Abstract
Background:
Facial burns represent between one-fourth and one-third of all burns. The long-term sequelae of periorbital burns include significant ectropion and lagophthalmos as a result of secondary burn contractures in the lower and upper eyelids, in addition to complete or incomplete alopecia of the eyebrows.
Methods:
A retrospective study of 14 reconstructive procedures for 12 postburn faces was conducted with all procedures performed since 2010 at the Department of Plastic Surgery, Al-Hussein University Hospital, and at the Craniofacial Unit, Nasser Institute Hospital. Four patients experienced chemical burns, and 8 patients experienced thermal burns. All patients underwent periorbital reconstruction using a bifurcated superficial temporal artery island flap to reconstruct the eyebrows, correct the lagophthalmos, and release the ectropion in both the upper and the lower eyelids. Two patients underwent bilateral periorbital flap reconstruction. The mean age of patients was 29 years, and the study was conducted on 8 males and 4 females. Patient satisfaction was assessed using a questionnaire completed by all patients postoperatively.
Results:
The complete release of both the upper and the lower eyelids was achieved in all cases, together with ideal replacement of brow hair; no complications were noted, apart from one case in which a loss of hair density in the new eyebrow was observed, combined with the partial loss of the flap in the lower eyelid. Patient satisfaction results were collected and assembled in a table.
Conclusion:
A bifurcated superficial temporal artery island flap is an innovative flap for reconstructing both burned eyebrows and eyelids.
Periorbital burns are considered a challenging problem of an important aesthetic unit of the face.1 Periorbital burns can result in excessive cicatricial healing and the distortion of soft tissue around the eye, which may result in eyelid distortion, scleral show, and/or loss of an eyebrow.2
Traditional problem solving includes skin grafts or moving the local flaps up to free flap; however, none of these approaches can address the different anatomical areas of interest, and each patient should always be presented with multiple solutions.3 Since the introduction of temporoparietal fascia flap in 1898 by Golovine,4 in ear reconstruction, and by Monks,5 in lower eyelid reconstruction, the flap has widely been used in various reconstructive situations. In 1983, Gillies6 described the use of the pedicled scalp flap based on the superficial temporal artery for the reconstruction of lip and eyebrow defects. Following that, Ellis et al7 reported 2 patients on whom the flap was used for lower eyelid and malar reconstruction with success. In 2001, Juri8 described the usage of the island scalp flap based on the superficial temporal artery to reconstruct eyebrow alopecia either congenital or postburn. In this study, we present a single pertinent solution to address all problems in the periorbital area. By using 2 island flaps based on the superficial temporal artery, we replace burnt eyebrow hair and release the upper and lower eyelids with soft tissue not amenable to contraction.
ANATOMY
Our idea arose from an understanding of the anatomical art of the superficial temporal artery. Lie et al9 in their anatomical study showed that the superficial temporal artery divides into 2 major branches, the frontal and the parietal, either at a higher position or at a lower position in relation to the horizontal line of the superior orbital rim (Fig. 1).10 They observed that the temporal branch of facial nerve and its terminal branches were located in the area inferior to the frontal artery and ran deeper to the temporoparietal fascia in the high-location type (Fig. 2), while when the frontal artery was a low-location type, one or more terminal branches of the temporal nerve emerged superior or interweaved with the frontal artery in the region above the horizontal plane of the upper orbital rim.9 Therefore, special care should be taken to avoid nerve damage during dissection of the pedicle of the flap based on the frontal branch.7
Fig. 1.
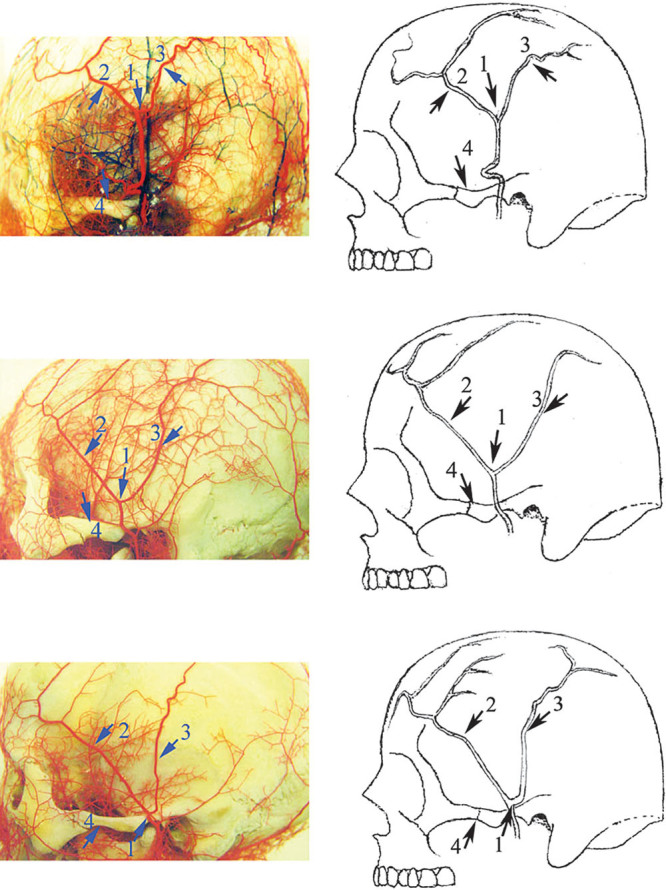
Illustrations of common branch patterns of the frontal branch of the superficial temporal artery. At the bifurcation point, 1, the superficial temporal artery divides into the anterior frontal branch, 2, and the posterior parietal branch, 3. The frontal branch can be classified as high-location type (64%) and low-location type (36%) based on its relationship to the horizontal line of the superior orbital rim. Eighty-four percent of the frontal branch originates at the level superior to the zygomatic arch, 4. The course of the main branch of the frontal branch can be classified as either linear or circuitous. As the bifurcation point rises, the inclination increases and the obliquely running frontal branch becomes horizontal. Reprinted with permission from Lei T, Xu DC, Gao JH, et al. Using the frontal branch of the superficial temporal artery as a landmark for locating the course of the temporal branch of the facial nerve during rhytidectomy: an anatomical study. Plast Reconstr Surg. 2005;116:623–629; discussion 630.
Fig. 2.
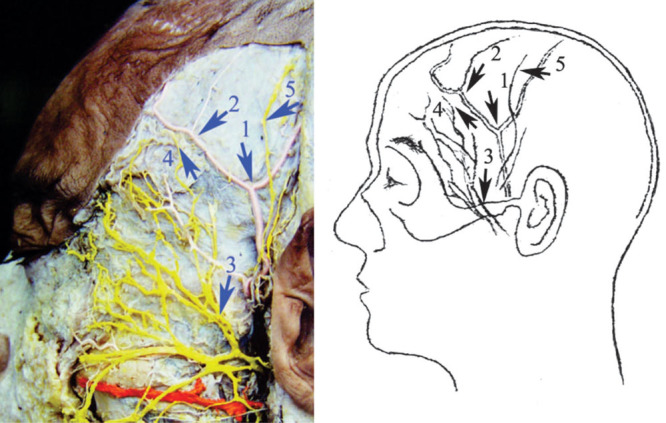
The temporal branch of the facial nerve (temporal branch) and its terminal branches distribute in the area inferior to the boundary of the frontal branch and run deeper to the frontal branch. 1, Bifurcation point of the superficial temporal artery; 2, frontal branch; 3, temporal branch of the facial nerve; 4, terminal branch of the temporal branch; 5, auricular temporal nerve. Reprinted with permission from Lei T, Xu DC, Gao JH, et al. Using the frontal branch of the superficial temporal artery as a landmark for locating the course of the temporal branch of the facial nerve during rhytidectomy: an anatomical study. Plast Reconstr Surg. 2005;116:623–629; discussion 630.
The frontal and parietal branches are similar in size. The mean diameters of the vessels are 2.14 mm for the superficial temporal artery, 1.61 mm for the frontal branch, and 1.68 mm for the parietal branch.11 Cadaver studies have shown that the position of the frontal branch is less variable than that of the parietal branch of the superficial temporal artery.13 Therefore, in our study, we determined the site of the parietal branch using palpation and Doppler ultrasound.
PATIENTS AND METHODS
A retrospective study was conducted involving 14 reconstructive procedures for 12 postburn faces with periorbital deformities in the form of alopecia in the eyebrow and severe ectropion in the lower and upper eyelids; all cases were operated on between January 2010 and December 2013 in the Department of Plastic Surgery, Al-Hussein University Hospital, Al-Azhar University, and in the Craniofacial Department, Nasser Institute. Four patients experienced chemical burns, and 8 patients experienced thermal burns. All were attended with the aim of reconstruction after having received their early treatment in a number of different hospitals. Some of the patients had received preventive therapy for hypertrophic scar, such as the application of pressure garments and/or silicone pads. All patients underwent periorbital reconstruction using a bifurcated superficial temporal artery island flap (BSTIF) to reconstruct the eyebrow and release ectropion in the upper and lower eyelids after proper preoperative assessment generally and locally. Two patients underwent bilateral flap reconstruction, and 10 patients underwent unilateral reconstruction. Mean follow-up time was 48 months. Table 1 presents the complete data of the patients. All patients signed a full and detailed consent, illustrating the steps of the operation, anesthesia methods, and medical photography.
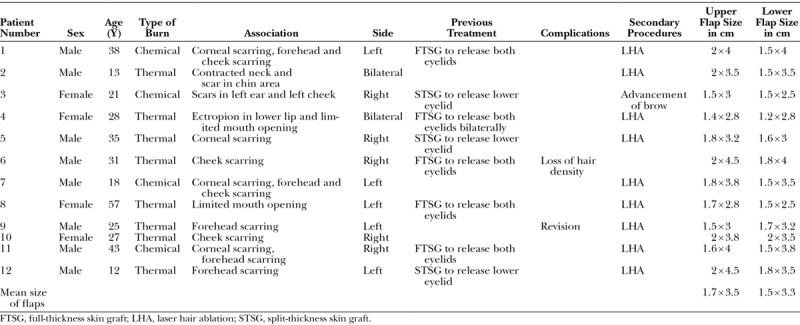
Table 1.
Complete Data of the Patients in the Study
A questionnaire was administered to assess patient satisfaction, and the points included the degree of satisfaction regarding the density and orientation of hairs, the symmetry with the other side, and the skin color match of the nonhairy flap. All patients in the study were asked to complete the questionnaire and to provide a score of 1 to 4 according to his/her degree of satisfaction. Then, the scores were summated from each questionnaire and scores rated as 16, excellent; 12–15, good; 8–11, fair; and 4–7, poor (Fig. 3).
Fig. 3.

Male patient, 13 years, single right eye with postburn scarring face and neck with severe bilateral periorbital cicatricial scarring. Lower lip ectropion and macrocheilia, late postoperative after bilateral BSTIF and microvascular radial forearm for the neck, and late postoperative with complete eye closure.
SURGICAL TECHNIQUE
At first, the release incision is designed to advance all possible tissues to be equal to or a part of the normal vertical length of the upper eyelid (Fig. 4A); after the full release, the transverse length of the parietal flap is positioned at the ideal position of the eyebrow to be refined later by laser hair ablation. Next, complete release of the lower eyelid is obtained with a subciliary incision. The superficial temporal artery and its branches are identified by digital palpation facilitated by Doppler ultrasound. The course of vessels is mapped and marked before incision. The 2 skin islands are designed to be located over the temporal area of the scalp and over the lateral aspect of the forehead along the temporal hairline (Fig. 4B). We have named the anterior island flap as the frontal flap (hairy or nonhairy), based on the frontal branch, and the parietal flap as the posterior flap (hairy flap), based on the parietal branch. The skin incision begins a few millimeters anterior to the tragus and extends upward after the course of the artery. A Y-shaped incision is made in the temporal region extending to the proximal part of both islands, and the superficial temporal artery and its branches are easily identified at this point and exposed. Then, the skin island borders are incised, and flap elevation proceeds from distal to proximal. Care should be taken to avoid injury of the pedicle where it enters the flap. The flap with its pedicle is then dissected to the level of the tragus to achieve an adequate arc of rotation for the flap (Fig. 4C, D). The 2 flaps are separated distally to proximally by direct vision in indirect illumination up to the level of the bifurcation (Fig. 5A). A wide subcutaneous tunnel between the flap and the recipient sites is dissected, and the flaps are transferred and sutured to the edges of the defective skin (Fig. 5B). A drain is placed, and the wound is closed in a single layer with nylon sutures and direct skin closure in all cases. Tips for harvesting the flap include taking care of hair follicles with preservation of thin layer of subcutaneous tissue deeper to hair follicles to avoid donor site alopecia. Incisions should be located away from arterial course and on anterior hair line. A wide tunnel is necessary to avoid congestion and a little bit of scalp subgaleal dissection to close the defect primarily.
Fig. 4.

A–D, After full release of the upper and lower eyelids, the defect was centered to occupy the future ideal position of the eyebrow; skin incision of the preplanned frontal and temporal flaps centered on the frontal and temporal branches, respectively; and complete elevation of the flap. A black line represents main artery, frontal branch and temporal branch.
Fig. 5.
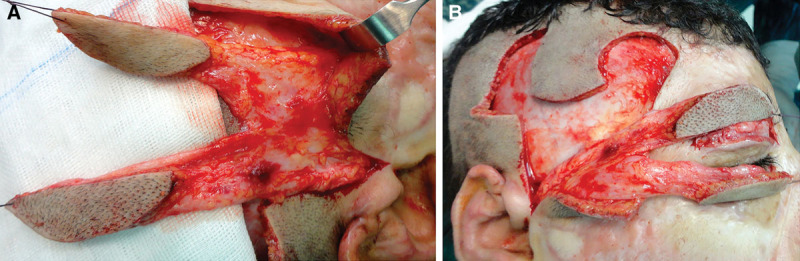
A and B, Separation of the flap under indirect illumination into frontal and temporal flaps, then insetting of the flaps to ensure that they cover both defects.
RESULTS
Over a period of 5 years, 12 patients (4 females and 8 males) were included in this study. Four patients experienced chemical burns, and 8 patients experienced thermal burns. All patients presented with the same criteria for periorbital reconstruction using a BSTIF to reconstruct their eyebrows and to release ectropion in their upper and lower eyelids. Two patients underwent bilateral flap reconstruction, and 10 patients underwent unilateral reconstruction; there were no flap failures and no postoperative infections. Two eyebrows of patients underwent surgical refinement, with one receiving scar revision 9 months after surgery and the other having the flap advanced for better positioning and symmetry 6 months after surgery. Laser hair removal was performed for 9 cases to design the new eyebrow to mimic the normal side. Ideal position of the eyelid was observed in 10 cases; however, in 2 cases, a postoperative residual scleral a range of 1 to 2 mm was observed, although neither of the upper or lower eyelids required a secondary release after the operation. No complications were noted, apart from one case in which the loss of hair density in the parietal flap was observed combined with the loss of the distal 5 mm of the frontal flap. We administered a questionnaire to assess patient satisfaction within this group; the points included the degree of patient satisfaction, the density and orientation of hairs, the symmetry with the other side, and the skin color match of the nonhairy flap. The results of the questionnaire are summarized in Table 2 (Figs. 6, 7).
Table 2.
Patient Satisfaction with the Results
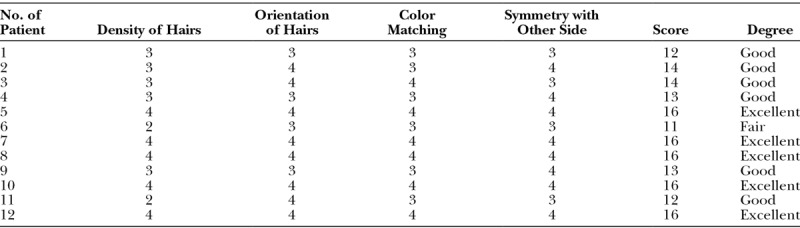
Fig. 6.

Late postoperative side view showing direct wound closure without skin grafts.
Fig. 7.

Male patient, 43 years, with postburn scarring of the left periorbital area with nonseeing left eye and late postoperative view.
DISCUSSION
A burned face is the single most important anatomical structure a burn surgeon is called upon to reconstruct. The periorbital area serves an important function in the identification of the individual and contains the organs of sight and personal identity. Distortion of this region can potentially cause functional impairment and deformities that lead to the withdrawal of the victim from society.14 The complex shape and form of the periorbital area renders reconstruction difficult, and the exposed position of the face allows only limited camouflage with clothing and makeup.9
The problems encountered in burned periorbital areas include alopecia in the eyebrows and ectropion in the upper and lower eyelids with lagophthalmos.
The goals of reconstruction should be to preserve, restore, and maintain function and appearance so that the cornea is protected from ulcers and painful conditions and the patient can function in society.15 To accomplish these goals, it is essential that the surgeon have an organized approach to the reconstruction of the burned periorbital area, including contracture release with replacement using the uncontracted option and restoration of the hair in the eyebrows.16
Eyebrows
The eyebrows function as an essential part of facial expression, conveying a spectrum of emotions including anger, sadness, and surprise. Their shape, proportion, angulation, symmetry, and size play a significant role in the perception of the face.17 The eyebrows are a unique area among hair-bearing areas in the body because of the notable thinness of the hair and the complicated pattern of hair direction. The orientation of the hairs varies according to their location within the eyebrow. Although hairs in the medial and lower eyebrows grow in the superolateral direction, those in the lateral and superior regions grow in the inferolateral direction. At the individual level, eyebrow hairs are short in length, small in diameter, and slow growing; all these characteristics are unique to the eyebrow.18
Eyebrow reconstruction works particularly well for those with extensive burn scarring of the face. The presence of hair can make the facial appearance more aesthetically pleasing by breaking up the uninterrupted area of scars. Options available for eyebrow reconstruction include micrografting,19,20 hair-bearing full-thickness skin grafts,21 and using vascularized island flaps based on the superficial temporal artery. However, cases of diffusely scarred and stiff recipient sites caused by burned or irradiated tissue represent the most difficult sites for successful transplantation.22,23
In cases where the recipient bed is not well vascularized because of burns or prior irradiation, pedicled vascularized scalp flaps based on the superficial temporal artery, either tunneled or tubed, may be used. This is typically a better reconstructive site technique, especially for men, because the thicker nature of male eyebrows is more appropriately matched by pedicled scalp flaps, which often cannot be thinned safely in a single operation to the extent appropriate for female patients, who typically possess a narrower eyebrow width.8 In fact, although the problems encountered with the use of the flap include the density and direction of hair, we typically find that the flaps yield better hair density than either grafts or hair transplantation and that the direction of the hair is more natural with a flap than in other options, as well.
In our cases, the reconstructed eye brow was refined to nearly normal by continuous toweling or laser hair ablation to achieve a finalized eyebrow shape according to patient preference. In some patients, the eyebrow may need to be advanced medially, which can be done under local anesthesia.
Eyelids
The most common periorbital problems are related to unopposed contraction of the scar tissue on the mobile lid margin, leading to ectropion.24 To correct this issue, the upper eyelid is released at the level of the supratarsal fold and is frequently reconstructed using a thick split-thickness skin graft because the skin of this area is more mobile. However, recurrence in the graft is common.2,3 Therefore, our solution for using the maximum available scarred tissue is to release the upper eyelid and occupy the defect with the temporal flap to resist recontracture and provide tissue for the future eyebrow.
The lower lid is released at the subciliary margin and is then managed using an full-thickness skin graft or local flaps, such as a laterally based myocutaneous upper eyelid flap or a superiorly based nasolabial flap, both of which are useful for lower lid ectropion.25 However, the use of skin grafts may lead to recurrent contracture, and the surrounding local flaps may not be available because of severe scarring, in addition to the added facial scarring.2,3 Therefore, the island superficial temporal artery flap provides an excellent and optimum solution for lower lid reconstruction with hidden scars. In some cases, the flap may be hairy, but the patient can undergo laser hair ablation to correct this issue.
Kajikawa and Ueda26 described unilateral extended superficial temporal artery flap surgery with 2 scalp paddles for the reconstruction of 2 eyebrows in their study. Bozkurt et al27 described the use of a medusa flap to reconstruct the periorbital area, although the authors actually used only a single skin paddle, not 2 skin paddles. In addition, they mentioned only 1 case in their report. Cöloğlu et al28 reported the use of an axial bilobed superficial temporal artery island flap (tulip flap) for the reconstruction of combined defects of the lateral canthus, including the lower and upper eyelids in 5 cases, although the author described only a single tailored island flap, not a chimeric flap. However, in the literature, no previous attempts have been made to use 2 paddles based on a single superficial temporal artery to reconstruct the eyebrow, upper eyelid, and lower eyelid simultaneously.
Limitations of usage of the flap include scarring of the temporal area or the previous use of temporoparietal fascia flap.
We consider this technique an innovative method for solving problems associated with periorbital burns and for helping patients reintegrate into society.
CONCLUSIONS
BSTIF is an innovative flap for reconstructing both burned eyebrows and eyelids. It is a new idea that reconstructs 3 different unique aesthetic facial units with a 1-stage island flap.
PATIENT CONSENT
Patients provided written consent for the use of their images.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Still JM, Jr, Law EJ, Belcher KE, et al. Experience with burns of the eyes and lids in a regional burn unit. J Burn Care Rehabil. 1995;16(3 Pt 1):248–252. doi: 10.1097/00004630-199505000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Malhotra R, Sheikh I, Dheansa B. The management of eyelid burns. Surv Ophthalmol. 2009;54:356–371. doi: 10.1016/j.survophthal.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 3.Fitzgerald O’Connor E, Frew Q, Din A, et al. Periorbital burns—a 6 year review of management and outcome. Burns. 2015;41:616–623. doi: 10.1016/j.burns.2014.08.022. [DOI] [PubMed] [Google Scholar]
- 4.Procede de cloture plastique de l’orbite apres l’exenteration. Arch Ophthalmol. 1898;18:679. [Google Scholar]
- 5.Monks GH. The restoration of a lower lid by a new method. Boston Med Surg J. 1898;139:385–387. [Google Scholar]
- 6.Gillies HD. Plastic Surgery of the Face. New York, NY: Gower Medical Publishing Ltd; 1983. [Google Scholar]
- 7.Ellis DS, Toth BA, Stewart WB. Temporoparietal fascial flap for orbital and eyelid reconstruction. Plast Reconstr Surg. 1992;89:606–612. doi: 10.1097/00006534-199204000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Juri J. Eyebrow reconstruction. Plast Reconstr Surg. 2001;107:1225–1228. doi: 10.1097/00006534-200104150-00021. [DOI] [PubMed] [Google Scholar]
- 9.Lei T, Xu DC, Gao JH, et al. Using the frontal branch of the superficial temporal artery as a landmark for locating the course of the temporal branch of the facial nerve during rhytidectomy: an anatomical study. Plast Reconstr Surg. 2005;116:623–629. doi: 10.1097/01.prs.0000174001.95115.9e. discussion 630. [DOI] [PubMed] [Google Scholar]
- 10.Zhong S-Z, Tao Y-S, Liu M-Z. The investigation of the superficial temporal artery and its bifurcation. Guang Dong Anat Bulletin. 1979;1:36. [Google Scholar]
- 11.Abul-Hassan HS, von Drasek Ascher G, Acland RD. Surgical anatomy and blood supply of the fascial layers of the temporal region. Plast Reconstr Surg. 1986;77:17–28. [PubMed] [Google Scholar]
- 12.Tan O, Atik B, Ergen D. Temporal Flap Variations for Craniofacial Reconstruction. Plast Reconstr Surg. 2007;119:152e–163e. doi: 10.1097/01.prs.0000261038.49905.b6. [DOI] [PubMed] [Google Scholar]
- 13.Chen TH, Chen CH, Shyu JF, et al. Distribution of the superficial temporal artery in the Chinese adult. Plast Reconstr Surg. 1999;104:1276–1279. doi: 10.1097/00006534-199910000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Achauer B. Burn Reconstruction. 1st ed. Stuttgart, NY: Thieme Verlag; 1991. [Google Scholar]
- 15.Wainwright DJ. Burn reconstruction: the problems, the techniques, and the applications. Clin Plast Surg. 2009;36:687–700. doi: 10.1016/j.cps.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Liu A, Pribaz J. Local flaps for burned face. In: Hyakusoku H, Orgill DP, Téot L, editors. Color Atlas of Burn Reconstructive Surgery. Heidelberg, Germany: Springer Verlag; 2010. pp. 178–185. [Google Scholar]
- 17.McCarthy JG. The Face. Vol. 2. Philadelphia, Pa.: WB Saunders; 1990. Plastic surgery general principles. pp. 1319–1323. [Google Scholar]
- 18.Ridgway EB, Pribaz JJ. The reconstruction of male hair-bearing facial regions. Plast Reconstr Surg. 2011;127:131–141. doi: 10.1097/PRS.0b013e3181fad328. [DOI] [PubMed] [Google Scholar]
- 19.Wang J, Fan J. Aesthetic eyebrow reconstruction by using follicular-unit hair grafting technique. Chin J Plast Surg. 2002;18:101–103. [PubMed] [Google Scholar]
- 20.Wang J, Fan J. Cicatricial eyebrow reconstruction with a dense-packing one- to two-hair grafting technique. Plast Reconstr Surg. 2004;114:1420–1426. doi: 10.1097/01.prs.0000138727.17753.73. [DOI] [PubMed] [Google Scholar]
- 21.Omranifard M, Ardakani MR, Abbasi A, et al. Follicular isolation technique with de-epithelialization for eyebrow and eyelash reconstruction. Plast Reconstr Surg. 2012;130:571–578. doi: 10.1097/PRS.0b013e31825dc00e. [DOI] [PubMed] [Google Scholar]
- 22.Brent B. Reconstruction of ear, eyebrow, and sideburn in the burned patient. Plast Reconstr Surg. 1975;55:312–317. [PubMed] [Google Scholar]
- 23.Feldman JJ. Facial burns. In: McCarthy JG, editor. Plastic Surgery. Philadelphia, Pa.: WB Saunders; 1990. p. 2153. [Google Scholar]
- 24.Wainwright DJ. Reconstruction of the peri-orbital region. In: Sood R, Achauer BM, editors. Achauer and Sood’s Burn Surgery: Reconstruction and Rehabilitation. Philadelphia, Pa.: WB Saunders; 2006. pp. 188–199. [Google Scholar]
- 25.Alghoul M, Pacella SJ, McClellan WT, et al. Eyelid reconstruction. Plast Reconstr Surg. 2013;132:288e–302e. doi: 10.1097/PRS.0b013e3182958e6b. [DOI] [PubMed] [Google Scholar]
- 26.Kajikawa A, Ueda K. Bilateral eyebrow reconstruction using a unilateral extended superficial temporal artery flap. Ann Plast Surg. 2003;50:416–419. doi: 10.1097/01.SAP.0000029627.89968.3E. [DOI] [PubMed] [Google Scholar]
- 27.Bozkurt M, Kulahci Y, Kapi E, et al. A new design for superficial temporal fascial flap for reconstruction of the eyebrow, upper and lower eyelids, and lacrimal system in one-stage procedure: medusa flap. Ann Plast Surg. 2009;63:636–639. doi: 10.1097/SAP.0b013e3181999e1b. [DOI] [PubMed] [Google Scholar]
- 28.Cöloğlu H, Koçer U, Oruç M, et al. Axial bilobed superficial temporal artery island flap (tulip flap): reconstruction of combined defects of the lateral canthus including the lower and upper eyelids. Plast Reconstr Surg. 2007;119:2080–2087. doi: 10.1097/01.prs.0000260602.32664.ba. [DOI] [PubMed] [Google Scholar]


