Summary:
Nasal osteotomies are a cornerstone step for closing an open roof deformity after dorsal hump surgery. Notwithstanding, the optimal method of nasal osteotomy remains controversial, as evidenced by the variety of approaches with no consensus between authors. Moreover, the election of the technique responds to surgeon’s preference. We proposed a new way to perform both medial and lateral osteotomies under direct vision. Direct vision of nasal osteotomies provides more predictable control and precision than blind procedures, making this procedure more reliable and easier for both novel and experienced surgeons. Other advantages include conservation of nasal muscle, angular vasculature, and periosteum, which allow less postoperative ecchymosis and edema and less risk of synechia and lacrimal sac injury.
Nasal osteotomies are truly a cornerstone step for closing an open roof deformity after dorsal hump surgery. Other indications for osteotomies in rhinoplasty include procedures to widen a narrow bony pyramid and narrow or straighten a wide or deviated nose. Despite being a crucial point in these frequent and highly demanding surgeries, the optimal method of nasal osteotomy remains controversial, as evidenced by the variety of approaches and variations, with no significant consensus between them.1–7 Thus, the election of the technique responds to surgeon’s preference. An ideal osteotomy technique should be precise, reproducible, and safe while minimizing postoperative sequel, including ecchymosis and edema. In an attempt to improve the available armamentarium regarding osteotomies in rhinoplasty, we offer a reliable concept of a new internal osteotomy approach.
OPERATIVE TECHNIQUE
Preoperatively, 2% lidocaine and 1/100,000 adrenaline is infiltrated through the sidewalls, tip, and dorsum of the nose. The procedure begins as a standard open rhinoplasty by means of a transcolumellar stair-step incision with bilateral standard marginal extensions. Then, the cutaneous flap is carefully elevated in a supraperichondrial plane by sharp dissection with scissors and retracted with an Aufricht retractor. Posteriorly, the critical point is to continue the dissection laterally by raising the periosteum. All the periosteum remains joined with all the soft tissues, from the midline to the lateral aspect beyond the nasomaxillary suture line. Once the entire nasal dorsum—both bone and cartilage—is exposed, a separation of the upper lateral cartilage from the septum is performed to prevent nasal mucosa damage. Thereafter, cartilaginous hump can be reduced with scalpel, and bony hump can be rasped or, in the case of being larger, removed with osteotome. Verification by palpation is paramount after any dorsal removal intent. Finally, under direct vision, osteotomies can be performed to close the open roof deformity (Fig. 1). Normally, a low-to-low lateral osteotomy is carried out combined with a medial oblique osteotomy. The mean dimensions are 18 mm in length to the vertical component and 4 mm in the sharp edge. Although this approach is standard, the specific type of osteotomy is evaluated individually in every patient.
Fig. 1.
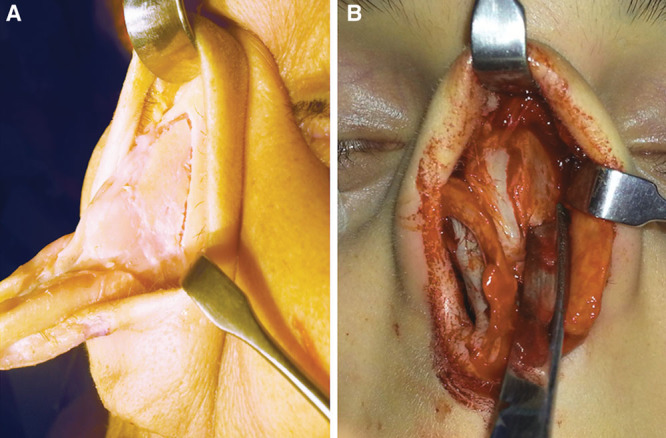
Osteotomies performed under direct vision in a cadaver by means of an open rhinoplasy approach (A). Intraoperative osteotomy under direct visualization of nasal bones (B).
After osteotomies and manipulation of the dorsum of the nose, the intervention on the tip can be performed as usual if necessary. Finally, sutures are placed to restructure columella, and a compressed foam nasal packing (Merocel, Polyvinyl alcohol sponge, Medtronic, Memphis, Tenn.) is applied to prevent the collapse of the nasal bones and stabilize the fracture. Some adhesive tape is collocated, and a thermoplastic-modeled pad is applied using gentle pressure, fixing the nose dorsum shape and stabilizing the osteotomies. The nasal packing is maintained for 24 hours while pad for 20 days. No nasal bone alterations have been reported for 1 year after the intervention (Fig. 2).
Fig. 2.

Preoperative (A) and 12-month postoperative (B) lateral views of a 25-year-old woman with nasal hump surgery and bilateral osteotomies under direct vision.
DISCUSSION
In rhinoplasty, nasal bone osteotomies play an important role in achieving the desired outcome for both patient and surgeon. Regarding patients, although they can refer little discomfort and pain related to the postoperative oedema and ecchymosis, the main problem remains the social disturbances and fright that it provokes. Conversely, surgeons try to elect the most precise technique; one that is safe and easy to perform while providing a good control of the osteotomy line. Although some variations have been described, the 2 main different techniques for closing an open roof deformity after dorsal removal are the internal continuous and the external perforator lateral osteotomy. The principal disadvantages of the internal osteotomy are the damage to the nasal mucosa that could produce synechia and nasal valve collapse and the damage to periosteum that produce postoperative bleeding and oedema.2 Adversely, performing an external perforator osteotomy requires a good deal of force to hammer the perforation. This, in turn, can cause an incomplete fracture whose mobilization may cause uncontrolled fracture lines, resulting in postoperative irregularities. Furthermore, a visible scar is a potential risk in the external approach.7 Despite the vast amount of clinical and cadaver studies contrasting both techniques there are supporting and conflicting arguments showing controversial results on comparison.1–3,8 Notwithstanding, both techniques include blind manipulation, which makes the outcome not entirely self-controlled but rather heavily dependent on the surgeon’s experience.
We propose a novel way to perform the internal osteotomy. It only requires an extra dissection from the nasal hump to the lateral borders in a subperiosteal plane by means of direct visualization. By elevating the superficial periosteum, it remains integral, diminishing the soft tissue injury and postoperative bleeding and blood collection. Furthermore, preservation of periosteum ensures stabilization of the mobilized nasal bones through a splinting action when replacing the periosteum to the original location. It also can camouflage any minor bony irregularities. Direct vision avoids harming the nasal mucosa while controlling the hammering force and the osteotome tip. Another advantage is conserving the medial canthal ligament attachment to the periosteum that diminishes the risk of lacrimal sac injury. Besides, the angular vasculature, whose rupture may be related to postoperative oedema and ecchymosis, can be displaced and protected within the elevated flap.3 In addition, the levator labii superioris alaeque nasi also remains uninterrupted, maintaining the functional unity and normal mobility of the nose.
Osteotomies under direct vision of nasal bones provide more predictable control and precision than blind procedures. By using the correct instrument, the likelihood of uncontrolled fracture lines is highly reduced. Furthermore, this approach gives an estimate of how much force is needed to break the bone, diminishing the risk of bone scattering, especially in aging noses with extremely fragile nasal bones. Technically, this approach does not lead to significant difficulties. After performing an open rhinoplasty, dissection is lightly continued laterally. The only pivotal point is practicing the dorsal correction before the osteotomies. Because the periosteum is elevated, nasal fragments after osteotomies could result in instability and therefore corrections at dorsal level should be always carried out earlier.
Once reporting this technique clinically with successful results after more than 1 year of follow-up, we suggest that this novel approach could be a new valuable tool for rhinoplasty. In this way, for docent and categorizing objectives, the new technique could be named direct open osteotomy to differentiate from internal and external classical osteotomies. To the best of our knowledge, this new internal approach offers a predictable strategy to achieve the desired outcome for obtaining adequate aesthetic brow lines in dorsal hump surgery, making this procedure more reliable and easier for both novel and experienced surgeons.
PATIENT CONSENT
The patient provided written consent for the use of her image.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Rohrich RJ, Muzaffar AR, Janis JE. Component dorsal hump reduction: the importance of maintaining dorsal aesthetic lines in rhinoplasty. Plast Reconstr Surg. 2004;114:1298–308. doi: 10.1097/01.prs.0000135861.45986.cf. discussion 1309–1312. [DOI] [PubMed] [Google Scholar]
- 2.Bohluli B, Moharamnejad N, Bayat M. Dorsal hump surgery and lateral osteotomy. Oral Maxillofac Surg Clin North Am. 2012;24:75–86. doi: 10.1016/j.coms.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Gryskiewicz JM, Gryskiewicz KM. Nasal osteotomies: a clinical comparison of the perforating methods versus the continuous technique. Plast Reconstr Surg. 2004;113:1445–1456. doi: 10.1097/01.prs.0000113031.67600.b9. discussion 1457. [DOI] [PubMed] [Google Scholar]
- 4.Yücel OT. Which type of osteotomy for edema and ecchymosis: external or internal? Ann Plast Surg. 2005;55:587–590. doi: 10.1097/01.sap.0000185396.94875.4a. [DOI] [PubMed] [Google Scholar]
- 5.Kiliç C, Tuncel Ü, Cömert E, et al. Effect of the rhinoplasty technique and lateral osteotomy on periorbital edema and ecchymosis. J Craniofac Surg. 2015;26:e430–e433. doi: 10.1097/SCS.0000000000001885. [DOI] [PubMed] [Google Scholar]
- 6.Ghazipour A, Alani N, Ghavami Lahiji S, et al. Buccal sulcus versus intranasal approach for postoperative periorbital oedema and ecchymosis in lateral nasal osteotomy. J Craniomaxillofac Surg. 2014;42:1456–1459. doi: 10.1016/j.jcms.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 7.Ghassemi A, Riediger D, Hölzle F, et al. The intraoral approach to lateral osteotomy: the role of a diamond burr. Aesthetic Plast Surg. 2013;37:135–138. doi: 10.1007/s00266-012-0011-2. [DOI] [PubMed] [Google Scholar]
- 8.Rohrich RJ, Janis JE, Adams WP, et al. An update on the lateral nasal osteotomy in rhinoplasty: an anatomic endoscopic comparison of the external versus the internal approach. Plast Reconstr Surg. 2003;111:2461–2462. doi: 10.1097/01.PRS.0000061005.27994.E3. discussion 2463. [DOI] [PubMed] [Google Scholar]


