Abstract
The aim of this study was to assess the status of cardiovascular health among a rural population in Northwest China and to determine the associated factors for cardiovascular health.
A population-based cross-sectional study was conducted in the rural areas of Hanzhong in Northwest China. Interview, physical examination, and fasting blood glucose and lipid measurements were completed for 2693 adults. The construct of cardiovascular health and the definitions of cardiovascular health metrics proposed by the American Heart Association were used to assess cardiovascular health. The proportions of subjects with cardiovascular health metrics were calculated, adjusting for age and sex. The multiple logistic regression model was used to evaluate the association between ideal cardiovascular health and its associated factors.
Only 0.5% (0.0% in men vs 0.9% in women, P = 0.002) of the participants had ideal cardiovascular health, whereas 33.8% (18.0% in men vs 50.0% in women, P < 0.001) and 65.7% (82.0% in men vs 49.1% in women, P < 0.001) of the participants had intermediate and poor cardiovascular health, respectively. The prevalence of poor cardiovascular health increased with increasing age (P < 0.001 for trend). Participants fulfilled, on average, 4.4 (95% confidence interval: 4.2–4.7) of the ideal cardiovascular health metrics. Also, 22.2% of the participants presented with 3 or fewer ideal metrics. Only 19.4% of the participants presented with 6 or more ideal metrics. 24.1% of the participants had all 4 ideal health factors, but only 1.1% of the participants had all 4 ideal health behaviors. Women were more likely to have ideal cardiovascular health, whereas adults aged 35 years or over and those who had a family history of hypertension were less likely to have ideal cardiovascular health.
The prevalence of ideal cardiovascular health was extremely low among the rural population in Northwest China. Most adults, especially men and the elderly, had a poor cardiovascular health status. To improve cardiovascular health among the rural population, efforts, especially lifestyle improvements, education and interventions to make healthier food choices, reduce salt intake, increase physical activities, and cease smoking, will be required at the individual, population, and social levels.
Keywords: cardiovascular health, China, epidemiology, rural area
1. Introduction
Cardiovascular disease (CVD) has been the leading cause of morbidity and mortality in developed countries[1,2] and some developing countries, such as China.[1,3] The 2013 Global Burden of Disease Study showed that cardiovascular deaths accounted for almost a third of all deaths globally.[1] In China, CVD is responsible for 41% of all annual deaths, and the increase in CVD mortality in rural residents is greater than that in urban citizens.[3]
The American Heart Association (AHA) Strategic Planning Task Force and Statistics Committee[4] developed the concept of “cardiovascular health” along with 7 health metrics, which were categorized as 4 health behaviors (smoking, diet, physical activity, body mass index [BMI]) and 4 health factors (smoking, blood pressure, total cholesterol [TC], fasting plasma glucose [FPG]). Given the importance of abstinence from smoking and smoking cessation for health promotion, smoking is listed in both the health factors and health behaviors.[4] With the use of the 7 metrics, the cardiovascular health status for a whole population is defined as ideal, intermediate, or poor.[4] Epidemiologic evidence indicates that ideal cardiovascular health is associated with a lower risk of CVD,[5–7] lower mortality rates of CVD and lower all-cause mortality,[8–10] as well as disease-free survival, better quality of life, and lower healthcare costs.[4]
Several studies have determined the status of the AHA-defined cardiovascular health in the USA and European populations.[9–19] However, the AHA's construct of cardiovascular health has not been widely used among populations from developing countries. There are no data available on the status of cardiovascular health, health behaviors, and health factors among rural populations of China. The purpose of this study was to assess the status of cardiovascular health and its associated metrics among rural adults in Northwest China.
2. Methods
2.1. Study population and data collection
A population-based cross-sectional study was conducted in the rural areas of Hanzhong, Shaanxi Province, in Northwest China between October 2010 and November 2010 to estimate CVD risk factors among rural adults. Hanzhong is relatively poor and less developed than the coastal, eastern and southern regions of China. A stratified cluster random sampling method was used for sample selection. There are 9 “township” regions in the study area, and an average of approximately 17 (ranging from 15 to 36) villages in each township region. We stratified the study according to the township, that is, each township was a stratum, and 1 village (cluster) was randomly chosen from each township. Using residential registration data, all the available and eligible adults in the chosen villages were informed and invited to participate in the survey several days before the survey. In each chosen village, adults who consented and came to the clinic of the village doctor, where the interview and physical examination were conducted, on a nominated survey day were chosen as subjects of the survey.
Information on the participants was collected through an interview that collected their age, sex, education, marital status, family economic level, smoking, physical activity, history of clinical CVD (coronary heart disease, heart failure, myocardial infarction, stroke, or other heart-related conditions), hypertension, diabetes and dyslipidemia, use of antihypertensive, antidiabetic and dyslipidemia medications, and family history of hypertension. Blood pressure was measured by trained doctors from the Hanzhong People's Hospital after the subject had rested for at least 5 minutes, using a standard mercury sphygmomanometer with the participant in the sitting position. Two blood pressure measurements separated by a 2-minute interval were obtained, and the mean of the 2 readings was used as the blood pressure value. Height and weight were measured with participants standing without shoes or heavy outer garments, from which BMI (kg/m2) was calculated. Dietary intake and alcohol consumption (including grape wine, rice wine, beer, and liquor) within the past year were assessed using a semi-quantified food frequency questionnaire. According to the reference in the Dietary Guidelines for Chinese (≤25 g/d alcohol for men and ≤15 g/d alcohol for women),[20] alcohol consumption was classified into 3 categories: nondrinking (did not consume any type of alcohol or consumed <1 drink per month), moderate drinking (men consumed ≤25 g/d alcohol and women consumed ≤15 g/d alcohol), and heavy drinking (men consumed >25 g/d alcohol and women consumed >15 g/d alcohol). To identify the family economic status of the participants, a wealth index based on communication tools, transportation tools, sources of water, and monthly incomes and expenses of the whole family was derived using a principal component analysis. The first principal component was selected as the wealth index. The participants’ family economic level was categorized into 3 groups of low, moderate and high, according to the tertiles of the wealth index.[21] The overnight fasting blood sample was collected from each subject by a qualified nurse. The fasting time was verified before blood sample collection, and the participants who had not fasted for at least 8 hours did not have their blood drawn. FPG and TC levels were analyzed enzymatically. Detailed information on the sampling, data collecting, and blood sample collecting, transporting, storing and analyzing have been described previously.[22]
2.2. Definition of cardiovascular health metrics and cardiovascular health
In accordance with the AHA's definition,[4] the status of each cardiovascular health metric was categorized as “ideal,” “intermediate,” and “poor” as follows.
2.2.1. Health behaviors
(1) Smoking: never smoking or having quit >12 months ago was defined as ideal; having quit smoking ≤12 months was defined as intermediate; and current active smoking was defined as poor. (2) BMI: BMI was classified as ideal (<25.0 kg/m2), intermediate (25.0–29.9 kg/m2), or poor (≥30.0 kg/m2). (3) Physical activity: participants who often performed farm labor or other heavy or moderate manual labor were categorized as ideal; participants who sometimes performed farm labor or other heavy or moderate manual labor were categorized as intermediate; and participants who hardly ever performed farm labor or other heavy or moderate manual labor were categorized as poor. (4) Diet: after adjusting for the level of dietary calorie intake, participants who achieved 4 to 5 diet goals (including ≥4.5 cups per day of fruits and vegetables, ≥ two 3.5-oz servings per week of fish, ≥ three 1-oz equivalent servings per day of fiber-rich whole grains, <1500 mg per day of sodium, and ≤ 36 oz per week of sugar-sweetened beverages for a 2000-kcal diet) were categorized as ideal; participants who achieved 2 to 3 items were categorized as intermediate; and those who achieved 0 to 1 items were categorized as poor.
2.2.2. Health factors
(1) Smoking: see definition in “health behaviors.” (2) TC: TC status was defined as ideal (<200 mg/dL, untreated), intermediate (200–239 mg/dL or treated to <200 mg/dL), and poor (≥240 mg/dL). (3) Blood pressure: blood pressure status was classified as ideal (systolic blood pressure [SBP] <120 mm Hg and diastolic blood pressure [DBP] <80 mm Hg, untreated), intermediate (SBP 120–139 mm Hg or DBP 80–89 mm Hg, or treated to SBP <120 mm Hg and DBP <80 mm Hg), or poor (SBP ≥140 or DBP ≥90 mm Hg). (4) FPG: FPG status was classified as ideal (<100 mg/dL, untreated), intermediate (100–125 mg/dL, or treated to <100 mg/dL), or poor (≥126 mg/dL).
2.2.3. Cardiovascular health
Considering these health metrics, we defined an overall measure of cardiovascular health as follows: “ideal” if all 7 cardiovascular health metrics are ideal and without a history of clinical CVD; “intermediate” if at least 1 metric is at an intermediate level and none are at a poor level among subjects without a CVD history or if all 7 metrics are at an ideal level among subjects with a CVD history; and “poor” otherwise (at least 1 metric is at a poor level among subjects without a CVD history or at least 1 metric is at an intermediate level among subjects with a CVD history).[4,5,23,24]
2.3. Ethics statement
The study complied with the Declaration of Helsinki and was reviewed and approved by the Ethics Committee of Xi’an Jiaotong University College of Medicine. Written informed consent had been obtained from each study participant.
2.4. Statistical analyses
The Complex Samples Procedure of SPSS 13.0 for Windows (SPSS Inc., Chicago, IL) was used for statistical analyses, accounting for township strata and village clusters. All statistical tests were 2-tailed, and statistical significance was set at P < 0.05. Continuous variables are presented as the mean ± SD. Categorical variables are presented as percentages. The proportions of ideal, intermediate and poor categories for each metric, and the overall cardiovascular health were calculated and adjusted for age and/or sex according to the 2010 Chinese National Census Population distribution. Differences between means were compared using general linear models. Chi-square tests and Fisher's exact tests were used to compare percentages. Multiple logistic regression was used to evaluate the association between ideal cardiovascular health (dependent variable) and its associated factors.
3. Results
3.1. General characteristics of the study population
A total of 3016 residents aged 20 to 80 years took part in the survey. However, 2693 participants had complete interview, diet, physical examination and blood sample data, and were included in the analysis. Forty-one participants who had no blood sample data (including 20 who refused to draw blood sample and 21 who did not fast overnight), 276 who had incomplete information on health factors or health behaviors, and 6 who had extreme energy intake (>5000 kcal/d or <500 kcal/d) were excluded.
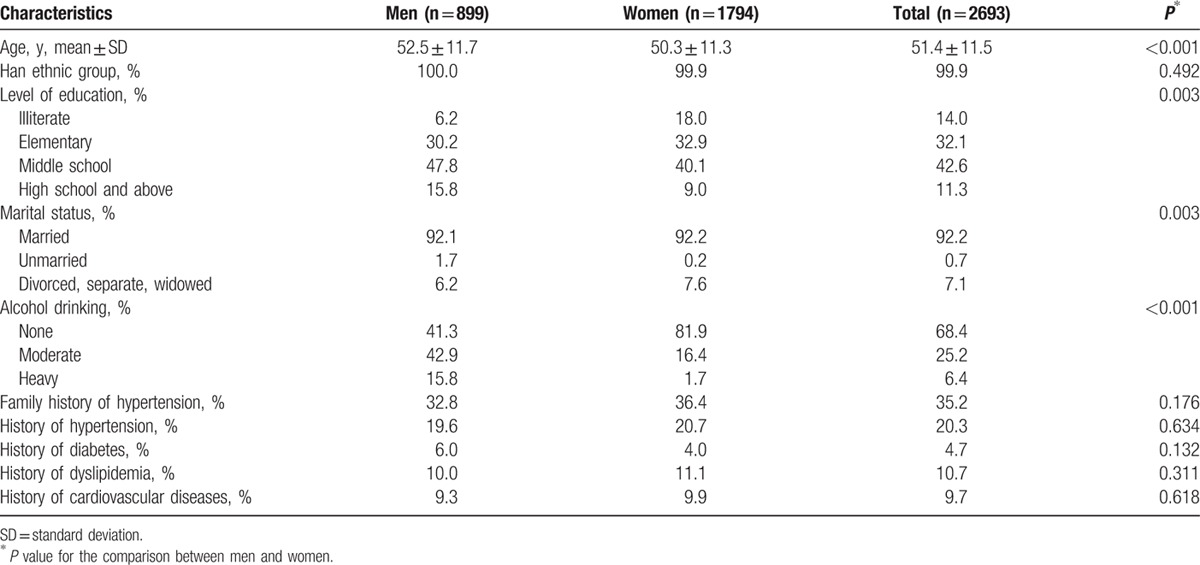
The socio-demographic characteristics and history of relevant diseases of the participants in the analysis are shown in Table 1. There were 899 (33.4%) participants who were men and 1794 (66.6%) who were women. The mean age of the participants was 51.4 ± 11.5 years. Most (99.9%) of the participants were ethnic Han Chinese, and 53.9% of them finished middle school education or above. A total of 92.2% participants were married. No statistically significant differences with respect to socio-demographic characteristics were detected between the 2693 subjects with complete data and the 323 excluded participants with incomplete data.
Table 1.
Characteristics of the study participants at the time of survey.
3.2. Distribution of individual cardiovascular health metrics
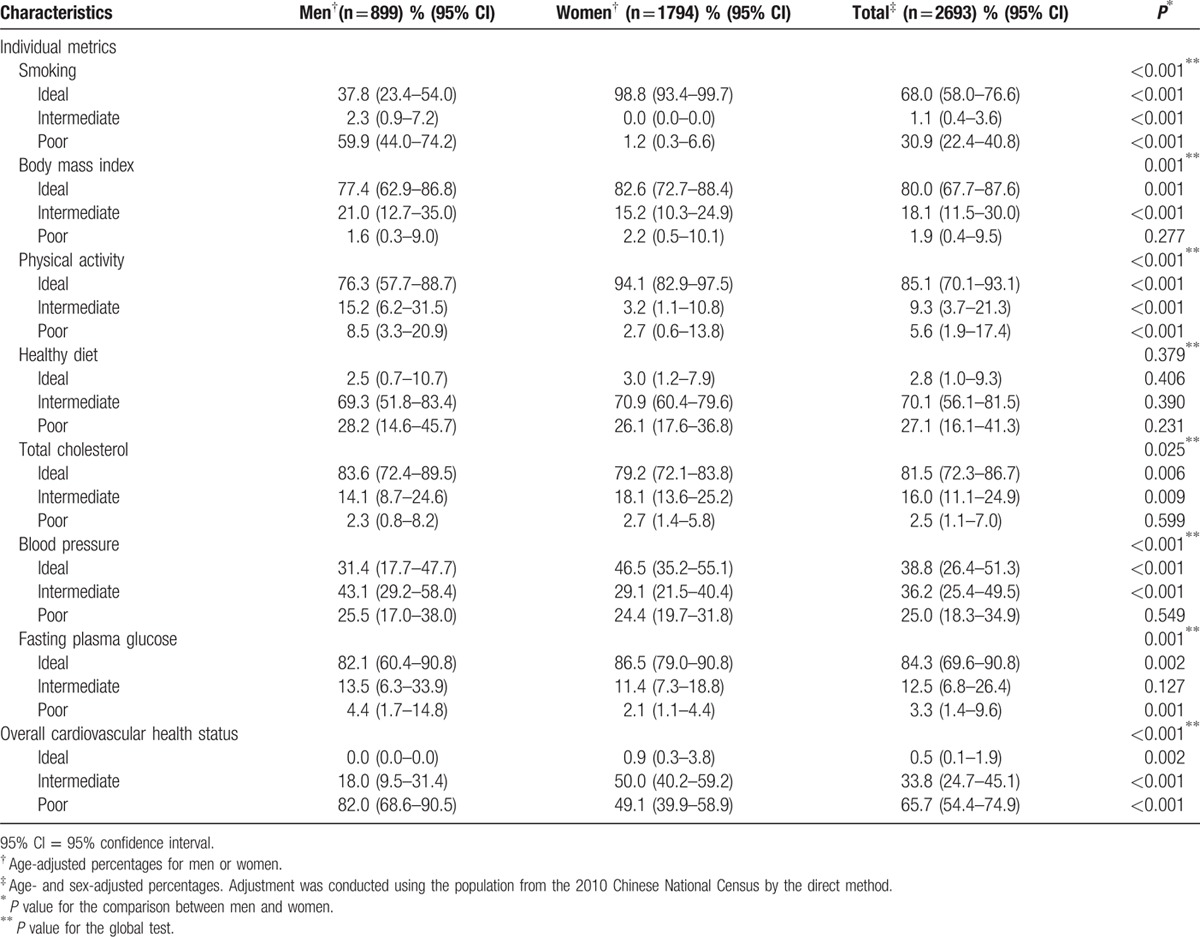
The distribution of individual cardiovascular health metrics in the study population is shown in Table 2. Most of the participants met the ideal cardiovascular health metrics for smoking, BMI, physical activity, TC, and FPG (68.0%, 80.0%, 85.1%, 81.5%, and 84.3%, respectively), whereas most of the participants’ diet and blood pressure levels were classified into intermediate and poor categories. Only 2.8% of the participants fulfilled 4 to 5 items of healthy diet, and 38.8% of the participants’ blood pressure values were <120/80 mm Hg. The percentages of women who met the ideal level for smoking, BMI, physical activity, blood pressure, and FPG were higher than those of men (all P < 0.01). Only for TC, the percentage of men who met ideal level was higher than that of women (P = 0.006). The percentages of men and women who met the ideal level of healthy diet were both low, and there was no gender difference (2.5% vs 3.0%, P = 0.406). The most prevalent poor metric was smoking (59.9%) for men and healthy diet (26.1%) for women.
Table 2.
Distribution of individual cardiovascular health metrics and overall cardiovascular health status.
Except for sugar-sweetened beverages intake, the healthy diet components were poorly met. Almost all participants (96.3% in total, 95.1% in men, and 97.5% in women) achieved the goal of sugar-sweetened beverages intake. However, only 52.2% (52.4% in men and 52.1% in women), 36.6% (34.2% in men and 39.0% in women), 8.4% (9.2% in men and 7.7% in women), and 7.6% (8.5% in men and 6.6% in women) of the participants achieved the goal of fiber-rich whole grains, fruit and vegetable, sodium, and fish intake, respectively.
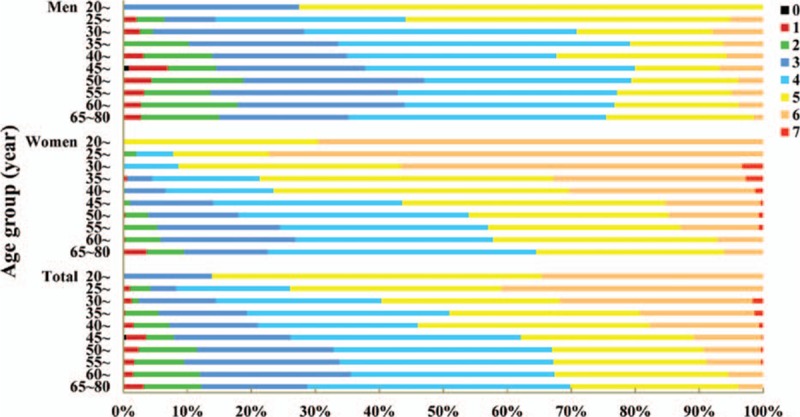
3.3. Distribution of cardiovascular health status
As presented in Table 2, only 0.5% participants achieved ideal cardiovascular health, and the proportion for men was lower than that for women (0.0% vs 0.9%, P = 0.002). The proportion of intermediate cardiovascular health was also low (33.8%), and it was lower in men than in women (18.0% vs 50.0%, P < 0.001). The remaining 65.7% of the participants had poor cardiovascular health. The prevalence of poor cardiovascular health increased with increasing age (P < 0.001 for trend, Fig. 1).
Figure 1.
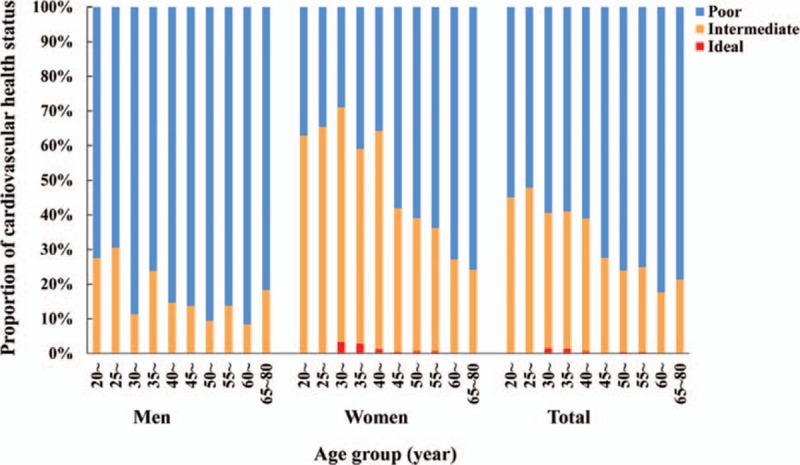
Distribution of cardiovascular health status among the study population by age and sex.
The participants fulfilled, on average, 4.4 (95% confidence interval [95% CI]: 4.2–4.7) ideal cardiovascular health metrics, with a decrease across age-groups (from 5.1 [95% CI: 4.7–5.4] in participants <25 years old to 3.9 [95% CI: 3.8–4.0] in participants 65 years or older; P < 0.001, Fig. 2). Women exhibited a higher number of ideal metrics than men across all age groups (4.9 [95% CI: 4.7–5.1] vs 3.9 [95% CI: 3.6–4.2], respectively, P < 0.001). A total of 22.2% of the participants presented with 3 or fewer ideal metrics (33.7% in men vs 10.5% in women, P < 0.001). Only 19.4% of the participants presented with 6 or more ideal metrics (4.6% in men vs 34.5% in women, P < 0.001, Fig. 3). The proportion of subjects who had 6 or more ideal metrics significantly decreased with increasing age, from 34.6% in participants under 25 years old to 3.9% in participants 65 years old or over (P < 0.001 for trend). A total of 24.1% of the participants were ideal on all 4 health factors, and only 1.1% were ideal on all 4 health behaviors; the proportions of men were lower than those of women (9.0% vs 39.6% on all 4 health factors, 0.1% vs 2.2% on all 4 health behaviors, both P < 0.001).
Figure 2.
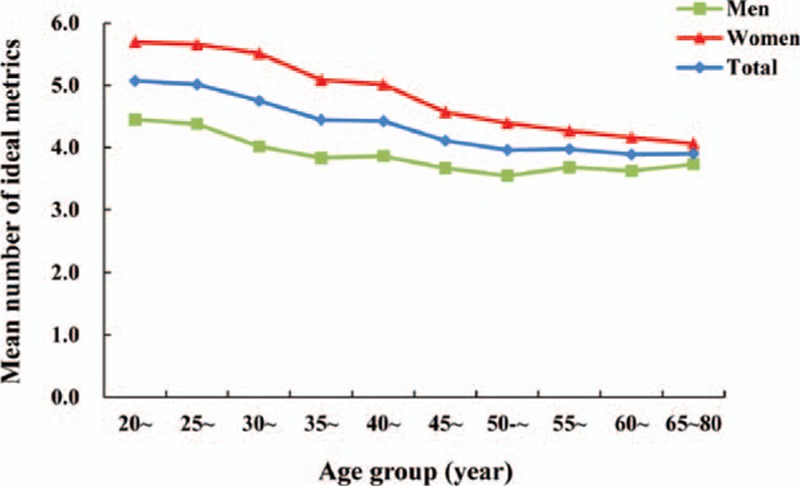
Mean numbers of ideal cardiovascular health metrics among the study population.
Figure 3.
Distribution of ideal cardiovascular health metrics number among the study population.
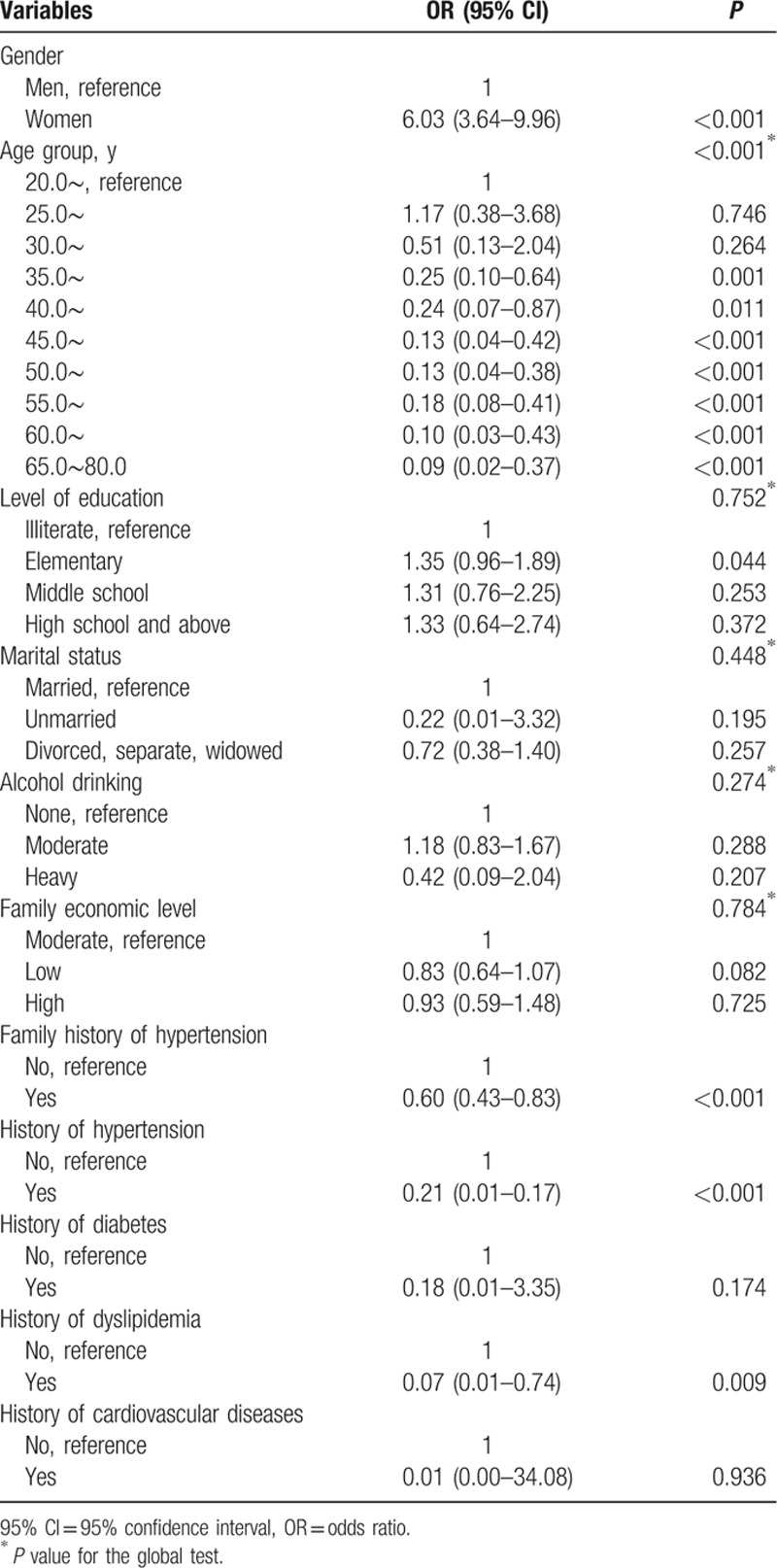
3.4. Multiple logistic regression analyses
Because of the low percentage (only 0.5%) of the participants who met the ideal cardiovascular health, having 6 or more ideal metrics with no history of clinical CVD was used as one category (ideal cardiovascular health) and having 5 or less ideal metrics or with a history of clinical CVD was used as another category (nonideal cardiovascular health) of outcome in the Complex Samples multiple logistic regression analysis on the associated factors for ideal cardiovascular health. History of hypertension, diabetes, dyslipidemia, and CVD were controlled for in the logistic regression model. The results are presented in Table 3. Women were 6.03 times more likely to have an ideal cardiovascular health compared with men (95% CI: 3.64–9.96). Compared with adults <25 years old, participants 35 years old or over were less likely to have ideal cardiovascular health and the ORs decreased with increasing age, from 0.25 (95% CI: 0.10–0.64) to 0.09 (95% CI: 0.02–0.37). Compared with adults without a family history of hypertension, participants with a family history of hypertension were less likely to have ideal cardiovascular health (OR: 0.60, 95% CI: 0.43–0.83). Education level, marital status, alcohol drinking, and family economic status were also explored, but no associations were found with ideal cardiovascular health (all P > 0.05).
Table 3.
Results of logistic regression analysis of associated factors for the ideal cardiovascular health.
4. Discussion
This study is the first population-based study to use the AHA-defined construct of cardiovascular health among the rural population in Northwest China. The results of our study showed that the prevalence of ideal cardiovascular health was extremely low, whereas poor cardiovascular health was prevalent among the rural population in Northwest China.
The estimated low prevalence (0.5%) of ideal cardiovascular health among the study population is consistent with the results from the USA (0.1–3.3%),[2,5,9–11,13–16] from Spain (0.2%),[17] from Srpska (0.02%),[18] from Italy (1.9%),[19] in urban adults from China (0.5%)[25] and from a health examination population in Southeast China (1.1%).[26] Our results add to previous reports that the prevalences of ideal cardiovascular health are very low in various countries and populations and indicate that effective efforts are needed to improve cardiovascular health levels among the rural population in Northwest China to prevent an epidemic of cardiovascular diseases.
Our study showed that women had a better cardiovascular health profile than men. This sex difference might be accounted for by the much higher prevalence of current smoking (59.9% vs 1.2%) whereas a lower prevalence of ideal physical activity (76.3% vs 94.1%) in men than those in women. With economic development and urbanization, physical activities have declined rapidly in Chinese adults, especially in men who do less household work.[27] Efforts should be taken to cease smoking and promote recreational physical activities and exercise among the rural population, especially among men, in Northwest China.
Moreover, our study found that the proportion of adults who met the ideal level on all 4 health behaviors (1.1%) was much lower than that of all 4 ideal health factors (24.1%). This finding indicates that education and interventions to promote people's lifestyle are much more necessary to improve the cardiovascular health among rural adults in Northwest China. A healthy diet was the least prevalent cardiovascular health metric among the study population. Only 8.4% of rural adults in Northwest China reached the goals for sodium intake. Studies showed that high sodium intake was a major risk factor for hypertension and increased the risks of heart attack, stroke, left ventricular hypertrophy, obesity, and renal disease.[28] Modest reductions in dietary salt could substantially reduce cardiovascular events and medical costs.[29–31] Du et al[32] reported that the Chinese population's sodium intake decreased from 6.6 g/d in 1991 to 4.7 g/d in 2009 but remained at double of that recommended. In China, sodium intake was higher in rural areas than in urban areas[32] and higher among Northerners than among Southerners; most of the dietary sodium was from salt added in home cooking.[33] Therefore, population strategies and measures targeted at individuals to reduce salt intake are necessary and urgent for the prevention and control of CVD among the rural population in Northwest China. Anderson and colleagues suggested that efforts to remove excess sodium from diets in rural China should focus on reducing salt in home cooking.[33] Moreover, because of the salt monopoly in China, introducing a low-sodium salt substitute and convincing the salt industry to gradually reduce the sodium content in China's entire salt supply may be possible.[34]
Physical inactivity is the greatest public health problem of the 21st century.[35] It has a major health effect worldwide, resulting in 6% burden of disease from coronary heart disease, 7% from type 2 diabetes, 10% from breast cancer, and 10% from colon cancer.[36] A decrease in or removal of this unhealthy behavior could improve health substantially.[36] The population of our study was composed of farmers in the rural areas of Northwest China. They usually worked in farming, and in the slack seasons, some of them went to work at rural factories as “blue-collar” workers. Studies showed that in China, more rural residents participated in work-related physical activity than their urban counterparts.[37] Rural residents’ intensity of physical activity during working hours was greater than that of urban citizens.[38] However, with China's rapid urbanization and economic growth in the past few decades, decreases in physical activity have been reported for several domains, including occupation, transportation and household activity, and work-related physical activity decreased in both rural and urban residents, but the rate of decrease was greater in rural areas than that in urban areas.[27,38,39] Moreover, compared with urban citizens, rural residents are more likely to be physically inactive in leisure time.[40]
Previous studies showed that the prevalence of metabolic syndrome (12.8% for men, 17.4% for women, 15.1% overall), according to the modified National Cholesterol Education Program Adult Treatment Panel III criteria, in this rural population was lower than the prevalence among urban adults in China (28.4% for men and 35.1% for women) and much lower than the prevalence among US adults (32.8% for men, 36.6% for women, 34.7% overall).[22,41,42] A meta-analysis also showed that the Chinese people in urban areas (24.9%) were more likely to suffer from metabolic syndrome than those in rural areas (19.2%).[43] Lower physical activity, lower intake of fruits and vegetables, and greater consumption of animal fat among urban citizens than rural residents might account for the difference in prevalence of metabolic syndrome between urban and rural areas. However, the rapid economic development and urbanization in China during the past few decades has increasingly promoted a sedentary lifestyle, an elevated consumption of energy-dense foods, and greater psychological stress, all of which increase the risk of metabolic syndrome, type 2 diabetes and CVD.[44–49] This has had a greater impact on rural residents, who generally have a lower education level, lower economic status, less awareness and knowledge of risk factors for health and poorer access to health care than urban residents.[44,47–53] Studies showed that the prevalence of metabolic syndrome and CVD mortality increased more among rural residents than urban residents during the past decade, and the gap between urban and rural residents became narrowed.[3,44] The burden of CVD will shift quickly to the rural people in China.
Thus, intervention strategies to promote physical activity, especially physical activity during leisure-time to compensate for declines in occupational and household activity, should be a major health priority in rural China. Fortunately, improving the availability of exercise facilities in communities and implementing fitness projects for rural residents have become a national policy, as highlighted in China's Twelfth Five-Year Plan (2011–2015) for Building the Public Sport Infrastructure.[54] This plan advocates the cooperation of central and local governments with civil society and public and private stakeholders to build new exercise facilities, such as community fitness parks and roadside open spaces with exercise and sports equipment, and to enhance the accessibility of existing facilities, for example, by opening the gymnasium and exercise facilities of schools, governments, enterprises, and organizations to the public.[54] Moreover, school education and mass media campaigns are also needed to improve the health behaviors of rural residents. They could protect people's health by providing health information, improving health literacy, and promoting physical activity, healthy diets, and other healthy behaviors.[55]
4.1. Limitations
Our study has some limitations. First, concerning data quality, although most health metrics were measured reliably and objectively, the physical activity data in the study population may be subject to reporting bias because they were based on self-reporting and evaluated according to the type and frequency of physical activity at work and due to housework in the past year. Specific instruments of physical activity were not used and the amount of activity (minutes per week) could not be derived. Second, some factors that may relate to CVD status were not recorded at all. For example, information about the participants’ family history of diabetes, stroke, coronary heart disease, and other cardiovascular diseases, as well as medication use for conditions except for hypertension, diabetes, or dyslipidemia were not collected in the study. Thus, we could not analyze the association between these variables and cardiovascular health status in the study population. As a result, the observed differences in health metrics may be confounded by unobserved heterogeneity. Third, all measurements of health behaviors and health factors were obtained from a single visit on the examination day; thus, there is a possibility of misclassification. For example, blood pressure measurement from a single visit usually overestimates hypertension prevalence.[56] However, measurements from a single visit are often used in epidemiologic studies. Fourth, recall bias may be another limitation in the measurement of physical activity, diet, smoking, and other information determined from questionnaires. Therefore, future studies are needed to confirm the cardiovascular health status and its associated factors among the rural population in Northwest China.
5. Conclusions
Our study indicated that the prevalence of ideal cardiovascular health was extremely low among the rural population in Northwest China, and most adults, especially men and the elderly, had a poor cardiovascular health status. To improve cardiovascular health among the rural population in Northwest China, efforts, especially lifestyle improvements, education and interventions to make healthier food choices, reduce salt intake, increase physical activities, and cease smoking, will be required at the individual, population and social levels, and should begin at a young age.
Acknowledgments
The authors thank the participants, organizers, and implementers of the survey, particularly Dr. Xianglin Xu, Mr. Yong Ren, and Ms. Shaomei Pan who were responsible for data collection. The authors are grateful to the village doctors for their efforts in the coordination of the fieldwork. They are also grateful to all the investigators for their contributions to data collection. Thanks also go to the editor and reviewers of the manuscript for their constructive comments and suggestions.
Footnotes
Abbreviations: 95% CI = 95% confidence interval, AHA = American Heart Association, BMI = body mass index, CVD = cardiovascular disease, DBP = diastolic blood pressure, FPG = fasting plasma glucose, OR = odds ratio, SBP = systolic blood pressure, TC = total cholesterol.
Funding: This work was supported by the Science and Technology Research and Development Program of Shaanxi Province, China (Grant No. 2013K14-02-15), the China Medical Board (Grant No. 08-925), and the National Natural Science Foundation of China (Grant No. 81230016). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to disclose.
References
- 1.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 385:117–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Go A S, Mozaffarian D, Roger V L, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 2014; 129:e28–e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu SS, Kong LZ, Gao RL, et al. Outline of the report on cardiovascular disease in China, 2010. Biomed Environ Sci 2012; 25:251–256. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's Strategic Impact Goal through 2020 and beyond. Circulation 2010; 121:586–613. [DOI] [PubMed] [Google Scholar]
- 5.Folsom AR, Yatsuya H, Nettleton JA, et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol 2011; 57:1690–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong C, Rundek T, Wright CB, et al. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: the northern Manhattan study. Circulation 2012; 125:2975–2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu S, Huang Z, Yang X, et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes 2012; 5:487–493. [DOI] [PubMed] [Google Scholar]
- 8.Liu Y, Chi HJ, Cui LF, et al. The ideal cardiovascular health metrics associated inversely with mortality from all causes and from cardiovascular diseases among adults in a Northern Chinese industrial city. PLoS One 2014; 9:e89161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA 2012; 307:1273–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation 2012; 125:987–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bambs C, Kip KE, Dinga A, et al. Low prevalence of “ideal cardiovascular health” in a community-based population: the heart strategies concentrating on risk evaluation (Heart SCORE) study. Circulation 2011; 123:850–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crichton GE, Elias MF, Davey A, et al. Cardiovascular health: a cross-national comparison between the Maine Syracuse Study (Central New York, USA) and ORISCAV-LUX (Luxembourg). BMC Public Health 2014; 14:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogunmoroti O, Younus A, Rouseff M, et al. Assessment of American Heart Association's Ideal Cardiovascular Health Metrics Among Employees of a Large Healthcare Organization: The Baptist Health South Florida Employee Study. Clin Cardiol 2015; 38:422–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shay CM, Ning H, Allen NB, et al. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation 2012; 125:45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim JI, Sillah A, Boucher JL, et al. Prevalence of the American Heart Association's “ideal cardiovascular health” metrics in a rural, cross-sectional, community-based study: the Heart of New Ulm Project. J Am Heart Assoc 2013; 2:e000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fang J, Yang Q, Hong Y, et al. Status of cardiovascular health among adult Americans in the 50 States and the District of Columbia, 2009. J Am Heart Assoc 2012; 1:e005371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graciani A, Leon-Munoz LM, Guallar-Castillon P, et al. Cardiovascular health in a southern Mediterranean European country: a nationwide population-based study. Circ Cardiovasc Qual Outcomes 2013; 6:90–98. [DOI] [PubMed] [Google Scholar]
- 18.Jankovic S, Stojisavljevic D, Jankovic J, et al. Association of socioeconomic status measured by education, and cardiovascular health: a population-based cross-sectional study. BMJ Open 2014; 4:e005222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vetrano DL, Martone AM, Mastropaolo S, et al. Prevalence of the seven cardiovascular health metrics in a Mediterranean country: results from a cross-sectional study. Eur J Public Health 2013; 23:858–862. [DOI] [PubMed] [Google Scholar]
- 20.Chinese Nutrition Society. The Dietary Guidelines for Chinese, 2010. Lhasa: Tibet People's Publishing House; 2011. [Google Scholar]
- 21.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography 2001; 38:115–132. [DOI] [PubMed] [Google Scholar]
- 22.Zhao Y, Yan H, Yang R, et al. Prevalence and determinants of metabolic syndrome among adults in a rural area of Northwest China. PLoS One 2014; 9:e91578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu HY, Sun ZH, Cao DP, et al. Cardiovascular health status in Chinese adults in urban areas: analysis of the Chinese Health Examination Database 2010. Int J Cardiol 2013; 168:760–764. [DOI] [PubMed] [Google Scholar]
- 24.Bi Y, Jiang Y, He J, et al. Status of cardiovascular health in chinese adults. J Am Coll Cardiol 2015; 65:1013–1025. [DOI] [PubMed] [Google Scholar]
- 25.Zeng Q, Dong SY, Song ZY, et al. Ideal cardiovascular health in Chinese urban population. Int J Cardiol 2013; 167:2311–2317. [DOI] [PubMed] [Google Scholar]
- 26.Lu Y, Shen S, Qi H, et al. Prevalence of ideal cardiovascular health in southeast Chinese adults. Int J Cardiol 2015; 184:385–387. [DOI] [PubMed] [Google Scholar]
- 27.Ng SW, Norton EC, Popkin BM. Why have physical activity levels declined among Chinese adults? Findings from the 1991–2006 China Health and Nutrition Surveys. Soc Sci Med 2009; 68:1305–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens 2009; 23:363–384. [DOI] [PubMed] [Google Scholar]
- 29.Bibbins-Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010; 362:590–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.He FJ, Marciniak M, Visagie E, et al. Effect of modest salt reduction on blood pressure, urinary albumin, and pulse wave velocity in white, black, and Asian mild hypertensives. Hypertension 2009; 54:482–488. [DOI] [PubMed] [Google Scholar]
- 31.Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low-sodium diet vs. high-sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride (Cochrane Review). Am J Hypertens 2012; 25:1–15. [DOI] [PubMed] [Google Scholar]
- 32.Du S, Batis C, Wang H, et al. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr 2014; 99:334–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anderson CA, Appel LJ, Okuda N, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc 2010; 110:736–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hvistendahl M. China tries to kick its salt habit. Science 2014; 345:1268–1269. [DOI] [PubMed] [Google Scholar]
- 35.Blair SN. Physical inactivity: the biggest public health problem of the 21st century. Br J Sports Med 2009; 43:1–2. [PubMed] [Google Scholar]
- 36.Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012; 380:219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muntner P, Gu D, Wildman RP, et al. Prevalence of physical activity among Chinese adults: results from the International Collaborative Study of Cardiovascular Disease in Asia. Am J Public Health 2005; 95:1631–1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xie G, Mai J, Zhao L, et al. Physical activity status of working time and its change over a ten-year period in Beijing and Guangzhou populations. Wei Sheng Yan Jiu 2008; 37:33–36. [PubMed] [Google Scholar]
- 39.Monda KL, Adair LS, Zhai F, et al. Longitudinal relationships between occupational and domestic physical activity patterns and body weight in China. Eur J Clin Nutr 2008; 62:1318–1325. [DOI] [PubMed] [Google Scholar]
- 40.Zheng J, An R. Satisfaction with local exercise facility: a rural-urban comparison in China. Rural Remote Health 2015; 15:2990. [PubMed] [Google Scholar]
- 41.Aguilar M, Bhuket T, Torres S, et al. Prevalence of the metabolic syndrome in the United States, 2003–2012. JAMA 2015; 313:1973–1974. [DOI] [PubMed] [Google Scholar]
- 42.Xu WH, Ruan XN, Fu XJ, et al. Prevalence of the metabolic syndrome in Pudong New Area of Shanghai using three proposed definitions among Chinese adults. BMC Public Health 2010; 10:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li R, Li W, Lun Z, et al. Prevalence of metabolic syndrome in mainland china: a meta-analysis of published studies. BMC Public Health 2016; 16:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lao XQ, Ma WJ, Sobko T, et al. Dramatic escalation in metabolic syndrome and cardiovascular risk in a Chinese population experiencing rapid economic development. BMC Public Health 2014; 14:983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Rezende LF, Rodrigues Lopes M, Rey-Lopez JP, et al. Sedentary behavior and health outcomes: an overview of systematic reviews. PLoS One 2014; 9:e105620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Leischik R, Foshag P, Strauss M, et al. Aerobic capacity, physical activity and metabolic risk factors in firefighters compared with police officers and sedentary clerks. PLoS One 2015; 10:e0133113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sperling LS, Mechanick JI, Neeland IJ, et al. The CardioMetabolic Health Alliance: working toward a new care model for the metabolic syndrome. J Am Coll Cardiol 2015; 66:1050–1067. [DOI] [PubMed] [Google Scholar]
- 48.Soler-Vila H, Garcia-Esquinas E, Leon-Munoz LM, et al. Contribution of health behaviours and clinical factors to socioeconomic differences in frailty among older adults. J Epidemiol Community Health 2016; 70:354–360. [DOI] [PubMed] [Google Scholar]
- 49.Leischik R, Dworrak B, Strauss M, et al. Plasticity of Health. German J Med 2016; 1:1–17. [Google Scholar]
- 50.Marmot MG, Shipley MJ. Do socioeconomic differences in mortality persist after retirement? 25 year follow up of civil servants from the first Whitehall study. BMJ 1996; 313:1177–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilkinson RG. Socioeconomic determinants of health. Health inequalities: relative or absolute material standards? BMJ 1997; 314:591–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Demakakos P, Biddulph JP, Bobak M, et al. Wealth and mortality at older ages: a prospective cohort study. J Epidemiol Community Health 2016; 70:346–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ugwuja E, Ogbonna N, Nwibo A, et al. Overweight and obesity, lipid profile and atherogenic indices among civil dervants in Abakaliki, South Eastern Nigeria. Ann Med Health Sci Res 2013; 3:13–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.General Administration of Sport of China. China's Twelfth Five-Year Plan (2011–2015) for Building the Public Sport Infrastructure. 2012; http://www.sport.gov.cn/n16/n33193/n33208/n33448/n33793/3425606.html Accessed Mar, 20, 2016. [Google Scholar]
- 55.World Health Organization. Global Strategy on Diet, physical Activity and Health 2004; http://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_english_web.pdf Accessed Mar, 20, 2016. [Google Scholar]
- 56.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA 2010; 303:2043–2050. [DOI] [PubMed] [Google Scholar]


