Supplemental Digital Content is available in the text.
KEY WORDS: antipsychotic medications, monotherapy, polypharmacy, state psychiatric hospitals, Hospital Based Inpatient Psychiatric Services (HBIPS) core performance measures 4 and 5
Abstract
Objectives:
The goal of this study was to explore antipsychotic medication prescribing practices in a sample of 86,034 patients discharged from state psychiatric inpatient hospitals and to find the prevalence of patients discharged with no antipsychotic medications, on antipsychotic monotherapy, and on antipsychotic polypharmacy. For patients discharged on antipsychotic polypharmacy, the study explored the adjusted rates of antipsychotic polypharmacy, the reasons patients were discharged on antipsychotic polypharmacy, the proportion of antipsychotic polypharmacy by mental health disorder, and the characteristics associated with being discharged on antipsychotic polypharmacy.
Methods:
This cross-sectional study analyzed all discharges for adult patients (18 to 64 y of age) from state psychiatric inpatient hospitals between January 1 and December 31, 2011. The relationship among variables was explored using χ2, t test, and analysis of variance. Logistic regression was used to determine predictors of antipsychotic polypharmacy.
Results:
The prevalence of antipsychotic polypharmacy was 12%. Of the discharged patients receiving at least 1 antipsychotic medication (adjusted rate), 18% were on antipsychotic polypharmacy. The strongest predictors of antipsychotic polypharmacy being prescribed were having a diagnosis of schizophrenia and a length of stay of 90 days or more. Patients were prescribed antipsychotic polypharmacy primarily to reduce their symptoms.
Conclusions:
Antipsychotic polypharmacy continues at a high enough rate to affect nearly 10,000 patients with a diagnosis of schizophrenia each year in state psychiatric inpatient hospitals. Further analysis of the clinical presentation of these patients may highlight particular aspects of the illness and its previous treatment that are contributing to practices outside the best-practice guideline. An increased understanding of trend data, patient characteristics, and national benchmarks provides an opportunity for decision-making that is sensitive to the patient’s needs and cognizant of the hospital’s accomplishments in adopting best practices.
Despite the lack of empirical evidence that antipsychotic polypharmacy produces superior outcomes to antipsychotic monotherapy, clinicians continue to prescribe multiple antipsychotic medications for patients with a diagnosis of schizophrenia.1–3 In fact, a number of treatment guidelines for schizophrenia recommend against the use of antipsychotic polypharmacy or only endorse it as a last resort after unsuccessful trials of monotherapy.4–8 There is clear evidence that antipsychotic polypharmacy presents complications for the patient, including risk of drug interactions, increased medication side effects, increased risk for metabolic disorders, and complex medication regimens, which may lead to medication nonadherence among patients.2,3,9
Clinical, societal, and patient factors can perpetuate the practice of antipsychotic polypharmacy.1,2,10–14 Clinical factors include side-effect management and insufficient trials of monotherapy.2,13 A measure of the effectiveness of schizophrenia treatment is reduction of positive symptoms, and antipsychotic medications are the most effective means for achieving this outcome.15 However, negative symptoms have a great impact on the everyday functioning of persons with schizophrenia and there is a lack of prescribing guidance to control these symptoms.15 Prescribing guidance also does not adequately address the complexity of monotherapy trials for persons with a long history of psychiatric illness, previous medication attempts, and complex medical comorbidity.
Societal factors include high patient-physician ratios, a fragmented health care system, and pressure to reduce hospital days. High patient-physician ratios reduce the amount of time a clinician can spend assessing a patient,16 limiting information on current and previous antipsychotic medication regimens. A fragmented health care system can result in a patient treated by >1 physician and, unless there is care coordination, management of medication regimens can become complex. In addition, clinicians are under pressure to shorten lengths of hospitalization, which may contribute to prescribing >1 antipsychotic medication to achieve symptom reduction more rapidly.1
Patient factors may also contribute to prescription patterns. Some patients may not be adhering to their medications as prescribed and, as a result, they may continue to experience significant schizophrenia symptoms. If the psychiatrist is unaware of the patient’s behavior, which is particularly likely in outpatient settings in which medication administration is solely the responsibility of the patient, then it is plausible that the outpatient psychiatrist may resort to antipsychotic polypharmacy.12 In the inpatient setting, patients who are admitted on a regimen of antipsychotic polypharmacy may be continued on this regimen for stabilization, while changing doses and combinations are evaluated.
Over the past 10 years, several new antipsychotic medications have come on the market. At the same time, there has been a growing recognition that antipsychotic polypharmacy needs to be brought to the attention of physicians.17 In 2011, The Joint Commission (TJC) began requiring psychiatric inpatient hospitals to monitor the number of patients discharged on multiple antipsychotic medications and the rationale given for antipsychotic polypharmacy through 2 performance measures from the Hospital Based Inpatient Psychiatric Services (HBIPS) core measures set. TJC used an expert panel that included physicians to develop these measures and defined scientifically validated appropriate justifications for polypharmacy as: (1) a history of 3 or more failed antipsychotic monotherapy trials, (2) cross-titrating antipsychotic medications to work toward monotherapy, or (3) the augmentation of clozapine.18 Previous research shows that when questionable prescribing practices are brought into focus, they are likely to change.11,19–22 Since the implementation of the HBIPS measures in 2011, there has been a nationwide trend toward reduction of antipsychotic polypharmacy in psychiatric inpatient hospitals.23
The existing literature on the characteristics of antipsychotic polypharmacy includes studies based on Medicaid claims data.24–28 The study described in this article adds to the knowledge base by examining data for adult patients discharged from state psychiatric inpatient hospitals, who would be excluded from Medicaid claims data due to the Institute for Mental Disease Exclusion rule. This rule states that any hospital having >16 beds, in which >50% of the beds are occupied by persons with a primary diagnosis of a mental disorder, is excluded from Medicaid reimbursement for care provided to patients who are 21 to 64 years of age.29
This study assessed the prescribing practices for antipsychotic medications in state psychiatric inpatient hospitals in 2011 to gain a national perspective on the prevalence and adjusted rates of prescription of antipsychotic polypharmacy, the reasons for which antipsychotic polypharmacy was prescribed, the most commonly prescribed combinations of antipsychotic medications, and the patient characteristics associated with being discharged on multiple antipsychotic medications. Unlike other studies, this study examined antipsychotic prescribing practices for all discharged adults, without preselecting by diagnosis. Trends for state psychiatric inpatient hospitals and comparison with other psychiatric inpatient hospitals are also explored. On the basis of this fuller understanding of the factors that contribute to antipsychotic polypharmacy, insights into quality initiatives that could help further reduce the use of antipsychotic polypharmacy are also provided.
METHOD
This study analyzed data extracted from the Behavioral Healthcare Performance Measurement System (BHPMS), a comprehensive proprietary national database of the National Association of State Mental Health Program Directors Research Institute Inc. (NRI), comprised of patient-level data submitted by state psychiatric inpatient hospitals in the United States and its territories. Hospitals extract patient-level data, including demographic data, diagnosis, medications, and follow-up information, from medical records and submit it to NRI’s BHPMS on a monthly basis to participate in common measures of quality of care such as the HBIPS performance measures. Hospitals submit patient-level data in specified formats (known as data files) as required by the BHPMS. The data files are processed using high-quality standards (no missing data for critical elements and <5% missing data for noncritical elements) before being accepted into the BHPMS Structured Query Language tables from which the data files are extracted for analysis. Data from 2 data files were used for the analysis described in this article. The episode data file provides a complete enumeration of unique episodes of care (eg, hospitalizations) that occurred between the first and the last days of a given month. The HBIPS data file represents patients discharged from psychiatric inpatient care during a given month, and hospitals may provide a random sample of discharges. The HBIPS data file consists of data that describe 5 content areas from the initial admission screening process, 4 content areas from the continuing care plan, and antipsychotic medications at discharge. To comply with the Health Insurance Portability and Accountability Act (HIPAA) and Federal privacy standards, all data extracted from NRI’s BHPMS system were deidentified and anonymous. All state psychiatric inpatient hospitals that participate in NRI’s BHPMS sign a data-sharing agreement that allows NRI’s researchers to use limited data sets to conduct secondary research and publicly disseminate the findings. This study was approved by the NRI Institutional Review Board.
All analyses were conducted using the SPSS statistical tool, version 22. All comparisons were based on α set at P<0.01 (2-sided).
Procedure
Patient-level data analyzed for this study were extracted from 2 linked data files within the BHPMS. Demographic data (gender, race, age, marital status, admission referral source, admission legal status, discharge type, living situation at discharge, discharge disposition, and Medicare coverage), admission date, discharge date, and mental health disorders were extracted from the episode data file. The variable “age groups” was created by regrouping age data. The “length of stay” variable was computed using admission and discharge dates. The number of antipsychotic medications, the reason for multiple antipsychotic medications, and the names of antipsychotic medications if provided were extracted from the HBIPS data file. The data from the 2 data files were linked using unique anonymous patient identifiers.
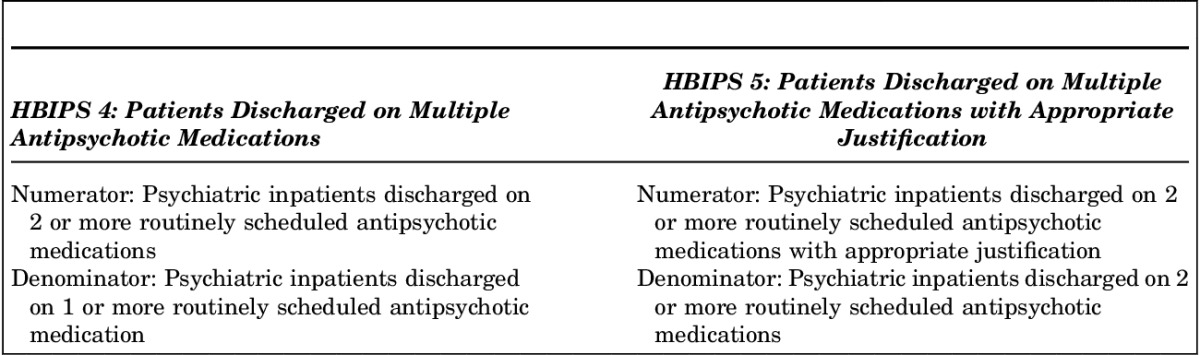
The HBIPS data were originally collected to calculate hospitals’ performance rates for HBIPS performance measures, 2 of which, HBIPS 4 and 5, are related to antipsychotic polypharmacy: the definitions for the measures as defined by TJC are presented in Table 1. Data on the number of antipsychotic medications prescribed at discharge were originally collected at a continuous level. The data were then recoded to create a 3-level variable used for study group comparisons among discharges: 0 antipsychotic medications; antipsychotic monotherapy; and antipsychotic polypharmacy. Antipsychotic monotherapy was defined as the prescription of 1 antipsychotic medication at the time of discharge. Antipsychotic polypharmacy was defined as the coprescription of >1 antipsychotic medication for an individual patient. It is important to note that this study did not assess all medications on which a patient was discharged; the focus was only on antipsychotic medications.
TABLE 1.
Hospital Based Inpatient Psychiatric Services (HBIPS) Core Performance Measures 4 and 5 as Defined by The Joint Commission
To gain a better understanding of antipsychotic polypharmacy, rates of polypharmacy were calculated in 2 ways. The prevalence or unadjusted antipsychotic polypharmacy rate was calculated as the number of discharges in which antipsychotic polypharmacy was prescribed divided by the total number of discharges during a given period. The unadjusted polypharmacy rate therefore includes patients who were not prescribed any antipsychotic medication in the denominator. To allow for better comparison across hospitals and to reinforce best practices, an adjusted polypharmacy rate was also calculated as follows: the number of discharges in which antipsychotic polypharmacy was prescribed divided by the number of discharges in which at least 1 antipsychotic medication was prescribed during a given period. The adjusted polypharmacy rate was defined in the HBIPS 4 measure and is used in public reporting by both TJC and the Centers for Medicare & Medicaid Services (CMS). Unadjusted and adjusted antipsychotic polypharmacy rates are provided for total populations as well as for demographic or clinical subgroups.
Study Population and Sample
The secondary analysis described in this article examined the use of antipsychotic medications among a national sample of state psychiatric inpatient hospitals. State psychiatric inpatient hospitals included in the study were enrolled in NRI’s BHPMS and participating in the HBIPS core measure data set at the time of the study; these hospitals represented approximately 80% of all state psychiatric inpatient hospitals serving adults. The study sample consisted of all discharges of adults 18 to 64 years of age between January 1 and December 31, 2011 for whom HBIPS data were provided. Although hospitals are permitted to provide a random sample of discharges, 83% of the hospitals provided complete data resulting in a study sample representing 78% of all discharges of adults from these hospitals. No exclusions were applied to the discharges that met the age requirement.
Mental Health Disorders
Hospitals submitted the mental health diagnosis codes active at the time of discharge using the International Classification of Diseases 9th Version, Clinical Modification (ICD-9-CM). A mental health disorder multilevel variable was created based on the frequency of the mental health disorders among patients. The hierarchy of mental health disorders was defined using the following 6 clusters: schizophrenia, depressive disorder, bipolar disorder, other psychoses, personality disorder, and anxiety disorder. A “no mental health disorder/other mental health disorders” category was created for those patients in whom none of those 6 diagnostic clusters was identified. Appendix A (http://links.lww.com/JPP/A9) shows the specific diagnostic codes associated with each diagnostic cluster. A patient’s primary, secondary, and tertiary diagnoses were reviewed to assign the patient to the appropriate cluster.
Other Characteristics
This study also explored differences in antipsychotic medication prescribing practices by region. The hospital’s location (state) was used to categorize discharges from hospitals as being in the Northeast, South, West, or Midwest. Appendix B shows the list of states by region (http://links.lww.com/JPP/A9).
The study also explored differences based on the calendar quarter of the discharges (1Q2011 through 4Q2011) to determine whether differences in medication prescribing practices occurred over time. The date of discharge was used to classify each discharge into a calendar quarter.
Descriptive Analysis
Cross tabulation determined the proportion of discharges with no antipsychotic medication prescribed, with antipsychotic monotherapy, and with antipsychotic polypharmacy by demographic covariates (gender, race, age, marital status, admission referral source, admission legal status, discharge type, living situation at discharge, discharge disposition, Medicare coverage, and length of stay) and by mental health disorder. Cross tabulation, t test, and analysis of variance (ANOVA) were also used to determine interaction among the demographic covariates. Mean comparisons were used to analyze the differences among study groups by age and length of stay at the continuous level. The χ2 test was used to evaluate for significant differences in antipsychotic medication prescribing by study region and by study quarter. Antipsychotic medication prescription practices were also investigated along the continuous age spectrum.
Further analyses were performed using data from the group who were discharged on antipsychotic polypharmacy. The percentage of antipsychotic polypharmacy in each participating state psychiatric inpatient hospital was explored and compared with the mean and median rates for the nation. The χ2 analysis was used to evaluate the prevalence of antipsychotic polypharmacy among discharged patients by mental health disorder and by study period. The reasons adult patients were discharged on antipsychotic polypharmacy were also explored. Hospitals have the option of reporting the names of the antipsychotic medications that are prescribed, and these data were used to evaluate the most frequent antipsychotic medication combinations.
Inferential Analysis
A binary logistic regression determined the likelihood of antipsychotic polypharmacy in a discharged sample. The logistic regression model included patient characteristics that were both available through NRI’s BHPMS, and that are common to other data systems (eg, available through TJC or through the CMS data systems). The use of this model assured that it could be replicated using a different data source or sample. Patient characteristics were entered in 4 steps. Step 1 included gender, age group, length of stay, and mental health disorders. Step 2 added Medicare coverage. Step 3 added discharge disposition. Step 4 added the interaction terms between each mental health disorder and length of stay. Odds ratios (95% confidence intervals) and P-values were calculated.
RESULTS
This study analyzed data from 86,034 discharges from 160 state psychiatric inpatient hospitals in 46 states and territories during calendar year 2011. The characteristics for patients discharged on no antipsychotic, antipsychotic monotherapy, and antipsychotic polypharmacy are presented in Table 2. Overall, the sample included a higher proportion of male (63%), white (58%), and never married (66%) patients. Discharged patients were, on average, 38 years old with an average length of stay of 116 days. Most discharged patients had an involuntary admission (89%), and one third of the patients were referred by the justice system. Eighty-five percent of patients had completed inpatient treatment at the time of discharge and 57% were discharged to a private house. Forty percent of the patients had a diagnosis of schizophrenia, followed by depressive disorders (24%), bipolar disorder (11%), other psychoses (6%), personality disorder (5%), and anxiety disorder (3%). Eleven percent were discharged with no mental health disorder or with a disorder not covered in this study.
TABLE 2.
Proportion of Discharges From State Psychiatric Inpatient Hospitals by Study Group
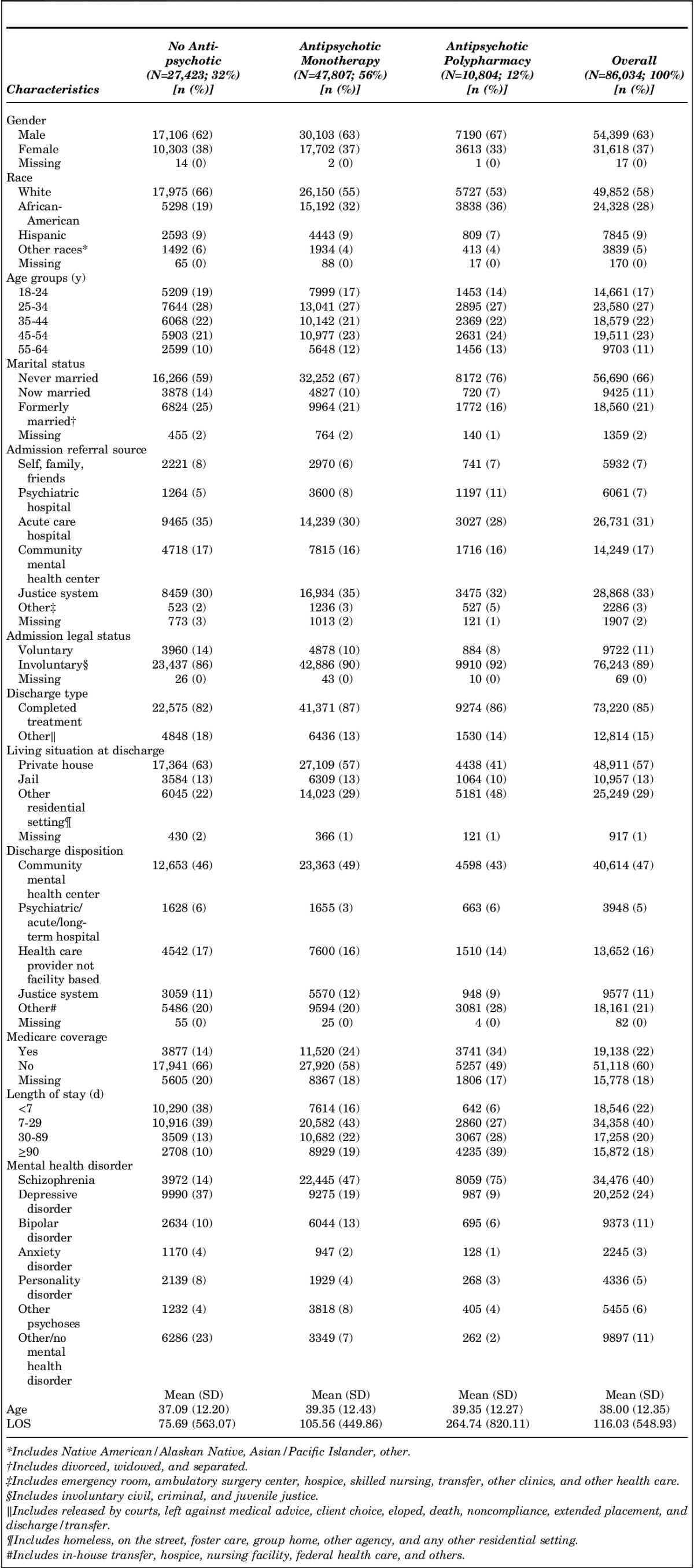
Among all discharges, 32% were not prescribed an antipsychotic medication at discharge, 56% were prescribed antipsychotic monotherapy, and 12% (unadjusted rate) were prescribed antipsychotic polypharmacy. Of the patients discharged with at least 1 antipsychotic medication, 18% were discharged on antipsychotic polypharmacy (adjusted antipsychotic polypharmacy rate).
Statistical analysis showed that patients who were male (67%), white (53%), 45 to 64 years old (37%), never married (76%), referred by the justice system (32%), discharged to a residential setting other than home or jail (48%), not covered by Medicare (49%), with longer stays or length of stays of 90 days or more (39%), and with a diagnosis of schizophrenia (75%) were disproportionately discharged on antipsychotic polypharmacy compared with the other categories in each characteristic. Patients discharged on no antipsychotic medication had significantly shorter lengths of stay (76 d) compared with patients discharged on antipsychotic monotherapy (106 d), and patients discharged on antipsychotic polypharmacy (265 d).
Differences by diagnosis cluster were also found. Patients in the group with schizophrenia (22,445/34,476), bipolar disorder (6044/9373), or other psychoses (3818/5455) were more likely to be discharged on antipsychotic monotherapy. Patients in the group with a depressive disorder (9990/20,252), anxiety disorder (1170/2245), or personality disorder (2139/4336) and patients with no mental health disorder/other disorder (6286/9897) were more likely to be discharged with no antipsychotic medication.
Given these relationships between antipsychotic polypharmacy and gender, race, age, marital status, admission referral source, living situation at discharge, Medicare coverage, and length of stay, bivariate relationships among these covariates were assessed (Appendix C) (http://links.lww.com/JPP/A9). Overall, marital status (never having been married) was found to be related to gender (male; χ22=3283.73, P<0.01), to race (African American; χ26=2839.33, P<0.01), to younger age (35 y or younger; F2,84,674=6921.43, P<0.01), and to longer length of stay (137 d or more; F2,84,674=135.56, P<0.01). Gender (female) was related to older age (39 y and older; t86,015=23.56, P<0.01), and to shorter length of stay (83 d or less; t86,015=13.52, P<0.01). White race was related to older age (39 y and older; F3,85,860=294.63, P<0.01), and African American race was related to longer length of stay (147 d or more; F3,85,860=37.97, P<0.01). Length of stay tended to increase with an increase in age (F4,86,033=267.78, P<0.01).
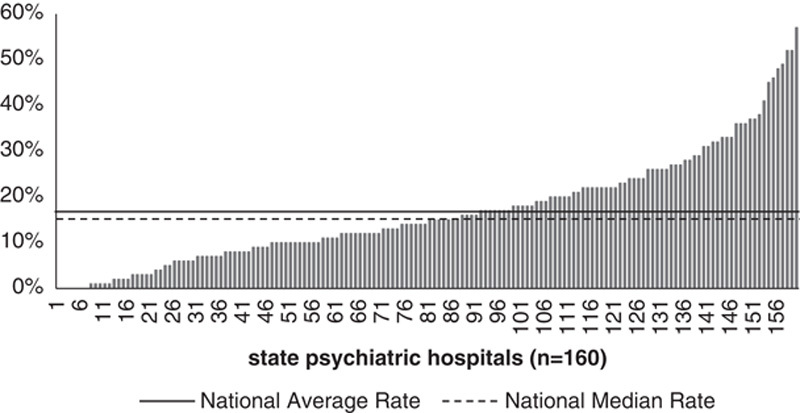
Prevalence of Prescription of Antipsychotic Medication by Study Region and by Study Quarter
Discharges on antipsychotic monotherapy (61%; 24,421/40,169) prevailed in the South. The Northeast region had the highest proportion of patients discharged on antipsychotic polypharmacy (20%; 2522/12,895) (Fig. 1). Given an unadjusted polypharmacy rate almost twice that of the other regions, analysis of patient characteristics indicated that significantly more patients in the Northeast region were older, had longer lengths of stay, and had a higher rate of schizophrenia diagnoses compared with the other regions, all factors previously shown to be related to higher rates of antipsychotic polypharmacy. Finally, the West region discharged the highest proportion of patients (45%; 5714/12,730) on no antipsychotic medication. When using the adjusted antipsychotic polypharmacy rate, the difference across regions was markedly lower with the Northeast region having the highest rate (26%; 2522/9769), and the South having the lowest rate (15%; 4239/28,660), and the Midwest (2645/13,166) and the West (1398/7016) regions falling in the middle (20%).
FIGURE 1.
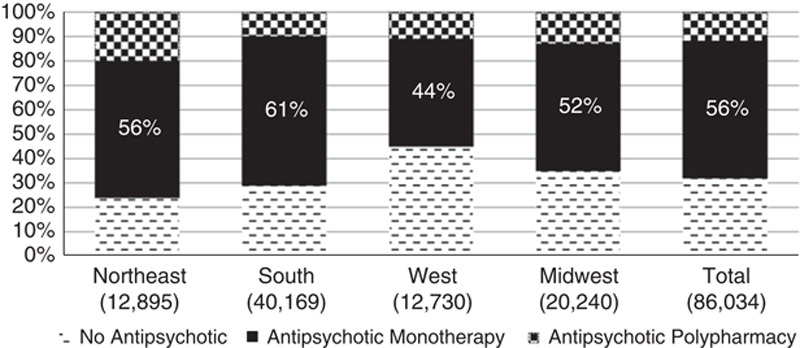
Prevalence of prescription of antipsychotic medication by study region.
No significant differences were found in the rate of antipsychotic polypharmacy among discharges by study quarter. However, in all quarters, the majority of patients were discharged on antipsychotic monotherapy.
Prevalence of Prescription of Antipsychotic Medication by Patient Age
The prevalence of antipsychotic medication prescribing practices along the age continuum was also explored (Fig. 2). The majority of patients were discharged on antipsychotic monotherapy. The slight upward trend of discharged patients on antipsychotic polypharmacy was constant as age increased. The prevalence of no antipsychotic medication being prescribed decreased with an increase in age. Increased age of a patient was positively associated with an increased likelihood of receiving antipsychotic polypharmacy.
FIGURE 2.
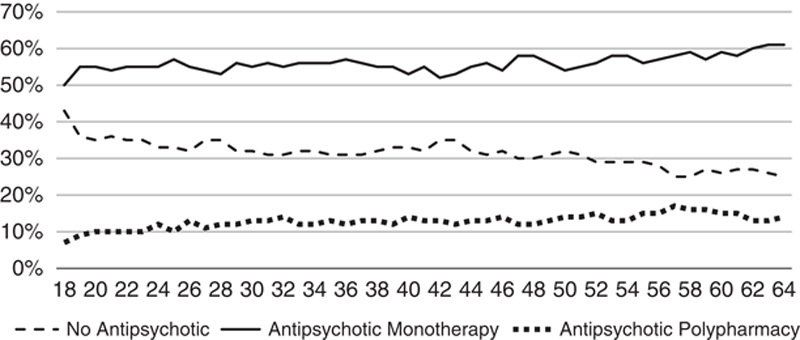
Percent of discharged patients by study group by age.
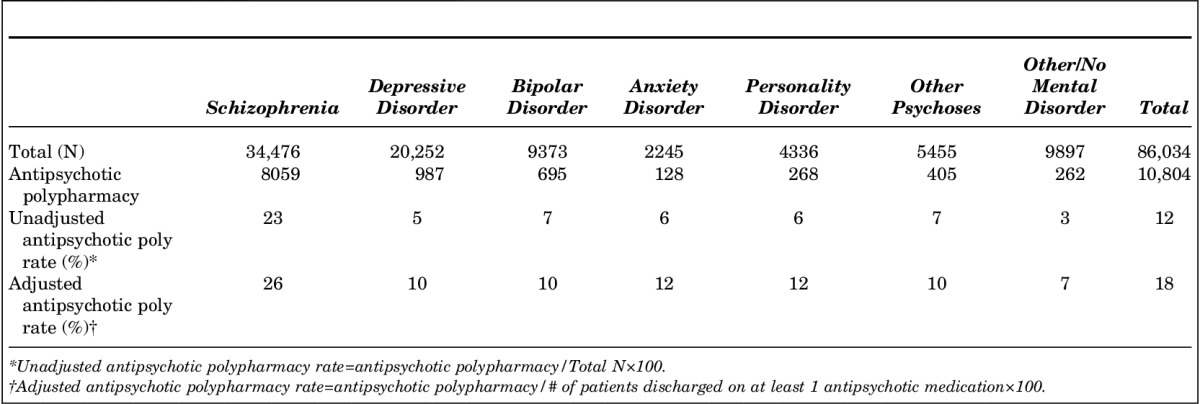
Percent of Polypharmacy in Each State Psychiatric Inpatient Hospital
Discharges from hospitals ranged from 2 to 3308, with an average of 538 discharges, and a median of 317 discharges per hospital in 2011. Hospitals discharged between 0% and 57% of their patients on antipsychotic polypharmacy (unadjusted rate), with an average of 17% and a median of 15% on antipsychotic polypharmacy (Fig. 3).
FIGURE 3.
Percent of antipsychotic polypharmacy in each state psychiatric hospital.
Reasons for Discharging Patients on Antipsychotic Polypharmacy
Patients were discharged on antipsychotic polypharmacy mainly to reduce symptoms (37%), due to a history of a minimum of 3 or more failed trials of monotherapy (19%), and due to a recommended plan to taper to monotherapy (10%). Although the patterns were relatively constant across patient ages, some notable differences were identified (Fig. 4). A history of 3 or more failed trails of monotherapy was more prevalent in older than younger patients. A recommended plan to taper to monotherapy was more prevalent in young adults (18 to 22 y of age) than in other adults.
FIGURE 4.
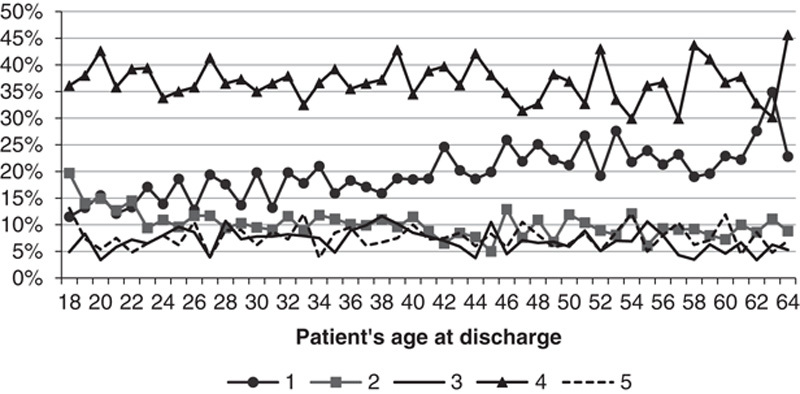
Reasons for discharging adult patients on antipsychotic polypharmacy (n=10,804). 1, History of a minimum of 3 or more failed trials of monotherapy; 2, Recommended plan to taper to monotherapy; 3, Augmentation of clozapine; 4, Sympton reduction; 5, Admitted on multiple antipsychotics.
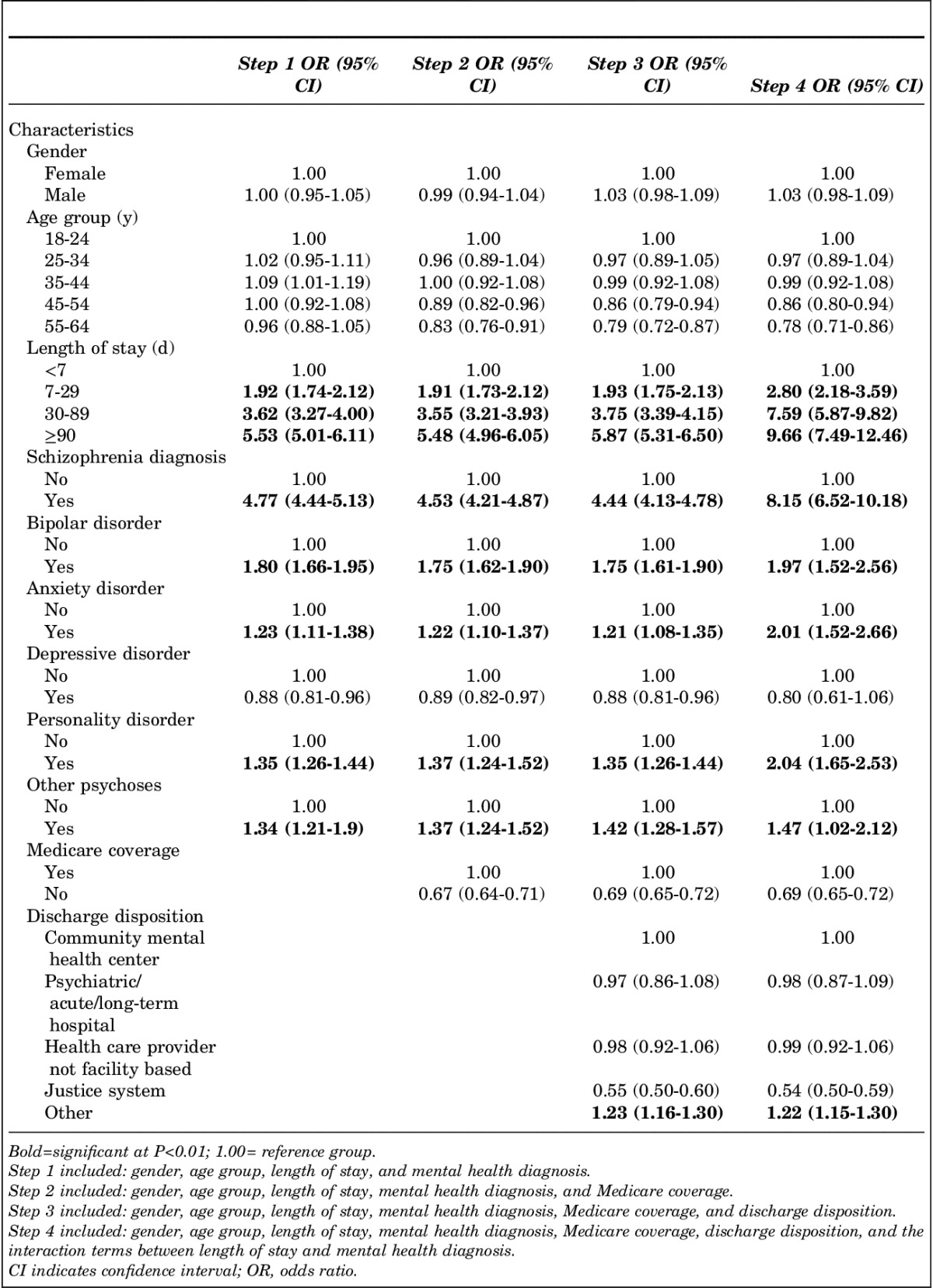
Antipsychotic Polypharmacy and Mental Health Disorders
Among patients discharged on antipsychotic polypharmacy, the majority had a diagnosis of schizophrenia (Table 3). Overall, 23% (8059/34,476) of patients with a diagnosis of schizophrenia were discharged on antipsychotic polypharmacy compared with 5% to 7% for all other diagnoses under study, nearly a 5-fold difference. However, the adjusted polypharmacy rate by diagnosis indicates a 2.6-fold difference.
TABLE 3.
Unadjusted and Adjusted Rates of Antipsychotic Polypharmacy Within Each Mental Disorder
Antipsychotic Polypharmacy Medication Combinations
Although the names of specific antipsychotic medications is optional information provided by the hospitals, data concerning specific medications were provided for nearly half of the patients discharged on antipsychotic polypharmacy. However, this was not a random representation of patients as several large states chose not to report these optional data. Therefore, analysis of medication combinations was not advisable as results would not be representative.
Likelihood of Antipsychotic Polypharmacy in a Discharged Sample
Table 4 presents the results of the logistic regression, using characteristics associated with being discharged on antipsychotic polypharmacy. The strongest characteristics were length of stay and a diagnosis of schizophrenia. Although gender, age, and Medicare coverage were found to be significantly related to antipsychotic polypharmacy, their importance was removed when including length of stay and diagnosis. When discharge disposition was added (Step 3), patients discharged to other (health care facilities) were more likely to be discharged on antipsychotic polypharmacy. When length of stay and diagnosis were entered as interaction terms (Step 4), the likelihood of a patient being discharged on antipsychotic polypharmacy almost doubled, reaching nearly 10 times the likelihood of receiving antipsychotic polypharmacy for patients with length of stay >90 days compared with extremely short stays and >8 times the likelihood for patients with a diagnosis of schizophrenia compared with others.
TABLE 4.
Likelihood of Antipsychotic Polypharmacy for Patients Discharged From State Psychiatric Inpatient Hospitals
DISCUSSION
The purpose of this study was to evaluate the prevalence of antipsychotic polypharmacy in a national sample of discharges from state psychiatric inpatient hospitals. It was found that the overall antipsychotic polypharmacy rate was 12%, with an adjusted rate of 18% for patients who were discharged on 1 or more antipsychotic medications. These rates were comparable with polypharmacy rates reported in the literature, such as 21% in Medicaid claims,22 and 14% for outpatients on Medicaid.26 In this study, the antipsychotic polypharmacy rate was higher (23%) for patients discharged with a diagnosis of schizophrenia, with an adjusted rate of 26% for patients with schizophrenia who were discharged on 1 or more antipsychotic medications. In 2011, the first year of reporting the HBIPS 4 measure, the national adjusted polypharmacy rate reported by TJC for adults 18 to 64 years of age was 15%. A comparable study performed in a New York state psychiatric inpatient hospital, which included only patients with a diagnosis of schizophrenia, found rates of 22% for antipsychotic polypharmacy with second generation antipsychotics at baseline, which underrepresents total antipsychotic polypharmacy as it does not include patients receiving first-generation agents.30
Antipsychotics are prescribed to decrease symptoms and suffering and, ideally, improve functioning,31 with symptom reduction the standard measure of therapeutic efficacy.15 This study found that clinicians reported using antipsychotic polypharmacy primarily to reduce patients’ symptoms (37%), which is consistent with other findings.3,32 Given the high prevalence of this rationale, additional studies may be needed to determine whether there is a new science base for this justification for patients with a diagnosis of schizophrenia. This finding, however, also poses concerns when the appropriateness of this rationale is not scientifically validated and also demonstrates lower performance on the publicly reported measures of antipsychotic medication use (HBIPS 4 and 5).18 As hospitals are required to report their performance on standardized core measures,19 the implication of not meeting minimum requirements from payers and accreditation agencies will result in below-target measure rates. TJC uses the HBIPS 5 measure rate in a hospital’s overall evaluation of performance, with a target of 85% compliance on best practices for all patients and all conditions.33 In the future, the CMS Inpatient Psychiatric Facility Quality Reporting Program is expected to move from a pay-for-reporting model to pay-for-performance, and consequently failure to meet minimum performance thresholds will result in reduced funding.
This study found that 36% of patients receiving antipsychotic polypharmacy had one of the recognized appropriate justifications according to TJC standards: 19% had a history of a minimum of 3 or more failed trials of monotherapy, 10% were recommended a plan to taper to monotherapy, and 7% were in clozapine augmentation. Although multiple and unsuccessful trials of monotherapy and augmentation of clozapine were justified by clinical guidance and research studies, recommending a taper to monotherapy reflects a reality of contemporary inpatient psychiatric care.19 However, these justifications were developed on the basis of analysis of already published studies that included only patients with schizophrenia or schizoaffective disorder who were not necessarily receiving psychiatric services in inpatient settings.19 In this study, 75% of the patients on antipsychotic polypharmacy had a diagnosis of schizophrenia. The low percentages for the 3 appropriate justifications suggest that implementation of the proposed best practices are taking place at a low rate. It could also suggest the need for accreditation agencies to revise and validate current standards and definitions of measures that could be more appropriate for psychiatric inpatient hospitals.
Because of lack of reporting of the names of antipsychotic medications (optional data) from the larger states in the sample, analysis of antipsychotic medication combinations was constrained. The rationale of clozapine augmentation was provided for only 7% of discharges in which antipsychotic polypharmacy was prescribed. A study using a similar population in state psychiatric inpatient hospitals found that augmentation of clozapine was provided to <50% of patients compared with augmentation of risperidone (to 69% of patients) and olanzapine (to 91%),30 which is counter to current clinical guidelines for patients with a diagnosis of schizophrenia.15,34,35 These findings support suggestions that antipsychotic polypharmacy is often tried before clozapine monotherapy,28 clozapine utilization is low,15 and current guidelines for polypharmacy do not represent usual practice for patients with severe mental illness.
Our findings showed that rates of antipsychotic polypharmacy differ by geographic region. The Northeast had the highest adjusted polypharmacy rate, with 26% of patients discharged on antipsychotic polypharmacy. In the West, 45% of patients were discharged on no antipsychotic medications, which converted to an adjusted polypharmacy rate of 20%. Although patient characteristics were highlighted to interpret a higher rate of polypharmacy in the Northeast, regional differences warrant further research to determine the causes of the variation and potentially the implementation of best practices to reduce antipsychotic polypharmacy.
On the basis of the logistic regression, the strongest predictors for patients being discharged on antipsychotic polypharmacy were a length of stay of 90 days or more and a diagnosis of schizophrenia. These 2 characteristics almost double the risk effect when the interaction terms between them were included in the model. State psychiatric inpatient hospitals have a significant proportion of patients with a diagnosis of schizophrenia (40%) and nearly 20% of patients who experience a longer hospital stay, suggesting a high-risk population needing special attention. Patients with depressive disorders were not at risk of antipsychotic polypharmacy and were as likely to receive no antipsychotic medications as antipsychotic monotherapy, which is consistent with the Food and Drug Administration’s 2006 approval for the use of antipsychotic medications with treatment-resistant major depressive episodes.
Limitations
This study had a number of limitations. The study group consisted of patients discharged from 160 state psychiatric inpatient hospitals across 46 states and territories, representing 80% of all state psychiatric inpatient hospitals for adults. In reporting on the HBIPS measures, hospitals are permitted to randomly select a sample of discharges in each month where the sampling methods would provide a representative sample of the original population. The vast majority of state psychiatric inpatient hospitals do not submit a random sample for the HBIPS measures but rather provide complete data. Therefore only data from the hospitals that provided complete data were included in this study, representing 78% of all state psychiatric inpatient discharges in 2011. This study used discharges, not a unique count of patients; therefore comparisons for patients with long-term episodes of care and patients with multiple episode of care were not undertaken. However, it is known that long-term residents represent 21% of the total episodes of care in a given year in state psychiatric inpatient hospitals.36 The publicly posted HBIPS 4 and 5 measures include only patients with planned discharges; therefore comparisons with the adjusted rate for the study group do not address the unknown percentage of unplanned discharges, for example, when a patient leaves against medical advice or is released by the judicial system. Data available for the study allow an assessment of the prescribing practices for multiple antipsychotic medications at discharge. The number of antipsychotic medications on admission and changes in medications during the hospital stay are unknown and would be an area for further study. Anecdotal evidence from some state psychiatric inpatient hospitals indicates that there has been a move to reduce the number of antipsychotic medications during the stay from 3 or more down to 2 agents at discharge, with the ultimate goal of further stabilization and a reduction to monotherapy in collaboration with the outpatient provider. Information on patients’ adherence to medication regimens involving multiple antipsychotics after discharge is unknown and would be an area for further study. Finally, this study focused on state psychiatric inpatient hospitals which could limit the generalizability of the findings to other psychiatric inpatient providers. Nevertheless, the study provides foundational data for this particular population which is greatly overlooked in the current literature.
CONCLUSIONS
Overall, the adjusted antipsychotic polypharmacy rate reported by TJC has decreased from 15% in 2011 to 13% in 201323 across nearly 600 psychiatric hospitals. CMS provided its first reporting of the adjusted polypharmacy rate for 2013 at 11% for adults 18 to 64 years of age across >1600 psychiatric hospitals.37 The prevalence of antipsychotic polypharmacy is thus an issue that needs continued attention.
This study found that the most significant factors contributing to higher rates of antipsychotic polypharmacy were a diagnosis of schizophrenia and longer hospitalizations. The rationale of symptom reduction was provided as often as all 3 TJC-defined appropriate justifications for polypharmacy combined (a history of 3 or more failed antipsychotic monotherapy trials, cross-titrating antipsychotic medications to work toward monotherapy, or the augmentation of clozapine). Given this fuller understanding of the factors contributing to antipsychotic polypharmacy in state psychiatric inpatient hospitals, some insights into quality initiatives that could help further reduce the use of antipsychotic polypharmacy can be gained.
Antipsychotic polypharmacy continues at a high enough rate to impact nearly 10,000 patients with a diagnosis of schizophrenia each year in state psychiatric inpatient hospitals. Given such a large sample, further analysis of the clinical presentations of these patients may highlight particular aspects of the illness and its previous treatment that are contributing to practices outside the best practice guidelines. Patients with multiple hospitalizations and patients with long hospitalizations may have such complex medical record documentation that information from previous stays has been purged, limiting the extent of the previous antipsychotic medication history available to the current physician. Thus, failed trials of monotherapy may be difficult or nearly impossible to abstract from a patient’s record. Physician grand rounds may be an avenue for further understanding the clinical rationales for both medication choices as well as polypharmacy. Physician consultation may be another avenue for developing strategies to reduce the number of antipsychotic medications during the hospitalization while maintaining functioning. Administrative policies may also have affected formulary options for physicians, resulting in the antipsychotic medication prescribing profile observed in this study. Basing these discussions on objective data that include trends over time, patient characteristics, and national benchmarks provides an opportunity for informed decision-making that is sensitive to the needs of patients and cognizant of other hospitals’ accomplishments toward best practices.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's Website, www.psychiatricpractice.com.
ACKNOWLEDGMENT
The authors thank G. Michael Lane, Jr, MA, MPH, for proofreading the manuscript from a clinical point of view.
Footnotes
Supported by the National Association of State Mental Health Program Directors Research Institute Inc.
The authors declare no conflicts of interest.
REFERENCES
- 1.Ananth J, Parameswaran S, Gunatilake S. Antipsychotic polypharmacy. Curr Pharm Des. 2004;10:2231–2238. [DOI] [PubMed] [Google Scholar]
- 2.Fisher MD, Reilly K, Isenberg K, et al. Antipsychotic patterns of use in patients with schizophrenia: polypharmacy versus monotherapy. BMC Psychiatry. 2014;14:341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fleischhacker WW, Uchida H. Critical review of antipsychotic polypharmacy in the treatment of schizophrenia. Int J Neuropsychopharmacol. 2014;17:1083–1093. [DOI] [PubMed] [Google Scholar]
- 4.Canadian Psychiatric Association. Clinical practice guidelines. Treatment of schizophrenia. Can J Psychiatry. 2005;50(suppl 1):7S–57S. [PubMed] [Google Scholar]
- 5.Gaebel W, Weinmann S, Sartorius N, et al. Schizophrenia practice guidelines: international survey and comparison. Br J Psychiatry. 2005;187:248–255. [DOI] [PubMed] [Google Scholar]
- 6.Lehman AF, Lieberman JA, Dixon LB, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(suppl):1–56. [PubMed] [Google Scholar]
- 7.Moore TA, Buchanan RW, Buckley PF, et al. The Texas Medication Algorithm Project antipsychotic algorithm for schizophrenia: 2006 update. J Clin Psychiatry. 2007;68:1751–1762. [DOI] [PubMed] [Google Scholar]
- 8.National Institute for Clinical Excellence. Clinical Guideline I Schizophrenia: Core Interventions in the Treatment and Management of Schizophrenia in Primary and Secondary Care. London: National Institute for Clinical Excellence; 2002. [Google Scholar]
- 9.Diaz E, Neuse E, Sullivan MC, et al. Adherence to conventional and atypical antipsychotics after hospital discharge. J Clin Psychiatry. 2004;65:354–360. [DOI] [PubMed] [Google Scholar]
- 10.Chakos MH, Glick ID, Miller AL, et al. Baseline use of concomitant psychotropic medications to treat schizophrenia in the CATIE trial. Psychiatr Serv. 2006;57:1094–1101. [DOI] [PubMed] [Google Scholar]
- 11.Clark RE, Bartels SJ, Mellman TA, et al. Recent trends in antipsychotic combination therapy of schizophrenia and schizoaffective disorder: implications for state mental health policy. Schizophr Bull. 2002;28:75–84. [DOI] [PubMed] [Google Scholar]
- 12.Freudenreich O, Goff DC. Antipsychotic combination therapy in schizophrenia. A review of efficacy and risks of current combinations. Acta Psychiatr Scand. 2002;106:323–330. [DOI] [PubMed] [Google Scholar]
- 13.Tsutsumi C, Uchida H, Suzuki T, et al. The evolution of antipsychotic switch and polypharmacy in natural practice—a longitudinal perspective. Schizophr Res. 2011;130:40–46. [DOI] [PubMed] [Google Scholar]
- 14.Zink M, Englisch S, Meyer-Lindenberg A. Polypharmacy in schizophrenia. Curr Opin Psychiatry. 2010;23:103–111. [DOI] [PubMed] [Google Scholar]
- 15.Ballon J, Stroup TS. Polypharmacy for schizophrenia. Curr Opin Psychiatry. 2013;26:208–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rapp MS, Kaplan A. Polypsychopharmacy revisited. Can J Psychiatry. 1981;26:569–573. [DOI] [PubMed] [Google Scholar]
- 17.Goren J, Parks J, Ghinassi F, et al. When is antipsychotic polypharmacy supported by research evidence? Implications for QI. Jt Comm J Qual Patient Saf. 2008;34:571–582. [DOI] [PubMed] [Google Scholar]
- 18.The Joint Commission. Specifications Manual for Joint Commission National Quality Core Measures. Oakbrook Terrace, IL: The Joint Commission; 2014. [Google Scholar]
- 19.Goren JL, Beck SE, Mills BJ, et al. Development and delivery of a quality improvement program to reduce antipsychotic polytherapy. J Manag Care Pharm. 2010;16:393–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thompson A, Sullivan SA, Barley M, et al. The DEBIT trial: an intervention to reduce antipsychotic polypharmacy prescribing in adult psychiatry wards—a cluster randomized controlled trial. Psychol Med. 2008;38:705–715. [DOI] [PubMed] [Google Scholar]
- 21.Patrick V, Schleifer SJ, Nurenberg JR, et al. Best practices: an initiative to curtail the use of antipsychotic polypharmacy in a state psychiatric hospital. Psychiatr Serv. 2006;57:21–23. [DOI] [PubMed] [Google Scholar]
- 22.Constantine RJ, Andel R, Tandon R. Trends in adult antipsychotic polypharmacy: progress and challenges in Florida’s Medicaid program. Community Ment Health J. 2010;46:523–530. [DOI] [PubMed] [Google Scholar]
- 23.The Joint Commission. America’s Hospitals: Improving Quality and Safety —The Joint Commission’s Annual Report. Oakbrook Terrace, IL: The Joint Commission; 2014. Available at: http://www.jointcommission.org/assets/1/18/tjc_annual_report_2014_final.pdf. Accessed May 2, 2016. [Google Scholar]
- 24.Depp C, Ojeda VD, Mastin W, et al. Trends in use of antipsychotics and mood stabilizers among Medicaid beneficiaries with bipolar disorder, 2001–2004. Psychiatr Serv. 2008;59:1169–1174. [DOI] [PubMed] [Google Scholar]
- 25.Ganguly R, Kotzan JA, Miller LS, et al. Prevalence, trends, and factors associated with antipsychotic polypharmacy among Medicaid-eligible schizophrenia patients, 1998–2000. J Clin Psychiatry. 2004;65:1377–1388. [DOI] [PubMed] [Google Scholar]
- 26.Gilmer TP, Dolder CR, Folsom DP, et al. Antipsychotic polypharmacy trends among Medicaid beneficiaries with schizophrenia in San Diego County, 1999–2004. Psychiatr Serv. 2007;58:1007–1010. [DOI] [PubMed] [Google Scholar]
- 27.Morrato EH, Dodd S, Oderda G, et al. Prevalence, utilization patterns, and predictors of antipsychotic polypharmacy: experience in a multistate Medicaid population, 1998–2003. Clin Ther. 2007;29:183–195. [DOI] [PubMed] [Google Scholar]
- 28.Velligan DI, Carroll C, Lage MJ, et al. Outcomes of Medicaid beneficiaries with schizophrenia receiving clozapine only or antipsychotic combinations. Psychiatr Serv. 2015;66:127–133. [DOI] [PubMed] [Google Scholar]
- 29.Department of Health and Human Services. State Medicaid Manual CMS Pub 45. Washington, DC: Department of Health and Human Services; 1994. Available at: https://cms.gov/Regulations-and-Guidance/guidance/Manuals/Paper-Based-Manuals-Items/CMS021927.html. Accessed May 3, 2016. [Google Scholar]
- 30.Megna JL, Kunwar AR, Mahlotra K, et al. A study of polypharmacy with second generation antipsychotics in patients with severe and persistent mental illness. J Psychiatr Pract. 2007;13:129–137. [DOI] [PubMed] [Google Scholar]
- 31.Gallego JA, Nielsen J, De HM, et al. Safety and tolerability of antipsychotic polypharmacy. Expert Opin Drug Saf. 2012;11:527–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sernyak MJ, Rosenheck R. Clinicians’ reasons for antipsychotic coprescribing. J Clin Psychiatry. 2004;65:1597–1600. [DOI] [PubMed] [Google Scholar]
- 33.The Joint Commission (TJC). Benchmark. Oakbrook Terrace, IL: TJC; 2011. [Google Scholar]
- 34.Argo T, Crismon ML, Miller AL, et al. Texas Medication Algorithm Project Procedural Manual: Schizophrenia Treatment Algorithm. Austin, TX: Texas Department of State Health Services; 2007. Available at: https://www.jpshealthnet.org/sites/default/files/tmapalgorithmforschizophrenia.pdf. Accessed May 2, 2016. [Google Scholar]
- 35.Buchanan R, Kreyengbuhl J, Kelly D, et al. The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr Bull. 2010;36:71–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hollen V, Ortiz G. Characteristics of State-Operated or Supported Psychiatric Hospital Inpatient Care. Falls Church, VA: National Association of State Mental Health Program Directors Research Institute Inc.; 2013. Available at: http://www.createspace.com/4106422. [Google Scholar]
- 37.Data. Medicare.Gov Web site. Inpatient Psychiatric Facility Quality Measure Data—National; 2015. Available at: https://data.medicare.gov/Hospital-Compare/Inpatient-Psychiatric-Facility-Quality-Measure-Dat/s5xg-sys6. Accessed May 27, 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's Website, www.psychiatricpractice.com.


