Supplemental Digital Content is available in the text.
Summary:
Gynecomastia is a benign proliferation of male breast glandular tissue. Gynecomastia can affect men at any stage of life. Traditional treatment options involved excisional surgeries with periareolar or T-shaped scars, which can leave more visible scars on the chest. The technique presented represents a technique used by the senior author, which relies on ultrasonic liposuction and pull-through technique to remove breast tissue. A retrospective chart review was performed, including all patients who were treated, from 2000 to 2013 by the senior author, for gynecomastia. A deidentified database was created to record patient characteristics, including age, height, weight, ptosis, stage of gynecomastia, and gynecomastia classification. Surgical approaches, complications, and revisions were also recorded. Our experience includes 75 patients with all grades of gynecomastia from 2000 to 2013. These cases span the evolution of our technique to include direct pull-through excision with ultrasound-assisted liposuction. The distribution of the grades I, II, III, and IV ptosis was 30.6%, 36 %, 22.6%, and 10.6% respectively. There were no complications in this series. Only one patient with grade III ptosis required revision surgery. This technique provides a safe and aesthetically pleasing way to treat gynecomastia with a low need for revision.
Gynecomastia is a benign proliferation of male breast glandular tissue, which may present as unilateral or bilateral. Its prevalence ranges from 90% in neonates1 to 50% to 70% in adolescents and elderly men.2–9 The diagnosis can typically be made with a careful history and physical exam. The essential goals of this study are to differentiate gynecomastia from cancer.
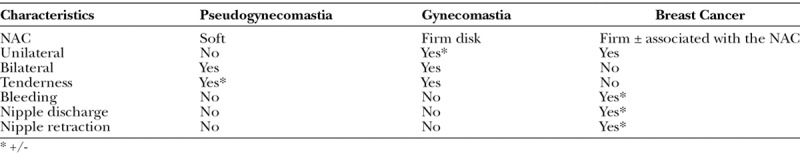
The first step is to determine on physical examination if the enlarged breast tissue is carcinoma. Breast carcinoma is typically unilateral, firm, nontender and may be located either behind or outside of the nipple areola complex (NAC). Additionally, cancer may have concomitant skin dimpling, nipple retraction, and nipple discharge or bleeding. In contrast, gynecomastia and pseudogynecomastia are typically bilateral, not hard, and are in line with the NAC. Patients with gynecomastia will have a disk of fibrous tissue behind the NAC, which patients with pseudogynecomastia do not have10 (Table 1). If carcinoma cannot be ruled out on physical examination, imaging should be used10 and suspicious masses should be biopsied.11
Table 1.
Pseudogynecomastia Gynecomastia Breast Cancer
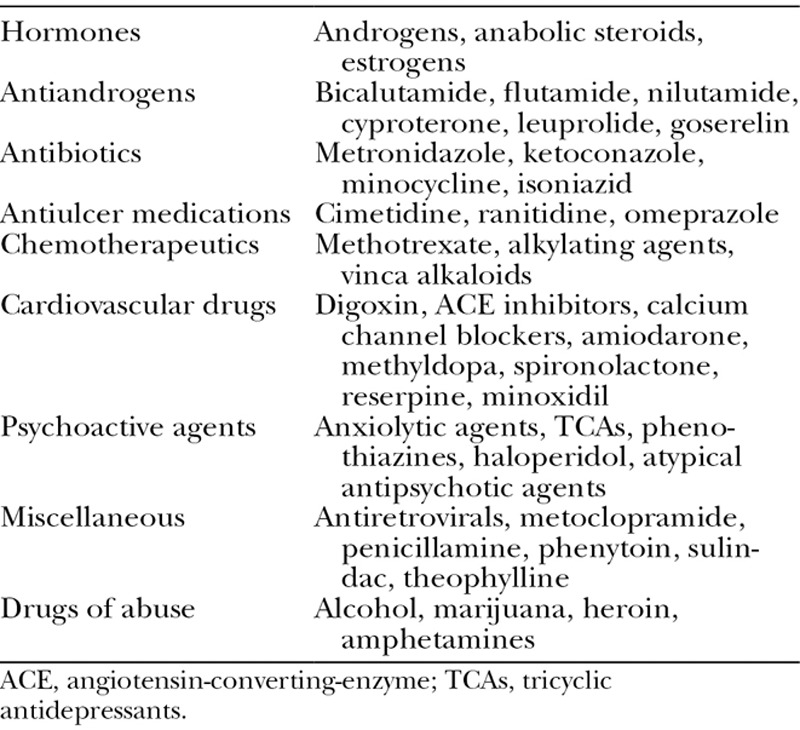
A myriad of medical treatment options are available to identify the type of gynecomastia (physiologic, pathologic, pharmacologic, and idiopathic) in proliferative phase (Tables 2 and 3). These treatments range from testosterone (in patients without hypogonadism), dihydrotestosterone, danazol, clomiphene citrate, testolactone, and raloxifene and tamoxifen.12,13 However, if gynecomastia is in its fibrous phase, or present for more than 1 year, it is unlikely to regress. In such circumstances, surgery is the best option for cosmetic improvement.
Table 2.
Categorization of Gynecomastia
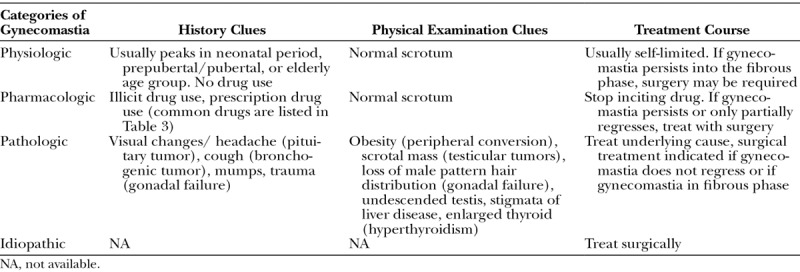
Table 3.
Drugs Associated with Gynecomastia
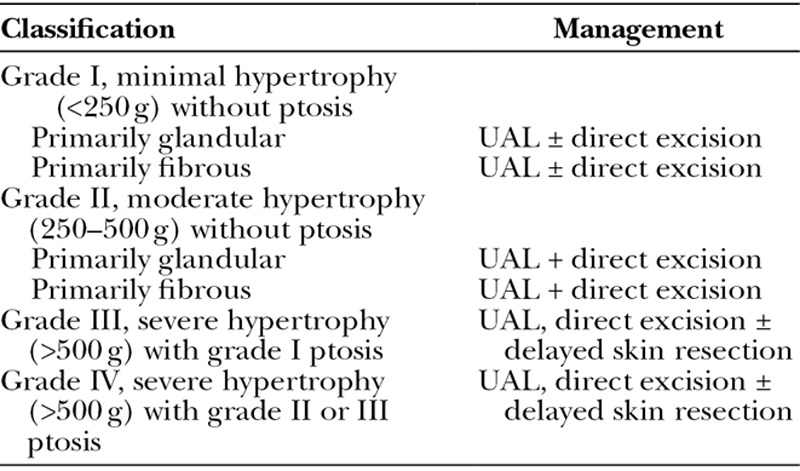
Surgical treatment historically has been subcutaneous mastectomy with or without direct skin incision, which was very successful at removing the subareolar fibrous disk but often left unacceptable scars. Rohrich et al14 introduced a step-wise approach employing a new classification system using ultrasound-assisted liposuction (UAL; Table 4).
Table 4.
Classification and Management of Gynecomastia
UAL has several advantages in the treatment of gynecomastia. UAL breaks up the dense fibroconnective tissue of the male breast more efficiently than suction-assisted lipectomy (SAL), and at higher energy settings, UAL has the capacity to remove the dense parenchymal tissue that SAL leaves behind.14 Additionally, UAL performed in the proper subdermal plane will affect the dermis, allowing for skin retraction in the postoperative period.15 The purpose of this study is to present the evolution of the technique developed by the senior author using the stage-based approach to treat gynecomastia. This will provide a safe graduated approach to achieve a cosmetically appealing result in patients with gynecomastia.
METHODS
Chart Review
A retrospective chart review was performed in accordance with the amended Declaration of Helsinki and was approved by the institutional review board at our institution. Patients with gynecomastia treated with the pull-through technique and UAL from 2000 to 2013 were reviewed. A de-identified database was created to record the patients’ characteristics including age, height, weight, ptosis, stage of gynecomastia, and gynecomastia classification. Surgical approaches, complications, and revisions were also recorded.
Surgical Technique: UAL and Pull-Through Excision Technique
Markings are made in the preoperative holding area with the patient sitting. The inframammary fold is marked. The adherent zones in the upper outer quadrants are marked to be avoided. The areas of excess tissue around and behind the nipple are also marked (Fig. 1). The patients are given general anesthesia and positioned supine with the arms abducted. A small 3- to 4-mm stab incision is made in the lateral inframammary fold and infiltrations of wetting solution performed in the “superwet” fashion (a 1:1 ratio of infiltrate to estimated aspirate; See video, Supplemental Digital Content 1, which demonstrates infiltrations of wetting solution performed in the “superwet” fashion (a 1:1 ratio of infiltrate to estimated aspirate, http://links.lww.com/PRSGO/A220). The wetting solution contains 1 ampoule of 1:1,000 epinephrine and 30 mL of 1% xylocaine in 1 L of lactated Ringer solution.
Fig. 1.
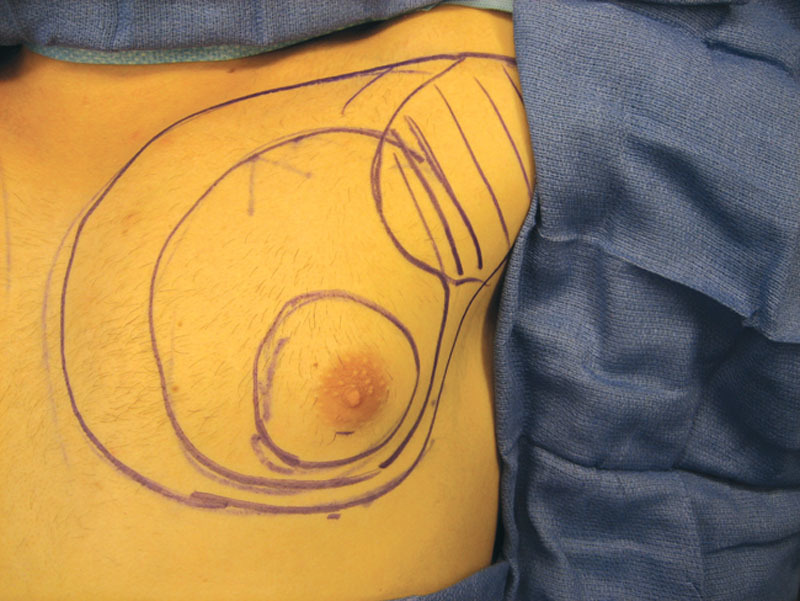
The inframammary fold and the areas of excess tissue around and behind the nipple are also marked along with the adherent zones in the upper outer quadrants.
UAL is performed with an ultrasound generator, a 5-mm blunt-tip cannula or a 4-mm golf-tee cannula, and a surgical aspirator for evacuation (See video, Supplemental Digital Content 2, which demonstrates an UAL performed with an ultrasound generator, a 5-mm blunt-tip cannula or a 4-mm golf-tee cannula, and a surgical aspirator for evacuation, http://links.lww.com/PRSGO/A221). Lysonix (Byron Medical, Carpinteria, Calif.) generators have energy levels set between 6 and 8. Aspirate volume and time of application are recorded. Constant, deliberate passes of the cannula are made through the intermediate fat layer in a radial pattern. Next, a bimanual technique using the nondominant hand guides the cannula through the subdermal layer. This addresses the dense fibrous tissue and allows for skin retraction. The periphery is feathered and the inframammary fold disrupted. This allows excess skin to re-drape and create a more gradual transition of the breast to the abdomen. The adherent zone marked preoperatively is suctioned minimally, if at all. SAL is then performed using a 3.7-mm cannula for evacuation and final contouring (See video, Supplemental Digital Content 3, which demonstrates an SAL performed using a 3.7-mm cannula for evacuation and final contouring, http://links.lww.com/PRSGO/A222). SAL proceeds from the deep to intermediate layer until endpoints are reached.
After evacuation is complete, a Kocher clamp is introduced through the stab incision (Fig. 2) and the residual subareolar dense tissue is grasped with a clamp (Fig. 3) pulled through the incision, and directly excised (Fig. 4). Once the appropriate contour is achieved, the lateral inframammary incisions are closed with a single 5-0 plain gut suture.
Fig. 2.

A Kocher clamp is introduced through the stab incision.
Fig. 3.

The residual subareolar dense tissue is grasped with a clamp.
Fig. 4.

The residual subareolar dense tissue is pulled through the incision and directly excised.
The chest wall is dressed with an abdominal pad and a double layer of topifoam (Fig. 5), and a compressive vest is worn for 4 weeks continuously followed by 4 weeks of nighttime wear only.
Fig. 5.
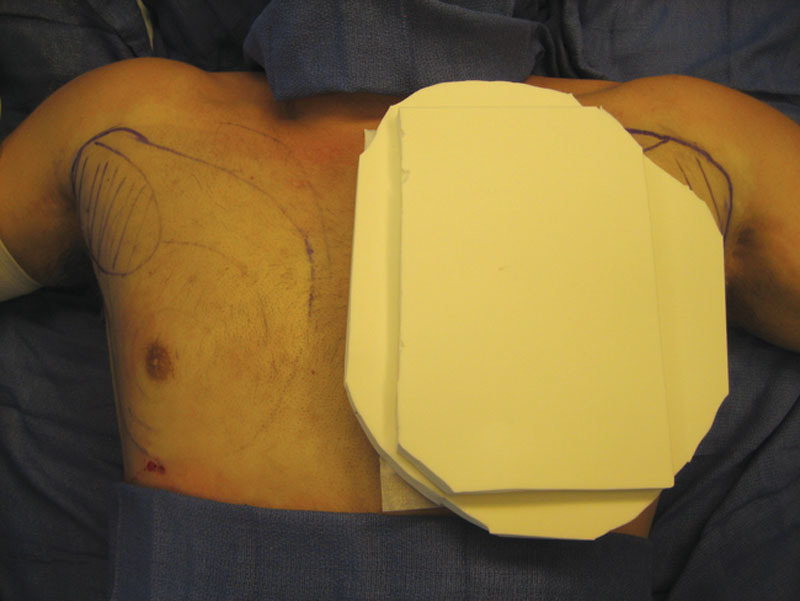
The chest wall is dressed with an abdominal pad and a double layer of topifoam.
RESULTS
Our experience includes 75 patients with all grades of gynecomastia from 2000 to 2013. These cases span the evolution of our technique to include direct pull-through excision with UAL.
As stated previously, patients with all grades of gynecomastia were included. The specific distribution is as follows: 23 (30.6%) with grade I, 27 (36 %) with grade II, 17 (22.6%) with grade III, and 8 (10.6%) with grade IV.
There were no complications in this series. Only one patient required revision surgery. He initially presented with grade III gynecomastia and required a return to the operating room for minor subareolar UAL suction and direct periareolar excision to obtain an optimum result.
DISCUSSION
The understanding of the etiology and pathophysiology of gynecomastia continues to slowly expand. Diagnostic algorithms have been developed to increase the efficiency and limit the use of unnecessary and costly diagnostic studies in select patient subgroups. Despite the advances in medical treatment of gynecomastia,10–12 surgery still remains the only effective treatment for patients with fibrous gynecomastia.
The senior author’s classification system for the surgical treatment of gynecomastia is based on the amount and character of the hypertrophied breast tissue and the degree of ptosis Table 4.14 The initial report of 61 patients treated from 1987 to 2000 demonstrated that UAL was effective for all grades. No further treatment was needed for patients with grade I or II gynecomastia. Forty-two percent of patients with grade III or IV gynecomastia required staged excision of remaining breast tissue and skin to obtain optimum results. As originally designed in the algorithm, if removal of redundant skin and/or resistant breast tissue was still required after UAL, a stage excision was planned for 6 to 9 months.14,16,17 This was to allow for maximal skin retraction and healing so that the magnitude of the eventual excision was minimized.
Since this publication, UAL has become widely accepted as the treatment for gynecomastia.17–19 Recently, however, there have been reports of combining UAL and subareolar excision techniques within the same setting. Excision techniques have included direct excision, “pull through” from small incisions, and the use of cartilage shavers.16,17,20–24 There have also been recent reports of laser-assisted liposuction to treat gynecomastia, but the experience remains limited and its utility continues to be defined.25–27 The evolution of our technique has paralleled these advances.11,14–16,18,20–22,24,28–85
The recent experience from our institution includes 75 patients treated simultaneously with UAL and direct excision with no complications and a single re-operation. This has demonstrated that this technique can be safely accomplished with good results. This represents an evolution from the original treatment algorithm of staging direct excision of 6 to 9 months after UAL. Furthermore, our results are in agreement with that of similar techniques combining liposuction with direct excision by other groups. Hammond et al16 reported treating 15 patients with no long-term complications and no re-operations. Lista and Ahmad20 reported treating 96 patients with 1.0% complications (2 seromas) and no revisions.
UAL provides the advantages of minimal scarring and efficient removal of both glandular and fibrotic breast tissue. A considerable amount of skin retraction is seen in patients with grade III and IV gynecomastia, often obviating the need for additional procedures to remove excess skin. Although not necessary for the majority of patients in our cohort, if residual skin excess necessitates additional tailoring with mastopexy techniques, we recommend the procedure be performed in a delayed fashion at 6 to 9 months. By delaying excision, the NAC is able to revascularize via a central pedicle, thereby allowing incision and mild undermining of surrounding breast flaps.
With these additional findings regarding the surgical management of gynecomastia, we still advocate grade-directed treatment, but have updated our treatment algorithm to include simultaneous UAL and direct excision via the pull-though technique obviating the need for a periareolar incision. The only exception and a contraindication for this technique is a patient with Klinefelter syndrome. These patients have a 60× greater risk of developing breast cancer (1:400 to 1:1,000) and thus should have a mastectomy to allow for complete removal and complete pathologic evaluation.
CONCLUSIONS
The evaluation of gynecomastia can be complex, but a step-wise approach that starts with careful history taking and physical examination simplifies the process. Extensive laboratory testing and diagnostic imaging may be avoided in certain subgroups. Although medical therapies have been shown to be effective in new-onset florid gynecomastia, the treatment of chronic fibrous gynecomastia remains surgical. Evolution of the treatment of gynecomastia to include liposuction and direct subareolar pull-through excision is a safe and effective treatment for the vast majority of patients with gynecomastia. Minimally invasive techniques through minimal incisions offer fast recovery, low complication rates, excellent cosmesis, and high tolerance.
Video Graphic 1.

See video, Supplemental Digital Content 1, which demonstrates infiltrations of wetting solution performed in the “superwet” fashion (a 1:1 ratio of infiltrate to estimated aspirate), http://links.lww.com/PRSGO/A220.
Video Graphic 2.

See video, Supplemental Digital Content 2, which demonstrates a UAL performed with an ultrasound generator, a 5-mm blunt-tip cannula or a 4-mm golf-tee cannula, and a surgical aspirator for evacuation, http://links.lww.com/PRSGO/A221.
Video Graphic 3.

See video, Supplemental Digital Content 3, which demonstrates an SAL performed using a 3.7-mm cannula for evacuation and final contouring, http://links.lww.com/PRSGO/A222.
Supplementary Material
Footnotes
Disclosure: Rod J. Rohrich, MD is a volunteer member of the Allergan Alliance for the Future of Aesthetics and receives instrument royalties from Eriem Surgical, Inc and book royalties from Taylor and Francis Publishing. The other authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.McKiernan JF, Hull D. Breast development in the newborn. Arch Dis Child. 1981;56:525–529. doi: 10.1136/adc.56.7.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nydick M, Bustos J, Dale JH, Jr, et al. Gynecomastia in adolescent boys. JAMA. 1961;178:449–454. doi: 10.1001/jama.1961.03040440001001. [DOI] [PubMed] [Google Scholar]
- 3.Sher ES, Migeon CJ, Berkovitz GD. Evaluation of boys with marked breast development at puberty. Clin Pediatr (Phila) 1998;37:367–371. doi: 10.1177/000992289803700606. [DOI] [PubMed] [Google Scholar]
- 4.Nuttall FQ. Gynecomastia as a physical finding in normal men. J Clin Endocrinol Metab. 1979;48:338–340. doi: 10.1210/jcem-48-2-338. [DOI] [PubMed] [Google Scholar]
- 5.Ley SJ. Cardiac surgery in an era of antiplatelet therapies: generating new evidence. Reflect Nurs Leadersh. 2002;28:35. [PubMed] [Google Scholar]
- 6.Carlson HE. Gynecomastia. N Engl J Med. 1980;303:795–799. doi: 10.1056/NEJM198010023031405. [DOI] [PubMed] [Google Scholar]
- 7.Niewoehner CB, Nuttal FQ. Gynecomastia in a hospitalized male population. Am J Med. 1984;77:633–638. doi: 10.1016/0002-9343(84)90353-x. [DOI] [PubMed] [Google Scholar]
- 8.Georgiadis E, Papandreou L, Evangelopoulou C, et al. Incidence of gynaecomastia in 954 young males and its relationship to somatometric parameters. Ann Hum Biol. 1994;21:579–587. doi: 10.1080/03014469400003582. [DOI] [PubMed] [Google Scholar]
- 9.Williams MJ. Gynecomastia. Its incidence, recognition and host characterization in 447 autopsy cases. Am J Med. 1963;34:103–112. doi: 10.1016/0002-9343(63)90044-5. [DOI] [PubMed] [Google Scholar]
- 10.Braunstein GD. Gynecomastia. N Engl J Med. 2007;357:1229–1237. doi: 10.1056/NEJMcp070677. [DOI] [PubMed] [Google Scholar]
- 11.Deepinder F, Braunstein GD. Gynecomastia: incidence, causes and treatment. Expert Rev Endocrinol Metabol. 2011;6:723–730. doi: 10.1586/eem.11.57. [DOI] [PubMed] [Google Scholar]
- 12.Alagaratnam TT. Idiopathic gynecomastia treated with tamoxifen: a preliminary report. Clin Ther. 1987;9:483–487. [PubMed] [Google Scholar]
- 13.Khan HN, Rampaul R, Blamey RW. Management of physiological gynaecomastia with tamoxifen. Breast. 2004;13:61–65. doi: 10.1016/j.breast.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Rohrich RJ, Ha RY, Kenkel JM, et al. Classification and management of gynecomastia: defining the role of ultrasound-assisted liposuction. Plast Reconstr Surg. 2003;111:909–923. doi: 10.1097/01.PRS.0000042146.40379.25. discussion 924–925. [DOI] [PubMed] [Google Scholar]
- 15.Rohrich RJ, Beran SJ, Kenkel JM, et al. Extending the role of liposuction in body contouring with ultrasound-assisted liposuction. Plast Reconstr Surg. 1998;101:1090–1102. doi: 10.1097/00006534-199804040-00033. discussion 1117. [DOI] [PubMed] [Google Scholar]
- 16.Hammond DC. Surgical correction of gynecomastia. Plast Reconstr Surg. 2009;124:61e–68e. doi: 10.1097/PRS.0b013e3181aa2dc7. [DOI] [PubMed] [Google Scholar]
- 17.Petty PM, Solomon M, Buchel EW, et al. Gynecomastia: evolving paradigm of management and comparison of techniques. Plast Reconstr Surg. 2010;125:1301–1308. doi: 10.1097/PRS.0b013e3181d62962. [DOI] [PubMed] [Google Scholar]
- 18.Hodgson EL, Fruhstorfer BH, Malata CM. Ultrasonic liposuction in the treatment of gynecomastia. Plast Reconstr Surg. 2005;116:646–653. doi: 10.1097/01.prs.0000173441.57812.e8. discussion 654. [DOI] [PubMed] [Google Scholar]
- 19.Ratnam BV. A new classification and treatment protocol for gynecomastia. Aesthet Surg J. 2009;29:26–31. doi: 10.1016/j.asj.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 20.Lista F, Ahmad J. Power-assisted liposuction and the pull-through technique for the treatment of gynecomastia. Plast Reconstr Surg. 2008;121:740–747. doi: 10.1097/01.prs.0000299907.04502.2f. [DOI] [PubMed] [Google Scholar]
- 21.Benito-Ruiz J, Raigosa M, Manzano M, et al. Assessment of a suction-assisted cartilage shaver plus liposuction for the treatment of gynecomastia. Aesthet Surg J. 2009;29:302–309. doi: 10.1016/j.asj.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 22.Prado AC, Castillo PF. Minimal surgical access to treat gynecomastia with the use of a power-assisted arthroscopic-endoscopic cartilage shaver. Plast Reconstr Surg. 2005;115:939–942. doi: 10.1097/01.prs.0000153237.35202.7d. [DOI] [PubMed] [Google Scholar]
- 23.Ramon Y, Fodor L, Peled IJ, et al. Multimodality gynecomastia repair by cross-chest power-assisted superficial liposuction combined with endoscopic-assisted pull-through excision. Ann Plast Surg. 2005;55:591–594. doi: 10.1097/01.sap.0000189664.88464.34. [DOI] [PubMed] [Google Scholar]
- 24.Bracaglia R, Fortunato R, Gentileschi S, et al. Our experience with the so-called pull-through technique combined with liposuction for management of gynecomastia. Ann Plast Surg. 2004;53:22–26. doi: 10.1097/01.sap.0000106429.37110.cf. [DOI] [PubMed] [Google Scholar]
- 25.Apfelberg DB, Rosenthal S, Hunstad JP, et al. Progress report on multicenter study of laser-assisted liposuction. Aesthetic Plast Surg. 1994;18:259–264. doi: 10.1007/BF00449791. [DOI] [PubMed] [Google Scholar]
- 26.Wollina U, Goldman A, Berger U, et al. Esthetic and cosmetic dermatology. Dermatol Ther. 2008;21:118–130. doi: 10.1111/j.1529-8019.2008.00179.x. [DOI] [PubMed] [Google Scholar]
- 27.Goldman A, Wollina U. Subdermal Nd-YAG laser for axillary hyperhidrosis. Dermatologic Surg. 2008;34:756–762. doi: 10.1111/j.1524-4725.2008.34143.x. [DOI] [PubMed] [Google Scholar]
- 28.Webster JP. Mastectomy for gynecomastia through a semicircular intra-areolar incision. Ann Surg. 1946;124:557–575. [PubMed] [Google Scholar]
- 29.Lynch RC. An operation for correction of gynecomastia through an areolar incision. Plast Reconstr Surg (1946) 1954;13:412–418. doi: 10.1097/00006534-195405000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Giacobine JW, Searle NB. Management of gynecomastia. Am J Surg. 1961;102:395–402. doi: 10.1016/0002-9610(61)90529-3. [DOI] [PubMed] [Google Scholar]
- 31.Von Kessel F, Pickrell KL, Huger WE, et al. Surgical treatment of gynecomastia: an analysis of 275 cases. Ann Surg. 1963;157:142–151. doi: 10.1097/00000658-196301000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pitanguy I. Transareolar incision for gynecomastia. Plast Reconstr Surg. 1966;38:414–419. doi: 10.1097/00006534-196611000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Letterman G, Schurter M. The surgical correction of gynecomastia. Am Surg. 1969;35:322–325. [PubMed] [Google Scholar]
- 34.Letterman G, Schurter M. Surgical correction of massive gynecomastia. Plast Reconstr Surg. 1972;49:259–262. doi: 10.1097/00006534-197203000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Simon BE, Hoffman S, Kahn S. Classification and surgical correction of gynecomastia. Plast Reconstr Surg. 1973;51:48–52. doi: 10.1097/00006534-197301000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Wray RC, Jr, Hoopes JE, Davis GM. Correction of extreme gynaecomastia. Br J Plast Surg. 1974;27:39–41. doi: 10.1016/0007-1226(74)90060-5. [DOI] [PubMed] [Google Scholar]
- 37.Eade GG. The radial incision for gynecomastia excisions. Plast Reconstr Surg. 1974;54:495–497. doi: 10.1097/00006534-197410000-00023. [DOI] [PubMed] [Google Scholar]
- 38.Bretteville-Jensen G. Surgical treatment of gynaecomastia. Br J Plast Surg. 1975;28:177–180. doi: 10.1016/0007-1226(75)90125-3. [DOI] [PubMed] [Google Scholar]
- 39.Artz S, Lehman JA., Jr. Surgical correction of massive gynecomastia. Arch Surg. 1978;113:199–201. doi: 10.1001/archsurg.1978.01370140089019. [DOI] [PubMed] [Google Scholar]
- 40.Balch CR. A transaxillary incision for gynecomastia. Plast Reconstr Surg. 1978;61:13–16. doi: 10.1097/00006534-197801000-00003. [DOI] [PubMed] [Google Scholar]
- 41.Davidson BA. Concentric circle operation for massive gynecomastia to excise the redundant skin. Plast Reconstr Surg. 1979;63:350–354. doi: 10.1097/00006534-197903000-00009. [DOI] [PubMed] [Google Scholar]
- 42.Huang TT, Hidalgo JE, Lewis SR. A circumareolar approach in surgical management of gynecomastia. Plast Reconstr Surg. 1982;69:35–40. [PubMed] [Google Scholar]
- 43.Welsh F. Handlebar moustache breast reduction. Plast Reconstr Surg. 1982;69:544–546. doi: 10.1097/00006534-198203000-00027. [DOI] [PubMed] [Google Scholar]
- 44.Teimourian B, Perlman R. Surgery for gynecomastia. Aesthetic Plast Surg. 1983;7:155–157. doi: 10.1007/BF01571338. [DOI] [PubMed] [Google Scholar]
- 45.Lewis CM. Lipoplasty: treatment for gynecomastia. Aesthetic Plast Surg. 1985;9:287–292. doi: 10.1007/BF01571048. [DOI] [PubMed] [Google Scholar]
- 46.Courtiss EH. Gynecomastia: analysis of 159 patients and current recommendations for treatment. Plast Reconstr Surg. 1987;79:740–753. doi: 10.1097/00006534-198705000-00010. [DOI] [PubMed] [Google Scholar]
- 47.Freiberg A, Hong C. Apple-coring technique for severe gynecomastia. Can J Surg. 1987;30:57–60. [PubMed] [Google Scholar]
- 48.Rosenberg GJ. Gynecomastia: suction lipectomy as a contemporary solution. Plast Reconstr Surg. 1987;80:379–386. [PubMed] [Google Scholar]
- 49.Abramo AC, Viola JC. Liposuction through an axillary incision for treatment of gynecomastia. Aesthetic Plast Surg. 1989;13:85–89. doi: 10.1007/BF01571474. [DOI] [PubMed] [Google Scholar]
- 50.Abramo AC. Axillary approach for gynecomastia liposuction. Aesthetic Plast Surg. 1994;18:265–268. doi: 10.1007/BF00449792. [DOI] [PubMed] [Google Scholar]
- 51.Aiache AE. Surgical treatment of gynecomastia in the body builder. Plast Reconstr Surg. 1989;83:61–66. doi: 10.1097/00006534-198901000-00011. [DOI] [PubMed] [Google Scholar]
- 52.Ward CM, Khalid K. Surgical treatment of grade III gynaecomastia. Ann R Coll Surg Engl. 1989;71:226–228. [PMC free article] [PubMed] [Google Scholar]
- 53.Becker H. The treatment of gynecomastia without sharp excision. Ann Plast Surg. 1990;24:380–383. doi: 10.1097/00000637-199004000-00015. [DOI] [PubMed] [Google Scholar]
- 54.Mladick RA. Gynecomastia. Liposuction and excision. Clin Plast Surg. 1991;18:815–822. [PubMed] [Google Scholar]
- 55.Rigg BM. Morselization suction: a modified technique for gynecomastia. Plast Reconstr Surg. 1991;88:159–160. [PubMed] [Google Scholar]
- 56.Brenner P, Berger A, Schneider W, et al. Male reduction mammoplasty in serious gynecomastias. Aesthetic Plast Surg. 1992;16:325–330. doi: 10.1007/BF01570695. [DOI] [PubMed] [Google Scholar]
- 57.Samdal F, Kleppe G, Amland PF, et al. Surgical treatment of gynaecomastia. Five years’ experience with liposuction. Scand J Plast Reconstr Surg Hand Surg. 1994;28:123–130. doi: 10.3109/02844319409071189. [DOI] [PubMed] [Google Scholar]
- 58.Kornstein AN, Cinelli PB. Inferior pedicle reduction technique for larger forms of gynecomastia. Aesthetic Plast Surg. 1992;16:331–335. doi: 10.1007/BF01570696. [DOI] [PubMed] [Google Scholar]
- 59.Stark GB, Grandel S, Spilker G. Tissue suction of the male and female breast. Aesthetic Plast Surg. 1992;16:317–324. doi: 10.1007/BF01570694. [DOI] [PubMed] [Google Scholar]
- 60.Murphy TP, Ehrlichman RJ, Seckel BR. Nipple placement in simple mastectomy with free nipple grafting for severe gynecomastia. Plast Reconstr Surg. 1994;94:818–823. doi: 10.1097/00006534-199411000-00010. [DOI] [PubMed] [Google Scholar]
- 61.Reyes RJ, Zicchi S, Hamed H, et al. Surgical correction of gynaecomastia in bodybuilders. Br J Clin Pract. 1995;49:177–179. [PubMed] [Google Scholar]
- 62.Rosenberg GJ. A new cannula for suction removal of parenchymal tissue of gynecomastia. Plast Reconstr Surg. 1994;94:548–551. doi: 10.1097/00006534-199409000-00023. [DOI] [PubMed] [Google Scholar]
- 63.Morselli PG. “Pull-through”: a new technique for breast reduction in gynecomastia. Plast Reconstr Surg. 1996;97:450–454. doi: 10.1097/00006534-199602000-00028. [DOI] [PubMed] [Google Scholar]
- 64.Botta SA. Alternatives for the surgical correction of severe gynecomastia. Aesthetic Plast Surg. 1998;22:65–70. doi: 10.1007/s002669900168. [DOI] [PubMed] [Google Scholar]
- 65.Colombo-Benkmann M, Buse B, Stern J, et al. [Surgical therapy of gynecomastia and its results]. Langenbecks Arch Chir Suppl Kongressbd. 1998;115:1282–1284. [PubMed] [Google Scholar]
- 66.Hamas RS, Williams CW. A sharp cutting liposuction cannula for gynecomastia. Aesthet Surg J. 1998;18:261–265. doi: 10.1016/s1090-820x(98)70054-8. [DOI] [PubMed] [Google Scholar]
- 67.Gingrass MK, Shermak MA. The treatment of gynecomastia with ultrasound-assisted lipoplasty. Semin Plast Surg. 1999;12:101–112. [Google Scholar]
- 68.Ohyama T, Takada A, Fujikawa M, et al. Endoscope-assisted transaxillary removal of glandular tissue in gynecomastia. Ann Plast Surg. 1998;40:62–64. doi: 10.1097/00000637-199801000-00013. [DOI] [PubMed] [Google Scholar]
- 69.Peters MH, Vastine V, Knox L, et al. Treatment of adolescent gynecomastia using a bipedicle technique. Ann Plast Surg. 1998;40:241–245. doi: 10.1097/00000637-199803000-00008. [DOI] [PubMed] [Google Scholar]
- 70.Smoot EC. Eccentric skin resection and purse-string closure for skin reduction with mastectomy for gynecomastia. Ann Plast Surg. 1998;41:378–383. doi: 10.1097/00000637-199810000-00005. [DOI] [PubMed] [Google Scholar]
- 71.Park AJ, Lamberty BG. Gynaecomastia: have Webster’s lessons been ignored? J R Coll Surg Edinb. 1998;43:89–92. [PubMed] [Google Scholar]
- 72.Chiu DT, Siegel HW. The pinwheel technique: an adjunct to the periareolar approach in gynecomastia resection. Ann Plast Surg. 1999;42:465–469. [PubMed] [Google Scholar]
- 73.Gasperoni C, Salgarello M, Gasperoni P. Technical refinements in the surgical treatment of gynecomastia. Ann Plast Surg. 2000;44:455–458. doi: 10.1097/00000637-200044040-00020. [DOI] [PubMed] [Google Scholar]
- 74.Ersek RA, Schaeferele M, Beckham PH, et al. Gynecomastia: a clinical review. Aesthet Surg J. 2000;20:381–386. [Google Scholar]
- 75.Persichetti P, Berloco M, Casadei RM, et al. Gynecomastia and the complete circumareolar approach in the surgical management of skin redundancy. Plast Reconstr Surg. 2001;107:948–954. doi: 10.1097/00006534-200104010-00007. [DOI] [PubMed] [Google Scholar]
- 76.Steele SR, Martin MJ, Place RJ. Gynecomastia: complications of the subcutaneous mastectomy. Am Surg. 2002;68:210–213. [PubMed] [Google Scholar]
- 77.Fruhstorfer BH, Malata CM. A systematic approach to the surgical treatment of gynaecomastia. Br J Plast Surg. 2003;56:237–246. doi: 10.1016/s0007-1226(03)00111-5. [DOI] [PubMed] [Google Scholar]
- 78.Wiesman IM, Lehman JA, Jr, Parker MG, et al. Gynecomastia: an outcome analysis. Ann Plast Surg. 2004;53:97–101. doi: 10.1097/01.sap.0000116256.01831.17. [DOI] [PubMed] [Google Scholar]
- 79.Walden JL, Schmid RP, Blackwell SJ. Cross-chest lipoplasty and surgical excision for gynecomastia: a 10-year experience. Aesthet Surg J. 2004;24:216–223. doi: 10.1016/j.asj.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 80.Babigian A, Silverman RT. Management of gynecomastia due to use of anabolic steroids in bodybuilders. Plast Reconstr Surg. 2001;107:240–242. doi: 10.1097/00006534-200101000-00039. [DOI] [PubMed] [Google Scholar]
- 81.Mladick RA. Continuing education: gynecomastia. Aesthet Surg J. 2004;24:471–479. doi: 10.1016/j.asj.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 82.Durani P, McCulley SJ. Transareolar and H-incisions for the surgical treatment of gynecomastia. Plast Reconstr Surg. 2007;119:1387–1388. doi: 10.1097/01.prs.0000255192.55526.e5. [DOI] [PubMed] [Google Scholar]
- 83.Haddad Filho D, Arruda RG, Alonso N. Treatment of severe gynecomastia (grade III) by resection of periareolar skin. Aesthet Surg J. 2006;26:669–673. doi: 10.1016/j.asj.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 84.Ratnam BV. A new classification and treatment protocol for gynecomastia. Aesthet Surg J. 2009;29:26–31. doi: 10.1016/j.asj.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 85.Prado AS, Castillo P. Gynecomastia: evolving paradigm of management and comparison of techniques. Plast Reconstr Surg. 2010;126:2291–2292. doi: 10.1097/PRS.0b013e3181f61b91. author reply 2292. [DOI] [PubMed] [Google Scholar]


