Abstract
Background.
Sharing information with patients within a consultation about their infection and value of antibiotics can help reduce antibiotic prescriptions for respiratory tract infections. However, we do not know how often information is given about antibiotics or infections, and if this is related to knowledge and attitudes.
Objectives.
To determine the public’s reported use of antibiotics, receipt of information from health professionals about antibiotics and resistance, trust in health professionals and knowledge levels about antibiotics and resistance.
Methods.
Face-to-face computer-assisted survey with 1625 adults over 15 years in randomly selected households using multistage sampling. Rim weighting was used to correct for any selection biases.
Results.
About 88% trusted their GP to determine the need for antibiotics. Of those who took antibiotics in the past year, 62% were for a throat infection, 60% for sinus infection and 42% for a cough. Although 67% who had been prescribed an antibiotic recalled being given advice about their infection or antibiotics, only 8% recalled information about antibiotic resistance. Those in lower social grades were less likely to recall advice. About 44% correctly indicated that antibiotics effectively treat bacterial rather than viral infections. Only 45% agreed that ‘healthy people can carry antibiotic resistant bacteria’.
Conclusion.
GPs and health carers are trusted decision-makers, but could share more information with patients about the need or not for antibiotics, self-care and antibiotic resistance, especially with younger patients and those of lower social grade. Better ways are needed for effective sharing of information about antibiotic resistance.
Key words. Family practice, information, knowledge, leaflets, questionnaire.
Introduction
As antibiotic resistance is related to antibiotic use, the general public and health professionals are being urged to use antibiotics more appropriately (1). Health care in the UK is centrally funded through the National Health Service (NHS) providing (mostly free) primary and specialist health care. GPs are responsible for registered populations of patients and hire a range of ancillary staff, and act as gatekeepers to most specialist care (2). Patients may also directly access out of hours primary care, emergency services (which are usually based in the hospital) and certain specialist services, i.e. genito-urinary medicine (2).
In the UK, the largest proportion of antibiotics are prescribed for patients in the community: general practice (74%), hospital outpatients (7%), dental practices (5%) and other community settings (3%), prescribing in hospital inpatients account for 11% of total consumption (3). Half of adults consulting their GP with a respiratory tract infection (RTI) expect an antibiotic, but there are many factors influencing their behaviour (4,5). Patients visit their GP practice with an RTI or fever because they perceive the illness is severe or lasting longer than expected; although about half expect an antibiotic, they also want reassurance and information on their illness (4). Satisfaction with a consultation is not necessarily related to receiving antibiotics (5,6). Sharing written information with patients or carers within a primary care consultation can reduce antibiotic prescriptions for RTIs and re-consultations (7,8), and the approach is cost-effective (9). Patients find information about the length of illness, self-care advice, when to consult and advice about antibiotic use helpful (10). This patient-centred approach with shared information about the infective illness and how to use antibiotics appropriately is therefore being encouraged in general practice (7), where 90% of patient contact takes place (11), with a patient leaflet for adult patients (launched in 2012 by the Royal College of General Practitioners in England). To address the gap in data on how often the general public are given information about antibiotics by primary care clinicians, we aimed to use a face-to-face interviewer administered questionnaire to determine the general public’s perceptions about receiving information about antibiotics and associated trust. We also wished to determine if receipt of information was associated with knowledge levels about antibiotics and resistance. Findings should help to inform public and professional education interventions to improve antibiotic use.
Methods
As we wanted the general public’s views, we undertook the survey through ‘Ipsos MORI’, an independent research agency who undertake a weekly face-to-face ‘Capibus’ survey in randomly selected homes across England. This survey was undertaken in January 2014; individuals aged 15 years and over were interviewed using computer-assisted interviewing. Respondents were selected for the face-to-face survey using a controlled form of random location sampling (12) where household areas are randomly selected. Interviewers set quotas based on the profile of the population, and data weighted by gender, age, ethnicity, working status, social grade, housing tenure and Government Office Region (GOR) for the area based on the profile of people living in that area; overall this gives a sample representative of the English general public. Households were visited throughout the week during the day, evenings and weekends to ensure that a wide range of individuals were able to participate.
Questionnaire schedule
The questions were developed collaboratively by the authors and Ipsos MORI health team and were based on recent qualitative and quantitative work with young people and the general public about their views and use of antibiotics (10) (Box 1). Respondents were asked which medical conditions they understood could be effectively treated with antibiotics, and whether they agreed or disagreed with statements about antibiotic resistance. Respondents were also asked about any infections in the last 12 months, and if they had taken antibiotics for them, whether they had visited a health professional with these infections, and if they had received any information about antibiotics and self-care of infections and whether this was in a written format. Throughout the questionnaire, the term antibiotics was used to refer to antibacterials and not antivirals and antifungals.
Box 1. Questions asked of respondents
1. Which of the following conditions, if any, do you think can be effectively treated by antibiotics?
2. In the last 12 months, since January 2013, which, if any, illnesses or infections have you had?
3. In the last 12 months when you have taken an antibiotic, where, if at all, was it prescribed?
4. In the last 12 months, approximately how many courses of antibiotics have you taken for [‘insert illnesses mentioned above’]?
5. In which, if any, of the following ways have you taken an antibiotic in the last 12 months?
6. Can I check, in the last 12 months, have you taken an antibiotic that has not been prescribed to you personally by a GP, nurse or dentist?
7. Thinking about instances when you visited a health professional for an infection you have had within the last 12 months, did you receive advice or information about any of the following?
8. Did the health care professional give you any printed information, such as a leaflet or a pamphlet about infections or antibiotics?
9. Where were you when you were given this information by a health care professional?
10. The following are statements some people have made regarding antibiotics. Please tell me to what extent you agree or disagree with the following?
Bacteria that are resistant to antibiotics spread easily from person to person.
Most coughs, colds and sore throats get better on their own without the need for antibiotics.
You do not need to finish a course of antibiotics if you are feeling better.
I trust my GP advice as to whether I need antibiotics or not.
I trust my nurse’s advice as to whether I need antibiotics or not.
I trust the pharmacist’s advice as to whether I need antibiotics or not.
Healthy people carry antibiotic-resistant bacteria.
Questionnaire data analysis
Data processing was carried out by a data analyst and statistician at Ipsos MORI. So that results are broadly representative of the population, a ‘rim weighting’ system (13) was used that weights to the latest set of census data or mid-year estimates and National Readership Survey defined profiles for age, region and working status—within gender and additional profiles on tenure, ethnicity and social grade (A high or B intermediate managerial, administrative or professional; C1 supervisory, clerical and junior managerial, administrative or professional; C2 skilled manual workers; D semi-skilled and unskilled manual workers; or E state pensioners, casual or lowest grade workers and unemployed). Rim weighting uses a mathematical algorithm to help provide an even distribution of results across the entire data set while balancing the categories defined above; it weights the specified characteristics simultaneously and disturbs each variable as little as possible. The Pearson chi-squared test was used to assess differences in percentages. The P value of <0.05 was used to determine significant difference.
Results
A total of 1625 individuals were recruited and interviewed according to the relevant quotas (Table 1).
Table 1.
Participant quotas, based on the profile of the population, and weighted by gender, age, ethnicity, working status, social grade, housing tenure and Government Office Region (GOR) set at a national level and the number of participants recruited in each
| Quota | Achieved | |
|---|---|---|
| Male | 795 | 826 |
| Female | 830 | 799 |
| 16–24 | 259 | 289 |
| 25–64 | 1035 | 943 |
| 65+ | 331 | 393 |
| Full-time work | 691 | 587 |
| Not full-time | 934 | 1038 |
Antibiotic use
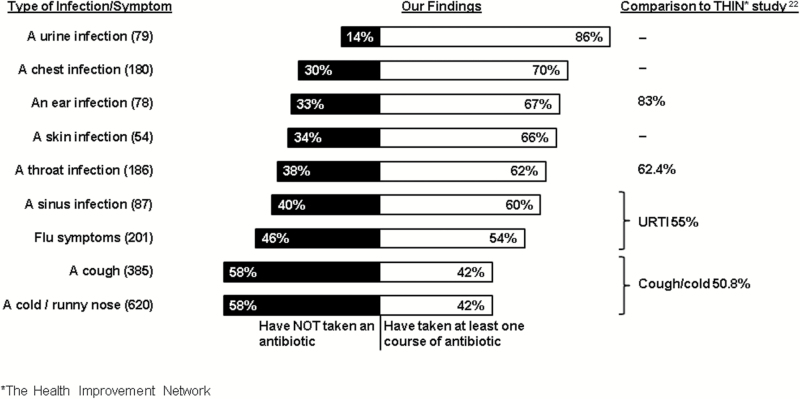
One-third (34%) of the total 1625 participants reported being prescribed an antibiotic in the last year. Two-thirds of the respondents (65%, 1052/1625) reported having an infection in the previous year; 52% (555/1052) of these reported being prescribed at least one course of an antibiotic. Forty-two per cent of those recounting a runny nose or cold in the last year reported taking an antibiotic for it, 42% with cough, 54% with flu symptoms, 60% with sinus infection, 62% with throat infection and 67% with ear infection (Fig. 1). There were no significant differences between any subgroups of respondent concerning antibiotic prescription for their reported infections. Of all respondents, 88% trusted their GPs’ advice, 69% their nurse and 66% their pharmacist’s advice as to whether they needed antibiotics or not for an infection.
Figure 1.
Percentage of respondents with each infection in the last 12 months who reported they have not taken (left-hand bar) or have taken at least one course of antibiotics (right-hand bar); and GP prescribing reported using The Health Improvement Network (THIN) data (22)
Information provision
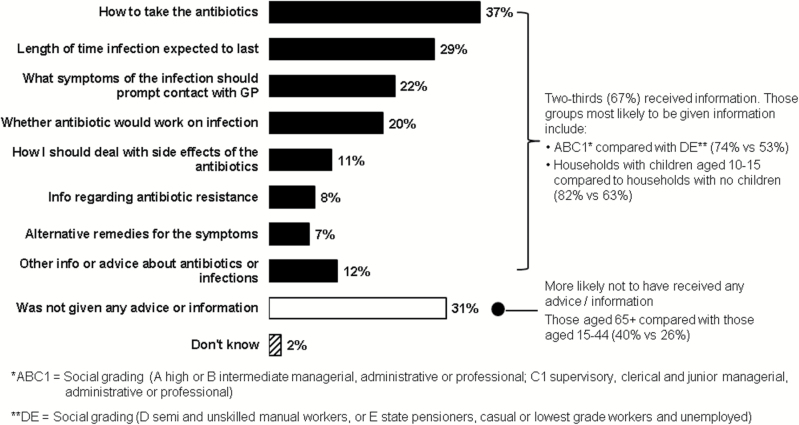
Almost half of those who had consulted a health professional in the last year for an infection, and 67% of those who received an antibiotic reported having been given some sort of advice. Only 8% who were prescribed an antibiotic recalled being given information on antibiotic resistance; 22% were given advice about what symptoms of the infection should prompt them to contact their GP surgery again (Fig. 2). Most advice about infections was provided at the GP surgery (76%) and 38% of all advice provided was in a printed format. Participants from higher social grades and also those educated to a higher level were more likely to report they had been given information about antibiotics or caring for their infection [80% social grade AB and 76% educated to A level (English academic exams taken by 18 year olds) or higher given any information versus 53% social grade DE and 55% with no formal qualifications; 32% AB given information about whether an antibiotic will work on an infection versus 15% C2DE].
Figure 2.
Advice given to those with an infection in the past year who were given an antibiotic
Knowledge on antibiotic use
Eighty-six per cent of all respondents [95% confidence interval (CI): 84.3–87.7%] agreed with the statement ‘Most coughs, colds, sore throats get better on their own without the need for antibiotics’; 77% (95% CI: 75–79%) agreed that ‘bacterial infections can be effectively treated with antibiotics’. Many incorrectly answered that non-bacterial infections could be effectively treated with antibiotics including viral infections (40%), fungal infections (26%), colds or flu (14%), and other illnesses such as allergic reactions (11%), hay fever (4%) or asthma (4%), and symptoms sometimes associated with infections such as inflammation or swelling (17%), pain (7%) and headaches (4%). Respondents 15–24 years were significantly more likely to say that antibiotics were effective for other illnesses or symptoms (anti-inflammatory 27%, fungi 33%, pain 14% and headache 9% versus over 25 years 15%, 24%, 6% and 3%, respectively). Combining these responses, only 44% (95% CI: 41.6–46.4%) chose correctly that bacterial infections, but not viruses, or colds and flu could be effectively treated with antibiotics. Women, 50% (95% CI: 47.6–52.4%, P < 0.001), were significantly more likely than men (38%) to answer in this way, as were those who were social grade ABC1, 53% (95% CI: 50.6–55.4%, P < 0.001) compared to DE, 30%.
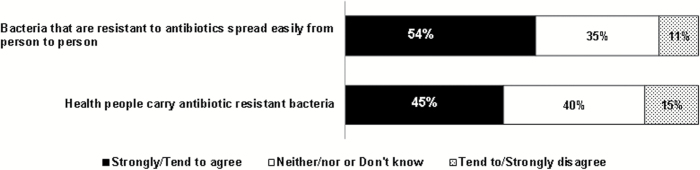
Knowledge on antibiotic resistance
About half of the respondents lacked knowledge about antibiotic resistance (Fig. 3). Fifty-four per cent (95% CI: 51.6–56.4%) agreed that ‘Bacteria that are resistant to antibiotics spread easily from person to person’ with no major differences by age, social grade or gender, if they had requested antibiotics in the past year or had children in the household. Only 45% (95% CI: 42.6–47.4%) agreed that ‘Healthy people carry antibiotic resistant bacteria’. Younger respondents were more likely to disagree with this statement than older respondents (20% 15–34 years versus 11% over 55 years P < 0.001), but otherwise there were no significant differences by social grade or gender, or if respondents had asked for antibiotics in the past year or had children in the household.
Figure 3.
Knowledge about the spread and carriage of resistant microorganisms (n = 1625)
Discussion
Main findings
Many members of the general public report taking antibiotics for infections that usually resolve at about the same rate whether or not they are treated with antibiotics. People have considerable trust in advice about antibiotic treatment from GPs, nurses and pharmacists. Those least knowledgeable on the topics covered in the interview were also the groups less likely to recall being given information about antibiotics and resistance; only half of social grade DE or with no formal education compared to over three-quarters of social grade AB or educated to A level or above recalled such advice. There is a substantial sector of the population who incorrectly endorse statements that antibiotics are effective for non-bacterial illnesses and symptoms sometimes associated with infections; this misunderstanding is greater in men, lower social grades, lower educated and younger sectors of the population. About half of the population does not know that antibiotic-resistant bacteria are carried by healthy people and can spread easily from person to person.
Strengths and limitations
The questions were asked of a representative sample from across England, and therefore the findings are likely to be representative of the general public’s opinions and reflect the public’s use of antibiotics and health services. The questions relating to antibiotic use and information provision required respondents to recall events in the previous year—which may be subject to some recall bias. More incorrect responses about antibiotics by lower educated individuals may have been due to misunderstanding about some of the terms; however, examples of the different types of infections and symptoms were provided. Although this study generated information about patients’ perceptions of their experiences, it does not tell us about the perspective of the health care provider.
Comparison with other literature
Most antibiotics in England are prescribed in general practice (74%) (3). Study findings highlight that almost half (49%) of respondents who visited their GP and had an infection in the past year did not receive any information about their infection or about antibiotics. Macfarlane was one of the first to show that informing previously well patients about the natural history of lower RTI (LRTI) symptoms is an effective strategy for reducing re-consultations (14.9% re-consulted when they received a leaflet versus 21.4% not receiving a leaflet) (8). A total of 88% of 1014 patients or carers visiting a GP in the Netherlands with an RTI reported receiving information about their infection (14). This is much higher than in our survey, but could partly be due to better recall by patients in the Netherlands as they were asked to complete the questionnaire immediately after their consultation. Receiving information/reassurance is more strongly associated with satisfaction than receiving an antibiotic prescription (adjusted odds ratio 10.6) (14). In a questionnaire survey of patients with acute sore throat, the three most common reasons for visiting the GP were examination to establish the cause of the symptoms, seeking pain relief and information on the course of the disease (15). Twenty-nine per cent of respondents in our survey who visited a health professional and were prescribed antibiotics reported that they received information about expected duration of symptoms, and only 7% remembered being given advice on symptom relief. Only 8% of patients in our survey were given any information regarding antibiotic resistance. In a small USA face-to-face questionnaire study based in family practice surgeries, 68% of patients reported that a doctor had ever discussed antibiotic resistance with them (16).
A European primary care study exploring variation in antibiotic prescribing decisions for LRTI across Europe found that a clinician’s commitment to shared decision-making greatly influenced their antibiotic prescribing (17), suggesting that if a clinician could explain their prescribing decisions to patients, this may help to reduce antibiotic prescribing (17). Our work suggests that there is scope to increase information sharing as 88% trusted their GP about whether they needed an antibiotic. Similar trust in GPs was found in an American study in which 95% of respondents reported that they trusted or were satisfied when their doctor told them that they did not need an antibiotic (16). Despite the known benefits of this shared information approach (7), systematic reviews have found that GPs prioritize meeting patients and carers perceived expectations, over evidence-based guidelines. These reviews have attributed diagnostic uncertainty and fear of possible complications in the patient as the GP’s attitudes most associated with misuse of antibiotic prescribing (18). In contrast to this, an American survey illustrated that 98% of patients thought that they had an important role in learning about multidrug-resistant organisms and 94% thought that getting information would help them to make choices that would improve care (19). Training GPs in enhanced communication skills for managing LRTIs that included discussion on the ‘pros and cons’ of antibiotics and ‘lifting the lid’ on antibiotics resulted in a safe reduction of antibiotic prescribing (9).
That being said, a greater lack of knowledge within the groups of patients in the lower social grades and educational attainment who have greater antibiotic use but are less likely to report being given any information suggests that more research is needed with these groups to understand how the difficult concept of antibiotic use and resistance can be portrayed. Recent qualitative studies indicate that patients believe that bacterial resistance is largely a hospital problem caused by poor environmental hygiene (20); few patients suggest that they could help control it, or see it as something that would affect them personally (20). Patients emphasized the need for simple language and incorporation of actual patient stories (19); more qualitative work with patients and health professionals is needed to determine how we can get messages about antibiotic resistance and use across. More patients in this 2014 survey correctly answered that coughs and colds get better on their own without antibiotics (86%) compared to similar English surveys in previous years (60% in 2008, 63% in 2009 and 69% in 2011) (21). However, care must be taken in comparing responses to previous similar surveys as the exact wording and order of the questions were different and may influence respondents. The percentage reporting receiving antibiotics for their infections was similar to that in a cross-sectional study using data from The Health Improvement Network (THIN), a computerized database of consultation and prescription data from 570 UK general practices covering 3.8 million active patients (22). As in this study, there were no clear trends by different patient groups (Fig. 1) (22). This suggests our data are valid and it could be an efficient way to monitor antibiotics use by patients over time, until antibiotic prescribing data are linked to indication.
The misunderstanding by respondents that viral infections can be effectively treated with antibiotics may explain some of the ongoing misuse of antibiotics, but this is a difficult concept to describe to patients as viral and bacterial RTIs can have similar initial presentations and both can cause severe illnesses. Indeed, previous research found that greater patient knowledge about activity of antibiotics against bacteria and viruses is not necessarily related to appropriate antibiotic use (23), demonstrating that concentrating on these differences is not appropriate. Providing patients with guidance on specific symptoms is more effective at reducing consultations and antibiotic use for RTIs (24).
Conclusion
When patients present with infections (and especially those in lower social grades and without formal educational qualifications), health care staff need to share more information about the need, or not, for antibiotics, and how patients can self-care for infections and the problems of antibiotic resistance. NICE guidance in England now recommends that good communication between patient and GP should be supported by evidence-based written information tailored to the patient’s needs (25). In England, the TARGET antibiotics toolkit (26) provides a patient information leaflet to help support this need; however, media campaigns would help to reinforce these messages. We need more research to determine how information about antibiotic resistance can be shared more effectively and whether this influences expectations for antibiotics for uncomplicated infections.
Declaration
Funding: Public Health England.
Ethical approval: the data collection for the survey was carried out by Ipsos MORI, an independent research agency who is bound by the rules of the Market Research Society, guidelines and regulations. Respondents gave informed consent and had the right to stop the interview at any point. Respondents were not given any financial incentive. All data were processed in accordance with the Data Protection Act 1998.
Conflict of interest: CAMM leads the development and writes evidence-based antibiotic guidance for primary care and leads the RCGP TARGET antibiotic toolkit development including a patient leaflet encouraging delayed/back-up prescribing. She is a member of ARHAI. Any payment for speaking at conferences goes to a research trust fund. CCB holds publically funded grants relating to the management of common infections, and one study is unconditionally supported by Alere through the loan of CRP point of care testing devices and kits. He has received fees for update lectures. No other authors declared any competing interests. AQ is head of Health Research at Ipsos MORI, she was not involved in the actual data collection process.
Acknowledgements
We would like to thank Daniel Marshall, Sarah Shepherd and David Jeans for advising on questionnaire development; the public who answered the questionnaire; and Katherine Butler for administrative support.
References
- 1. Department of Health. UK 5 Year AMR Strategy. In: Health Do. London, UK: Grown Copyright, 2013, pp. 43. [Google Scholar]
- 2. Uusküla A, Ricketts EJ, Rugman C, et al. Provision of chlamydia testing, and training of primary health care staff about chlamydia testing, across four European countries. BMC Public Health 2014; 14: 1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. EUSPAR. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) 2010 to 2014: Report 2015. London: Public Health England, 2015. [Google Scholar]
- 4. McNulty CA, Nichols T, French DP, Joshi P, Butler CC. Expectations for consultations and antibiotics for respiratory tract infection in primary care: the RTI clinical iceberg. Br J Gen Pract 2013; 63: e429–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Coenen S, Francis N, Kelly M, et al. ; GRACE Project Group. Are patient views about antibiotics related to clinician perceptions, management and outcome? A multi-country study in outpatients with acute cough. PLoS One 2013; 8: e76691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. Br Med J 1998; 317: 637–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Francis NA, Butler CC, Hood K, et al. Effect of using an interactive booklet about childhood respiratory tract infections in primary care consultations on reconsulting and antibiotic prescribing: a cluster randomised controlled trial. Br Med J 2009; 339: b2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Macfarlane JT, Holmes WF, Macfarlane RM. Reducing reconsultations for acute lower respiratory tract illness with an information leaflet: a randomized controlled study of patients in primary care. Br J Gen Pract 1997; 47: 719–22. [PMC free article] [PubMed] [Google Scholar]
- 9. Cals JW, Ament AJ, Hood K, et al. C-reactive protein point of care testing and physician communication skills training for lower respiratory tract infections in general practice: economic evaluation of a cluster randomized trial. J Eval Clin Pract 2011; 17: 1059–69. [DOI] [PubMed] [Google Scholar]
- 10. Bunten A, Hawking M, McNulty C. Patient information can improve antibiotic prescribing. Nurs Pract 2015; 82: 61–3. [Google Scholar]
- 11. NHS England (London Region)/Primary Care Transformation Programme. Transforming Primary Care in London: General Practice A Call to Action. London: NHS England, 2013. [Google Scholar]
- 12. Crouch S, Housden M. Random market sampling. In: Marketing Research for Managers. 3rd edn. Oxford, UK: Butterworth-Heinemann, 2003, pp. 155. [Google Scholar]
- 13. Little RJ, Wu M-M. Models for contingency tables with known margins when target and sampled populations differ. J Am Stat Assoc 1991; 86: 87–95. [Google Scholar]
- 14. Welschen I, Kuyvenhoven M, Hoes A, Verheij T. Antibiotics for acute respiratory tract symptoms: patients’ expectations, GPs’ management and patient satisfaction. Fam Pract 2004; 21: 234–7. [DOI] [PubMed] [Google Scholar]
- 15. van Driel ML, De Sutter A, Deveugele M, et al. Are sore throat patients who hope for antibiotics actually asking for pain relief? Ann Fam Med 2006; 4: 494–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Filipetto FA, Modi DS, Weiss LB, Ciervo CA. Patient knowledge and perception of upper respiratory infections, antibiotic indications and resistance. Patient Prefer Adherence 2008; 2: 35–9. [PMC free article] [PubMed] [Google Scholar]
- 17. Brookes-Howell L, Hood K, Cooper L, et al. Understanding variation in primary medical care: a nine-country qualitative study of clinicians’ accounts of the non-clinical factors that shape antibiotic prescribing decisions for lower respiratory tract infection. BMJ Open 2012; 2: e000796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lopez-Vazquez P, Vazquez-Lago JM, Figueiras A. Misprescription of antibiotics in primary care: a critical systematic review of its determinants. J Eval Clin Pract 2012; 18: 473–84. [DOI] [PubMed] [Google Scholar]
- 19. Gudnadottir U, Fritz J, Zerbel S, et al. Reducing health care-associated infections: patients want to be engaged and learn about infection prevention. Am J Infect Control 2013; 41: 955–8. [DOI] [PubMed] [Google Scholar]
- 20. Hawkings NJ, Wood F, Butler CC. Public attitudes towards bacterial resistance: a qualitative study. J Antimicrob Chemother 2007; 59: 1155–60. [DOI] [PubMed] [Google Scholar]
- 21. McNulty C, Joshi P, Butler CC, et al. Have the public’s expectations for antibiotics for acute uncomplicated respiratory tract infections changed since the H1N1 influenza pandemic? A qualitative interview and quantitative questionnaire study. BMJ Open 2012; 2: e000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hawker JI, Smith S, Smith GE, et al. Trends in antibiotic prescribing in primary care for clinical syndromes subject to national recommendations to reduce antibiotic resistance, UK 1995-2011: analysis of a large database of primary care consultations. J Antimicrob Chemother 2014; 69: 3423–30. [DOI] [PubMed] [Google Scholar]
- 23. McNulty CA, Boyle P, Nichols T, Clappison P, Davey P. Don’t wear me out–the public’s knowledge of and attitudes to antibiotic use. J Antimicrob Chemother 2007; 59: 727–38. [DOI] [PubMed] [Google Scholar]
- 24. Andrews T, Thompson M, Buckley DI, et al. Interventions to influence consulting and antibiotic use for acute respiratory tract infections in children: a systematic review and meta-analysis. PLoS One 2012; 7: e30334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. National Institute for Health and Clinical Excellence. Respiratory Tract Infections—Antibiotic Prescribing. Prescribing of Antibiotics for Self-Limiting Respiratory Tract Infections in Adults and Children in Primary Care. NICE Clinical Guideline 69. http://www.nice.org.uk/guidance/cg69/evidence/full-guideline-196853293 (accessed on 5 February 2016). [PubMed] [Google Scholar]
- 26. TARGET Antibiotics Toolkit. The Royal College of General Practitioners http://www.rcgp.org.uk/clinical-and-research/toolkits/target-antibiotics-toolkit.aspx (accessed on 4 February 2016).