Abstract
Introduction:
Leiomyoma of the bladder is a rare tumor arising from the submucosa. Most patients with bladder leiomyoma may present with urinary frequency or obstructive urinary symptoms. However, there are a few cases of bladder leiomyoma coexisting with uterine leiomyoma presenting as dyspareunia. We herein report an unusual case of coexisting bladder leiomyoma and uterine leiomyoma presenting as dyspareunia.
Case presentation:
A 44-year-old Asian female presented to urologist and complained that she had experienced dyspareunia over the preceding several months. A pelvic ultrasonography revealed a mass lesion located in the trigone of urinary bladder. The mass lesion was confirmed on contrast-enhanced computed tomography (CT). The CT scan also revealed a lobulated and enlarged uterus consistent with uterine leiomyoma. Then, the biopsies were then taken with a transurethral resection (TUR) loop and these biopsies showed a benign proliferation of smooth muscle in a connective tissue stroma suggestive of bladder leiomyoma. An open local excision of bladder leiomyoma and hysteromyomectomy were performed successfully. Histological examination confirmed bladder leiomyoma coexisting with uterine leiomyoma.
Conclusion:
This case highlights a rare presentation of bladder leiomyoma, dyspareunia, as the chief symptom in a patient who had coexisting uterine leiomyoma. Bladder leiomyomas coexisting with uterine leiomyomas are rare and can present with a wide spectrum of complaints including without symptoms, irritative symptoms, obstructive symptoms, or even dyspareunia.
Keywords: dyspareunia, leiomyoma, leiomyoma of the bladder, uterine leiomyoma
1. Introduction
Female dyspareunia, defined as persistent or recurrent pain associated with penile–vaginal intercourse, can occur for a variety of reasons—ranging from physiological problems to psychological factors.[1] A medical evaluation for dyspareunia usually consists of a thorough medical history, a pelvic exam, or other tests such as pelvic ultrasonography. Leiomyoma is uncommon benign tumor of bladder.[2] Although bladder tumors is one of the most common malignancies worldwide,[3–5] leiomyoma accounts only for <1% of all the urinary bladder tumors.[6] Leiomyoma of bladder usually presents with obstructive voiding symptoms or irritative urinary symptoms. However, to our knowledge only, several previous cases had involved dyspareunia symptoms.[7] We herein report a rare case of both bladder leiomyoma and uterine leiomyoma coexisting in a female whose chief complaint was dyspareunia.
2. Case presentation
A 44-year-old Asian female, gravida 2, para 2, with no significant previous medical history, presented to urologist and complained that she had experienced dyspareunia over the preceding several months. The nature of the pain was a deep pain, which she experienced every time she attempted intercourse. She did not have vaginal discharge. No psychological factors can be found for her painful intercourse. She denied any episodes of gross hematuria, fever, chills, or irritative urinary symptoms. A pelvic bimanual examination was difficult to perform because of the patient's discomfort. No significant findings were detected on physical examination. Urinary tract infection was excluded as results of urinalysis and urine cytology were normal. The results of other laboratory tests including renal function, liver function, complete blood cell count, and coagulation function were also within the normal range.
A pelvic ultrasonography revealed a 6.6 × 5.8 cm2 mass lesion located in the trigone of urinary bladder. The mass lesion was confirmed on contrast-enhanced CT to be an enhanced 7.2 × 6.1 cm2 soft tissue mass in the right paravaginal area. CT scan also revealed a lobulated and enlarged uterus consistent with uterine leiomyoma (Fig. 1). There was no evidence of thickening of the urinary bladder wall and locoregional invasion. Flexible office cystoscopy was attempted and revealed a rounded, smooth, submucosal mass arising from the trigone of urinary bladder distorting the medial margin of both ureteric orifices. Double J stents could be passed with ease bilaterally. Retrograde pyelogram demonstrated no filling defects or dilation of the both ureters. The biopsies taken with a transurethral resection (TUR) loop showed a benign proliferation of smooth muscle in a connective tissue stroma suggestive of leiomyoma. After a careful discussion about the 2 options of further treatment, open surgical excision, and repeated TUR, the patient opted to receive open surgical excision. Then, an open local excision of this well-encapsulated tumor was performed, in which a 7.3 × 6.1 × 5.8 cm3 grayish-white tumor was removed (Fig. 2) and hysteromyomectomy was also performed at the same time. Histological examination revealed intersecting fascicles of smooth muscle (Figs 3, 4) without any evidence of malignant change and thus diagnosis of leiomyoma was confirmed. The postoperative period was uneventful, and the patient was discharged on postoperative day 10. The urinary catheter was removed after 2 weeks. Over an 8-month follow-up period, the patient made no complaint of dyspareunia and no bladder leiomyoma was detected by pelvic ultrasonography and cystoscopic examinations.
Figure 1.
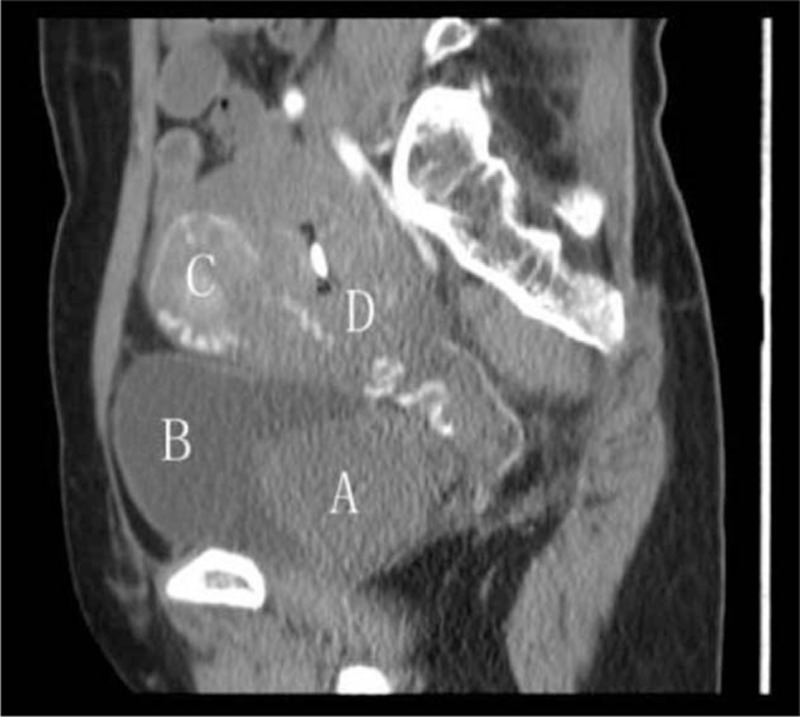
CT reveals round homogeneous solitary tumor protruding into the urinary bladder and lobulated enlargement of the uterus consistent with uterine leiomyoma: (A) bladder leiomyoma, (B) bladder, (C) uterine leiomyoma, (D) uterus. CT = computed tomography.
Figure 2.
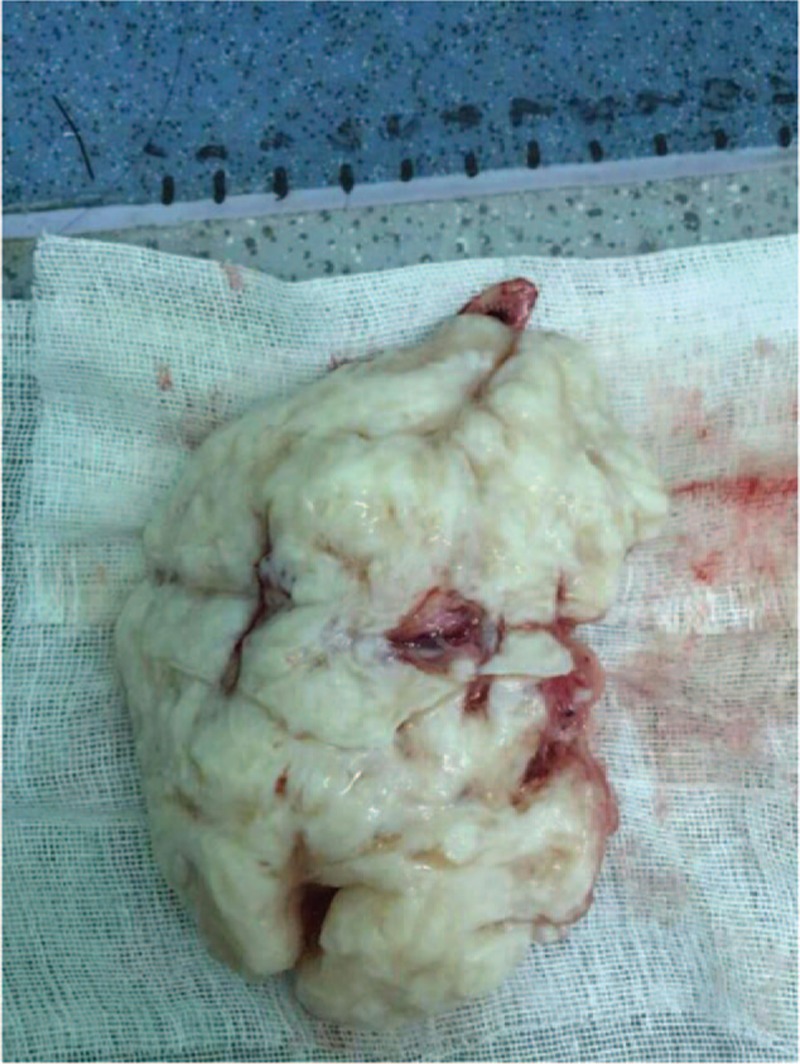
Grossly, the mass is white-gray in color. The specimen is 9.5 × 8.5 × 6.5 cm3 in size.
Figure 3.
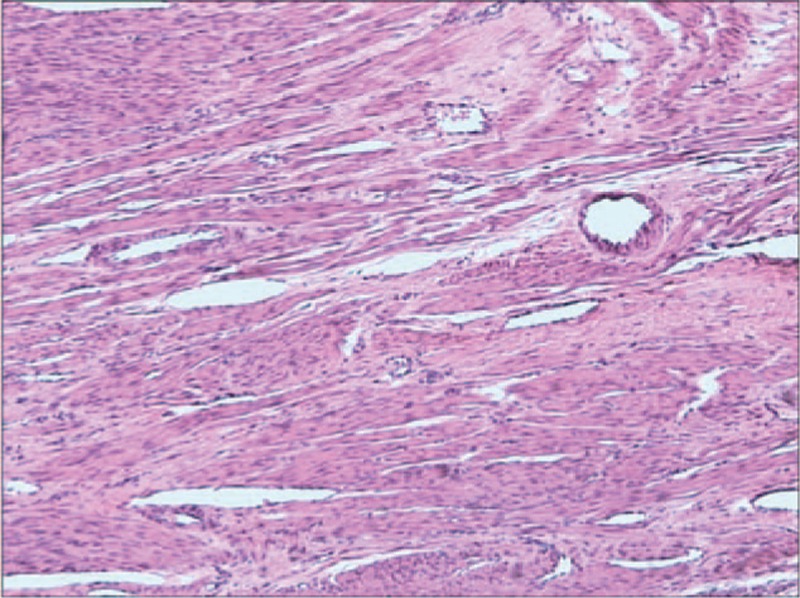
Bladder leiomyoma composed of intersecting fascicles of smooth muscle (HE, ×400). HE = hematoxylin and eosin.
Figure 4.
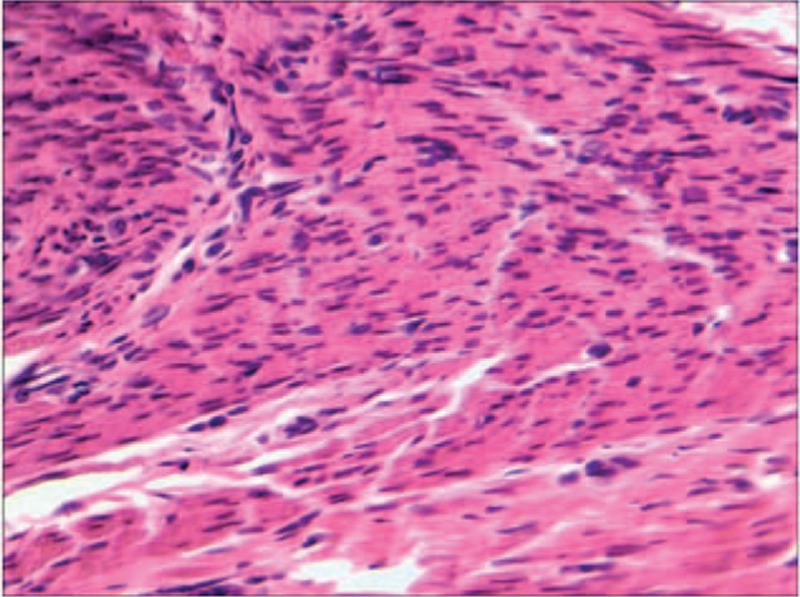
Uterine leiomyoma shows morphopathological changes similar to those of bladder leiomyoma (HE, ×400). HE = hematoxylin and eosin.
3. Discussion
Leiomyoma is a benign smooth muscle neoplasm or tumor that can occur in any organ, but it is most often seen in the uterus.[8,9] However, leiomyomas of the bladder are rare benign tumors.[10–12] The patient in this case had concomitant bladder leiomyoma and uterine leiomyoma which made the presentation even more uncommon. To our knowledge, only limited numbers of this kind of reports have been published.[13] The coexistence of these tumors in our case may have been merely coincidental, as their etiologic relationship is uncertain. It has recently been reported that uterine leiomyoma may be the similar disease as endometriosis.[14] Further studies are required to provide answers to etiologic relationship between bladder and uterine leiomyomas.
Leiomyoma of the bladder is the most common mesenchymal tumor in the bladder.[15] It was first reported by Virchow in 1931.[16] There are about 200 cases that have been reported in the medical literature.[10] A study showed that leiomyoma of the bladder was female preponderance (76%), and median age was 44 in 37 patients.[17] The precise etiology of this epidemiologic observation remains a mystery. However, it has been reported that estrogen may associate with the growth of leiomyomas.[8,18,19] The immunohistochemical and pathologic findings of bladder leiomyomas are similar to uterine leiomyomas.[20] It was suggested that estrogen may influence the development of bladder leiomyoma. In addition, estrogen receptors have been identified in urinary leiomyomas. In the present case, leiomyoma appeared in a premenopausal woman, which was consistent with what was reported in the prior clinical literature.[2,17] It was suggested that estrogen may have a certain relationship with bladder leiomyomas.[21,22] Further work is needed to clarify the concrete mechanism that can lead to the initiation of bladder leiomyoma.
There are similar morphopathological changes between bladder leiomyomas and uterine leiomyomas.[13] Microscopically, bladder leiomyomas are composed of interlacing and whorling bundles of smooth muscle cells. The nuclei of smooth muscle cells are oval to cigar-shaped, blunt-ended, centrally located and showing no nuclear atypia or mitotic activity.[2,23] Bladder leiomyoma usually have fewer than 2 mitotic figures per high power field.[17] Grossly, bladder leiomyoma can be intravesical, intramural, or extravesical. Of these 3 types of bladder leiomyomas, the intravesical forms are most likely to cause irritation, obstruction, or bleeding symptoms because they protrude into the lumen of the bladder.[24]
CT, MRI, and ultrasonography are regularly used to make the diagnosis of leiomyoma of the urinary bladder. Both CT and MRI can be used to assess the site, dimensions, and any extension of the tumor. Real-time imaging and transvaginal ultrasonography can give accurate information about localization of the mass and its relation to surrounding structures. However, none of them is a confirmatory method. The definitive diagnosis of leiomyoma of the urinary bladder and differentiation from leiomyosarcoma requires histopathological examination. Cystoscopy with biopsy of the mass will usually yield a definitive diagnosis.
Goluboff et al[17] reviewed all related literature and indicated that the most common symptoms for urinary leiomyoma were obstructive voiding symptoms (49%).Of the remaining patients, 38% presented with irritative symptoms, 11% with hematuria, and 19% were asymptomatic. However, Knoll et al[25] reviewed the literature and indicated that the most frequent clinical manifestations were irritative voiding symptoms. It was suggested that leiomyoma of the bladder are symptomatic for 2 reasons: anatomic location and size. Specifically, tumors that are present at ureteral openings or near the bladder neck tend to lead to obstructive symptoms, whereas larger tumors are more likely to cause irritative symptoms. In the present case, the tumors were located in the trigone of urinary bladder near the bladder neck and the chief complaint of our patient was dyspareunia. It was unusual and suggests that patients with dyspareunia may also require a careful urological evaluation.[7]
Finally, urologist and pathologists should be aware of the possibility that dyspareunia of unknown etiology may be resulted from the coexisting bladder and uterine leiomyomas.
4. Conclusions
In summary, this case study describes an unusual presentation of bladder leiomyoma, dyspareunia, as the chief symptom in a patient who also had uterine leiomyoma. Traditionally, the etiology of dyspareunia may include physical causes and psychological issues. Sometimes, it can be difficult for us to tell whether psychological factors or organic factors are associated with dyspareunia. However, it is necessary to take into account the possibility that the coexisting bladder and uterine leiomyomas may have an unusual clinical manifestation such as dyspareunia.
Footnotes
Abbreviations: CT = computed tomography, MRI = magnetic resonance imaging, TUR = transurethral resection.
Authorship: WL, JX, HL, and LJ contributed to the conception and design of the study. CS and SL conducted the work and collected the data. WL, LJ, CS, SL, and QZ drafted the manuscript. All authors approved the final version to be published.
Funding: This study was financially supported by the public project grant (2016C37138,2016C33244) from the Science and Technology Department of ZheJiang Province, China, and the public project grant (2014JYZB07) from the Science and Technology bureau of Lishui, ZheJiang Province, China. Informed patient consent was obtained for publication of this case report. The committee of human research at Wenzhou Medical University approved the study.
The authors have no conflicts of interest to disclose.
References
- 1.Ryan L, Hawton K. Female dyspareunia. BMJ 2004; 328:1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dewaele T, D’Hooghe L, Weyers S, et al. Leiomyoma of the urinary bladder. JBR-BTR 2014; 97:263. [DOI] [PubMed] [Google Scholar]
- 3.Han E, Jang SY, Kim G, et al. Rosiglitazone use and the risk of bladder cancer in patients with type 2 diabetes. Medicine 2016; 95:e2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shen Z, Xie L, Chen T, et al. Risk factors predictive of recurrence and progression for patients who suffered initial recurrence after transurethral resection of stage pT1 bladder tumor in Chinese population: a retrospective study. Medicine 2016; 95:e2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chou R, Selph SS, Buckley DI, et al. Treatment of muscle-invasive bladder cancer: a systematic review. Cancer 2016; 122:842–851. [DOI] [PubMed] [Google Scholar]
- 6.Jiang XZ, Xu C, Zhang NZ, et al. Influence of clinical characteristics and tumor size on symptoms of bladder leiomyoma: a pooled analysis of 61 cases. Chin Med J 2012; 125:2436–2439. [PubMed] [Google Scholar]
- 7.Kim IY, Sadeghi F, Slawin KM. Dyspareunia: an unusual presentation of leiomyoma of the bladder. Rev Urol 2001; 3:152–154. [PMC free article] [PubMed] [Google Scholar]
- 8.Peng S, Zhang L, Hu L, et al. Factors influencing the dosimetry for high-intensity focused ultrasound ablation of uterine fibroids: a retrospective study. Medicine 2015; 94:e650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luo X, Shu SR, Ma XF, et al. The research of feasibility and efficacy of radiofrequency ablation in treating uterine fibroids. Medicine 2015; 94:e1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu S. Imaging findings of atypical leiomyoma of the urinary bladder simulating bladder cancer: a case report and literature review. Med Ultrason 2013; 15:161–163. [DOI] [PubMed] [Google Scholar]
- 11.Ortiz M, Henao DE, Cardona Maya W, et al. Leiomyoma of the urinary bladder: a case report. Int Braz J 2013; 39:432–434. [DOI] [PubMed] [Google Scholar]
- 12.Erdem H, Yildirim U, Tekin A, et al. Leiomyoma of the urinary bladder in asymptomatic women. Urol Ann 2012; 4:172–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain SK, Tanwar R, Mitra A. Bladder leiomyoma presenting with LUTS and coexisting bladder and uterine leiomyomata: a review of two cases. Rev Urol 2014; 16:50–54. [PMC free article] [PubMed] [Google Scholar]
- 14.Baranov VS, Ivaschenko TE, Yarmolinskaya MI. Comparative systems genetics view of endometriosis and uterine leiomyoma: two sides of the same coin? Syst Biol Reprod Med 2016; 62:93–105. [DOI] [PubMed] [Google Scholar]
- 15.Tavora F, Kryvenko ON, Epstein JI. Mesenchymal tumours of the bladder and prostate: an update. Pathology 2013; 45:104–115. [DOI] [PubMed] [Google Scholar]
- 16.JL K. Leiomyoma of the bladder with a report of a case and a review of the literature. J Urol 1931; 26:575–589. [Google Scholar]
- 17.Goluboff ET, O’Toole K, Sawczuk IS. Leiomyoma of bladder: report of case and review of literature. Urology 1994; 43:238–241. [DOI] [PubMed] [Google Scholar]
- 18.Neto AG, Gupta D, Biddle DA, et al. Urinary bladder leiomyoma during pregnancy: report of one case with immunohistochemical studies. J Obstetr Gynaecol 2002; 22:683–685. [DOI] [PubMed] [Google Scholar]
- 19.Larsson G. Multiple leiomyomata of the urinary bladder in a hysterectomized woman. Acta Obstetricia Gynecologica Scandinavica 1994; 73:78–80. [DOI] [PubMed] [Google Scholar]
- 20.Matsuo H, Kurachi O, Shimomura Y, et al. Molecular bases for the actions of ovarian sex steroids in the regulation of proliferation and apoptosis of human uterine leiomyoma. Oncology 1999; 57 suppl 2:49–58. [DOI] [PubMed] [Google Scholar]
- 21.Huang HY, Chen WJ, Sung MT, et al. Atypical leiomyoma of the urinary bladder—a rare tumor occurring in a young female with concurrent breast carcinoma—an influence of sex steroid hormone? Scand J Urol Nephrol 2002; 36:231–233. [DOI] [PubMed] [Google Scholar]
- 22.Nunez Mora C, Julve Villalta E, Hardisson Hernaez D, et al. Bladder leiomyoma during pregnancy. Archivos Espanoles Urologia 1999; 52:510–513. [PubMed] [Google Scholar]
- 23.Park JW, Jeong BC, Seo SI, et al. Leiomyoma of the urinary bladder: a series of nine cases and review of the literature. Urology 2010; 76:1425–1429. [DOI] [PubMed] [Google Scholar]
- 24.Kalathia J, Agrawal S, Chipde SS, et al. Total endoscopic management of a large bladder leiomyoma. Urol Ann 2015; 7:527–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Knoll LD, Segura JW, Scheithauer BW. Leiomyoma of the bladder. J Urol 1986; 136:906–908. [DOI] [PubMed] [Google Scholar]


