Description
A 45-year-old man whose parents emigrated from Hong Kong presented with a 2-year history of recurrent epistaxis, neck lump and worsening vision. He had never smoked.
Baseline ophthalmology assessment confirmed left vision loss to finger-counting. Infection screens including retroviral, hepatitis and Epstein-Barr virus were negative. A positron emission tomography scan revealed nasopharyngeal mass with direct invasion into bilateral orbital fossae and bilateral neck nodes (figures 1A and 2A). An incisional biopsy performed under general anaesthesia confirmed dedifferentiated adenoid cystic carcinoma (d-ACC) stage cT4N2cM0 (figure 3).
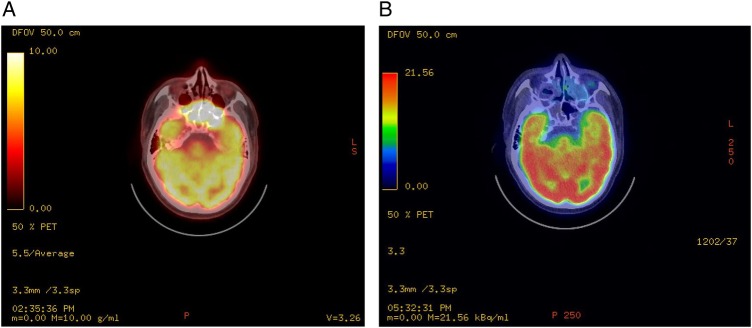
Figure 1.
(A) PET scan before treatment revealed very abnormal metabolically active soft tissue bone extending from the nasopharynx to maxillary antra, ethmoid, sphenoid, orbits and mid-cranial fossa. There is clear bone destruction of the sinuses walls and base of the skull. (B) Post-treatment PET scan performed 8 months later revealed complete disease remission of primary disease at the base of skull. There is no local metabolically active disease. PET, positron emission tomography.
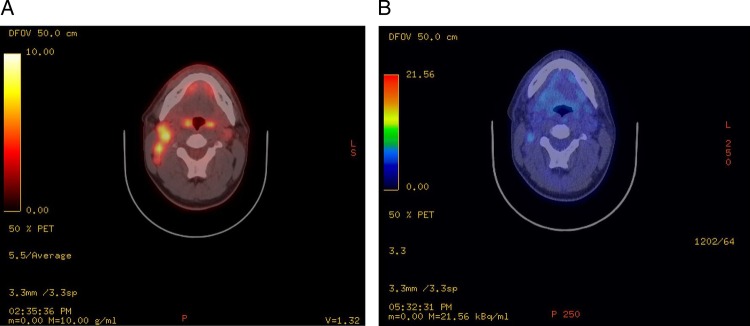
Figure 2.
(A) PET scan before treatment showed enlarged metabolically active right cervical lymphadenopathy involving levels 2 and 3 measuring 2.1×4.3 cm. Prominent left level 2 node is also noted measuring 1.1×0.9 cm demonstrating mild increased metabolic activity. PET, positron emission tomography. (B) Post-treatment PET scan showed a mildly active right level 2 node which measures 1.4×0.6 cm with unknown significance. No other metabolically active cervical nodes identified. PET, positron emission tomography.
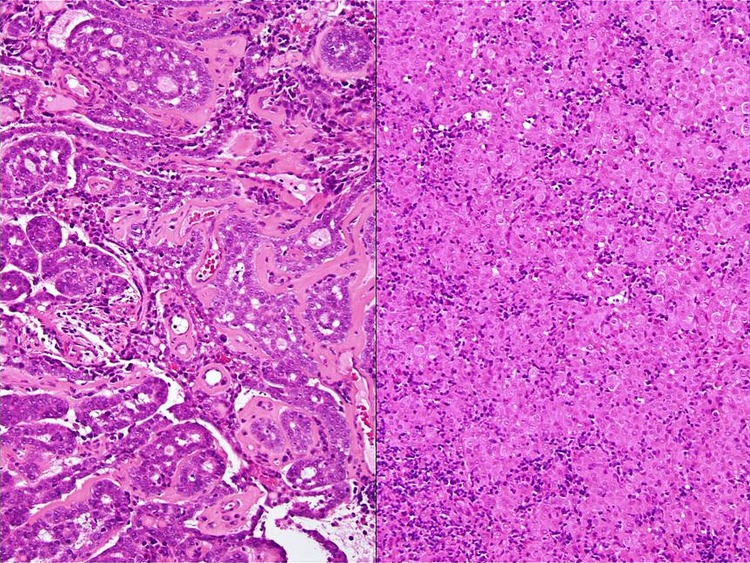
Figure 3.
Photomicrographs of histology tissue (image on the left) showing low-grade adenoid cystic carcinoma, tubulo-cribriform pattern with abundant eosinophilic basement membrane material, numerous pseudolumina and occasional true glandular lumina, contrasted against (image on the right) more poorly differentiated elements showing well-defined, pleomorphic, large epithelioid cells disposed in solid/insular architecture. The latter is accompanied by more conspicuous interstitial lymphoplasmacytic inflammatory cell infiltrate albeit with minimal intratumoural lymphocytosis proper (H&E; original magnifications ×10).
Multimodality treatment was recommended. He was started on neoadjuvant triplet chemotherapy docetaxel (75 mg/m2), cisplatin (75 mg/m2) and fluorouracil (750 mg/m2) (TPF regime) for three cycles. Reassessment with imaging showed good partial response and therefore he was treated with radical chemoradiotherapy (Tomotherapy 65 Gy in 30 fractions with synchronous Cisplatin).
Post-treatment functional imaging confirmed complete remission in the primary and left-sided neck node with minimal uptake of uncertain significance in a right level 2 neck node (figures 1B and 2B). At 10 months after treatments, patient remained stable and showed no evidence of disease recurrence. Skull base multidisciplinary team (MDT) has scheduled reimaging in 3-month time. Patient was kept under an MDT (ENT, Clinical Oncology and Ophthalmology) follow-up for every 12 weeks.
Adenoid cystic carcinoma is a malignancy of the salivary glands with a mean survival of 4.3 years and 43–57% of patients present with lymph node metastasis.1 d-ACC is a rare variant with high-grade transformation and is reported in only 40 case reports worldwide.1 2
Learning points.
Adenoid cystic carcinoma is a malignancy of the salivary glands with 5-year survival rate of 77.3% and 10-year survival rate of 59.6%.3 However, once high-grade transformation occurs, dedifferentiated adenoid cystic carcinoma has 5-year survival rate of 16.7% and 10-year survival rate of 8.3%.1 This is a rare variant and is only reported in over 40 case reports worldwide.1
Adenoid cystic carcinoma is usually a low-grade malignancy treated predominantly with surgery followed by adjuvant radiotherapy. In this case, surgical clearance was not feasible due to locally advanced T4 disease.
Patients who present with recurrent epistaxis, neck lump and visual impairment with a Far East and North African heritage should raise the suspicion of nasopharyngeal carcinoma. However, dedifferentiated adenoid cystic carcinoma can present with similar clinical history and findings and can only be differentiated by histopathology analysis.
Footnotes
Contributors: ISB consented the patient, reviewed the literature, performed data analysis and drafted the manuscript. ATW is Consultant Histopathologist who prepared and described the histopathology slides and revised the manuscript. SKA is the attending Consultant ENT and Skull Base Surgeon and reviewed the manuscript. CSB is attending Consultant Clinical Oncologist who reviewed the literature, performed data analysis and revised the manuscript. AH is the attending Consultant Clinical Oncologist who identified the patient, revised the manuscript and supervised the case-report write up.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hellquist H, Skálová A, Barnes L et al. Cervical lymph node metastasis in high-grade transformation of head and neck adenoid cystic carcinoma: a collective international review. Adv Ther 2016;33:357–68. 10.1007/s12325-016-0298-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costa AF, Altemani A, Hermsen M. Current concepts on dedifferentiation/high-grade transformation in salivary gland tumors. Patholog Res Int 2011;2011:325965 10.4061/2011/325965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lloyd S, Yu JB, Wilson LD et al. Determinants and patterns of survival in adenoid cystic carcinoma of the head and neck, including an analysis of adjuvant radiation therapy. Am J Clin Oncol 2011;34:76–81. 10.1097/COC.0b013e3181d26d45 [DOI] [PubMed] [Google Scholar]