Abstract
Introduction:
We investigated the effect of postural changes on various cardiovascular parameters across gender. Twenty-eight healthy subjects (16 male, 12 female) were observed at rest (supine) and subjected to 3 interventions; head-down tilt (HDT), HDT with lower body negative pressure (HDT+ LBNP at −30 mm Hg), and head-up tilt (HUT), each for 10 minutes separated by a 10 minutes recovery period.
Methods:
Measurements were recorded for heart rate (HR), standard deviation of the normal-to-normal intervals, root mean square of successive differences between the normal-to-normal intervals, heart rate variability-low frequency (LFRRI), heart rate variability-high frequency (HFRRI), low frequency/high frequency ratio (LFRRI/HFRRI), systolic blood pressure (SBP), mean arterial pressure (MAP), diastolic blood pressure (DBP), total peripheral resistance index (TPRI), stroke index (SI), cardiac index (CI), index of contractility (IC), left ventricular work index, and left ventricular ejection time.
Results:
Across all cardiovascular parameters, there was a significant main effect of the intervention applied but there was no significant main effect of gender across all parameters.
Conclusions:
The results suggest that there are no specific gender differences in regards to the measured variables under the conditions of this study. Furthermore, these results suggest that in healthy subjects, there appears to be evidence that LBNP partially elicits similar cardiovascular responses to HUT, which supports the use of LBNP as an intervention to counteract the effects of central hypovolemia.
Keywords: gender, head-down tilt, head-up tilt, lower body negative pressure, orthostasis, syncope
1. Introduction
1.1. Orthostatic intolerance due to fluid shifts
The transition from supine to standing causes a drop in arterial blood pressure. A fall in systolic blood pressure (SBP) of at least 20 mm Hg, or 10 mm Hg in diastolic blood pressure (DBP), within 3 minutes of standing is defined as orthostatic hypotension.[1] This occurs as 500 to 1000 mL of blood shifts from the upper to lower body,[2] as a consequence of gravitational forces. Consequently, there is a reduction in venous return leading to reductions in stroke volume, arterial blood pressure, and eventually cerebral blood flow. This leads to compensatory effects activating the sympathetic nervous system, the renin-angiotensin system, and subsequent aldosterone release.
When an individual is lying down, blood volume is distributed based on physiological demand.[2] After 1 minute of standing, gravity induces roughly 500 mL of blood to shift to the lower body. After 20 to 30 minutes there is substantial loss of plasma volume from blood to the tissues. In healthy individuals, there is a 14% drop in plasma volume after 20 minutes in the upright position, the majority of the drop occurring within the initial 10 minutes. As arterial pressure decreases the baroreceptors become unloaded initiating parasympathetic withdrawal and activation of the sympathetic nervous system via baroreflex-mediated autonomic regulation. The withdrawal of parasympathetic action rapidly increases heart rate (HR), within 1 to 2 cardiac cycles. The sympathetic activation, however, yields a slower response, within 6 to 8 cardiac cycles, causing vascular resistance, vascular tone, and cardiac contractility to increase and further increase HR.[3–5] Meanwhile, cerebral autoregulation occurs, initiated by changes in carbon dioxide, myogenic tone and metabolic demand, causing vasodilation of cerebral arterioles.[6–9]
1.2. Gender differences in cardiovascular regulation
It has been shown in a number of studies that females have greater orthostatic hypotension than males upon standing up[10–12] and have greater incidence of orthostatic intolerance than males.[13–15] Briefly, following aspects have been reported:
gender affects sympathetic response to postural changes.[16] Furthermore, gender specific interindividual relationships between vascular resistance, cardiac output, and sympathetic activity in the maintenance of arterial pressure has been reported. Fu et al[17] demonstrated in healthy young males, arterial pressure was maintained by a balance between cardiac output and sympathetic nerve activity, whereas, young females had reduced autonomic support to maintain blood pressure. While Fritsch-Yelle et al[18] stated that females showed a greater tendency to postflight orthostatic hypotension and presyncope than males. This is likely to be due to the differences, which appear between genders while under physiological stress. Furthermore and in contrast to males, it has been shown, muscle sympathetic nerve activity (MSNA) in females is not related to total peripheral resistance (TPR).
It has been postulated that gender differences in maintaining arterial pressure could be due to hormone action on β-adrenergic receptors offsetting α-adrenergic vasoconstriction differentially in young women.[19] It is thought that these differences, in part, give rise to reduced orthostatic tolerance in young women compared to their male counterparts, while also experiencing a greater increase in HR during cardiovascular stress.[20]
Harm et al[20] noted that females were less able to tolerate the upright posture, down to the reduced ability to maintain venous return and cardiac output.
1.3. Aims and objectives
Significant decreases in arterial blood pressure, due to postural change, can be described as orthostatic hypotension. Based on the published literature[10–20] predisposition of an individual to postural hypotension is likely to be influenced by gender. This study was, therefore, designed to examine the effects of fluid shifts following various postural changes and lower body negative pressure (LBNP) application (i.e., head-down tilt [HDT], HDT + LBNP, and head-up tilt [HUT] effects on cardiovascular responses were tested in a single protocol) across gender. It is hypothesized that: cardiovascular parameters such as blood pressure and HR will be affected with the changes in fluid shifts induced by posture and by additional application of LBNP; greater differences in the hemodynamic responses occur during HUT than HDT; the addition of LBNP during HDT will bring about similar cardiovascular changes those that occur during upright position[21,22]; and the cardiovascular stress responses to the orthostatic challenges of the experiment will differ across gender. Assessing how posture affects cardiovascular responses may prove useful in discerning any gender variance in control of blood pressure, and in particular to susceptibility of an individual (especially females) to orthostatic intolerance.
2. Methodology
2.1. Subjects
To avoid the effect of confounding variables such as age, height, or fitness, a total of 28 healthy (16 males: 12 females) subjects were selected of similar age, height, and fitness. The exclusion criteria for the study included: history of vasovagal syncope, vertigo, and vestibular disturbance and excluding cardiovascular, respiratory, and neurological diseases.
Subjects were instructed to not engage in any exercise or stressful activity 48 hours before testing, while also being told to abstain from consuming caffeine and other alternative stimulants 24 hours before testing. To account for random and circadian rhythm effects on the cardiovascular system, 1 subject per day was tested at the same time (0900–1100) within a quiet darkened laboratory.
Subjects gave their written informed consent to participate in the study, which received approval from the Ethics Committee of the Medical University of Graz. Previous to giving consent, all potential subjects were familiarized with the test protocol and informed of their right to withdraw at any time. Additionally, individuals received a full comprehensive medical examination.
2.2. Sample size calculations
Using means and standard deviations of cardiovascular responses during orthostatic loading from previous studies,[23–25] error probability (α) of 0.05 and power (1 − β) of 0.80, and using these values in an online power and sample size calculator, total number of males and females subjects required was 22.
2.3. Protocol
Each experiment started with a 10-minute supine rest period to obtain cardiovascular baseline measurements. After 10-minutes, the electronically controlled tilt table was brought to 6° head-down (HDT) position. After 10-minutes the tilt table was reverted back to the supine position. The tilt table was then put back into the 6° HDT with the addition of 30 mm Hg LBNP for a further 10-minutes before returning back to the supine position for 10-minutes. The tilt table was then brought to 70° head-up (HUT) position for a further 10-minutes before returning to 0° for a 3-minute recovery to ensure the body had returned to cardiovascular baseline measurements. A schematic diagram of the protocol is provided below (Fig. 1).
Figure 1.
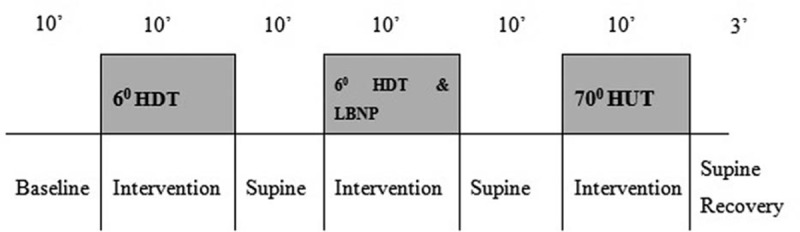
A schematic diagram of the protocol used.
During the protocol the development of presyncopal symptoms were monitored. If any subject developed presyncope the experiment was terminated immediately. Presyncope was defined as[26,27]: blood pressure dropping below 80 mm Hg or by ≥20 mm Hg/minute; diastolic by ≥10 mm Hg/minute; and/or HR decreasing by ≥15 bpm. Additionally subjects were instructed to avoid any unnecessary movements, remain as still as possible and breathe normally at all times.
2.4. Hemodynamic and autonomic nervous system monitoring
To monitor blood pressure the Peñáz principle was used.[28] Total peripheral resistance was calculated using the following formula: mean arterial pressure (MAP)/cardiac index (CI). MAP was calculated using the following formula: DBP + 1/3 (SBP–DBP). The measurement of CI refers to the performance of the heart, which is normalized to the subject's body surface area; this was calculated using the following formula: cardiac output/body surface area. The measurement of stroke index (SI) refers to stroke volume normalized to the subject's body surface area; this was calculated using the following formula: stroke volume/body surface area. Impedance cardiography, shows changes in thoracic impedance converted to reflect changes in thoracic fluid/volume over time, was carried out utilizing the original Kubicek et al[29] approach however using an improved estimate (Task Force Monitor, TFM). For details of the hemodynamic parameters and how they were estimated see Grasser et al[30] and Lackner et al.[31]
The electrodes for electrocardiogram (ECG)/impedance were placed along with upper arm and subjects also wore a finger blood pressure cuff.[32] ECG and impedance electrodes were positioned on the neck and mid-clavicular line at the xiphoid process level in the thoracic region.[32]
2.5. Data collection and data analysis
Control (supine) data were taken before the HDT and in between the various analogues to allow for reequilibration of gravity-related fluid shifts and stabilization of the hemodynamic/hormonal parameters. Additionally a recovery period was utilized to ensure subject's return to baseline levels.
Throughout the protocol, data were reported and calculated beat-to-beat. Power spectrum analysis of HR variability assesses sympathovagal balance. Low (LF: 0.04–0.15 Hz) and high frequency (HF: 0.15–0.40 Hz) power components of RR-intervals (RRI), DBP, and SBP were evaluated. Baroreceptor sensitivity was calculated from continuous monitoring of HR and SBP. An increase/decrease of beat-to-beat RRI and SBP in the same direction for at least 3 cardiac cycles was used to calculate steepness of the regression line.
The myocardial contractility parameters were attained through impedance cardiography measurement.[30] The index of contractility (IC) reflects aortic peak flow and the maximum impedance changes (ΔZ/Δtmax) normalized to the ground impedance Z0. The left ventricular work index was calculated as (MAP − pulmonary capillary occlusion pressure; fixed to 7 mm Hg ∗ cardiac index ∗ const.
2.6. Statistical analyses
Data were analyzed by PASW Statistics 20 Software package (SPSS, IBM Corp., NY) using a general linear model (GLM). With the within-subjects factor phase (Rest, HDT, Supine, HDT + LBNP, Supine, HUT, post-HUT) and the between subjects factor sex. This allowed the observation of the effect of different conditions (main effect phase) and, importantly, different time courses between gender (interaction phase x gender; hypothesis iv) as well. To correct violations of sphericity, the degrees of freedom were corrected using Greenhouse–Geisser (ε < 0.75).[31] The results are presented as the mean ± standard deviation (SD). The alpha level of significance was set at 5% (P < 0.05).
3. Results
3.1. Subject characteristics
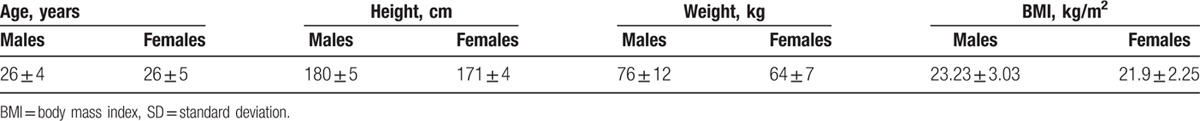
The study was completed by 16 healthy males and 12 healthy females. The subject characteristics are displayed below, Table 1 (mean ± SD).
Table 1.
Subject characteristics (mean ± SD).
Across the 15 parameters observed there was a significant effect of tilt-phase measured across all phases (P < 0.001) (Tables 2–5).
Table 2.
Mean (±SD) values for heart rate, SDDN, RMSSD, heart rate variability-low frequency, heart rate variability-high frequency and low frequency/high frequency ratio, with F-statistics for phase and gender.
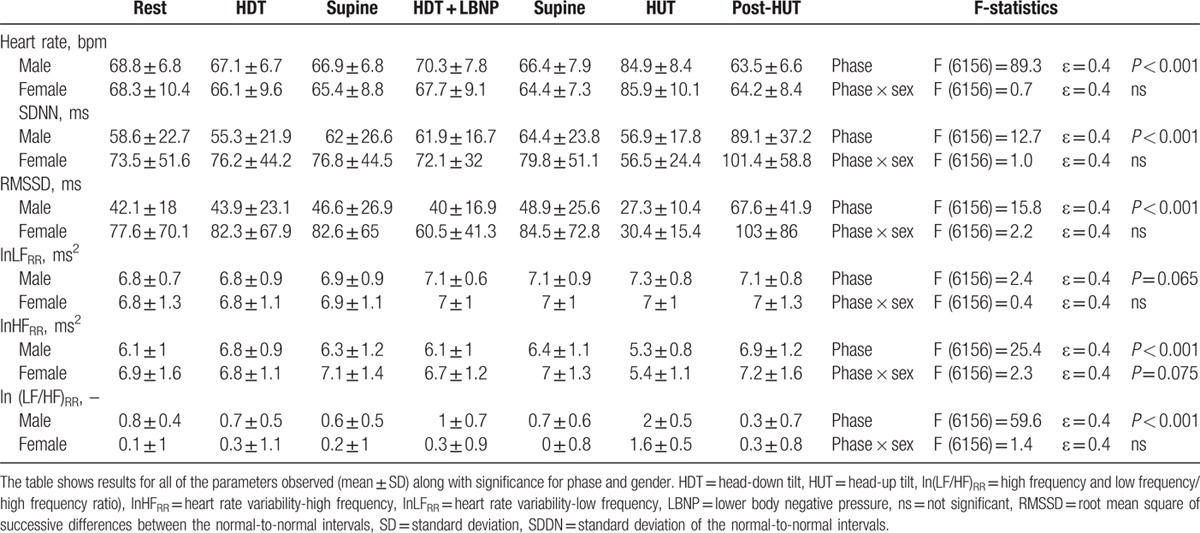
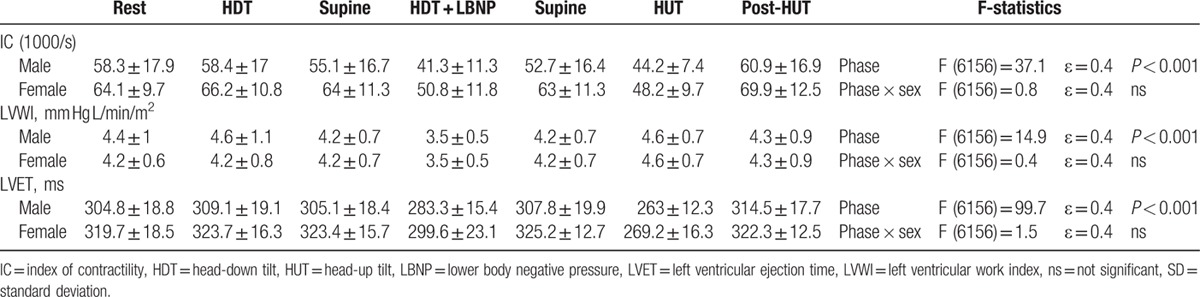
Table 5.
Mean (±SD) values for index of contractility, left ventricular work index, and left ventricular ejection time, with F-statistics for phase and gender.
HR and HR variability data are presented in Table 2. Between gender, HR changes range from 63.5 ± 6.6 to 64.2 ± 8.4 bpm in males versus females resulting in a range of 21.4 versus 21.7 bpm, respectively. As a result no significant gender difference was observed. Furthermore, it is interesting to note HR variability results showed no gender difference, although SDNN changes during supine versus HUT are shown to be greater in females versus males; 79.8 ± 51.1 to 56.5 ± 24.4 ms versus 64.4 ± 23.8 to 56.9 ± 17.8 ms.
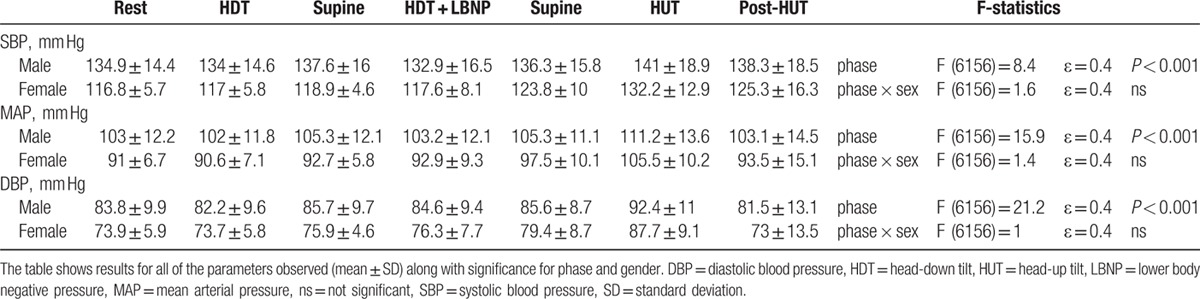
Blood pressure associated parameters are presented in Table 3. A greater range of MAP was observed in females versus males; 90.6 ± 7.1 to 105.5 ± 10.2 mm Hg versus 102 ± 11.8 to 111.2 ± 13.6 mm Hg. However, no statistical differences between gender was observed.
Table 3.
Mean (±SD) values for systolic blood pressure, mean arterial pressure, and diastolic blood pressure, with F-statistics for phase and gender.
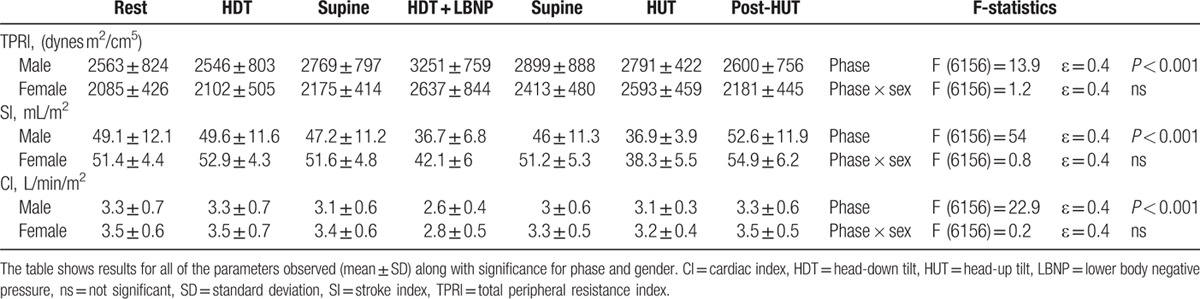
Alternate hemodynamic parameters are presented in Table 4. Both stroke volume and cardiac output, when normalized to body surface area (SI and CI), appear to be greater in females versus males; (SI: 51.4 ± 4.4 vs 49.1 ± 12.1; and CI: 3.5 ± 0.6 vs 3.3 ± 0.7). Similar changes were observed throughout the change of phase resulting in no significant difference across gender.
Table 4.
Mean (±SD) values for total peripheral resistance index, stroke index and cardiac index, with F-statistics for phase and gender.
Last, data from left ventricular ejection time, presented in Table 5 shows HDT + LBNP partially elicits HUT like effects, results from HDT versus HDT + LBNP versus HUT across both males (309.1 ± 19.1 vs 283.3 ± 15.4 vs 263 ± 12.3 ms) and females (323.7 ± 16.3 vs 299.6 ± 23.1 vs 269.2 ± 16.3 ms) show similar trends. Although greater values are observed in females, no significance was observed across gender.
In addition no significant gender difference were seen for HR (P = 0.76), SDNN (P = 0.29), root mean square of successive differences between the normal-to-normal intervals (P = 0.07), LFRR (P = 0.68), HFRR (P = 0.27), SI (P = 0.23), CI (P = 0.25), IC (P = 0.1), and left ventricular work index (P = 0.59). However, significant difference was seen for LFHFrr (P = 0.005), SBP (P = 0.004), MAP (P = 0.02), DBP (P = 0.02), total peripheral resistance index (TPRI) (P = 0.05), and left ventricular ejection time (P = 0.02).
4. Discussion
In the present study, we observed cardiovascular parameters across a number of interventions, which induce various fluid shifts (e.g., HDT, HDT + LBNP, and HUT). All of the cardiovascular parameters tested were significantly altered dependent on the intervention applied. Our data also suggest that there are no differences across gender with regards to blood pressure regulation, myocardial contractility, and sympathetic nerve activity.
4.1. Gender differences in cardiovascular regulation
Within the literature there appears to be conflicting findings as to whether there are differences in sympathetic reflex responses across gender. The majority,[33,34] however not without debate,[35] of the studies appear to conclude that females show a lower cardiovascular response to a range of stressors than their male counterparts. Within this study, it was observed that there was no difference between males and females across the various cardiovascular parameters, within the range of tilt table phases utilized. In spite of numerous studies showing a greater occurrence of orthostatic intolerance in females,[10,39,40,48,49] and the role that the sympathetic nervous system plays in blood pressure regulation during change in posture,[36,37] there is very little knowledge of cardiovascular and sympathetic nerve activity in response to fluid shifts, secondary to postural changes between gender in young subjects. Our results show that there are no differences in changes in MAP across gender in young healthy persons.
Shoemaker et al,[16] however, reported different results. Their results suggested differences in MAP between men and women, with a lower muscle sympathetic nerve activity reported in females. Although there appears to be greater stimuli to increase sympathetic nerve activity in females, it does not appear to have a significant influence in activating the sympathetic pathways; therefore, no difference is noted in comparison to males. This appears to show that there could potentially be a difference between males and females in either the sensitivity of sensory afferent fibers or in central integration and alteration of reflex input signals. It has been reported that the sensory signals that contribute to the sympathetic response during postural changes associated with HUT are initiated in the cardiac chambers, aortic and carotid structures, and vestibular receptors.[16] Additionally, the results presented here are in agreement with the work of Ray[34] and colleagues who suggested that sex does not influence vestibule-sympathetic activation.
From the literature, evidence of regional baroreceptor function and its relationship to gender differences in cardiovascular regulation remains limited. The detection of alterations in venous return, which exert control over specific sympathetic nerve activity, takes place in afferent neurons residing in the cardiac chambers and pulmonary structures.[38] The volume of fluid, which appears to shift during postural changes, has been suggested to be lower in females than males,[10] which is shown across our results (reflected in the changes in the thoracic fluid content). However, there seems to be a larger shift in fluid from the thoracic region during HUT for females versus males. Therefore, the findings of the current study do not entirely agree with those of Shoemaker et al.[16]
It has also been suggested that due to a lower body mass and blood volume, the cardiac filling pressure is not different between males and females.[33] This appears to be the case in our study as well as there is a similar trend in SI and CI (the indexes normalize these values to the subject's body surface area). Our findings therefore lend support to the concept that the pressure of venous filling may not be a key factor in influencing gender-specific autonomic responses to fluid shifts.
During an increase in MAP, the aortic arch baroreceptors send powerful inhibitory signals to the sympathetic activity.[38] In our study, we did not observe any difference in the sensitivity of the above-mentioned receptors between males and females, in response to an increase in MAP, which would cause increased sympatho-inhibition. The rise in MAP during the HUT intervention was slightly higher in females than in males, thus a larger aortic baroreflex gain should have been observed. However, we observed no significant differences between males and females. In summary, the role of gender on baroreflex sensitivity and control remains vague.[49]
Similar to the absence of gender differences observed in MAP, females did not demonstrate a change in response of reflex HR alterations during postural changes. This observation is not in agreement with previous studies which explored HR responses to postural stress tests.[10,32] Additionally, analysis of HR dynamics in females induced by tilting[10] do not support the notion that females have an increase in vagal cardiac control at rest, and as a result larger withdrawal of parasympathetic activity during postural changes.[32] This is particularly interesting as most of the studies in which HR variability across gender was investigated have reported the LF/HF ratio to be significantly lower in females when compared to males.[36,39,40] This has been suggested to be due to the lower LF power in females. Some studies did not, however, see such gender differences in LF.[37] In addition, studies comparing time domain measures reported that the SDNN and RMSDD were lower in females. As a result of such consistent findings it has been generally accepted that lower LF and higher HF power in females represents a more pronounced parasympathetic cardiac regulation in females, while higher LF and lower HF power suggests a more dominant sympathetic influence in males.[41] However, in the present study, no differences were observed between males and females.
It was expected that a smaller sympathetic response during fluid shifts would be related to a smaller response in TPRI when comparing females to males. However, our results show no difference in TPRI response in females during HUT; this is not surprizing as the changes in CI and MAP showed no differences between genders. However, these results do not agree with Shoemaker et al,[16] who reported that MAP was increased in males compared to females. They also reported an apparent dissociation between sympathetic nerve activity and TPR, arising due to a number of other factors, which contribute to blood pressure regulation. The vasoconstrictor response depends not only on sympathetic nerve activity but also neurotransmitter levels, adrenergic receptor density, and postsynaptic mechanisms, which control calcium levels in vascular smooth muscle. Currently, the part each of these factors play toward contributing to gender differences is indistinct. For instance, there is conflicting evidence for and against – females showing a greater sensitivity in adrenergic receptors.[10,38] Furthermore, TPR appears to be influenced by nonsympathetic vasoconstriction factors such as local myogenic or veno-arteriolar constrictor response.[42–44] Finally, it is still unknown how regional vascular responses to sympathetic excitation differ between genders.
5. Limitations
During testing, females were not controlled to a specific phase of their menstrual cycle. It has been shown that particular phases of the menstrual cycle during exercise have an effect on the neural responses to sympathetic stimulation.[45,46] It has also been shown by Saeki et al,[50] using low frequency blood pressure oscillations, that sympathetic responses to postural changes are indeed affected by the menstrual phase. However, low-frequency power, as an indicator of sympathetic activation using direct comparisons of MSNA and frequency-specific spectral power characteristics of HR and blood pressure,[47] is still being debated. Therefore, this could have contributed to some uncertainty around the effects of menstrual phase on baroreflex sympathetic control.
Additionally, within the female group, none were identified as taking oral contraceptives, which adds another degree of uncertainty of the hormonal profile of the females. However, with the assumption that all of the females were at varying stages of their menstrual cycle, the current findings could be a representative finding of the generalized response of females to an important gender difference in the cardiovascular response to postural changes and fluid shifts. Furthermore, the small sample size could limit the generalizability of this study.
Finally, differences in our protocol and that used by other researchers could also have contributed to the differences in our findings.[47–50] Although our protocols were lasting for 10 minutes each, many of the other reported studies used longer periods of central hypovolemia.
6. Conclusions
The alteration of posture induces cardiovascular stressors on the body due to the shifting of fluid. In particular, the upright position causes the greatest translocation of blood from the thoracic region to the lower limbs. As a result, appropriate autonomic reflexes need to occur to affect peripheral vascular tone and HR, which reduce the effects of the change in posture on cardiac output and venous return. Our data show that there are no specific gender differences in regards to the regulation of the cardiovascular system, with no significant difference noted across all measured variables (although they react to a dissimilar extent).
Additionally, our results in healthy subjects show that LBNP partially elicits similar cardiovascular responses to HUT, which shows support to the use of LBNP as an intervention in microgravity. However, further studies need to be carried out at a number of varying levels of LBNP to find the most appropriate level of application.
Furthermore, given the importance of the everyday problem of fluid shifts it is important to note that, to our knowledge, there are no other studies currently showing evidence of the affects of fluid shifts (simulated by 10 minutes of HDT, HDT with lower body negative pressure at −30 mm Hg, and HUT) in the same subjects and across gender on the cardiovascular system. Our results certainly are novel in this regard, as they show that perturbations such as the ones used in our study, and which simulate daily living, do not cause cardiovascular changes that differ across gender. Further studies should examine the effects of these perturbations in the same females in different menstrual phases or in older persons.
Acknowledgements
The authors thank the participants for their time and co-operation.
Footnotes
Abbreviations: CI = Cardiac index, DBP = Diastolic blood pressure, HDT = Head down tilt, HR = Heart rate, HRV-HF = Heart rate variability - high frequency, HRV-LF = Heart rate variability - low frequency, HUT = Head up tilt, IC = Index of contractility, LBNP = Lower body negative pressure, LF_RRI/HF_RRI = Low frequency/high frequency ratio, LVET = Left ventricular ejection time, LVWI = Left ventricular work index, MAP = Mean arterial pressure, RMSSD = Root mean square of successive differences between the normal-to-normal intervals, SBP = Systolic blood pressure, SDDN = Standard deviation of the normal-to-normal intervals , SI = Stroke index, TPRI = Total peripheral resistance index.
The authors have no funding and conflicts of interest to disclose.
References
- 1.Schatz I, Bannister R, Freeman R, et al. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. Neurology 1996; 46:1470–11470. [DOI] [PubMed] [Google Scholar]
- 2.Robertson D. The pathophysiology and diagnosis of orthostatic hypotension. Clin Auton Res 2008; 18:2–7. [DOI] [PubMed] [Google Scholar]
- 3.Bullock J, Boyle J, Wang MB. Physiology. Vol 578. 4th edPhiladelphia: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 4.Guyton AC, Hall JE. Textbook of Medical Physiology. 9th edToronto, ON, Canada: Harcourt Canada Limited; 1995. [Google Scholar]
- 5.Smith JJ, Kampine JP. Circulatory Physiology: The Essentials. 3rd edBaltimore: Williams and Wilkins; 1990. [Google Scholar]
- 6.Low PA, Novak V, Spies JM, et al. Cerebrovascular regulation in the postural orthostatic tachycardia syndrome (POTS). AJMS 1999; 317:124–133. [DOI] [PubMed] [Google Scholar]
- 7.Newell DW, Aaslid R. Transcranial Doppler. New York: Raven Press; 1992. [Google Scholar]
- 8.Panerai RB. Assessment of cerebral pressure autoregulation in humans-a review of measurement methods. Physiol Meas 1998; 19:305. [DOI] [PubMed] [Google Scholar]
- 9.Tiecks FP, Lam AM, Aaslid R, et al. Comparison of static and dynamic cerebral autoregulation measurements. Stroke 1995; 26:1014–1019. [DOI] [PubMed] [Google Scholar]
- 10.Convertino VA. Gender differences in autonomic functions associated with blood pressure regulation. Am J Physiol 1998; 275:R1909–R1920. [DOI] [PubMed] [Google Scholar]
- 11.Ludwig D, Convertino V, Goldwater D, et al. Logistic risk model for the unique effects of inherent aerobic capacity on+ Gz tolerance before and after simulated weightlessness. Aviat Space Environ Med 1987; 58:1057–1061. [PubMed] [Google Scholar]
- 12.White DD, Gotshall RW, Tucker A. Women have lower tolerance to lower body negative pressure than men. J Appl Phys 1996; 80:1138–1143. [DOI] [PubMed] [Google Scholar]
- 13.Frey M, Hoffler GW. Association of sex and age with responses to lower-body negative pressure. J Appl Phys 1988; 65:1752–1756. [DOI] [PubMed] [Google Scholar]
- 14.Frey MAB, Tomaselli CM, Hoffler WG. Cardiovascular responses to postural changes: differences with age for women and men. J Clin Pharmacol 1994; 34:394–402. [DOI] [PubMed] [Google Scholar]
- 15.Gillum RF. The epidemiology of resting heart rate in a national sample of men and women: associations with hypertension, coronary heart disease, blood pressure, and other cardiovascular risk factors. Am Heart J 1988; 116:163–174. [DOI] [PubMed] [Google Scholar]
- 16.Shoemaker JK, Hogeman CS, Khan M, et al. Gender affects sympathetic and hemodynamic response to postural stress. Am J Physiol Heart Circ Physiol 2001; 281:H2028–H2035. [DOI] [PubMed] [Google Scholar]
- 17.Fu Q, Witkowski S, Okazaki K, et al. Effects of gender and hypovolemia on sympathetic neural responses to orthostatic stress. Am J Physiol 2005; 289:R109–R116. [DOI] [PubMed] [Google Scholar]
- 18.Fritsch-Yelle JM, Whitson PA, Bondar RL, et al. Subnormal norepinephrine release relates to presyncope in astronauts after spaceflight. J Appl Phys 1996; 81:2134–2141. [DOI] [PubMed] [Google Scholar]
- 19.Hart EC, Charkoudian N, Wallin BG, et al. Sex and ageing differences in resting arterial pressure regulation: the role of the β-adrenergic receptors. J Appl Phys 2011; 589:5285–5297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harm DL, Jennings RT, Meck JV, et al. Invited review: gender issues related to spaceflight: a NASA perspective. J Appl Phys 2001; 91:2374–2383. [DOI] [PubMed] [Google Scholar]
- 21.Warren J, Brannon E, Stead E, Jr, et al. The effect of venesection and the pooling of blood in the extremities on the atrial pressure and cardiac output in normal subjects with observations on acute circulatory collapse in three instances. J Clin Invest 1945; 24:337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weissler A, Warren J, Estes E, et al. Vasodepressor syncope factors influencing cardiac output. Circulation 1957; 15:875–882. [DOI] [PubMed] [Google Scholar]
- 23.Blaber AP, Hinghofer-Szalkay H, Goswami N. Blood volume redistribution during hypovolemia. Aviat Space Environ Med 2013; 84:59–64. [DOI] [PubMed] [Google Scholar]
- 24.Goswami N, Gorur P, Pilsl U, et al. Effect of orthostasis on endothelial function: a gender comparative study. PLoS One 2013; 8:e71655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goswami N, Bruner M, Xu D, et al. Short-arm human centrifugation with 0.4 g at eye and 0.75 g at heart level provides similar cerebrovascular and cardiovascular responses to standing. Eur J Appl Physiol 2015; 115:1569–1575. [DOI] [PubMed] [Google Scholar]
- 26.Goswami N, Evans J, Schneider S, et al. Effects of individualized centrifugation training on orthostatic tolerance in men and women. PLoS One 2015; 10:e0125780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O'Shea D, Lackner HK, Rössler A, et al. Influence of bed rest on plasma galanin and adrenomedullin at presyncope. Eur J Clin Invest 2015; 45:679–685. [DOI] [PubMed] [Google Scholar]
- 28.Wesseling K. Finger arterial pressure measurement with Finapres. Z Kardiol 1995; 85:38–44. [PubMed] [Google Scholar]
- 29.Kubicek W, Patterson R, Witsoe D. Impedance cardiography as a noninvasive method of monitoring cardiac function and other parameters of the cardiovascular system. Ann N Y Acad Sci 1970; 170:724–732. [Google Scholar]
- 30.Grasser E, Goswami N, Hinghofer-Szalkay H. Presyncopal cardiac contractility and autonomic activity in young healthy males. Physiol Res 2009; 58:817–821. [DOI] [PubMed] [Google Scholar]
- 31.Lackner HK, Goswami N, Papousek I, et al. Time course of cardiovascular responses induced by mental and orthostatic challenges. Int J Psychophysiol 2010; 75:48–53. [DOI] [PubMed] [Google Scholar]
- 32.Fortin J, Habenbacher W, Heller A, et al. Non-invasive beat-to-beat cardiac output monitoring by an improved method of transthoracic bioimpedance measurement. Comp Biol Med 2006; 36:1185–1203. [DOI] [PubMed] [Google Scholar]
- 33.Montgomery LD, Kirk PJ, Payne PA, et al. Cardiovascular responses of men and women to lower body negative pressure. Aviat Space Environ Med 1977; 48:138–145. [PubMed] [Google Scholar]
- 34.Ray CA. Effect of gender on vestibular sympathoexcitation. Am J Physiol 2000; 279:R1330–R1333. [DOI] [PubMed] [Google Scholar]
- 35.Sanders JS, Ferguson DW, Mark AL. Arterial baroreflex control of sympathetic nerve activity during elevation of blood pressure in normal man: dominance of aortic baroreflexes. Circulation 1988; 77:279–288. [DOI] [PubMed] [Google Scholar]
- 36.Evans JM, Ziegler MG, Patwardhan AR, et al. Gender differences in autonomic cardiovascular regulation: spectral, hormonal, and hemodynamic indexes. J Appl Phys 2001; 91:2611–2618. [DOI] [PubMed] [Google Scholar]
- 37.Stein PK, Kleiger RE, Rottman JN. Differing effects of age on heart rate variability in men and women. Am J Cardiol 1997; 80:302–305. [DOI] [PubMed] [Google Scholar]
- 38.Luzier AB, Nawarskas JJ, Añonuevo J, et al. The effects of gender on adrenergic receptor responsiveness. J Clin Pharmacol 1998; 38:618–624. [DOI] [PubMed] [Google Scholar]
- 39.Agelink MW, Malessa R, Baumann B, et al. Standardized tests of heart rate variability: normal ranges obtained from 309 healthy humans, and effects of age, gender, and heart rate. Clin Autonom Res 2001; 11:99–108. [DOI] [PubMed] [Google Scholar]
- 40.Bigger JT, Fleiss JL, Steinman RC, et al. RR variability in healthy, middle-aged persons compared with patients with chronic coronary heart disease or recent acute myocardial infarction. Circulation 1995; 91:1936–1943. [DOI] [PubMed] [Google Scholar]
- 41.Smetana P, Malik M. Sex differences in cardiac autonomic regulation and in repolarisation electrocardiography. Pflügers Arch 2013; 465:699–717. [DOI] [PubMed] [Google Scholar]
- 42.Henriksen O, Amtorp O, Faris I, et al. Evidence for a local sympathetic venoarteriolar“ reflex” in the dog hindleg. Circ Res 1983; 52:534–542. [DOI] [PubMed] [Google Scholar]
- 43.Lash J, Reilly T, Thomas M, et al. Adrenergic and pressure-dependent vascular regulation in sedentary and trained rats. Am J Physiol 1993; 265:H1064–H11064. [DOI] [PubMed] [Google Scholar]
- 44.Lundvall J. Myogenic mechanisms in the control of systemic resistance and transcapillary fluid exchange in man. J Hypertens Suppl 1989; 7:S85–91. [PubMed] [Google Scholar]
- 45.Ettinger SM, Silber DH, Collins BG, et al. Influences of gender on sympathetic nerve responses to static exercise. J Appl Phys 1996; 80:245–251. [DOI] [PubMed] [Google Scholar]
- 46.Minson CT, Halliwill JR, Young TM, et al. Influence of the menstrual cycle on sympathetic activity, baroreflex sensitivity, and vascular transduction in young women. Circulation 2000; 101:862–868. [DOI] [PubMed] [Google Scholar]
- 47.Taylor JA, Williams TD, Seals DR, et al. Low-frequency arterial pressure fluctuations do not reflect sympathetic outflow: gender and age differences. Am J Physiol 1998; 274:H1194–H1201. [DOI] [PubMed] [Google Scholar]
- 48.Barnett SR, Morin RJ, Kiely DK, et al. Effects of age and gender on autonomic control of blood pressure dynamics. Hypertension 1999; 33:1195–1200. [DOI] [PubMed] [Google Scholar]
- 49.Hinojosa Laborde C, Chapa I, Lange D, et al. Gender differences in sympathetic nervous system regulation. Clin Exp Pharmacol Physiol 1999; 26:122–126. [DOI] [PubMed] [Google Scholar]
- 50.Saeki Y, Atogami F, Takahashi K, et al. Reflex control of autonomic function induced by posture change during the menstrual cycle. J Autonom Nervous Syst 1997; 66:69–74. [DOI] [PubMed] [Google Scholar]


