E20–24. doi: 10.1002/jhm.549. [DOI] [PubMed] [Google Scholar]
- 40.Musich S, Cheng Y, Wang SS, Hommer CE, Hawkins K, Yeh CS. Pharmaceutical cost-saving strategies and their association with medication adherence in a Medicare supplement population. J Gen Intern Med. 2015;30:1208–1214. doi: 10.1007/s11606-015-3196-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, Agoritsas T, Mistry N, Iorio A, Jack S, Sivaramalingam B, Iserman E, Mustafa RA, Jedraszewski D, Cotoi C, Haynes RB. Interventions for enhancing medication adherence. Cochrane Database Sys Rev. 2014;11:CD000011. doi: 10.1002/14651858.CD000011.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schedlbauer A, Davies P, Fahey T. Interventions to improve adherence to lipid lowering medication. Cochrane Database Sys Rev. 2010;3:CD004371. doi: 10.1002/14651858.CD004371.pub3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.