Abstract
Objectives
Pedicle-lengthening osteotomy is a novel surgery for lumbar spinal stenosis (LSS), which achieves substantial enlargement of the spinal canal by expansion of the bilateral pedicle osteotomy sites. Few studies have evaluated the impact of this new surgery on spinal canal volume (SCV) and neural foramen dimension (NFD) in three different types of LSS patients.
Methods
CT scans were performed on 36 LSS patients (12 central canal stenosis (CCS), 12 lateral recess stenosis (LRS), and 12 foraminal stenosis (FS)) at L4-L5, and on 12 normal (control) subjects. Mimics 14.01 workstation was used to reconstruct 3D models of the L4-L5 vertebrae and discs. SCV and NFD were measured after 1 mm, 2 mm, 3 mm, 4 mm, or 5 mm pedicle-lengthening osteotomies at L4 and/or L5. One-way analysis of variance was used to examine between-group differences.
Results
In the intact state, SVC and NFD were significantly larger in the control group compared with the LSS groups (P<0.05). After lengthening at L4, the percentage increase in SCV (per millimetre) was LRS>CCS>FS>Control. After lengthening at L5 and L4-L5, the percentage increase in SCV (per millimetre) was LRS>FS>CCS>Control. After lengthening at L4 and L4-L5, the percentage increase in NFD (per millimetre) was FS>CCS>LRS>Control. After lengthening at L5, the percentage increase in NFD (per millimetre) was CCS>LRS>control>FS.
Conclusions
LRS patients are the most suitable candidates for treatment with pedicle-lengthening osteotomy. Lengthening L4 pedicles produced larger percentage increases in NFD than lengthening L5 pedicles (p < 0.05). Lengthening L4 pedicles may be the most effective option for relieving foraminal compression in LSS patients.
Cite this article: P. Li, L. Qian, W. D. Wu, C. F. Wu, J. Ouyang. Impact of pedicle-lengthening osteotomy on spinal canal volume and neural foramen size in three types of lumbar spinal stenosis. Bone Joint Res 2016;5:239–246. DOI: 10.1302/2046-3758.56.2000469.
Keywords: Pedicle lengthening, Spinal stenosis, Spinal canal volume, Neural foraminal dimension, 3D reconstructions
Article focus
This study aimed to investigate the impact of different pedicle-lengthening osteotomies on spinal canal volume (SCV) and neural foramen dimensions (NFD) in three types of lumbar spinal stenosis (LSS) patients and normal subjects.
The pedicle-lengthening osteotomies performed at L4 and/or L5.
The LSS include central canal stenosis (CCS), lateral recess stenosis (LRS) and foraminal stenosis (FS).
Key messages
LRS patients are the most suitable candidates for treatment with pedicle-lengthening osteotomy.
Lengthening L4 pedicles produced larger percentage increases in NFD than lengthening L5 pedicles (p < 0.05).
Lengthening L4 pedicles may be the most effective option for relieving foraminal compression in LSS patients.
Strengths and limitations
Pedicle-lengthening osteotomy is a new minimally-invasive surgery for lumbar spinal stenosis, which produced larger percentage increases of spinal canal volume and neural foramen dimension in LSS patients than normal subjects.
In the current study, a larger number of normal and LSS patients were considered in order to obtain clinically relevant data.
As this study was performed based on CT data, future controlled comparative studies will be required to more accurately validate Pedicle-lengthening osteotomy and traditional surgical techniques.
Introduction
Lumbar spinal stenosis (LSS) is a common spinal disease in elderly individuals, typically characterised by an anatomic reduction of the lumbar spinal canal volume or intervertebral foramen size.1 Degenerative LSS can involve the central canal, lateral recess, foramina, or any combination of these locations.2 Central canal stenosis (CSS) may result from a decrease in the anteroposterior, transversal, or combined diameters of the canal due to bulging of the intervertebral disc and/or hypertrophy of the facet joints and the ligamentum flavum.3 Lateral recess stenosis (LRS) is caused by decreased disc height, facet joint hypertrophy and/or vertebral endplate osteophytosis.3 Foraminal stenosis can be either anteroposterior, resulting from a combination of disc space narrowing and hypertrophy of the facet joint capsule, and/or vertical, resulting from posterolateral osteophytes protruding into the foramen along with a laterally herniated disc.4 As LSS progresses, degenerative changes reduce the available space for neural elements. This can induce lower back pain, lower extremity pain, and neurogenic claudication.
Symptomatic LSS is the most frequent cause for lumbar spinal surgery in patients older than 65 years.5 Laminectomy with or without lumbar fusion is an effective clinical treatment for patients with symptomatic stenosis.6 Conventional open laminectomy involves removal of parts of the vertebral lamina, ligament flavum and a medial portion of the facet joints to alleviate compression of the neural structures. However, decompression surgery is associated with surgical trauma, may cause post-operative lumbar instability and may require a prolonged hospital stay, which may in turn lead to long-term morbidity.7 These concerns are magnified when treating fragile, elderly patients.
Pedicle-lengthening osteotomy is a new minimally invasive surgery for LSS, which involves lengthening the lumbar pedicles through bilateral percutaneous pedicle osteotomies.8,9 This technique is associated with reduced soft-tissue damage, iatrogenic instability and recovery time compared with conventional surgery.8
Previous studies merely focused on the cross-sectional areas of the spinal canal and neural foramen in normal subjects.9,10 Measurements assessing the cross-sectional area may be inaccurate because they do not objectively reflect compression on the spinal cauda equina and in multi-level situations.11 Furthermore, pre-operative lumbar canal size may be larger in normal subjects than in LSS patients.12 Therefore, we believe that spinal canal volume (SCV) may be the more accurate parameter to evaluate the impact of pedicle-lengthening osteotomy on LSS (Fig. 1).
Fig. 1.

L4 vertebrae before (upper) and after (lower) pedicle-lengthening osteotomy. The volume of the spinal canal is indicated.
This study aimed to investigate the impact of different pedicle-lengthening osteotomies at L4 and/ or L5 on SCV and neural foramen dimensions (NFD) in three types of LSS patients and normal subjects.
Patients and Methods
The study consisted of 36 LSS patients and 12 healthy volunteers who underwent lumbar (L4-L5) computed tomography examination at our medical centre between June 2013 and June 2014. Patients with scoliosis, kyphosis, spondylolisthesis and previous lumbar surgery were excluded. Of the 36 LSS patients, 12 patients (male: female ratio, 7:5; mean age, 62 years; 51 to 78) were diagnosed with L4-L5 central canal stenosis (CCS), 12 patients (male: female ratio, 5:7; mean age, 65 years; 57 to 81) were diagnosed with L4-L5 lateral recess stenosis (LRS), and 12 patients (male: female, 9:3; mean age, 63 years; 53 to 77) were diagnosed with L4-L5 foraminal stenosis (FS). The diagnosis of spinal stenosis was based on the patients’ clinical symptoms and radiologic criteria.13 A total of 12 normal subjects (male: female 8:4; mean age, 36 years; 25 to 50) were randomly sampled from healthy volunteers in whom spiral CT was performed in the same medical centre. Subjects with lumbar spine diseases such as lumbar spine deformity, trauma and lumbar spine degeneration were excluded. The normal subjects served as the control group. Ethical approval was obtained from our Human Research Ethics Committee. All subjects provided written informed consent.
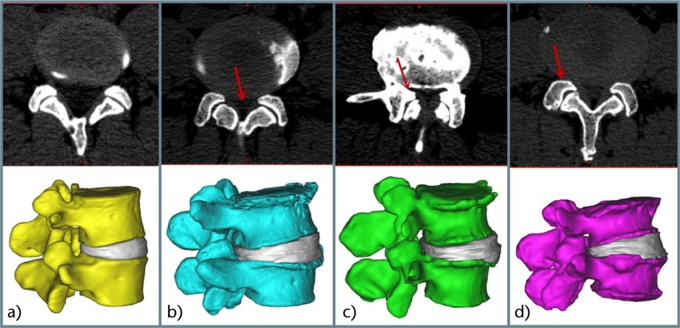
CT scans of the lumbar spine were obtained using a 64-channel LightSpeed scanning system (GE Healthcare, Milwaukee, Wisconsin) from all subjects in a supine and neural position. Primary DICOM images at a voxel resolution of 512×512 pixels and a slice thickness of 0.625 mm were imported into Mimics software v14.01 (Materialise Corp., Leuven, Belgium). An interactive image-processing strategy including “Thresholding”, “Region growing” and “Edit masks” was used to establish the L4-L5 vertebrae and disc models (Fig. 2).
Fig. 2.
Models of L4-L5 vertebrae and discs: a) control; b) central canal stenosis; c) lateral recess stenosis; d) foraminal stenosis.
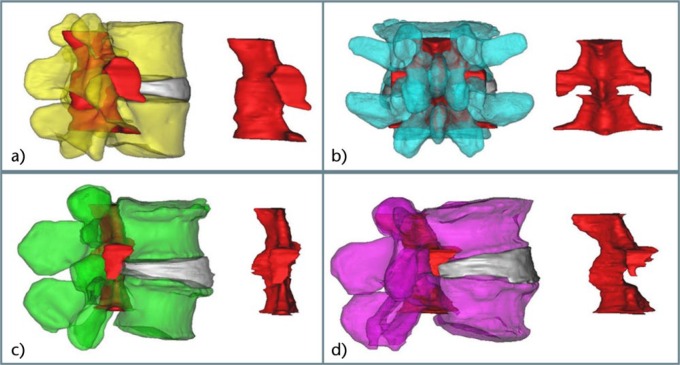
SCV was evaluated in the L4-L5 3D models using “Lasso” under “Multiple slice edit” in Mimics software (Fig. 3). For clinical purposes, the spinal canal was considered to constitute three zones, including a central canal between the medial margins of the facet joints and two lateral canals beneath the facet joints and entering the neural foramen. Accordingly, the dimensions of SCV at L4-L5 were limited laterally by the borders of the central and lateral canals, superiorly by the superior rim of the bilateral L4 pedicles, and inferiorly by the inferior rim of the bilateral L5 pedicles. The dimensions of SCV at the level of the vertebral body were limited anteriorly by the posterior margin of the vertebral body, laterally by the interior margins of the bilateral pedicles, and posteriorly by the anterior margin of the ligamentum flavum. The dimensions of SCV at the level of the intervertebral disc were limited anteriorly by the posterior margin of the intervertebral disc, laterally by the exterior margin of the intervertebral foramen, and posteriorly by the anterior margin of the ligamentum flavum.
Fig. 3.
Spinal canal volume in L4-L5 models: a) control; b) central canal stenosis; c) lateral recess stenosis; d) foraminal stenosis.
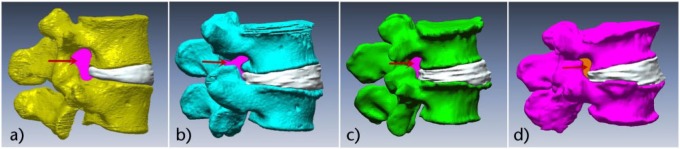
To measure NFD, Rapidform XOS (INUS Technology Inc., Seoul, South Korea) was used to create a sagittal oblique plane through the medial margins of the pedicles at L4 and L5. Subsequently, an enclosed curve was traced along the medial margin of the caudal L4 pedicle, the posterior margins of the L4 vertebral body, L4-L5 disc and L5 vertebral body, the interior margin of the cranial L5 pedicle, the anterior margin of the facet joints, and back along the caudal L4 pedicle. The area of each enclosed curve was defined as the NFD and measured bilaterally (Fig. 4).
Fig. 4.
Neural foraminal dimensions in L4-L5 models: a) control; b) central canal stenosis; c) lateral recess stenosis; d) foraminal stenosis.
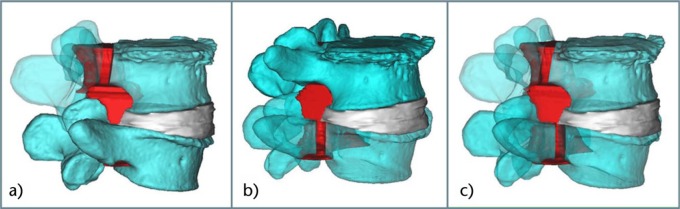
SCV and NFD were measured in the intact state and after the simulated 1 mm, 2 mm, 3 mm, 4 mm, or 5 mm pedicle-lengthening procedures at L4 and/or L5. First, the L4-L5 vertebrae model was modified by cutting the bilateral pedicle bones at the junction of the vertebral body and pedicles. Next, “Reposition” in Mimics software was used to simulate expansion of the bilateral pedicles by 1 mm, 2 mm, 3 mm, 4 mm, or 5 mm. Pedicle-lengthened spine models were established and SCV and NFD were evaluated (Figs 5 and 6). One researcher measured all the data using the Mimics and Rapidform workstation. All parameters were measured by the first author (PL), and the mean was used as the final value.
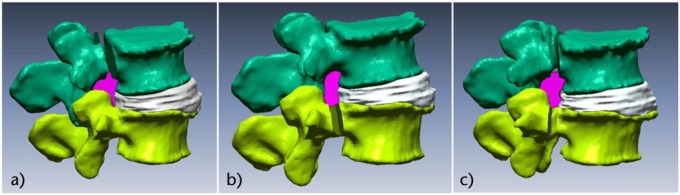
Fig. 5.
Spinal canal volume after simulated pedicle-lengthening at L4 and/or L5: a) pedicle-lengthening at L4; b) pedicle-lengthening at L5; c) pedicle-lengthening at L4 and L5.
Fig. 6.
Neural foraminal dimensions after simulated pedicle-lengthening at L4 and/or L5 levels: a) pedicle-lengthening at L4; b) pedicle-lengthening at L5; c) pedicle-lengthening at L4 and L5.
Data were described as mean and standard deviation (sd). One-way analysis of variance (ANOVA) was used to examine between-group differences. Statistical analysis was performed using the Statistical Package for the Social Sciences v13.0 (SPSS Inc., Chicago, Illinois). Statistical significance was defined as p < 0.05.
Results
Measurements of SCV and NFD in the intact state and after gradual lengthening of pedicles at L4 and/or L5 are shown in Tables i to vi in the Supplementary Material.
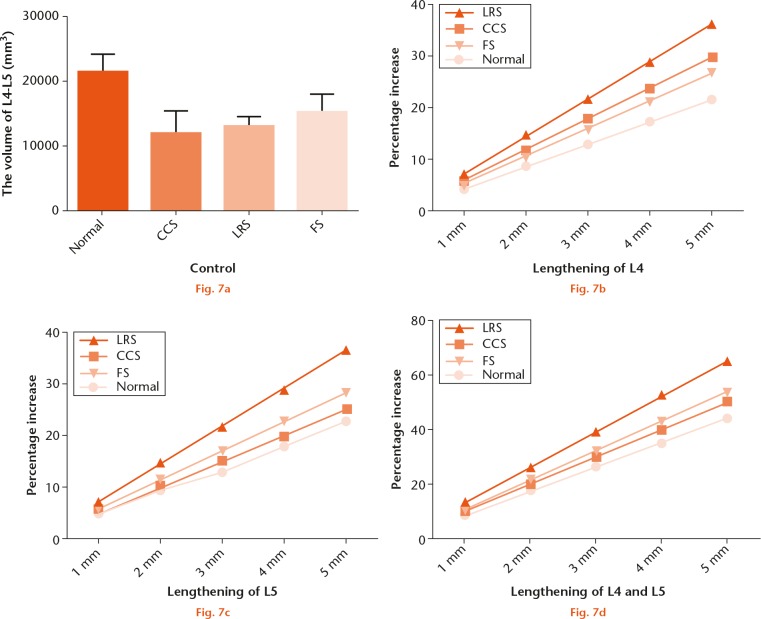
In the intact state, SCV was significantly larger in the control group compared with the LSS groups (p < 0.05, see Fig. 7a). SCV was largest in the control group (mean 21 590.6 mm3 sd 2638.5) compared with the FS group (mean 15 175.7 mm3 sd 2785.3), LRS group (mean 13 032.0 mm3 sd 1583.8), and the CCS group (mean 11 979.5 mm3 sd 3353.1). In all of the lengthened states, the percentage increase in SCV was larger in the LSS groups than it was in the control group (Figs 7b, 7c and 7d). After lengthening at L4, the percentage increase in SCV was LRS>CCS>FS>Control (Fig. 7b). After lengthening at L5 and L4+L5, the percentage increase in SCV was LRS>FS>CCS>Control (Figs 7c and 7d). After lengthening at L4, SCV increased by 4.3%, 5.9%, 7.2%, and 5.3% per millimetre in the control, CCS, LRS, and FS groups, respectively. After lengthening at L5, SCV increased by 4.6%, 5.0%, 7.3%, and 5.7% per millimetre in the control, CCS, LRS, and FS groups, respectively. After lengthening at L4+L5, SCV increased by 8.8%, 10.0%, 13.1%, and 10.8% per millimetre in the control, CCS, LRS, and FS groups, respectively. Lengthening at L5 produced larger percentage increases in SCV compared with lengthening at L4, except in the CSS group. However, the differences were not significant. Lengthening at L4+L5 produced significantly larger percentage increases in SCV compared with lengthening at L4 or L5 alone (p < 0.05).
Measurements of spinal canal volume in the intact state and after 1 mm, 2 mm, 3 mm, 4 mm, or 5 mm pedicle-lengthening at L4 and/or L5: a) the original spinal canal volume (SCV) of control, canal stenosis (CCS), lateral recess stenosis (LRS) and foraminal stenosis (FS) group. SCV was significantly larger in the control group compared with the LSS groups, p < 0.001; b) increased percentage of SCV of control, CCS, LRS and FS group after gradual lengthening the L4 pedicle by 1 mm, 2 mm, 3 mm, 4 mm, 5 mm, the percentage increase was LRS>CCS>FS>Control, p < 0.001 for all lengthening distance; c) increased percentage of SCV of control, CCS, LRS and FS group after gradual lengthening the L5 pedicle by 1 mm, 2 mm, 3 mm, 4 mm, 5 mm. The percentage increase was LRS>FS>CCS>Control, p = 0.003 at 1 mm, p < 0.001 at 2 mm to 5 mm; d) increased percentage of SCV of control, CCS, LRS and FS group after gradual lengthening the L4 and L5 pedicles by 1 mm, 2 mm, 3 mm, 4 mm, 5 mm, the percentage increase was LRS>FS>CCS>Control, p < 0.001 for all lengthening distance.
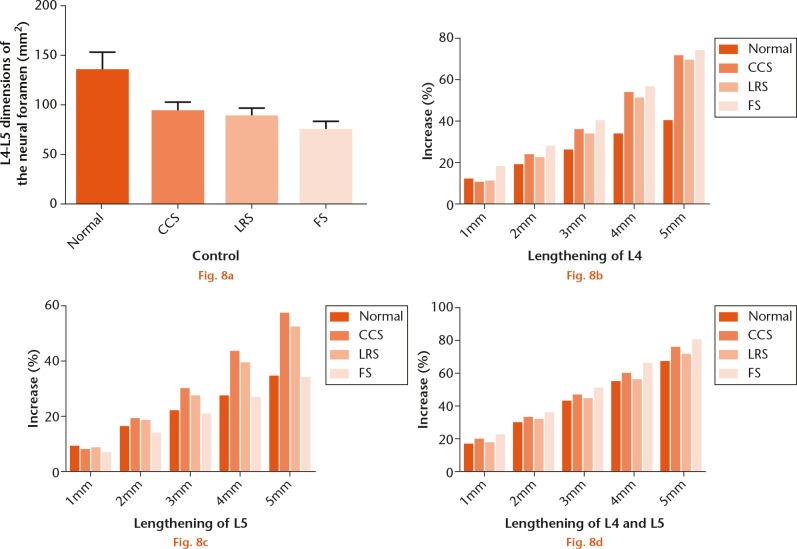
In the intact state, NFD was significantly larger in the control group compared with the LSS groups (p < 0.05, see Fig. 8a). NFD was largest in the control group (mean 134.3 mm2 sd 18.5) compared with the CCS group (mean 93.3 mm2 sd 9.5), the LRS group (mean 87.7 mm2 sd 9.7), and the FS group (mean 74.8 mm2 sd 8.6). In all of L4+L5 lengthened states from 1 mm to 5 mm, the percentage increase in NFD was larger in the LSS groups compared with the control group (Figs 8b, 8c and 8d). After lengthening at L4 by 1 mm, the percentage increase in NFD was FS>control>LRS>CCS. After lengthening at L4 from 2 mm to 5 mm, the percentage increase in NFD was FS>CCS > LRS>control (Fig. 8b). After lengthening at L5 by 1 mm, the percentage increase in NFD was control>LRS>CCS>FS. After lengthening at L5 from 2 mm to 5 mm, the percentage increase in NFD was CCS>LRS>control>FS (Fig. 8c). After lengthening at L4+L5 from 1 mm to 5 mm, the percentage increase in NFD was FS>CCS>LRS>control (Fig. 8d). After lengthening at L4, NFD increased by 8.7%, 12.9%, 12.4%, and 14.3% per millimetre in the control, CCS, LRS, and FS groups, respectively. After lengthening at L5, NFD increased by 7.2%, 10.4%, 9.7%, and 6.7% per millimetre in the control, CCS, LRS, and FS groups, respectively. After lengthening at L4+L5, NFD increased by 14.0%, 15.5%, 14.6%, and 16.9% per millimetre in the control, CCS, LRS, and FS groups, respectively. Lengthening at L4 produced significantly larger percentage increases in NFD compared with lengthening at L5 (p < 0.05). Lengthening at L4+L5 produced significantly larger percentage increases in NFD compared with lengthening at L4 or L5 alone (p < 0.05).
Measurements of neural foraminal dimensions (NFD) in the intact state and after 1 mm, 2 mm, 3 mm, 4 mm, or 5 mm pedicle-lengthening at L4 and/or L5: a) the original NFD of control, canal stenosis (CCS), lateral recess stenosis (LRS) and foraminal stenosis (FS) group, NFD was significantly larger in the control group compared with the three LSS groups, p < 0.001; b) increased percentage of NFD of control, CCS, LRS and FS group after gradual lengthening of the L4 pedicle by 1 mm, 2 mm, 3 mm, 4 mm, 5 mm, the percentage increase was FS>control>LRS>CCS at 1 mm and FS>CCS>LRS>control at 2 mm to 5 mm, p < 0.001 for all lengthening distance; c) increased percentage of NFD of control, CCS, LRS and FS group after gradual lengthening of the L5 pedicle by 1 mm, 2 mm, 3 mm, 4 mm, 5 mm, the percentage increase was control>LRS>CCS>FS at 1 mm and CCS>LRS>control>FS at 2 mm to 5 mm, p = 0.04 at 1 mm, p = 0.001 at 2 mm, p < 0.001 at 3 mm to 5 mm; d) increased percentage of NFD of control, CCS, LRS and FS group after gradual lengthening of the L4 and L5 pedicle by 1 mm, 2 mm, 3 mm, 4 mm, 5 mm, the percentage increase FS>CCS>LRS>control, p < 0.001 at 1 mm, p = 0.045 at 2 mm, p = 0.04 at 3 mm, p = 0.004 at 4 mm, p = 0.006 at 5 mm.
Discussion
Traditional open laminectomy can enlarge the cross-sectional area of the spinal canal, but cannot enlarge the area of the neural foramen. Pedicle-lengthening osteotomy provides a novel strategy for enlarging both the spinal canal and neural foramen in LSS patients. This procedure is carried out under fluoroscopic guidance. Bilateral pedicle osteotomies are performed using a manual bone saw, which cuts the pedicle from inside the pedicle passages at the junction with the vertebral body. Subsequently, two adjustable lengthening implants are positioned across the osteotomy sites. Implant lengthening causes the gaps at the osteotomy sites to expand, leading to an enlarged spinal canal and neural foramen.8,9 The current study investigated the impact of pedicle-lengthening osteotomy on SCV and NFD in three types of LSS patients. We chose the L4-L5 level because this region is most commonly affected by LSS.14
Most previous assessments of LSS have focused on measuring the cross-sectional area or sagittal diameter of the lumbar canal in a 2D axial plane using CT or MRI.15 However, simple measurements of cross-sectional area or a radial line may depend on the thickness of a scan and/or the section angle, which may lead to inaccuracies.16 Such measurements do not reflect compression on neural elements and LSS. It is more accurate to directly measure the volume of the lumbar canal.
Few studies have reported lumbar canal volume measured in cadavers.17 These data represent useful reference values but have little clinical application. There is only one report of lumbar canal volume in normal volunteers18 and none in LSS patients. Yuan et al10 used a 3D digital model to simulate pedicle-lengthening osteotomy in the lumbar spine, and demonstrated that this procedure can significantly enlarge the lumbar canal and the intervertebral foramen. While informative, this 3D digital model was based on one normal subject, and the effects of disc protrusion and ligament hypertrophy on the lumbar canal were not considered. It is conceivable that different results will be obtained in three types of LSS patients, and a larger sample size is needed to confirm statistical significance. In the current study, a larger number of normal and LSS patients was considered in order to obtain clinically relevant data.
A study conducted by Zhang et al19 reported that the mean canal stenosis index after posterior indirect reduction and pedicle screw fixation without laminectomy was 84.8% (sd 7.3%) compared with 32.9% (sd 7.8%) before the operation, which indicated that there is a more than twofold increase of the mean canal stenosis index following the procedure. Other studies conducted by Lee et al20 reported that the ratio increase of cross-sectional spinal canal area was 163.8%. According to the study conducted by Mlyavykh et al,8 lengthening of less than 5 mm with pedicle-lengthening osteotomy could provide favourable clinical results and increase spinal canal volume by 65.2%. This indicates that a smaller increase provides more favourable clinical results in pedicle-lengthening osteotomy compared with more traditional surgery. A 3D-computed tomography study of cervical spinal canal enlargement after en bloc open-door laminoplasty reported that the bony spinal canal volume increased by 45%,21 consistent with our results. However, the pedicle-lengthening osteotomy may cause less nerve adhesion and lumbar instability, as the minimally invasive surgery keeps muscle intact (especially the tissues around the nerve) which in turn may reduce long-term morbidity compared with traditional surgery.
Using a combined CT scanning and 3D modelling technique, we measured SCV and NFD in models of normal subjects and LSS patients after 1 mm, 2 mm, 3 mm, 4 mm, or 5 mm pedicle-lengthening osteotomies at L4 and/or L5. Neural compression can occur in three canals/regions within the lumbar spine: the central canal, which is bordered by the vertebral body, disc, and articular processes; the lateral recess canal, which extends from the dural sac to the lumbar pedicles; and the neural foramen or nerve root canal, which lies below the pedicles.22 Thus, in this study, SCV was measured in each of the three canal regions. Considering the effects of disc protrusion and ligament hypertrophy on SCV, we included the posterior margin of a bulging disc and the anterior margin of the ligamentum flavum in our measurements.
We measured SCV and NFD in control and LSS groups in the intact and lengthened states. In the intact state, SCV was significantly smaller in the LSS groups compared with the control groups. In the lengthened states, there were significantly larger percentage increases in SCV in the LSS groups compared with the control group. Pedicle-lengthening osteotomy produced the largest percentage increases in SCV in the LRS group. There was no consistent trend in percentage increases of the NFD among the LSS groups. Pedicle-lengthening osteotomies produced various effects on SCV and NFD depending on the pedicle level. Lengthening of L5 pedicles produced larger increases in SCV compared with lengthening of L4 pedicles in all groups, except in CCS. In the CCS group, lengthening of L4 pedicles produced a larger percentage increase (mean 5.9%) in SCV compared with lengthening of L5 pedicles (mean 5.0%). Lengthening of L4 pedicles produced larger increases in NFD compared with lengthening of L5 pedicles in all groups, especially in FS. Lengthening L4 and L5 pedicles together produced larger percentage increases than lengthening L4 or L5 pedicles alone. Taken together, these data suggest that LRS patients would benefit from the largest SCV increase, and lengthening L4 pedicles may be the ideal option for relieving neural compression in the foramina.
Currently, few clinical studies on pedicle-lengthening osteotomy have been reported. Kiapour et al9 demonstrated that pedicle-lengthening osteotomy can produce substantial increases in the cross-sectional areas of the spinal canal and neural foramen without significantly changing normal spinal kinematics. Mlyavykh et al8 reported favourable clinical outcomes in 19 LSS patients at 12 months’ follow-up. In that study, the clinical results turned out to be minimal blood loss in all cases; only two to five lightly bloodied 4×4 inch sponges were used to clean the incisional areas and the mean procedure times for a one-level and a two-level procedure were 63 minutes and 118 minutes, respectively. There were no operative complications. However, a clinical study involving 355 patients undergoing open laminectomy reported more significant amounts of blood loss with four patients requiring a blood transfusion.23 In this study the mean operative times of a one-level and a two-level procedure were 94.2 and 109.2 minutes respectively, and 62 patients experienced complications. This indicates that a less morbid clinical result can be obtained after pedicle-lengthening osteotomy rather than traditional laminectomy. Future controlled comparative studies will be required to more accurately validate the two different surgical techniques.
In conclusion, this study investigated the impact of pedicle-lengthening osteotomy on SCV and NFD in patients with three types of LSS (CCS, LRS and FS) compared with normal subjects. Pedicle-lengthening osteotomy produced larger percentage increases in SCV and NFD in LSS patients than in normal subjects. LRS patients may benefit from larger increases in SCV than other LSS groups. Lengthening L4 pedicles produced larger percentage increases in NFD than lengthening L5 pedicles. These data indicate that LRS patients are the most suitable for treatment with pedicle-lengthening osteotomy, and that lengthening L4 pedicles may be the most effective option for relieving foraminal compression in LSS patients.
Footnotes
Author Contribution: P. Li: Reconstruction, Writing the paper.
L. Qian: Performed simulated surgeries, Writing the paper.
W. D. Wu: Measurement.
C. F. Wu: Collection of CT images.
J. Ouyang: Data analysis.
P. Li and L. Qian contributed equally to this work as co-first authers.
ICMJE conflict of interest: None declared.
Supplementary Material
Tables showing spinal canal volume and pedicle-lengthening osteotomy and neural foraminal dimension and pedicle-lengthening osteotomy can be found alongside this paper at http://www.bjr.boneandjoint.org.uk/
Funding Statement
None declared.
References
- 1. de Schepper EI, Overdevest GM, Suri P, et al. Diagnosis of lumbar spinal stenosis: an updated systematic review of the accuracy of diagnostic tests. Spine (Phila Pa 1976) 2013;38:E469-E481. [DOI] [PubMed] [Google Scholar]
- 2. Daffner SD, Wang JC. The pathophysiology and nonsurgical treatment of lumbar spinal stenosis. Instr Course Lect 2009;58:657-668. [PubMed] [Google Scholar]
- 3. Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol 2010;24:253-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jenis LG, An HS. Spine update. Lumbar foraminal stenosis. Spine (Phila Pa 1976) 2000;25:389-394. [DOI] [PubMed] [Google Scholar]
- 5. Andreisek G, Imhof M, Wertli M, et al. A systematic review of semiquantitative and qualitative radiologic criteria for the diagnosis of lumbar spinal stenosis. AJR Am J Roentgenol 2013;201:W735-746. [DOI] [PubMed] [Google Scholar]
- 6. Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine (Phila Pa 1976) 2010;35:1329-1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fredman B, Arinzon Z, Zohar E, et al. Observations on the safety and efficacy of surgical decompression for lumbar spinal stenosis in geriatric patients. Eur Spine J 2002;11:571-574. [DOI] [PubMed] [Google Scholar]
- 8. Mlyavykh S, Ludwig SC, Mobasser JP, et al. Twelve-month results of a clinical pilot study utilizing pedicle-lengthening osteotomy for the treatment of lumbar spinal stenosis. J Neurosurg Spine 2013;18:347-355. [DOI] [PubMed] [Google Scholar]
- 9. Kiapour A, Anderson DG, Spenciner DB, et al. Kinematic effects of a pedicle-lengthening osteotomy for the treatment of lumbar spinal stenosis. J Neurosurg Spine 2012;17:314-320. [DOI] [PubMed] [Google Scholar]
- 10. Yuan C, Zhu H, Song D, et al. Impact and clinical significance of pedicle length on spinal canal and intervertebral foramen area. Int J Clin Exp Med 2014;7:163-169. [PMC free article] [PubMed] [Google Scholar]
- 11. Dong F, Shen C, Jiang S, et al. Measurement of volume-occupying rate of cervical spinal canal and its role in cervical spondylotic myelopathy. Eur Spine J 2013;22:1152-1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sirvanci M, Bhatia M, Ganiyusufoglu KA, et al. Degenerative lumbar spinal stenosis: correlation with Oswestry Disability Index and MR imaging. Eur Spine J 2008;17:679-685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mamisch N, Brumann M, Hodler J, et al. Radiologic criteria for the diagnosis of spinal stenosis: results of a Delphi survey. Radiology 2012;264:174-179. [DOI] [PubMed] [Google Scholar]
- 14. Siebert E, Prüss H, Klingebiel R, et al. Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol 2009;5:392-403. [DOI] [PubMed] [Google Scholar]
- 15. Willén J, Danielson B, Gaulitz A, et al. Dynamic effects on the lumbar spinal canal: axially loaded CT-myelography and MRI in patients with sciatica and/or neurogenic claudication. Spine (Phila Pa 1976) 1997;22:2968-2976. [DOI] [PubMed] [Google Scholar]
- 16. Eubanks BA, Cann CE, Brant-Zawadzki M. CT measurement of the diameter of spinal and other bony canals: effects of section angle and thickness. Radiology 1985;157:243-246. [DOI] [PubMed] [Google Scholar]
- 17. Dai LY, Xu YK, Zhang WM, Zhou ZH. The effect of flexion-extension motion of the lumbar spine on the capacity of the spinal canal. An experimental study. Spine (Phila Pa 1976) 1989;14:523-525. [PubMed] [Google Scholar]
- 18. Miao J, Wang S, Park WM, et al. Segmental spinal canal volume in patients with degenerative spondylolisthesis. Spine J 2013;13:706-712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhang Z, Chen G, Sun J, et al. Posterior indirect reduction and pedicle screw fixation without laminectomy for Denis type B thoracolumbar burst fractures with incomplete neurologic deficit. J Orthop Surg Res 2015;10:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lee S, Srikantha U. Spinous Process splitting Laminectomy: Clinical outcome and Radiological analysis of extent of decompression. Int J Spine Surg 2015;9:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Baba H, Uchida K, Maezawa Y, et al. Three-dimensional computed tomography for evaluation of cervical spinal canal enlargement after en bloc open-door laminoplasty. Spinal Cord 1997;35:674-679. [DOI] [PubMed] [Google Scholar]
- 22. Ciricillo SF, Weinstein PR. Lumbar spinal stenosis. West J Med 1993;158:171-177. [PMC free article] [PubMed] [Google Scholar]
- 23. Nerland US, Jakola AS, Solheim O, et al. Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ 2015;350:h1603. [DOI] [PMC free article] [PubMed] [Google Scholar]