Abstract
We report the case of a 58-year-old man with proliferative diabetic retinopathy in both eyes, and a history of recurrent anterior uveitis in the right eye, who underwent panretinal laser photocoagulation (PRP) for the retinopathy in both eyes, following which he developed hypopyon uveitis in the right eye. The condition was managed with topical steroids and cycloplegics, to which he readily responded. The case highlights that there is a breakdown of the blood aqueous barrier consequent to PRP. Patients with a history of uveitis are predisposed to develop recurrent uveitis after the said procedure and should be closely watched for such complications.
Background
Panretinal photocoagulation (PRP) is currently the standard treatment for proliferative diabetic retinopathy (PDR) with high-risk characteristics.1 It has been reported that PRP causes a transient breakdown of the blood aqueous barrier (BAB).2 We report a case of hypopyon uveitis that developed after PRP in a patient with a history of acute anterior uveitis.
Case presentation
A 58-year-old man, known to have moderate non-proliferative diabetic retinopathy for the past 3 years, visited our diabetic clinic for a routine follow-up with no presenting symptoms. He had a history of episodes of acute anterior uveitis in the right eye 1 year and 3 years ago, respectively, both times treated with topical steroids and cycloplegics. All systemic causes of uveitis were ruled out with elaborate investigations. He was a known case of diabetes mellitus type 2 and primary hypertension for the past 9 years. On examination, he had a best-corrected distant visual acuity of 20/25 and 20/30. The eyelids and adnexae were normal. The anterior segment was quiet with early nuclear cataract in both eyes. Fundus examination in both eyes showed multiple dot and blot haemorrhages in all quadrants, and microaneurysms and hard exudates in the macula (figure 1). The intraocular pressure (IOP) was 15 mm Hg in both eyes, assessed using Goldmann applanation tonometry. Fundus fluorescein angiography revealed neovascularisation elsewhere in the superior quadrant in both eyes. Optical coherence tomography showed no macular oedema in either eye. The diagnosis was therefore changed to bilateral PDR, for which the patient was treated with Pan Retinal laser Photocoagulation (PRP) in both eyes. The procedure was carried out in two sittings 1 week apart, with a 532 nm laser (PASCAL photocoagulator, OptiMedica), using 300 mW power, 30 ms pulse duration and 200 µm spot size. The total number of laser spots delivered in the two sittings were 3300 in the right and 3175 in the left eye. The patient was advised follow-up after 6 weeks. However, he visited the clinic 18 days after the laser treatment, with symptoms of pain, redness, watering and blurring of vision in the right eye for the past 4 days. On examination, the distant visual acuity of the right eye had dropped from 20/25 to 20/40. The same eye had ciliary congestion, a few Descemet membrane folds in the cornea and fine keratic precipitates on the corneal endothelium. The anterior chamber (AC) had cells 3+, flare 1+ and a 1 mm high hypopyon (figure 2A). There was pigment dispersion on the anterior capsule of the lens. On fundus examination, the media were hazy due to reaction in the AC and due to cataract, but the optic disc and the retinal vessels could be visualised, and disc and vessels seen. The left eye was unaffected. The IOP was 12 mm and 14 mm Hg in the right and left eye, respectively. There was no history of any constitutional symptoms in this patient's recent past.
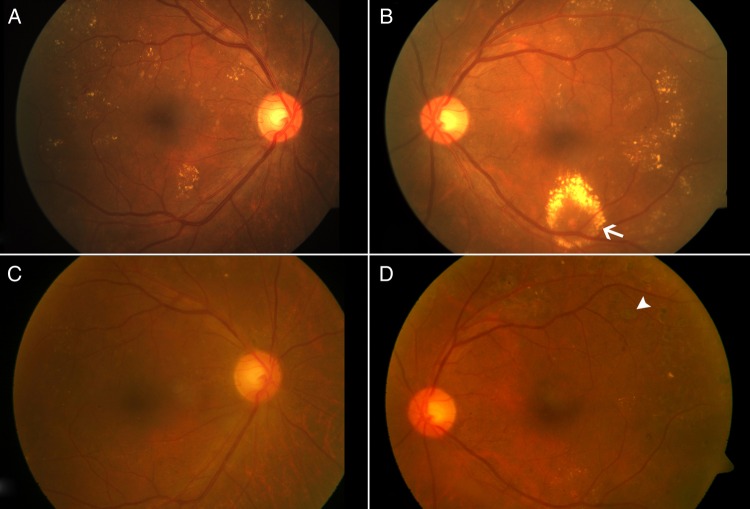
Figure 1.
Colour fundus photographs of the right and left eye. (A) and (B): both eyes showing multiple dot and blot haemorrhages in all quadrants, and microaneurysms and hard exudates (arrow) in the macula. There was presence of neovascularisation in the periphery. (C) and (D): fundus photographs after 1 month of panretinal photocoagulation (PRP), showing PRP marks (arrow head). The hard exudates had also regressed.
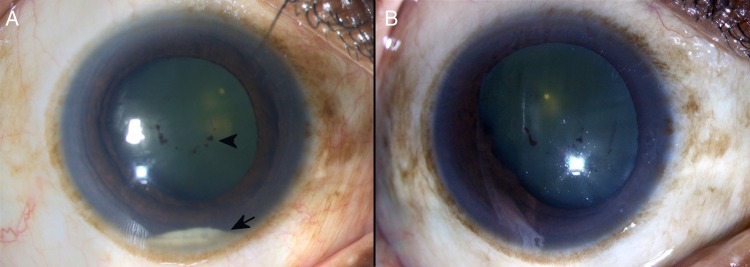
Figure 2.
(A) Colour photograph of the anterior segment of the right eye 2 weeks after panretinal photocoagulation, showing hypopyon (arrow) and pigments on anterior lens capsule (arrowhead). (B) Colour photograph of the anterior segment of the right eye, showing resolution of hypopyon after treatment with topical steroids and cycloplegics.
Investigations
The patient had fasting and postprandial blood sugar levels of 78 and 135 mg/dL, respectively. He was non-reactive for HIV by ELISA and non-reactive for rapid plasma regain. He had an induration of 8 mm 72 hours after tuberculin test. Chest radiograph was normal. The serum ACE level was within normal limits (38.7 units/L). The erythrocyte sedimentation rate was 20 mm/hour. The blood haemoglobin level, and the total and differential leucocyte counts, were within normal limits. The renal function tests were normal with a serum creatinine level of 0.8 mg/dL. The results ruled out the systemic causes of secondary uveitis in the eye.
Differential diagnosis
Based on the clinical picture, a clinical diagnosis of ‘acute anterior uveitis of the right eye—post retinal laser photocoagulation’, was concluded. A differential diagnosis of endogenous endophthalmitis was also considered. However, the absence of any systemic source of infection as confirmed with the results of systemic investigations ruled out the second diagnosis.
Treatment
The patient was treated with topical prednisolone acetate 1% eye drops along with topical cycloplegics.
Outcome and follow-up
The visual acuity of the right eye returned to 20/25 within 2 weeks and the eye was quiet with no signs of uveitic reaction in the anterior or posterior segment (figure 2B). The topical steroids were gradually tapered over the next 4 weeks.
Discussion
Moriarty et al2 measured the breakdown of the BAB after PRP in 25 eyes of 25 patients of PDR, with a laser flare photometer. The authors concluded that there was a significant increase in aqueous flare value at 3, 24 and 48 hours compared with at baseline but not at 72, 96 and 168 hours nor at 8 weeks. However, our patient presented with acute hypopyon uveitis 18 days after the PRP when the BAB should have been restored and the eye quietened.
Lee and van Heuven3 reported a case of hypopyon uveitis following PRP in a 55-year-old diabetic man with a history of previous repair of a retinal detachment by scleral buckle and vitrectomy. The authors hypothesised that anterior segment ischaemia caused by the scleral buckle predisposed patients with diabetes to the complication of hypopyon uveitis following PRP.
Sinha et al4 reported a case of hypopyon uveitis that developed following the first sitting of PRP in a patient with uncontrolled diabetes mellitus. The authors ascribed poor glycaemic control to the predisposition for breakdown of the blood ocular barrier in their case.
Ours is an atypical case of a patient who had good glycaemic control and no surgical cause for anterior segment ischaemia, who atypically presented to us with hypopyon uveitis more than 2 weeks after PRP. We hypothesise that the two past episodes of acute anterior uveitis were the cause of a compromised BAB in our case. The procedure of PRP therefore precipitated the uveitic reaction in the affected eye. The case highlights the need for a close watch for recurrence of acute uveitis following laser photocoagulation in cases with a history of uveitis.
Learning points.
It is important to rule out a history of uveitis in any form before performing panretinal photocoagulation (PRP) in a patient.
Past episodes of uveitis can lead to a compromised blood aqueous barrier and such patients may be predisposed to exacerbations and recurrence of uveitis.
Patients having a history of uveitis and undergoing PRP should be followed up early and more frequently to check for recurrence of uveitis.
Good glycaemic control may not be sufficient to prevent such recurrence in these patients.
Footnotes
Contributors: MT and PKR were involved in the treatment of the patient. MT and VA were involved in writing the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Early photocoagulation for diabetic retinopathy: ETDRS report number 9. Ophthalmology 1991;98(Suppl 5):766–85. 10.1016/S0161-6420(13)38011-7 [DOI] [PubMed] [Google Scholar]
- 2.Moriarty AP, Spalton DJ, Shilling JS et al. Breakdown of the blood aqueous barrier after argon laser panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology 1996;103:833–8. 10.1016/S0161-6420(96)30607-6 [DOI] [PubMed] [Google Scholar]
- 3.Lee BL, van Heuven WA. Hypopyon uveitis following panretinal photocoagulation. Ophthalmic Surg Lasers 1997;28:505–7. [PubMed] [Google Scholar]
- 4.Sinha MK, Narayanan R, Chhablani JK. Hypopyon uveitis following panretinal photocoagulation in a diabetic patient. Semin Ophthalmol 2014;29:166–8. 10.3109/08820538.2013.807846 [DOI] [PubMed] [Google Scholar]