Abstract
Background:
Association between cataract and the risk of ischemic heart disease (IHD) development is not completely clear.
Purpose:
The primary aim of the study was to evaluate the association between cataract and the risk of incident IHD. The secondary aim was to investigate the subsequent IHD risk of patients with cataracts undergoing cataract surgery.
Methods:
Retrospective data from the Longitudinal Health Insurance Database 2000 (LHID2000) was analyzed. Study participants were composed of patients with cataracts (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM] code 366) (n = 32,456), and a comparison cohort without the cataracts (n = 32,456) from 2000 to 2010. Cox proportional hazards regression was used to address the hazard ratio (HR) of IHD associated with cataract.
Results:
Within 12 years of follow up, the overall incidence rates of IHD were 24.2 per 1000 person-years in the cataract cohort and 18.2 per 1000 person-years in the noncataract cohort with an adjusted hazard ratio (aHR) of 1.35 (95% CI = 1.29–1.41; P < 0.001). Furthermore, the cataract patients undergoing cataract surgery were associated with a higher risk of IHD compared with those cataract patients without surgery (aHR = 1.07, 95% CI: 1.01–1.14; P < 0.05).
Conclusions:
Our finding suggested that patients with cataracts are at an increased risk of subsequent IHD development.
Keywords: cataract, cataract surgery, cohort study, incidence, ischemic heart disease
1. Introduction
Ischemic heart disease (IHD) is one of the major causes of mortality in the developed countries; inflammation and oxidative injury are the major players in atherosclerosis.[1–4] Cataract is a common cause of visual impairment in the elderly population; reduced antioxidant and oxidative stress are associated with the pathogenesis of senile cataract.[5–12]
Previous studies have demonstrated the positive correlation between cataract and the risk of IHD separately in specified population.[11,13–16] However, population-based studies addressing the association between cataract and the subsequent IHD risk were limited in the literature.[11,13,16] Furthermore, the effect of cataract surgery on the risk of IHD among patients with cataracts was not well defined.[11,13,16] Therefore, the purpose of the study was to evaluate the association between cataract and the risk of incident IHD. Moreover, the subsequent IHD risk of patients with cataracts undergoing cataract surgery was also investigated.
2. Methods
2.1. Data source
This present study was designed as a population-based retrospective cohort study to focus on the risk of IHD between patients with and without cataracts. The National Health Insurance (NHI) program, a single-payer national insurance system, covers more than 99% of the 23.74 million citizens in Taiwan.[17] In this study, the claim data of the Longitudinal Health Insurance Database 2000 (LHID2000) consisted of claims data by randomly selecting 1,000,000 enrollees from insured people for the period of 1996–2011. LHID2000 was established, maintained, and released by the National Health Research Institutes (NHRI). Data files were linked with the identifications of patients that had been anonymized to protect the privacy of the beneficiaries. The diagnostic codes provided in the LHID2000 for each outpatient visit or hospitalization contained up to 5 coded diagnoses according to the International Classification of Diseases, 9th Revision Clinical Modification (ICD-9-CM) classification. The Institutional Review Board of China Medical University and Hospital in Taiwan approved this study (CMUH-104-REC2-115).
2.2. Study population
We identified patients with newly diagnosed cataracts (ICD-9-CM code 366) from 2000 to 2010 as the cataract cohort. The index date for the patient was the date of the first medical visit for cataract. We excluded patients who were diagnosed with IHD (ICD-9-CM codes 410–414) before the index date, and missing information on demographics. The noncataract cohort was selected from the population without a history of cataract documented in the LHID2000. Patients in the cataract and noncataract cohorts were 1:1 matching based upon a propensity score.[18] Using a logistic regression, the propensity score was calculated to measure the probability of the disease status, based upon the baseline variables including year of the index date, age, gender, and comorbidities of hypertension (ICD-9-CM codes 401–405), diabetes mellitus (ICD-9-CM code 250), hyperlipidemia (ICD-9-CM code 272), stroke (ICD-9-CM codes 430–438), asthma (ICD-9-CM code 493), chronic obstructive pulmonary disease (ICD-9-CM codes 491, 492, 496), chronic renal disease (ICD-9-CM code 585), chronic liver disease (ICD-9-CM code 571), dementia (ICD-9-CM codes 290, 294.1, 331.0), neoplasm (ICD-9-CM codes 140–239), atrial fibrillation (ICD-9-CM code 427), and heart failure (ICD-9-CM code 428). The study outcome was a diagnosis of IHD during the 12-year follow-up. The study patients were followed up from the index date until the date of IHD diagnosis, withdrawal from the NHI program, or the end of 2011 (December 31, 2011).
2.3. Statistical analysis
The distributions of the categorical demographic characteristics and comorbidities were compared between the cataract cohort and the noncataract cohort. The standardized difference was used to quantify the differences in means or prevalence between the cataract and the noncataract cohorts for continuous and categorical matching variables. A value of standardized mean difference equaled 0.05 or less; indicative of a negligible difference in means between the cataract and the noncataract cohorts.[19] To estimate the cumulative incidence of IHD in the cataract and the noncataract cohorts, we performed the Kaplan–Meier method, with significance based on the log-rank test. The incidence densities of IHD were estimated by dividing the number of IHD by the number of person-years stratified by sex, age, and comorbidity. Univariable and multivariable Cox proportion hazard regression models were employed to examine the effect of cataract on the risk of IHD, expressed as hazard ratios (HRs) with 95% confidence intervals (CIs). The multivariable Cox models were adjusted for age, sex, and comorbidities of hypertension, diabetes mellitus, hyperlipidemia, stroke, asthma, chronic obstructive pulmonary disease, chronic renal disease, chronic liver disease, dementia, neoplasm, atrial fibrillation, and heart failure. All data analyses were performed using the SAS statistical package (version 9.4 for Windows; SAS Institute, Cary, NC). A 2-tailed P-value of <0.05 indicated the statistical significance level.
3. Results
Basic characteristics of the cataract patients and their matched noncataract patients are shown in Table 1. The mean ages of the cataract and the noncataract cohorts were 62.3 (±9.97) and 62.1 years (±10.9), respectively. The distribution of age, sex, and comorbidity showed similar after propensity score matching. In these 2 cohorts, most people were women (53.9% vs 53.1 %). The major comorbidity was hypertension (40.9% vs 43.2%) in these 2 cohorts. During the mean follow-up period of 5.94 years for the cataract cohort and 5.41 years for the noncataract cohort, the Kaplan–Meier analysis for the cumulative incidence of IHD in the cataract and noncataract cohort demonstrated that the risk of IHD was significantly higher in the cataract cohort than in the noncataract cohort by the end of the 12-year follow up (Fig. 1, log rank test, P < 0.001).
Table 1.
Demographic characteristics and comorbidities in patients with and without cataracts.
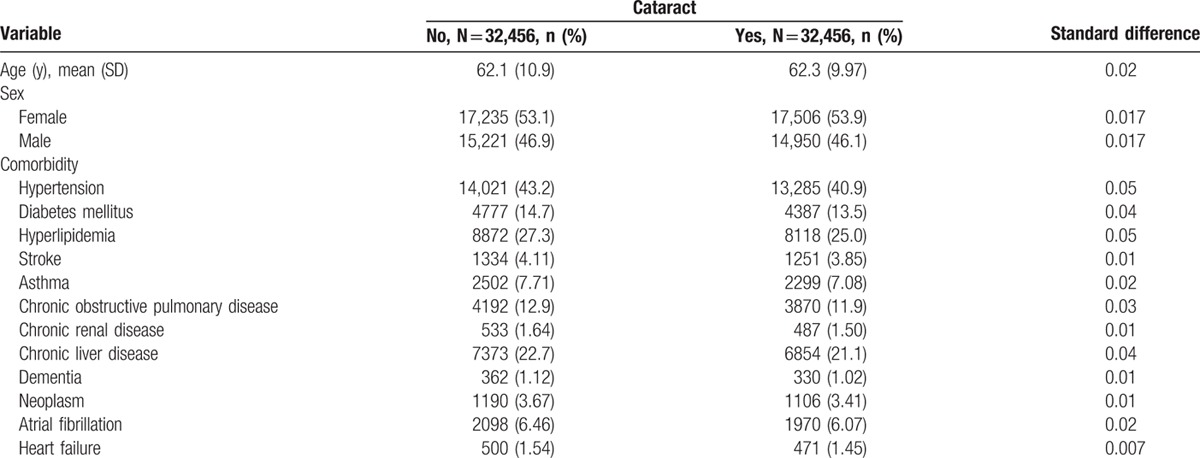
Figure 1.
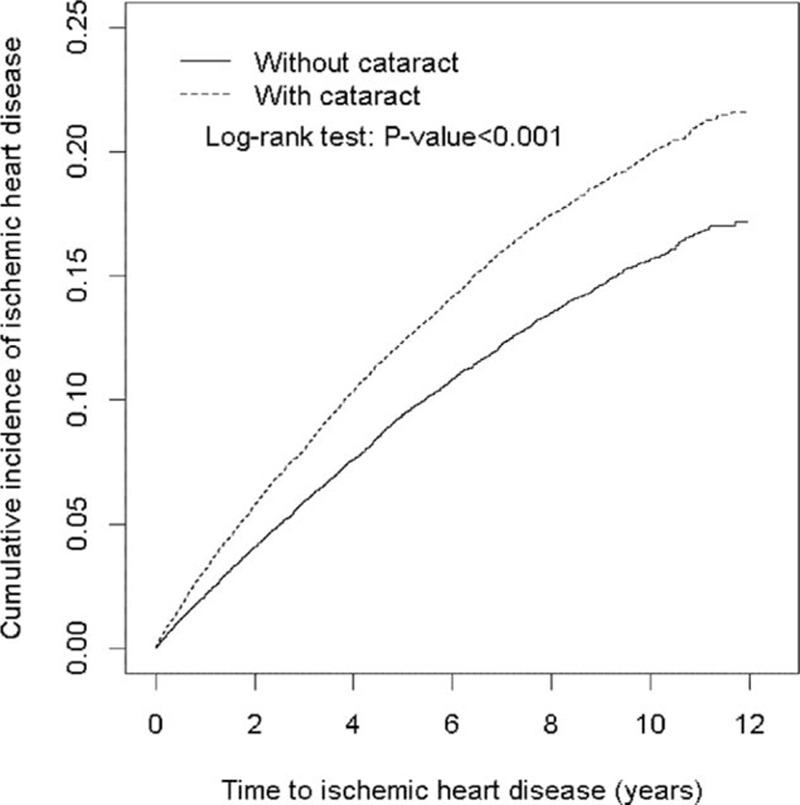
Cumulative incidence curves of ischemic heart disease (IHD) for groups with and without cataracts.
The incidence density rate and HR of IHD stratified by sex, age, and comorbidity between patients with and without cataracts are shown in Table 2. Within 12 years of follow up, the overall incidence rates of IHD were 24.2 per 1000 person-years in the cataract cohort and 18.2 per 1000 person-years in the noncataract cohort with an adjusted hazard ratio (aHR) of 1.35 (95% CI = 1.29–1.41). With the relative risk of 1.33, the estimated population attributable risk (PAR) of IHD associated with cataract patients was 1.04 per 100 or 0.01% for the population. Of 100 cases of IHD, only 1–2 would be prevented if cataract completely disappeared from the general population. The incidence density of IHD was higher in men than in women in both cohorts. The aHR of IHD was significantly higher in the cataract cohort than in the noncataract cohort for both men (aHR = 1.34, 95% CI = 1.26–1.43) and women (aHR = 1.36, 95% CI = 1.28–1.45). The incidence of IHD increased with age in both cohorts.
Table 2.
Comparison of incidence and hazard ratio of ischemic heart disease stratified by sex, age, and comorbidity between patients with and without cataracts.
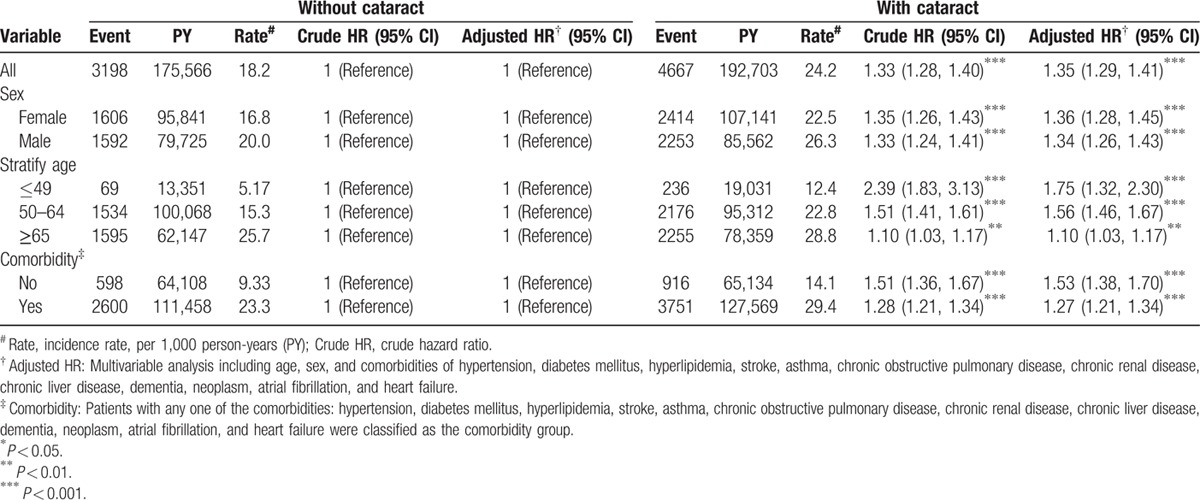
The age-specific cataract to noncataract cohorts aHR of IHD were significant higher for all age group (aHR = 1.75, 95% CI = 1.32–2.30 for aged ≤49 years; aHR = 1.56, 95% CI = 1.46–1.67 for aged 50–64 years; aHR = 1.10, 95% CI = 1.03–1.17 for aged ≥65 years). Furthermore, patients with comorbidities had an increased IHD incidence in both cohorts. However, the comorbidity-specific cataract to noncataract cohort relative risk of IHD was significant for patients without comorbidities (aHR = 1.53, 95% CI = 1.38–1.70) and for patients with comorbidities (aHR = 1.27, 95% CI = 1.21–1.34).
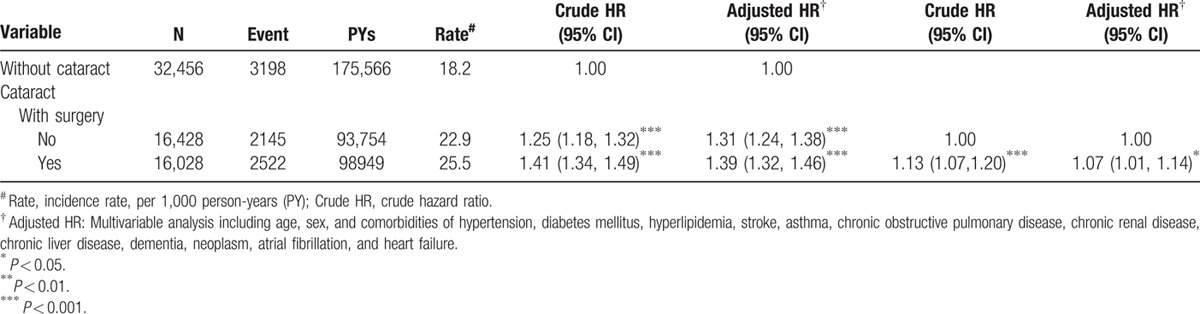
To investigate the subsequent IHD risk of patients with cataracts undergoing cataract surgery, we conducted a subgroup analysis. A total of 32,456 cataract patients were included; of them, 16028 patients received cataract surgery, and the remaining 16,428 patients did not receive cataract surgery. The incidence rates of IHD were 18.2 per 1000 person-years in the patients without cataracts, 22.9 per 1000 person-years in the cataract patients without surgery, and 25.5 per 1000 person-years in the cataract patients undergoing cataract surgery. The relative risk of IHD for the cataract patients undergoing cataract surgery to those without cataracts showed significant differences, with an aHR of 1.39 (95% CI = 1.32–1.46). In addition, the relative risk of IHD for the patients with cataracts without surgery to those without cataracts also showed significant differences, with an adjusted HR of 1.31 (95% CI = 1.24–1.38). Furthermore, the cataract patients undergoing cataract surgery were associated with a higher risk of IHD compared with those cataract patients without surgery (aHR = 1.07, 95% CI: 1.01–1.14), as shown in Table 3.
Table 3.
Incidence and hazard ratio of ischemic heart disease among cataract patients with and without surgery compared to patients without cataracts.
4. Discussion
In this nationwide population-based retrospective cohort study, our results showed that cataract patients are at an increased risk of incident IHD in the future, particularly in the younger population. Furthermore, the cataract patients undergoing cataract surgery were associated with a higher risk of IHD compared with those cataract patients without surgery.
The strength of our research is that it is a population-based observational study and there are adequate patients to minimize the confounding factors.[17] Propensity score analysis was used to minimize the observable selection bias with the attempt to simulate the randomization process.[18]
Although cataract is a localized ocular disease, increasing studies support the link between cataract and atherosclerosis.[11,13–16] A variety of mechanisms was involved, including inflammation, accumulation of advanced glycation end products, and oxidative injury.[3–12,20–22] Our finding is consistent with the previous investigations[11,13–16]; furthermore, to our best knowledge, this is the first population-based study to demonstrate the inverse relationship between IHD risk and the advancement of age among patients with cataracts. We believed that less traditional IHD risk factors in the younger subjects, in comparison to those with advanced age, leading to this inverse relationship. This finding is important for cataract patients; additional investigations are necessary to confirm our result and to explore the mechanism involved.
In our study, a subgroup analysis was conducted to further evaluate the subsequent IHD risk of patients with cataracts undergoing cataract surgery. Our findings showed that patients with cataracts undergoing cataract surgery were not associated with a reduced risk of IHD in comparison to those cataract patients without surgery. The possible explanation for our finding is that atherosclerotic process is a continuum, and it cannot be modified by the localized cataract surgery but the IHD risk factors[1–4,11,13–16]; indicating that cataract might be considered as the marker of IHD instead of a direct causative effect.
5. Limitations
First, diagnoses of cataract, IHD, and comorbidity were completely dependent on ICD codes. Therefore, the accuracy of the claims data might influence the results significantly. However, a mechanism to verify the diagnosis has been made by Taiwan's NHI. Second, several IHD risk factors, such as family history of premature IHD, smoking, body mass index, physical inactivity and emotional stress could not be obtained from the LHID2000. However, propensity score matching analysis was used to ensure the validity of the results by reducing selection bias.[18] Third, the severity of cataract cannot be clearly identified due to the limitation of the LHID2000. Fourth, the study was analyzed from Taiwanese database; therefore the result might be inappropriate to apply for other populations. Finally, the mortality data were not available in our dataset. Therefore, we were unable to conduct the analysis to see whether there is higher mortality in the cataract cohort.
6. Conclusions
In conclusion, our finding suggested that patients with cataracts are at an increased risk of subsequent IHD development, particularly in the younger population.
Footnotes
Abbreviations: CI = confidence interval, HR = hazard ratio, ICD-9-CM = International Classification of Diseases, 9th Revision, Clinical Modification, IHD = ischemic heart disease, NHI = National Health Insurance.
Funding: This study is supported in part by Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW105-TDU-B-212-133019), the Ministry of Science and Technology (MOST 103-2314-B-039-029, MOST 104-2314-B-039-048), China Medical University Hospital (DMR-100-005, DMR-103-003, DMR-104-006, DMR-105-013), Academia Sinica Taiwan Biobank Stroke Biosignature Project (BM10501010037), NRPB Stroke Clinical Trial Consortium (MOST 104-2325-B-039-005), Tseng-Lien Lin Foundation, Taichung, Taiwan, Taiwan Brain Disease Foundation, Taipei, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan.
The authors have no conflicts of interest to disclose.
References
- 1.Bonow RO, Smaha LA, Smith SC, Jr, et al. World Heart Day 2002: the international burden of cardiovascular disease: responding to the emerging global epidemic. Circulation 2002; 106:1602–1605. [DOI] [PubMed] [Google Scholar]
- 2.Libby P. Inflammation in atherosclerosis. Nature 2002; 420:868–874. [DOI] [PubMed] [Google Scholar]
- 3.Hiller R, Sperduto RD, Reed GF, et al. Serum lipids and age-related lens opacities: a longitudinal investigation: the Framingham studies. Ophthalmology 2003; 110:578–583. [DOI] [PubMed] [Google Scholar]
- 4.Maxwell SRJ, Lip GYH. Free radicals and antioxidants in cardiovascular disease. Br J Clin Pharmacol 1997; 44:307–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christen WG, Glynn RJ, Chew EY, et al. Folic acid, vitamin B, and vitamin B in combination and age-related cataract in a randomized trial of women. Ophthalmic Epidemiol 2016; 23:32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mares J. Food antioxidants to prevent cataract. JAMA 2015; 313:1048–1049. [DOI] [PubMed] [Google Scholar]
- 7.Kruk J, Kubasik-Kladna K, Aboul-Enein HY. The role oxidative stress in the pathogenesis of eye diseases: current status and a dual role of physical activity. Mini Rev Med Chem 2015; 16:241–257. [DOI] [PubMed] [Google Scholar]
- 8.Awodele O, Oreagba IA, Olayemi SO, et al. Evaluation and comparison of the indices of systemic oxidative stress among Black-Africans with age-related cataracts or primary glaucoma. Middle East Afr J Ophthalmol 2015; 22:489–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rautiainen S, Lindblad BE, Morgenstern R, et al. Total antioxidant capacity of the diet and risk of age-related cataract: a population-based prospective cohort of women. JAMA Ophthalmol 2014; 132:247–252. [DOI] [PubMed] [Google Scholar]
- 10.Abraham AG, Condon NG, West Gower E. The new epidemiology of cataract. Ophthalmol Clin North Am 2006; 19:415–425. [DOI] [PubMed] [Google Scholar]
- 11.Hu FB, Hankinson SE, Stampfer MJ, et al. Prospective study of cataract extraction and risk of coronary heart disease in women. Am J Epidemiol 2001; 153:875–881. [DOI] [PubMed] [Google Scholar]
- 12.Trevithick JR, Mitton KP. Vitamin C and E in cataract risk reduction. Int Ophthalmol Clin 2000; 40:59–69. [DOI] [PubMed] [Google Scholar]
- 13.Nemet AY, Vinker S, Levartovsky S, et al. Is cataract associated with cardiovascular morbidity? Eye (Lond) 2010; 24:1352–1358. [DOI] [PubMed] [Google Scholar]
- 14.Lindblad BE, Håkansson N, Philipson B, et al. Metabolic syndrome components in relation to risk of cataract extraction: a Prospective Cohort Study of Women. Ophthalmology 2008; 115:1687–1692. [DOI] [PubMed] [Google Scholar]
- 15.Goodrich ME, Cumming RG, Mitchell P, et al. Plasma fibrinogen and other cardiovascular disease risk factors and cataract. Ophthalmic Epidemiol 1999; 6:279–290. [DOI] [PubMed] [Google Scholar]
- 16.Podgor MJ, Kannel WB, Cassel GH, et al. Lens changes and the incidence of cardiovascular events among persons with diabetes. Am Heart J 1989; 117:642–648. [DOI] [PubMed] [Google Scholar]
- 17.Database NHIR. Taiwan, http://nhird.nhri.org.tw/en/index.html (cited in 2015). [Last cited on 2016 June 23]. [Google Scholar]
- 18.Parsons LS (2004) Performing a 1:N Case-Control Match on Propensity Score. Proceedings of the 29th SAS Users Group International Conference. Montréal, Canada. [Google Scholar]
- 19.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 2009; 28:3083–3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pradhan AD, Manson JE, Buring JE, et al. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA 2001; 286:327–334. [DOI] [PubMed] [Google Scholar]
- 21.Klein BE, Klein R, Lee KE. Diabetes, cardiovascular disease, selected cardiovascular disease risk factors, and the 5-year incidence of age-related cataract and progression of lens opacities: the Beaver Dam Eye study. Am J Ophthalmol 1998; 126:782–790. [DOI] [PubMed] [Google Scholar]
- 22.Thompson JR, Sparrow JM, Gibson JM, et al. Cataract and survival in an elderly nondiabetic population. Arch Ophthalmol 1993; 111:675–679. [DOI] [PubMed] [Google Scholar]


