Abstract
Heparin-induced thrombocytopenia syndrome is an acquired potentially life-threatening prothrombotic disorder caused by antibodies that recognize complexes of platelet factor 4 bound to heparin or heparin-like molecules. It typically occurs after exposure to unfractionated heparin, to a lesser extent after exposure to low-molecular-weight heparins, and rarely after exposure to fondaparinux. Herein, we report the case of a 48-year-old woman who developed severe thrombocytopenia, bilateral pulmonary embolism, and bilateral adrenal hemorrhages after total knee arthroplasty without evidence of heparin exposure. Antibodies to the heparin-platelet factor 4 complex and serotonin-release assay were positive. Spontaneous heparin-induced thrombocytopenia syndrome should be considered in patients with unexplained thrombocytopenia after knee replacement surgery even without heparin exposure, and a high index of suspicion for adrenal hemorrhage is needed in patients with fever, abdominal pain, and shock.
Keywords: Adrenal hemorrhage, Deep venous thrombosis, Heparin-induced thrombocytopenia, Pulmonary embolism, Total knee arthroplasty
Introduction
Heparin-induced thrombocytopenia (HIT) is an acquired, potentially life-threatening, prothrombotic disorder caused by antibodies that recognize complexes of platelet factor 4 (PF4) bound to heparin or heparin-like molecules [1]. It typically occurs after exposure to unfractionated heparin, to a lesser extent after exposure to low-molecular-weight heparin (LMWH), and rarely after exposure to fondaparinux [2], [3]. Although HIT is invariably related to heparin exposure, few reports described patients who developed HIT without any history of heparin exposure [4], [5], [6], [7]. Herein, we report the case of a 48-year-old woman who developed severe thrombocytopenia, bilateral pulmonary embolism (PE), and bilateral adrenal hemorrhages (BAHs) after total knee arthroplasty (TKA) without evidence of heparin exposure.
Case history
A 48-year-old female patient with left knee osteoarthritis underwent primary left TKA (Nex Gen High Flex, Zimmer Inc., Warsaw, IN, USA) uneventfully. She received aspirin postoperatively for deep venous thrombosis (DVT) prophylaxis. The patient started continuous passive motion exercise the day after the surgery, and the drain was removed after putting out an insignificant amount. She continued to do well in regards to pain and knee function and was discharged home on postoperative day (POD) 3. On POD 8, she was readmitted to the hospital for low-grade fever and abdominal pain. Her platelet count on admission was 362,000/μL which then dropped to 187,000/μL on the following day (before any heparin exposure). She then received LMWH for DVT prophylaxis on the second day of readmission, and her platelet count dropped further to 57,000/μL (POD 10).
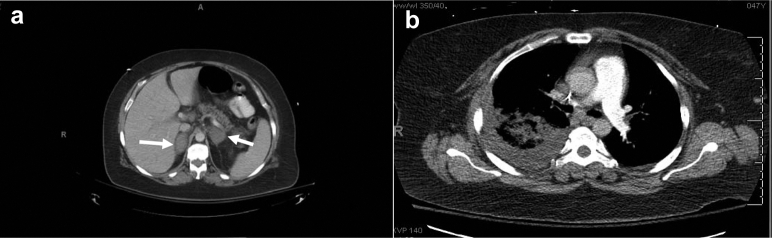
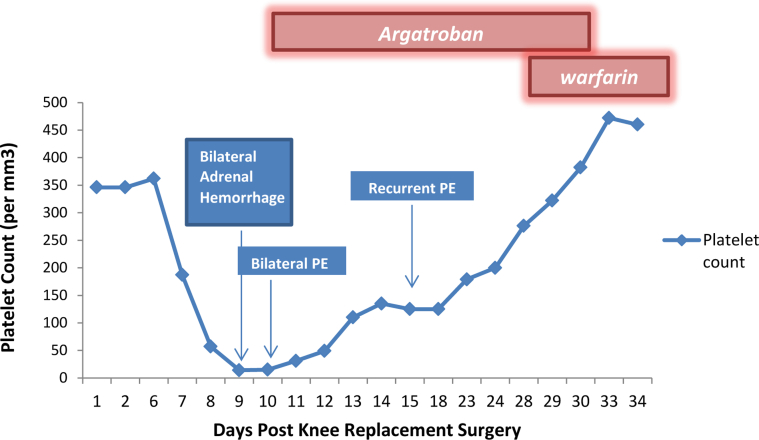
Peripheral blood smear analysis confirmed her thrombocytopenia and did not show any evidence of microangiopathic hemolysis. Anticardiolipin antibodies and lupus anticoagulants were not present. In light of her progressive thrombocytopenia, there was a concern for HIT. Immunoglobulin G–specific PF4-heparin enzyme immunoassay and the platelet serotonin–release assay were strongly positive (100% serotonin release at 0.1 U/mL of heparin and 0% serotonin release at 100 U/mL of heparin). The patient then developed severe abdominal pain with profound hypotension and was immediately transferred to the intensive care unit. Computed tomography (CT) of the abdomen and pelvis showed BAHs (Fig. 1a). The patient was empirically started on pulse steroids for possible adrenal insufficiency with marked improvement in her vital status. However, platelet count dropped further to 15,000/μL, and she developed pleuritic chest pain and became more tachypneic, which raised the suspicion for possible PE. CT pulmonary angiography showed bilateral PE (Fig. 1b), and therapeutic anticoagulation was initiated with argatroban, a direct thrombin inhibitor, with a target-activated partial thromboplastin time (PTT) of 1.5 to 2 times baseline level. Her platelet count began to increase gradually, but the anticoagulation was frequently interrupted because of supratherapeutic PTT values. The patient then developed recurrent pleuritic chest pain and tachycardia which raised the concern for recurrent PE. Repeat CT pulmonary angiography confirmed the presence of new bilateral PE (Fig. 2) for which an inferior vena cava filter was placed. She continued anticoagulation with argatroban and was bridged to warfarin after her platelet count had risen to over 150,000/μL.
Figure 1.
Axial CT images demonstrating (a) bilateral adrenal gland enlargements and diffuse hemorrhage (arrows) and (b) bilateral pulmonary emboli.
Figure 2.
Clinical course of a patient with spontaneous HIT presenting as bilateral adrenal hemorrhage and bilateral pulmonary emboli.
Throughout her hospital readmission, the patient continued to work with physical therapy. Gradual improvement in the muscle strength and range of motion (ROM) of the knee was noted. On discharge, the patient was able to ambulate without significant knee pain. Her ROM was 0° to 100°, and the knee incision was healing without any wound complications. The patient continued to follow-up and her platelet count remained normal. She also continued on steroids replacement therapy for adrenal insufficiency after she failed multiple weaning trials. At 1-year postoperative, the knee wound was completely healed. The patient was ambulating without any assisted devices, and she had 0 to 120° of active ROM without any pain. Follow-up radiographs showed maintained alignment of the prosthesis without any signs of loosening or instability.
Discussion
We described a rare case of life-threatening spontaneous HIT after TKA, presenting as BAHs (indicating bilateral adrenal vein thrombosis) and bilateral PE, triggered by administration of LMWH without any previous heparin exposure. Our patient received 325-mg aspirin twice daily for DVT prophylaxis after TKA. An extensive review of the patient's preoperative and postoperative medication history did not show any evidence of heparin exposure (no heparinized devices or heparin flushes). The only exposure to heparin was during her second hospitalization where she received 1 time prophylactic LMWH. Of note, her platelet count already represented a 50% drop from the admission platelet count even before she received the LMWH.
Although HIT is invariably triggered by preceding heparin exposure, there are few case reports describing patients with clinical and serologic features of HIT despite the absence of previous heparin exposure [7], [8]. Our patient had knee arthroplasty 8 days before the onset of thrombocytopenia. Heparin-like molecules, such as glycosaminoglycans can be released during knee replacement surgery triggering the generation of anti-PF4/heparin complexes [9], [10]. Thus, it is possible that our patient had preexisting anti-PF4/Heparin antibodies before any heparin exposure, resulting from the knee surgery, and on LMWH exposure, there was a rapid drop in her platelet count.
Our patient also developed recurrent PE because of frequent interruption of the argatroban dosing in the setting of supratherapeutic PTT. PTT is used to monitor argatroban dosing but can be confounded by the severe HIT itself or by the associated comorbidities [11]. Supratherapeutic PTT, however, does not necessarily indicate a supratherapeutic drug level, which is considered a drawback of using direct thrombin inhibitor therapy in treating HIT.
Future surgeries can be a challenge in patients with history of HIT because they are at a theoretical increased risk of rapid-onset HIT. Current American College of Chest Physicians guidelines recommend against heparin reexposure in patients with a history of HIT [12]. Nevertheless, heparin can still be used, for short term only, in patients who require cardiac surgery provided that repeat PF4/heparin antibodies are negative. DVT prophylaxis can be achieved with fondaparinux [3], [13] in patients with creatinine clearance >30 mL/min or with argatroban in patients with creatinine clearance <30 mL/min [14].
Summary
In summary, we report a rare case of spontaneous HIT presenting as severe thrombocytopenia, recurrent PE, and BAH after TKA. Spontaneous HIT should be considered in patients with unexplained thrombocytopenia after knee replacement surgery even without heparin exposure, and a high index of suspicion for adrenal hemorrhage is needed in patients with fever, abdominal pain, and shock.
Acknowledgments
The authors would like to thank Kelly A. Keating, PhD for her editing of the article.
Footnotes
No author associated with this paper has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2015.07.003.
Appendix. Supplementary data
References
- 1.Kelton J.G., Arnold D.M., Bates S.M. Non heparin anticoagulants for heparin-induced thrombocytopenia. N Engl J Med. 2013;368(8):737. doi: 10.1056/NEJMct1206642. [DOI] [PubMed] [Google Scholar]
- 2.Bhatt V.R., Aryal M.R., Shrestha R., Armitage J.O. Fondaparinux-associated heparin-induced thrombocytopenia. Eur J Haematol. 2013;91(5):437. doi: 10.1111/ejh.12179. [DOI] [PubMed] [Google Scholar]
- 3.Warkentin T.E., Cook R.J., Marder V.J. Anti-platelet factor 4/heparin antibodies in orthopedic surgery patients receiving antithrombotic prophylaxis with fondaparinux or enoxaparin. Blood. 2005;106(12):3791. doi: 10.1182/blood-2005-05-1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Warkentin T.E., Safyan E.L., Linkins L.A. Heparin-induced thrombocytopenia presenting as bilateral adrenal hemorrhages. N Engl J Med. 2015;372(5):492. doi: 10.1056/NEJMc1414161. [DOI] [PubMed] [Google Scholar]
- 5.Perrin J., Barraud D., Toussaint-Hacquard M., Bollaert P.E., Lecompte T. Rapid onset heparin-induced thrombocytopenia (HIT) without history of heparin exposure: a new case of so-called ‘spontaneous’ HIT. Thromb Haemost. 2012;107(4):795. doi: 10.1160/TH11-12-0825. [DOI] [PubMed] [Google Scholar]
- 6.Warkentin T.E., Basciano P.A., Knopman J., Bernstein R.A. Spontaneous heparin-induced thrombocytopenia syndrome: 2 new cases and a proposal for defining this disorder. Blood. 2014;123(23):3651. doi: 10.1182/blood-2014-01-549741. [DOI] [PubMed] [Google Scholar]
- 7.Mallik A., Carlson K.B., DeSancho M.T. A patient with ‘spontaneous’ heparin-induced thrombocytopenia and thrombosis after undergoing knee replacement. Blood Coagul Fibrinolysis. 2011;22(1):73. doi: 10.1097/MBC.0b013e328340ff11. [DOI] [PubMed] [Google Scholar]
- 8.Warkentin T.E., Makris M., Jay R.M., Kelton J.G. A spontaneous prothrombotic disorder resembling heparin-induced thrombocytopenia. Am J Med. 2008;121(7):632. doi: 10.1016/j.amjmed.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Ahmad S., Haas S., Hoppensteadt D.A., Lietz H., Reid U., Bender N. Differential effects of clivarin and heparin in patients undergoing hip and knee surgery for the generation of antiheparin-platelet factor 4 antibodies. Thromb Res. 2002;108:49. doi: 10.1016/s0049-3848(02)00397-3. [DOI] [PubMed] [Google Scholar]
- 10.Warkentin T.E., Cook R.J., Marder V.J., Greinacher A. Anti-PF4/heparin antibody formation postorthopedic surgery thromboprophylaxis: the role of nondrug risk factors and evidence for a stoichiometry-based model of immunization. J Thromb Haemost. 2010;8:504. doi: 10.1111/j.1538-7836.2009.03735.x. [DOI] [PubMed] [Google Scholar]
- 11.Cuker A., Cines D.B. How I treat heparin-induced thrombocytopenia. Blood. 2012;119(10):2209. doi: 10.1182/blood-2011-11-376293. [DOI] [PubMed] [Google Scholar]
- 12.Linkins L.A., Dans A.L., Moores L.K. American College of Chest Physicians. Treatment and prevention of heparin-induced thrombocytopenia: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e495S. doi: 10.1378/chest.11-2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harenberg J., Jorg I., Fenyvesi T. Treatment of heparin-induced thrombocytopenia with fondaparinux. Haematologica. 2004;89:1017. [PubMed] [Google Scholar]
- 14.Matthai W.H., Jr., Hursting M.J., Lewis B.E., Kelton J.G. Argatroban anticoagulation in patients with a history of heparin-induced thrombocytopenia. Thromb Res. 2005;116(2):121. doi: 10.1016/j.thromres.2004.11.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.