Abstract
Objectives
Patient transfers between hospitals are becoming more common in the United States. Disease-specific studies have reported varying outcomes associated with transfer status. However, even as national quality improvement efforts and regulations are being actively adopted, forcing hospitals to become financially accountable for the quality of care provided, surprisingly little is known about transfer patients or their outcomes at a population level. This population-wide study provides timely analyses of the characteristics of this particularly vulnerable and sizable inpatient population. We identified and compared characteristics and outcomes of transfer and nontransfer patients.
Methods
With the use of the 2009 Nationwide Inpatient Sample, a nationally representative sample of U.S. hospitalizations, we examined patient characteristics, in-hospital adverse events, and discharge disposition for transfer versus nontransfer patients in this observational study.
Results
We identified 1,397,712 transfer patients and 31,692,211 nontransfer patients. Age, sex, race, and payer were significantly associated with odds of transfer (P < 0.05). Transfer patients had higher risk-adjusted inpatient mortality (4.6 versus 2.1, P < 0.01), longer length of stay (13.3 versus 4.5, P < 0.01), and fewer routine disposition discharges (53.6 versus 68.7, P < 0.01). In-hospital adverse events were significantly higher in transfer patients compared with nontransfer patients (P < 0.05).
Conclusions
Our results suggest that transfer patients have inferior outcomes compared with nontransfer patients. Although they are clinically complex patients and assessing accountability as between the transferring and receiving hospitals is methodologically difficult, transfer patients must nonetheless be included in quality benchmark data to assess the potential impact this population has on hospital outcome profiles. With hospital accountability and value-based payments constituting an integral part of health care reform, documenting the quality of care delivered to transfer patients is essential before accurate quality assessment improvement efforts can begin in this patient population.
Keywords: patient safety, interfacility transfers, patient safety indicators
Transfer admissions account for an increasing percentage of overall hospital admissions and health care costs in the United States. Each year, patients transferred between acute care hospitals constitute approximately 3.5% of all hospital inpatient admissions (1.5 million admissions).1,2 Interhospital transfer of patients occurs for diverse reasons including need for specialty care, physician consultation/second opinion, as well as patient preference and convenience. Transfer patients as a group are more complex, require high levels of health care (e.g., specialty services), and have high resource use (e.g., longer hospital stays), which are costly.3–6
The Patient Protection and Affordable Care Act ties financial incentives to the quality of hospital performance, which is intended to improve patient outcomes.7 Currently, these incentives focus on adherence to process measures and patient outcomes. The Center for Medicare and Medicaid Services (CMS) has identified benchmarks of performance, which include a range of general and disease-specific administrative claims-based quality indicators.8 Most of these indicators focus on elective admissions in relatively stable populations. Currently, specifications for CMS mortality and readmissions indicators handle transfers differently, with mortality assigned to the first hospital, whereas readmissions are attributed to the hospital that discharges the patient to a nonacute setting (e.g., home, skilled nursing facility). Patients entering the health care system for unplanned emergency care, as well as interhospital transfers, were excluded in earlier versions of these indicators and are not included uniformly in all national measures. The variation in assigning transfer patients to or excluding them from national benchmarks limits the comparative accuracy of case-mix adjustment and severity of illness across hospitals. Some groups claim that inclusion of transfers leaves tertiary referral centers at a disadvantage for CMS's value-based payment modifiers and does not provide a complete picture of the quality of care delivered across hospitals.9 Measurement choices tend to be based on assumptions about care for transfer patients instead of direct exam of data for this population.
To provide a nationwide profile of the understudied population of transfer patients, we compared patient demographics and outcomes between interhospital transfer patients and nontransfer patients for nonroutine hospital admissions in this observational study. Our goal was to describe patient and hospital characteristics associated with transfer status and to compare outcomes of transfer versus nontransfer patients at a population level using hierarchical modeling. Our analyses fill an important gap in the evidence regarding the quality of care these patients receive.
METHODS
Data Sources
We used 2 national data sources for the analyses. First, the Nationwide Inpatient Sample (NIS) by the Agency for Healthcare Research and Quality's Healthcare Cost and Utilization Project (HCUP) was used to identify adult patients with a transfer status. The NIS is the largest, publicly available, all-payer, inpatient database in the United States.10 The NIS consists of a nationally representative sample of administrative billing records of acute care, nonfederal hospitals. The NIS collects information on 5 to 8 million inpatient stays annually, from approximately 1050 hospitals, or 20% of all community hospitals in the United States. The NIS data set contains deidentified hospitalization information on primary and secondary diagnoses and procedures, patient demographics, hospital characteristics, length of stay (LOS), payer, total charges, admission source, discharge status, as well as inpatient mortality. Second, we used the Web tool HCUPnet to obtain data on national longitudinal trends in hospital transfer rates from 1993 to 2011.2 Our query on HCUPnet included trends on all-payer hospital inpatient admissions using the NIS data source, which includes pediatric and routine admissions, by admission status over time.
Study Population
Our cohort included adult patient discharges (age ≥ 18 y) admitted in 2009. Patients were defined as transfers if their source of admission was from a different acute care hospital from their discharging hospital. We excluded routine admissions from our analyses because we assumed routine admissions to be planned admissions to a hospital that is capable of treating the patient's existing medical condition. We also excluded patients admitted from a non–acute care facility, including long-term care facilities or skilled nursing homes; admissions involving routine births; and patients missing admission source.
Comorbidity and Injury Severity
Patient comorbidity was calculated using the Elixhauser Comorbidity Index.11 The Elixhauser Comorbidity Index can be used with any administrative data set that includes 30 coexisting medical conditions that could influence patient outcomes.
Definition of Patient Outcomes
Our primary outcomes included transfer status, risk-adjusted inpatient mortality, and quality of care received as defined by the development of an adverse event while in a hospital. In-hospital adverse events were identified by Agency for Healthcare Research and Quality's Patient Safety Indicators (PSIs), Version 4.4.12,13 Patient Safety Indicators are based on Medicare Severity Diagnosis Related Groups and International Classification of Diseases, Ninth Revision, Clinical Modification codes. Patient Safety Indicator risk adjustment includes age, sex, age-sex interactions, diagnosis-related group, and comorbidities assessed using the Elixhauser Comorbidity Index.11 Each adverse event has a unique set of inclusion and exclusion criteria and risk adjustors.14 The software program's ascertainment of events excludes those flagged or designated as present on admission by the PSI software algorithm. For this study, we included 5 PSIs: hospital-acquired pressure ulcer (PSI03), death among surgical inpatients with serious treatable complications (failure to rescue [PSI04]), postoperative (PO) respiratory failure (PSI11), PO deep vein thrombosis or pulmonary embolism (PSI12), and PO sepsis (PSI13). For PSI03, we removed the PSI's coded exclusion for transfer patients. Transfer patients are typically excluded from analyses of hospital-acquired pressure ulcers (PSI03) because of the lack of consistent present-on-admission designation in administrative data sets.
Secondary outcomes included LOS, total charges, and patient disposition at discharge, as defined by the NIS. Nonroutine disposition at discharge included patients discharged to an acute care hospital, home health care, a skilled nursing facility or intermediate care facility, against medical advice, and unknown destinations.
Sensitivity Analysis
To identify a well-defined population with severe disease in need of timely intervention, we conducted sensitivity analyses, limiting our data set to patients receiving a major operating room procedure during their hospital admission, as defined by the NIS. For transfer patients, this was defined as a major operating room procedure at the receiving hospital.
Statistical Analyses
With the use of our first data source, the 2009 NIS database, basic patient demographics, outcomes, and hospital characteristics were evaluated using Roa-Scott χ2 for categorical variables, Student t test for normally distributed continuous variables, and Kruskal Wallis test of Wilcoxon rank sums for other continuous variables. Regression models were built to determine factors associated with transfer status and mortality. The NIS data were weighted to account for the survey-design nature of the data collection.
The trend analysis for the HCUPnet data was assessed between 1993 and 2011 using a full-forward joinpoint regression.15 This method describes changing trends over time segments and estimates the amount of change over different segments, thus identifying significant changes in trends over time. Pairwise comparisons can be made to identify differences in parallelism between 2 rates.
Statistical analysis was performed using SAS software (SAS Institute Inc, Cary, NC) and the Joinpoint Regression software program.16
RESULTS
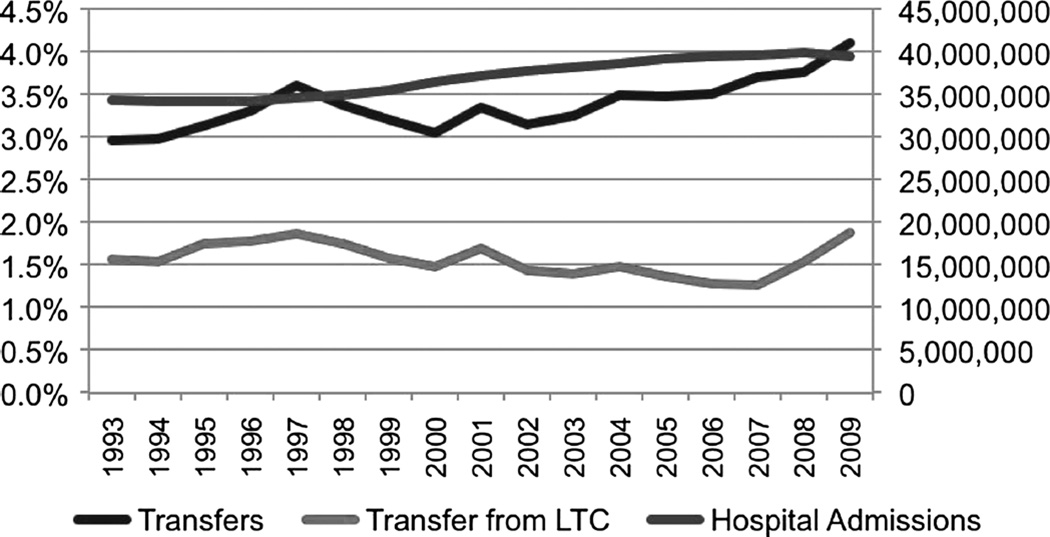
In 2009, a total of 1,397,712 patients with emergent conditions were transferred between acute care hospitals, representing 4% of our study population (Fig. 1). From 1993 to 2009, hospital admissions due to transfers increased annually by 1.56% compared with nontransfer patient admissions (1.10%) (P = 0.0413). Significant differences in age distribution existed between transfer and nontransfer patients (P < 0.0001), with a greater proportion of older patients in the transfer group. Males were more likely to be transferred compared with females (50.6% versus 49.6%; P < 0.0001). A larger proportion of unreported race category was seen in transfer patients, which resulted in smaller proportions of white, black, and Hispanic racial categories for transfer patients compared with nontransfer patients (P < 0.0001). Patients with private and Medicaid primary payers were less likely to be transferred compared with patients with Medicare as a primary payer (P < 0.0001). Transfer patients were less likely to receive an operating room procedure (P = 0.0009) but had a higher number of coded comorbidities, 3.0 versus 2.5 (P < 0.0001). Weekend admission did not differ between transfer and nontransfer patients (Table 1).
FIGURE 1.
Trends in hospital admissions and percentage of transfer admissions in U.S. hospitals, 1993 to 2009. The total number of hospital admissions is shown on the right axis and depicted by the black line. The percentage of admissions transferred from another hospital is shown on the left axis and depicted in red, and the percentage of transfers from long-term care facilities (LTC) is in blue.
TABLE 1.
Distribution of Patient and Admission Characteristics Stratified by Patient Admission Source, Nontransfer Versus Transfer
| Characteristic | Nontransfers | Transfers | P |
|---|---|---|---|
| n (%) | 31,692,211 (96) | 1,397,712 (4) | |
| Age category, % | <0.0001 | ||
| 18–39 | 25.4 | 14.4 | |
| 40–64 | 34.0 | 37.6 | |
| 65–74 | 15.7 | 19.8 | |
| ≥75 | 24.9 | 28.2 | |
| Male, % | 39.6 | 50.6 | <0.0001 |
| Race, % | <0.0001 | ||
| White | 58.5 | 56.7 | |
| Black | 11.8 | 8.4 | |
| Hispanic | 9.3 | 5.5 | |
| Other/missing | 20.4 | 29.4 | |
| Insurance, % | <0.0001 | ||
| Private | 30.8 | 25.9 | |
| Medicaid | 15.4 | 11.5 | |
| Medicare | 44.0 | 53.0 | |
| Self-pay | 4.7 | 2.7 | |
| Elixhauser Comorbidity Index, mean (median) |
2.5 (2.0) | 3.0 (3.0) | <0.0001 |
| OR procedure | 30.4 | 27.2 | 0.0009 |
| Weekend admission | 19.3 | 20.1 | 0.1164 |
Transfer patients were more likely to be routed to teaching hospitals (P < 0.0001), urban hospitals (P = 0.0018), and hospitals classified as large bed size as defined by the NIS (P = 0.0119). Patients were transferred to hospitals with a lower percentage of registered nurses (RNs) among all nurses (92.0 versus 92.8, P < 0.0001) as well as a higher mean of RN full-time equivalents (FTEs) to 1000 patient-adjusted days (4.37 versus 4.07, P < 0.0001) and licensed practical nurse FTEs to 1000 patient-adjusted days (0.34 versus 0.29, P < 0.0001) (Table 2).
TABLE 2.
Distribution of Hospital Characteristics Stratified by Patient Admission Source, Nontransfer Versus Transfer
| Characteristic | Nontransfers | Transfers | P |
|---|---|---|---|
| n (%) | 31,692,211 (96) | 1,397,712 (4) | |
| Teaching hospital, % | 44.5 | 59.4 | <0.0001 |
| Urban location, % | 87.4 | 92.6 | 0.0018 |
| Hospital location, % | <0.0001 | ||
| Northeast | 58.5 | 56.7 | |
| Midwest | 11.8 | 8.4 | |
| South | 9.3 | 5.5 | |
| West | 20.4 | 29.4 | |
| Hospital bed size, % | 0.0119 | ||
| Small | 12.1 | 12.3 | |
| Medium | 24.4 | 17.9 | |
| Large | 63.5 | 69.8 | |
| RNs among all nurses, mean (median) |
92.8 (95.0) | 92.0 (96.0) | <0.0001 |
| RN FTEs to 1000 patient-adjusted days mean (median) |
4.07 (4.0) | 4.37 (4.40) | <0.0001 |
| LN FTEs to 1000 patient-adjusted days mean (median) |
0.29 (0.2) | 0.34 (0.2) | <0.0001 |
LN, licensed practical nurse.
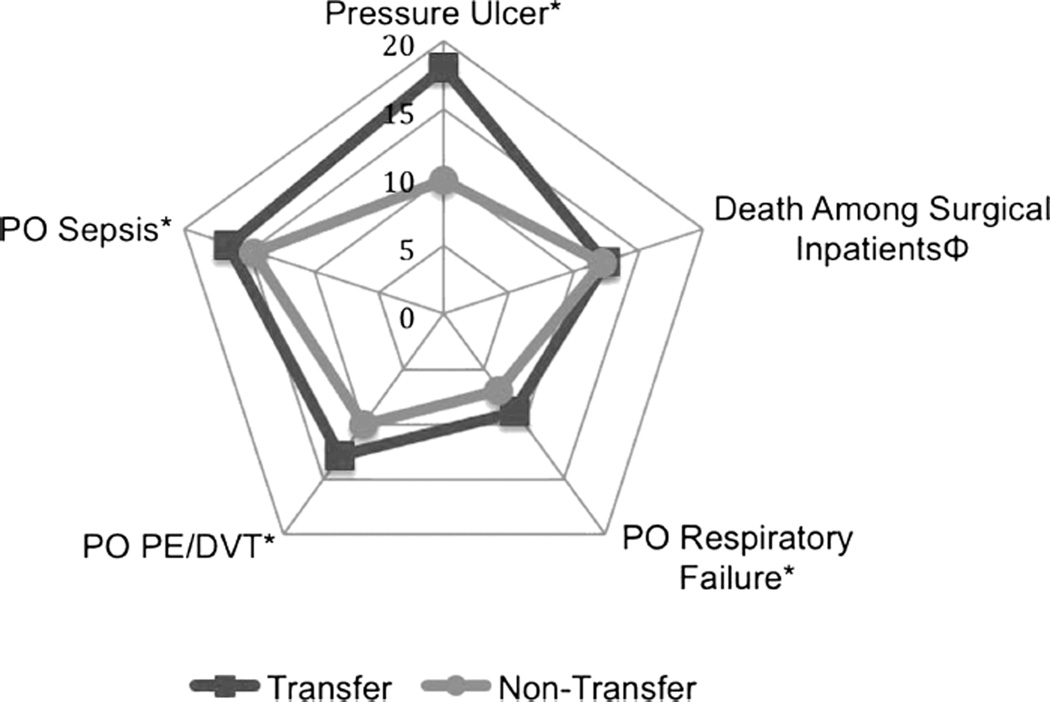
Transfer patients had significantly higher risk-adjusted PSI rates for 4 of the 5 indicators analyzed: PSI03 pressure ulcer (risk-adjusted rates [RARs]: 18.14 versus RAR: 9.82, P < 0.0001), PSI11 PO respiratory failure (RAR: 8.81 versus RAR: 6.87, P = 0.0012), PSI12 PO pulmonary embolism and/or deep vein thrombosis (RAR: 12.82 versus RAR: 10.75, P = 0.0035), and PSI13 PO sepsis (RAR: 16.5 versus RAR: 14.6, P = 0.0432). PSI04, death among surgical inpatients with serious treatable conditions, did not differ significantly between transfer and nontransfer patients (RAR: 125.2 versus RAR: 121.7, respectively, P = 0.0597) (Fig. 2). Because the 95% confidence intervals (CIs) do not overlap, these rates are significantly different at P < 0.05.
FIGURE 2.
Distribution of nationwide risk-adjusted PSI rates per 1000 patients at risk, 2009. ФRates displayed are per 100 patients at risk for visual purposes. *P < 0.05.
Transfer patients had a higher risk-adjusted inpatient mortality compared with nontransfer patients (4.6% versus 2.1% [P < 0.0001]). They also had greater resource use compared with nontransfer patients. Transfer patients had a longer LOS (13.3 versus 4.5 days [P < 0.0001]); a smaller proportion of patients were discharged with routine disposition (53.6% versus 68.7%); and higher proportions of transfer patients were discharged to skilled nursing facilities, intermediate care facilities, and home health care (P < 0.0001) (Table 3).
TABLE 3.
Distribution of Patient Outcomes Stratified by Patient Admission Source, Nontransfer Versus Transfer
| Characteristic | Nontransfers | Transfers | P |
|---|---|---|---|
| Risk-adjusted inpatient mortality |
2.1 | 4.6 | <0.0001 |
| LOS, mean (median)* | 4.5 (3.0) | 13.3 (6.0) | <0.0001 |
| Charges, mean (median)* | $32,501 ($18,499) |
$57,283 ($29,144) |
<0.0001 |
| Discharge disposition | <0.0001 | ||
| Routine | 68.7 | 53.6 | |
| Acute care hospital | 2.17 | 4.49 | |
| Other hospital | 14.74 | 19.52 | |
| Home health care | 11.05 | 15.56 | |
| Other | 3.34 | 6.83 |
Kruskal-Wallis test.
Compared with patients aged 18 to 39 years, patients aged 65 to 74 years had the highest odds of being transferred (odds ratio [OR], 1.626; 95% CI, 1.45–1.82) followed by patients aged 40 to 64 years (OR, 1.541; CI, 1.41–1.68) and patients 75 years or older (OR, 1.414; CI, 1.24–1.62) (P < 0.0001). Males had greater odds of being transferred (OR, 1.392; CI, 1.36–1.43), and whites had higher odds of being transferred than blacks (OR, 0.732; CI, 0.62–0.86) and Hispanics (OR, 0.728; CI, 0.59–0.90) (P < 0.0001). Primary payer was also associated with transfer status. Medicare patients had 17% increased odds associated with transfer status compared with those with private insurance (OR, 1.165; CI, 1.08–1.25). Odds ratios of transfer for Medicaid and self-pay patients were not significantly different from private insurance payers (Table 4). Transfer status was significantly associated with increased mortality compared with nontransfer patients, both in univariate (13.22% versus 3.67%, P < 0.0001) and multivariate models (OR, 2.045; CI, 1.907–2.193) (data not shown).
TABLE 4.
Multivariate Logistic Regression Model for Transfer Status Admission
| Risk Factor | OR | 95% CI | P |
|---|---|---|---|
| Age category | <0.0001 | ||
| 18–39 | Reference | ||
| 40–64 | 1.541 | 1.41–1.68 | |
| 65–74 | 1.626 | 1.45–1.82 | |
| ≥75 | 1.414 | 1.24–1.62 | |
| Male versus female | 1.392 | 1.36–1.43 | <0.0001 |
| Race | <0.0001 | ||
| White | Reference | ||
| Black | 0.732 | 0.62–0.86 | |
| Hispanic | 0.728 | 0.59–0.90 | |
| Other/missing | 1.607 | 1.22–2.11 | |
| Primary payer | 0.0456 | ||
| Private | Reference | ||
| Medicaid | 1.035 | 0.93–1.15 | |
| Medicare | 1.165 | 1.08–1.25 | |
| Self-pay | 1.069 | 0.93–1.23 | |
| Weekend versus weekday | 1.039 | 0.98–1.11 | 0.2378 |
As a sensitivity analysis attempting to look at a group of seriously injured patients requiring a high-technology intervention, we restricted our analyses to a group of patients requiring timely emergency surgery. Limiting the analyses to patients receiving a major surgical procedure produced similar results to our complete analysis (Table 5), with differences in transfer status based on primary payer, race, and weekend admission.
TABLE 5.
Sensitivity Analysis: Multivariate Logistic Regression Model for Transfer Status Admission in Patients Receiving a Major Operating Room Procedure
| Risk Factor | OR | 95% CI | P |
|---|---|---|---|
| Age category | <0.0001 | ||
| 18–39 | Reference | ||
| 40–64 | 1.940 | 1.67–2.25 | |
| 65–74 | 1.697 | 1.50–1.92 | |
| ≥75 | 1.555 | 1.35–1.78 | |
| Male versus female | 1.717 | 1.65–1.78 | <0.0001 |
| Race | <0.0001 | ||
| White | Reference | ||
| Black | 0.758 | 0.62–0.93 | |
| Hispanic | 0.655 | 0.53–0.81 | |
| Other/missing | 1.625 | 1.21–2.18 | |
| Primary payer | 0.0074 | ||
| Private | Reference | ||
| Medicaid | 1.326 | 1.20–1.47 | |
| Medicare | 1.244 | 1.16–1.34 | |
| Self-pay | 1.233 | 1.04–1.46 | |
| Weekend versus weekday | 2.068 | 1.91–2.24 | <0.0001 |
Adjusted for disease severity using Elixhauser comorbidities.
DISCUSSION
This is the first report to characterize transfer patients and their health outcomes at a population level. Our data expand on previous disease- and site-specific studies and provide national evidence that transfer patients have higher rates of mortality, more in-hospital adverse events, and use substantially more resources (e.g., longer LOS and more discharges to other types of facilities). As quality health care delivery, including patient safety, becomes a fundamental part of the Affordable Care Act's value-based payment reform and hospitals become accountable for patient outcomes, it is essential that patients transferred for care, some of the most complicated admissions, be included in standard quality measures.
Our multivariate analyses found that, in addition to patient comorbidity, nonclinical factors such as race, payer, and sex were all significantly associated with transfer status. Previous studies have shown that women are less likely to be transferred compared with men for specific conditions, such as myocardial infarction17 and trauma.18 Our study amplifies this knowledge, providing evidence that sex disparities exist at a national level, regardless of condition or site. Furthermore, we show that both blacks and Hispanics were less likely to be transferred compared with white patients, even after adjusting for payer and patient severity. These results are consistent with other studies for acute myocardial infarction.17,19 Primary payer was also significantly associated with transfer status. Prior studies have reported that patients with private health insurance are less likely to be transferred compared with patients on Medicare,18,20 although more recent studies suggest that this apparent disparity may be weakening.21 Nonetheless, our findings suggest that patients with private insurance are less likely to be transferred than those insured by public payers or who are “self-pay.” The potential financial benefits derived by the index admission hospital from privately insured patients could, in part, explain this finding. Our data set did not allow us to account for other possible causes of transfer such as patient preference or transfer to a facility closer to home after specialty intervention, any of which could explain some of these differences.
At a population level, without examining disease-specific conditions, our data indicate that transfer status was associated with worse outcomes. Transfer patients had almost double the risk-adjusted mortality rates compared with nontransfer patients. For patients who survived their hospital stay, 15% fewer transfer patients had a routine discharge disposition compared with nontransfer patients, with more patients discharged to acute care hospitals or home health care. Furthermore, our data suggest that certain in-hospital adverse events were significantly greater among transfer patients compared with nontransfer patients, with risk-adjusted complications doubled for transfer patients. Failure to improve and patient deterioration could be reasons for transfer and substantially influence our reported higher rates of inpatient adverse events after transfer. Patient deterioration might be poorly captured in the risk adjustment because we cannot account for care provided during a transfer patient's index hospital admission. Differences noted could also be due to timing of transfer during the illness spectrum (transfer for specialty care versus transfer to lower level of care) and existence of effective specialty intervention.
Many disease-specific studies have shown that timely transfers of patients with medical conditions in need of specialty services produce better patient outcomes and lower mortality rates.22–25 Transferring this subset of patients for proven, higher level of care is a positive aspect of our medical system; however, the factors associated with transfer in our study seem to reflect other potential rationales for transfer (or not), suggesting that it is important to further evaluate disparities in access to specialty care (clinical and nonclinical characteristics associated with transfer), outcomes, and quality of care for the population of transfer patients. Because we are creating a methodology to assess quality of care for transfer patients, these data are essential to include.
We performed sensitivity analyses, limiting our data to patients with a major surgical procedure, to account for disease-specific differences and needs for transfer. This limitation had little effect on our findings and highlighted specific disparities among transfer patients. Our sensitivity analysis still estimates that race and payer are important factors associated with transfer and that transfer status was significantly associated with increased inpatient mortality, even after correcting for important comorbidities.
We recognize several limitations of the study. First, with the use of administrative data, we are not able to clinically characterize patients as fully as is possible with exam of medical records. In particular, we are not able to assess clinical details about reasons for transfer or nontransfer. Although we have attempted to risk-adjust the outcomes reported, risk-adjustment is based on secondary diagnoses, and these codes are not always adequately reported.11 We have included race in our regression models. Because several states participating in the NIS do not provide information on patient race, there are a large number of patients with missing data. In an attempt to correct for this limitation, we include missing race as a separate race category. Despite these limitations, these data provide a previously unpublished view of the characteristics of transfer patients and hospitals as well as outcomes of and quality of care of transfer patients in the United States.
CONCLUSIONS
The number of patients being transferred between acute care facilities continues to grow in the United States, and these patients have high medical needs and demand more resources. These are complex patients, and accountability is difficult because of shared responsibility across multiple hospitals. However, we provide evidence that these patients have worse outcomes than their nontransfer counterparts, supporting the need to develop and refine measures of quality of care for these patients. As new regulations force hospitals to become financially accountable for patient outcomes, carefully constructed national quality measures for transfer care should be designed and validated.
Acknowledgments
Supported by the Agency for Healthcare Research and Quality.
Footnotes
The authors disclose no conflict of interest.
REFERENCES
- 1.Steiner C, Elixhauser A, Schnaier J. The Healthcare Cost and Utilization Project: an overview. Eff Clin Pract. 2002;5:143–151. [PubMed] [Google Scholar]
- 2.Rockville, MD: Agency for Healthcare Research and Quality; [Accessed February 22, 2013]. HCUPnet. Healthcare Cost and Utilization Project (HCUP). 1993–2011. http://hcupnet.ahrq.gov/ [PubMed] [Google Scholar]
- 3.Munoz E, Soldano R, Gross H, et al. Diagnosis related groups and the transfer of general surgical patients between hospitals. Arch Surg. 1988;123:68–71. doi: 10.1001/archsurg.1988.01400250078014. [DOI] [PubMed] [Google Scholar]
- 4.Borlase BC, Baxter JT, Benotti PN, et al. Surgical intensive care unit resource use in a specialty referral hospital: I. Predictors of early death and cost implications. Surgery. 1991;109:687–693. [PubMed] [Google Scholar]
- 5.Human and Health Services, editor. Healthcare Cost and Utilization Project. Facts and Figures 2009. Rockville, MD: Agency for Healthcare Research & Quality; 2011. [Google Scholar]
- 6.Nathens AB, Maier RV, Brundage SI, et al. The effect of interfacility transfer on outcome in an urban trauma system. J Trauma. 2003;55:444–449. doi: 10.1097/01.TA.0000047809.64699.59. [DOI] [PubMed] [Google Scholar]
- 7.U.S. Department of Health & Human Services. The Patient Protection and Affordable Care Act. Washington, DC: U.S. Government; 2010. [Google Scholar]
- 8.Centers for Medicare and Medicaid Services. Value-Based Payment Modifier. Baltimore, MD: CMS; 2013. [Google Scholar]
- 9.Stelfox HT, Straus SE. Measuring quality of care: considering measurement frameworks and needs assessment to guide quality indicator development. J Clin Epidemiol. 2013;66:1320–1327. doi: 10.1016/j.jclinepi.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 10.HCUP Nationwide Inpatient Sample (NIS) Rockville, MD: Agency for Healthcare Research and Quality; [Accessed February 22, 2013]. Healthcare Cost and Utilization Project (HCUP). 2011. www.hcup-us.ahrq.gov/nisoverview.jsp. [Google Scholar]
- 11.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 12.McDonald KM, Romano PS, Geppert J, et al. Measures of Patient Safety Based on Hospital Administrative Data - The Patient. Rockville (MD): Agency for Healthcare Research and Quality; 2002. [PubMed] [Google Scholar]
- 13.Agency for Healthcare Research and Quality. Quality Indicators. Rockville, MD: U.S. Department of Health & Human Services; 2012. [Accessed October 2014]. Available at http://www.qualityindicators.ahrq.gov/software/SAS.aspx. [Google Scholar]
- 14.Human and Health Services, editor. Agency for Healthcare Research and Quality. AHRQ Quality Indicator: Risk Adjustment Coefficients for the PSI. Rockville, MD: Agency for Healthcare Research & Quality; 2011. [Google Scholar]
- 15.Downey JR, Hernandez-Boussard T, Banka G, et al. Is patient safety improving? National trends in patient safety indicators: 1998–2007. Health Serv Res. 2012;47:414–430. doi: 10.1111/j.1475-6773.2011.01361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 17.Gurwitz JH, Goldberg RJ, Malmgren JA, et al. Hospital transfer of patients with acute myocardial infarction: the effects of age, race, and insurance type. Am J Med. 2002;112:528–534. doi: 10.1016/s0002-9343(02)01072-0. [DOI] [PubMed] [Google Scholar]
- 18.Selassie AW, McCarthy ML, Pickelsimer EE. The influence of insurance, race, and gender on emergency department disposition. Acad Emerg Med. 2003;10:1260–1270. doi: 10.1111/j.1553-2712.2003.tb00611.x. [DOI] [PubMed] [Google Scholar]
- 19.Cooke CR, Nallamothu B, Kahn JM, et al. Race and timeliness of transfer for revascularization in patients with acute myocardial infarction. Med Care. 2011;49:662–667. doi: 10.1097/MLR.0b013e31821d98b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nathens AB, Maier RV, Copass MK, et al. Payer status: the unspoken triage criterion. J Trauma. 2001;50:776–783. doi: 10.1097/00005373-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Green A, Showstack J, Rennie D, et al. The relationship of insurance status, hospital ownership, and teaching status with interhospital transfers in California in 2000. Acad Med. 2005;80:774–779. doi: 10.1097/00001888-200508000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Glickman SW, Greiner MA, Lin L, et al. Assessment of temporal trends in mortality with implementation of a statewide ST-segment elevation myocardial infarction (STEMI) regionalization program. Ann Emerg Med. 2012;59:243–252. e241. doi: 10.1016/j.annemergmed.2011.07.030. [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez-Stawinski GV, Chang AS, Navia JL, et al. Regional referral system for patients with acute mechanical support: experience at the Cleveland Clinic Foundation. ASAIO J. 2006;52:445–449. doi: 10.1097/01.mat.0000225265.11371.ed. [DOI] [PubMed] [Google Scholar]
- 24.Lyden P. Thrombolytic therapy for acute stroke—not a moment to lose. N Engl J Med. 2008;359:1393–1395. doi: 10.1056/NEJMe0806335. [DOI] [PubMed] [Google Scholar]
- 25.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]