Abstract
Study Objectives:
Real life ocular measures of drowsiness use average blink duration, amplitude and velocity of eyelid movements to reflect drowsiness in drivers. However, averaged data may conceal the variability in duration of eyelid closure episodes, and more prolonged episodes that indicate higher levels of drowsiness. The current study aimed to describe the frequency and duration of prolonged eyelid closure episodes during acute sleep deprivation.
Methods:
Twenty male professional drivers (mean age ± standard deviation = 41.9 ± 8.3 years) were recruited from the Transport Workers Union newsletter and newspaper advertisements in Melbourne, Australia. Each participant underwent 24 hours of sleep deprivation and completed a simulated driving task (AusEd), the Psychomotor Vigilance Task, and the Karolinska Sleepiness Scale. Eyelid closure episodes during the driving task were recorded and analyzed manually from digital video recordings.
Results:
Eyelid closure episodes increased in frequency and duration with a median of zero s/h of eyelid closure after 3 h increasing to 34 s/h after 23 h awake. Eyelid closure episodes were short and infrequent from 3 to 14 h of wakefulness. After 17 h of sleep deprivation, longer and more frequent eyelid closure episodes began to occur. Episodes lasting from 7 seconds up to 18 seconds developed after 20 h of wakefulness. Length of eyelid closure episodes was moderately to highly correlated with the standard deviation of lateral lane position, braking reaction time, crashes, impaired vigilance, and subjective sleepiness.
Conclusions:
The frequency and duration of episodes of prolonged eyelid closure increases during acute sleep deprivation, with very prolonged episodes after 17 hours awake. Automated devices that assess drowsiness using averaged measures of eyelid closure episodes need to be able to detect prolonged eyelid closure episodes that occur during more severe sleep deprivation.
Citation:
Alvaro PK, Jackson ML, Berlowitz DJ, Swann P, Howard ME. Prolonged eyelid closure episodes during sleep deprivation in professional drivers. J Clin Sleep Med 2016;12(8):1099–1103.
Keywords: drowsiness, sleepiness, eyelid closure episodes, professional drivers, averaged data, automated devices
INTRODUCTION
Sleep deprivation and resultant drowsiness are common causes of impaired performance and motor vehicle accidents (MVA) in both the general population and professional drivers.1,2 A lack of real-time drowsiness measures has hampered efforts to develop and assess interventions for sleep deprivation. Objective measures of real-time drowsiness that accurately identify sleepy individuals before and during driving events can potentially prevent MVAs by alerting the driver to significant drowsiness levels and in turn suggest the use of countermeasures, such as a nap or caffeine. They would also provide an opportunity to evaluate the impact of different driving schedules, identifying high risk schedules that result in drowsy driving and assisting with the design of safer work schedules.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Measures of eyelid closure episodes accurately reflect drowsiness in drivers, but most ocular devices of eyelid closure episodes use average blink duration. Averaged data may conceal variability in duration of eyelid closure episodes, and more prolonged episodes indicate more extreme drowsiness.
Study Impact: This study identified increasing frequency and duration of prolonged eyelid closure lasting up to 18 seconds after 17–23 hours of sleep deprivation, both emphasizing the substantial risk of driving after acute sleep deprivation and the necessity for ocular based alertness monitors to detect these prolonged episodes.
Slow, prolonged eyelid closure is associated with drowsiness, and recent studies have suggested that the speed, duration, and amplitude of eyelid closure episodes are promising real-time indicators of drowsiness.3,4 Indeed, automated devices that measure eyelid closure episodes in real time have been developed.3 They rely on averaged values of these eyelid closure metrics rather than identifying individual episodes of prolonged eyelid closure. For example, the percentage of eyelid closure (PERCLOS)5 reflects the proportion of time an eyelid covers more than 80% of the pupil during a 1-min time interval. PERCLOS is associated with increased drowsiness,4 decreased vigilance and psychomotor performance, and lane departures and crashes during simulated driving in sleep deprived drivers.4–8 Similarly, the average blink duration and amplitude and velocity of eyelid movements are related to impaired vigilance, frequent lapses in attention, and real-life adverse driving events.3,9,10 However, average measures could mask the variability in duration of eyelid closure episodes and more prolonged episodes that indicate higher levels of drowsiness. Previous studies have yet to describe the frequency and duration of prolonged eyelid closure episodes during acute sleep deprivation. Such information would inform methods for automated measurement, and hence is the topic of this study. We hypothesized that prolonged episodes of eyelid closure would become more frequent with increasing acute sleep deprivation in professional drivers.
METHODS
Participants
Twenty male professional drivers (mean age ± SD = 41.9 ± 8.3 years) were recruited via the Transport Workers Union newsletter and newspaper advertisements. Each participant must have driven for ≥ 30 h/week for a period > 12 months to be eligible. Participants with contraindications to sleep deprivation, symptoms of excessive sleepiness or a sleep disorder, medical conditions (e.g., depression, stroke, dementia), a history of learning disability, drug abuse, or a brain injury that might affect neuropsychological performance were excluded from the study.11
Protocol
Participants attended a screening session followed by a 24-h test session on a separate day. In the first session, written informed consent was obtained, and the participants were screened against the inclusion criteria and undertook a practice session on the driving task to overcome learning effects. Participants completed a sleep diary for one week before the 24-h test session.
For the second session, participants were instructed to wake at 07:00 and arrive at the laboratory by 08:30 on the morning of the test session following a full night of sleep (7.2 ± 1.4 h) as documented by a sleep diary. They remained awake for 24 h and were continuously monitored by laboratory staff. A test battery including the driving task, the psychomotor vigilance task and the Karolinska Sleepiness Scale was completed 7 times during the 24-h acute sleep deprivation period at 09:00, 12:00, 16:00, 20:00, 24:00, 03:00, and 06:00. Participant sleepiness was recorded immediately after the driving simulation. Participants undertook passive activities in between testing sessions, such as reading or watching videos. They were also prohibited from caffeine consumption on the day of the test session and from smoking for 30 min prior to a test battery. Taxis were provided to and from the laboratory. Participants were reimbursed AU$200 to cover the time they spent involved in the study. This study was approved by the Human Research and Ethics Committee at Austin Health, Melbourne, Victoria.
Outcome Measures
The AusEd driving simulator (AusEd, Woolcock Institute, Sydney, Australia)12 was used to measure driving performance. The drive included a 30-min nighttime drive on a two-lane highway, with standard lane divisions, road edges marked with reflective posts, and a series of curved and straight components. The instructions for drivers were to stay in the center of the left lane (consistent with Australian driving rules) and remain within a 60 to 80 km/h speed on the speedometer. Lateral lane position, variation in speed, braking reaction time (ms), and mean number of crashes (off road, stoppage events, and truck collisions) were recorded. Each drive session contained identical road conditions and truck presentation times. This driving simulation program is sensitive to sleep deprivation and alcohol.13,14
Slow eyelid closure was assessed manually during the simulated driving task via digital video recordings of the face, using infrared light.5 A scorer (MH) scrolled through the video in 0.5-s frames, recording each eyelid closure episodes (80% closure as per PERCLOS) ≥ 1 s and the duration of the episode.5 The scorer was blinded to the participant details, the time and date of the recording and the driving simulation outcomes. The frequency and duration of eyelid closure episodes were calculated for each 30-min driving simulation session.
Reaction time was measured by the Psychomotor Vigilance Task (PVT), a 10-min computer based timed task that involves reacting to a visual stimulus that is presented at varying intervals 10 times per minute.15 Median reaction time and the number of lapses (reaction time > 500 ms), both of which are sensitive to circadian effects and sleep deprivation,13 were recorded for each session. Sustained attention and a rapid stimulus response are required for The PVT and driving a motor vehicle.16,17
The Multivariable Apnea Predictor Questionnaire (MAPQ)18 is a measure of sleep disordered breathing that contains items on age, gender, body mass index, and the frequency of snorting or gasping, loud snoring, and episodes of choking, breathing stopping, or struggling for breath at night. The total scores vary from 0 to 1.0, with higher scores indicating higher probably of sleep disordered breathing. Studies have validated the MAPQ in clinical populations to differentiate between low risk and at least mild risk of sleep disordered breathing, with a cutoff score of 0.5 yielding an acceptable combination of sensitivity (88%) and specificity (55%).18
The Epworth Sleepiness Scale (ESS) is a measure of subjective sleepiness.19 The ESS is an 8-item self-report questionnaire that asks about tendency to fall asleep in different everyday life situations over the past 4 weeks. Total scores range from 0 to 24, with higher scores suggesting higher levels of sleepiness. ESS Scores > 10 suggest clinically significant sleepiness.19
The Karolinska Sleepiness Scale (KSS) is a 9-item self-report measure for subjective sleepiness.20 Scores range from 1 to 9, with lower scores indicated alertness and higher scores indicating sleepiness. The KSS has been validated as a measure of sleepiness against electroencephalography and performance vigilance measures.20,21
Statistical Analysis
Stata 12.0 was used to calculate all statistics. Means and standard deviations were used for demographic variables. Three participants had missing values replaced, because they were too sleepy to complete the final test session, by linear extrapolation and interpolation.22 Log transformations were computed for speed and lateral lane position to produce a normal distribution.11 The duration of eyelid closure episodes lasting ≥ 1.0 s were recorded, grouped into 3-s bins, and the frequency per hour reported for each drive. Seconds per hour of eyelid closure was also calculated for each drive. The Friedman test was used to assess the effect of hours awake on the rate of slow eyelid closure. The relationship between seconds per hour of eyelid closure, driving performance, and vigilance measures and subjective sleepiness was assessed using the Spearman correlation.
RESULTS
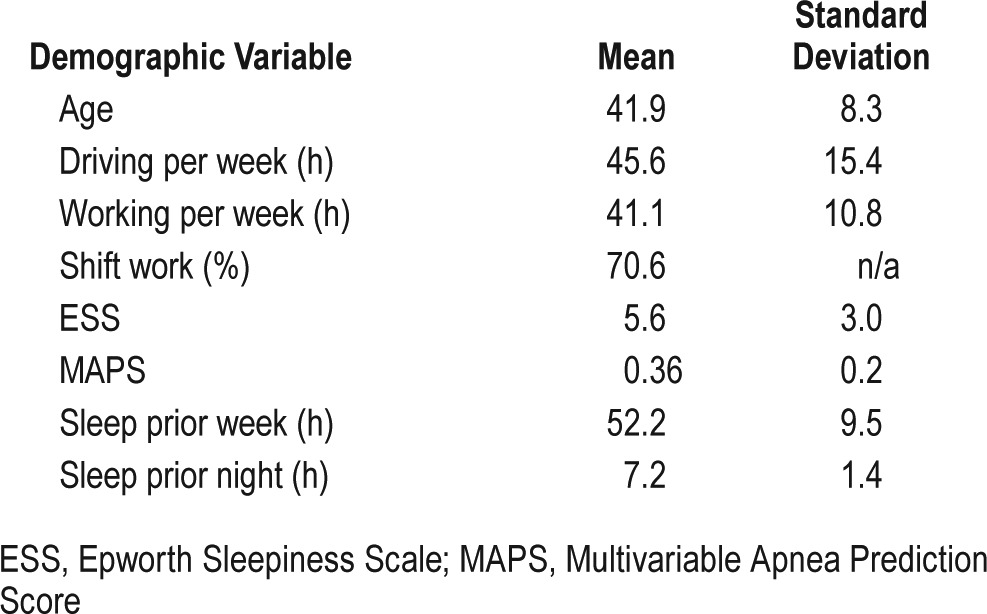
The professional drivers were on average 42 years old (SD = 8.3), drove 45 h per week and worked 41 h per week. Most worked shift work, and the average ESS and MAPS scores did not indicate clinically significant symptoms of sleepiness or sleep apnea. They averaged 52 h of sleep in the previous week, and 7.2 h of sleep the night before the study. Table 1 displays the demographic information for the professional drivers.
Table 1.
Demographic information of professional drivers.
Infrequent episodes of eyelid closure were evident from 3 to 14 h of wakefulness, mainly of short duration between 1 to 3 s (Figures 1 and 2). There was a progressive increase towards longer and more frequent eyelid closure episodes after 17 h awake, where 6-s episodes became common. Episodes lasting from 7 s up to 18 s developed after 20 h of wakefulness (Figure 1). Increased frequency of eyelid closure was significantly correlated with the standard deviation of lateral lane position (r = 0.60, p < 0.01), braking reaction time (r = 0.50, p < 0.01), and crashes (r = 0.43, p < 0.01). There were also moderate correlations with impaired vigilance and subjective sleepiness (Table 2).
Figure 1. Frequency of eyelid closure episodes by duration of time (hours) awake.
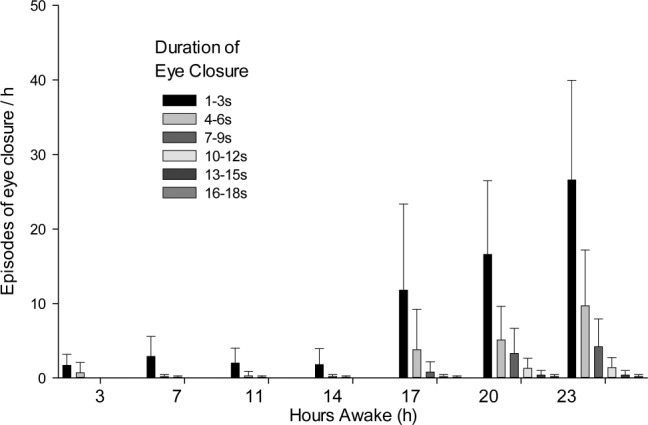
Figure 2. Slow eyelid closure compared to hours awake.

Table 2.
Correlations between slow eyelid closure, performance and subjective sleepiness.
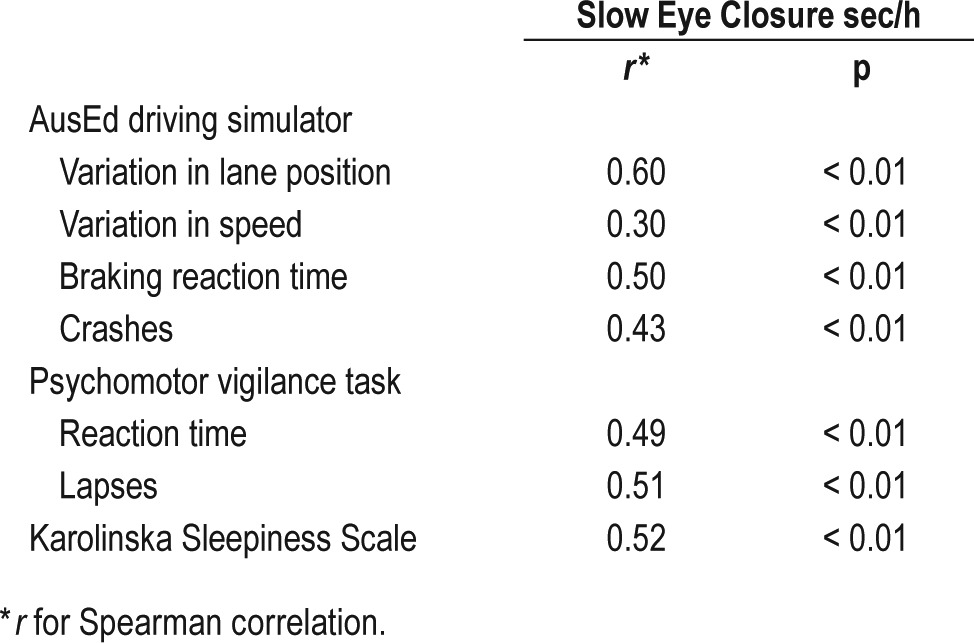
Figure 2 shows slow eye closure (seconds per hour) during each driving session compared to hours awake, and the box plots for the outliers at the 90th, 75th, 50th, 25th, and 10th percentiles. The Friedman test demonstrated an effect of hours awake on the rate of slow eyelid closure, χ2 = 64.1, p < 0.01.
DISCUSSION
This study found that episodes of prolonged eyelid closure were infrequent during the first 14 hours of sleep deprivation, but spiked and continued to increase in both duration and frequency after 17 hours of sleep deprivation, lasting much longer than previously suggested from automated measures.3,23 The changes in prolonged eyelid closure reflect previously documented decrements in behavioral performance and increased subjective sleepiness during acute sleep deprivation,23 and were related to impaired driving performance and vigilance in this study.
The changes in eyelid closure likely resulted from the combined effects of accumulating homeostatic and circadian sleep pressure due to acute sleep deprivation that continued into and beyond the circadian nadir. Such changes likely reflect increased alpha and theta activity from wakefulness on an electroencephalogram (EEG).24 The findings were unlikely to be due to a sleep disorder or previous sleep restriction, as professional drivers with obstructive sleep apnea and high levels of self-reported sleepiness were excluded from the study, and each participant reported over seven hours of sleep the morning before participation.11 The findings suggest that severe physiological impairment can occur during acute sleep deprivation even in those without underlying sleep disorders or prior sleep restriction, a situation that is commonly faced by transport drivers working shift work.2
Episodes of eyelid closure while driving were longer than previously suggested by averaged data from automated devices, particularly after 17 hours of sleep deprivation.3,23 Consequently, while the results support the pursuit of simple automated methods for measuring ocular movements to assess and monitor drowsiness, they suggest that averaged data are influenced by a large range of eyelid closure episode length, particularly during extended sleep deprivation. Given the low variability in duration and frequency of eye closure episodes before but high variability after 17 hours of wakefulness, averaged measures of eyelid closure episodes may be useful during shorter periods of sleep deprivation but may fail to detect the true magnitude of eyelid closure episodes, and hence severity, of drowsiness after sleep deprivation of over 17 hours. Indeed, sleep-related driving events are positively and strongly associated with higher maximum blink durations in real-life settings.10
The increased frequency of prolonged eyelid closure episodes after 17 hours awake is particularly important given that it takes less than three seconds to run off the road when driving at approximately 100 km per hour.25 These results enhance our understanding of the mechanisms underlying impaired vigilance and attention in professional and nonprofessional drivers26,27 and the associated crash risk. They suggest that automated devices for drowsiness detection based on ocular measures should be capable of detecting discrete and prolonged episodes of eyelid closure, while acknowledging that other ocular measures may detect more subtle signs of drowsiness. The results support trials of devices that can accurately measure eyelid movements to monitor drowsiness in drivers. Trials need to demonstrate accuracy in field settings and the efficacy of devices for changing driver behavior and reducing risk.28 Devices that measure fatigue have often been released before scientific evaluation has determined their accuracy.29 Dawson et al.28 suggest a due diligence guideline to ensure drowsiness detection devices are validated before commercial use including: independent peer-reviewed, laboratory studies that validate the measure (e.g., eyelid closure episode); determination of cutoff scores for dangerously high levels of drowsiness; and finally, devices should be validated in field studies, including evaluating their impact on relevant occupational adverse events such as crashes.
A potential limitation of this study is the questionable applicability to nonprofessional drivers, as scholars have argued that professional drivers self-select to become more resistant to sleep deprivation.30 However, recent studies have found no difference in measures of sleepiness and driving performance between professional and nonprofessional drivers during sleep deprivation.11 Given this it is likely that eyelid closure episodes in sleep deprived nonprofessional drivers are likely to be at least as long as those in professional drivers. Confirming these changes in nonprofessional drivers would help gauge the generalization of these results.
The current study found that episodes of very prolonged eyelid closure were more frequent and prolonged when driving after being awake for 17 hours, with episodes of eyelid closure as long as 18 seconds, while prolonged episodes were much less frequent up to 14 hours of wakefulness. The results support restricting shift duration for professional drivers to avoid driving after prolonged periods of wake. Furthermore, the results suggest that while averaged measures of eyelid closure episodes can accurately reflect drowsiness in less sleep deprived individuals, automated devices should also be capable of detecting prolonged eyelid closure episodes that occur during more severe sleep deprivation. Trials are required to demonstrate the accuracy of such devices in field settings, and whether they provide the impetus for drivers to take preventive measures to avoid drowsy driving and appropriate countermeasures when they become impaired.
DISCLOSURE STATEMENT
This was not an industry supported study. This study was supported by a grant from Vic Roads, Melbourne, Australia. Dr. Berlowitz has recived use of equipment from ResMed. The other authors have indicated no financial conflicts of interest. No off-label or investigational use was reported by the authors. This work was performed at the Institution for Breathing and Sleep, Melbourne, Australia.
ACKNOWLEDGMENTS
The authors thank Dr. David Joffe and colleagues for providing the AusEd software and Dr John Gora for his assistance with collecting the data.
ABBREVIATIONS
- ESS
Epworth Sleepiness Scale
- h
hour(s)
- km
kilometer(s)
- KSS
Karolinska Sleepiness Scale
- MAPQ, Multivariable Apnea Prediction Questionniare min
minute(s)
- MVA
motor vehicle accident
- PERCLOS
percent of time with eyelids closed
- PVT
Psychomotor Vigilance Task
- s
second(s)
- SD
standard deviation
REFERENCES
- 1.Connor J, Norton R, Ameratunga S, Robinson E, Wigmore B, Jackson R. Prevalence of driver sleepiness in a random population-based sample of car driving. Sleep. 2001;24:688–94. doi: 10.1093/sleep/24.6.688. [DOI] [PubMed] [Google Scholar]
- 2.Howard ME, Desai AV, Grunstein RR, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–21. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- 3.Wilkinson VE, Jackson ML, Westlake J, et al. The accuracy of eyelid movement parameters for drowsiness detection. J Clin Sleep Med. 2013;9:1315–24. doi: 10.5664/jcsm.3278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson ML, Kennedy GA, Clarke C, et al. The utility of automated measures of ocular metrics for detecting driver drowsiness during extended wakefulness. Accid Anal Prev. 2016;87:127–33. doi: 10.1016/j.aap.2015.11.033. [DOI] [PubMed] [Google Scholar]
- 5.Wierwille WW, Ellsworth LA. Evaluation of driver drowsiness by trained raters. Accid Anal Prev. 1994;26:571–81. doi: 10.1016/0001-4575(94)90019-1. [DOI] [PubMed] [Google Scholar]
- 6.Jackson ML, Raj S, Croft RJ, et al. Slow eyelid closure as a measure of driver drowsiness and its relationship to performance. Traffic Inj Prev. 2016;17:251–7. doi: 10.1080/15389588.2015.1055327. [DOI] [PubMed] [Google Scholar]
- 7.Chua ECP, Yeo SC, Lee ITG, et al. Sustained attention performance during sleep deprivation associates with instability in behavior and physiologic measures at baseline. Sleep. 2014;37:27–39. doi: 10.5665/sleep.3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wierwille W. Historical perspective on slow eyelid closure: whence PERCLOS?. Ocular Measures of Driver Alertness: Technical Conference Proceedings; April 26-27, 1999; Herndon, Virginia: Transportation Safety Associates; 1999. [Google Scholar]
- 9.Anderson C, Chang AM, Sullivan JP, Ronda JM, Czeisler CA. Assessment of drowsiness based on ocular parameters detected by infrared reflectance oculography. J Clin Sleep Med. 2013;9:907–20. doi: 10.5664/jcsm.2992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ftouni S, Sletten TL, Howard M, et al. Objective and subjective measures of sleepiness, and their associations with on-road driving events in shift workers. J Sleep Res. 2013;22:58–69. doi: 10.1111/j.1365-2869.2012.01038.x. [DOI] [PubMed] [Google Scholar]
- 11.Howard ME, Jackson ML, Swann P, Berlowitz DJ, Grunstein RR, Pierce RJ. Deterioration in driving performance during sleep deprivation is similar in professional and nonprofessional drivers. Traffic Inj Prev. 2014;15:132–7. doi: 10.1080/15389588.2013.800637. [DOI] [PubMed] [Google Scholar]
- 12.Desai AV, Wilsmore B, Bartlett DJ, et al. The utility of the AusEd driving simulator in the clinical assessment of driver fatigue. Behav Res Methods. 2007;39:673–81. doi: 10.3758/bf03193039. [DOI] [PubMed] [Google Scholar]
- 13.Howard ME, Jackson ML, Kennedy GA, Swann P, Barnes M, Pierce RJ. The interactive effects of extended wakefulness and low-dose alcohol on simulated driving and vigilance. Sleep. 2007;30:1334–40. doi: 10.1093/sleep/30.10.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vakulin A, Baulk SD, Catcheside PG, et al. Effects of moderate sleep deprivation and low-dose alcohol on driving simulator performance and perception in young men. Sleep. 2007;30:1327–33. doi: 10.1093/sleep/30.10.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dinges DF, Powell JW. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav Res Methods Instrum Comput. 1985;17:652–5. [Google Scholar]
- 16.Dorrian J, Rogers NL, Dinges DF. Psychomotor vigilance performance: neurocognitive assay sensitive to sleep loss. In: Kushida C, editor. Sleep deprivation. Clinical issues, pharmacology, and sleep loss effects. New York: Marcel Dekker; 2005. pp. 39–70. [Google Scholar]
- 17.Jackson ML, Croft RJ, Kennedy GA, Owens K, Howard ME. Cognitive components of simulated driving performance: sleep loss effects and predictors. Accid Anal Prev. 2013;50:438–44. doi: 10.1016/j.aap.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 18.Maislin G, Pack AI, Kribbs NB, et al. A survey screen for prediction of apnea. Sleep. 1995;18:158–66. doi: 10.1093/sleep/18.3.158. [DOI] [PubMed] [Google Scholar]
- 19.Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 20.Åkerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosci. 1990;52:29–37. doi: 10.3109/00207459008994241. [DOI] [PubMed] [Google Scholar]
- 21.Kaida K, Takahashi M, Åkerstedt T, et al. Validation of the Karolinska sleepiness scale against performance and EEG variables. Clin Neurophysiol. 2006;117:1574–81. doi: 10.1016/j.clinph.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 22.Hair J, Anderson R, Tatham R, Black W. Multivariate data analysis. 5th ed. New Jersey: Prentice-Hall; 1984. [Google Scholar]
- 23.Gillberg M, Kecklund G, Akerstedt T. Relations between performance and subjective ratings of sleepiness during a night awake. Sleep. 1994;17:236–41. doi: 10.1093/sleep/17.3.236. [DOI] [PubMed] [Google Scholar]
- 24.Strijkstra AM, Beersma DGM, Drayer B, Halbesma N, Daan S. Subjective sleepiness correlates negatively with global alpha (8-12 Hz) and positively with central frontal theta (4-8 Hz) frequencies in the human resting awake electroencephalogram. Neurosci Lett. 2003;340:17–20. doi: 10.1016/s0304-3940(03)00033-8. [DOI] [PubMed] [Google Scholar]
- 25.Lisper HO, Laurell H, Van Loon J. Relation between time to falling asleep behind the wheel on a closed track and changes in subsidiary reaction time during prolonged driving on a motorway. Ergonomics. 1986;29:445–53. doi: 10.1080/00140138608968278. [DOI] [PubMed] [Google Scholar]
- 26.Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 27.Jackson ML, Croft RJ, Owens K, et al. The effect of acute sleep deprivation on visual evoked potentials in professional drivers. Sleep. 2008;31:1261–9. [PMC free article] [PubMed] [Google Scholar]
- 28.Dawson D, Searle AK, Paterson JL. Look before you (s)leep: evaluating the use of fatigue detection technologies within a fatigue risk management system for the road transport industry. Sleep Med Rev. 2014;18:141–52. doi: 10.1016/j.smrv.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 29.Dawson D. Validation in the context of commercialization: the white rabbit effect. Sleep Med. 2011;12:205–6. doi: 10.1016/j.sleep.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 30.Williamson AM, Feyer AM, Friswell R. Melbourne, Victoria, Australia: National Transport Commission; 2004. Fatigue and performance in heavy truck drivers working day shift, night shift or rotating shifts. [Google Scholar]


