Abstract
Sleep-related abnormal sexual behaviors (sexsomnia) are classified as a subtype of NREM sleep parasomnias. Sexsomnia has been reported as part of parasomnia overlap disorder (POD) in two other patients. We present the case of a 42-year-old male patient with video-polysomnography (vPSG) documented POD. The patient had sleepwalking, sleep-related eating, confusional arousals, sexsomnia, sleeptalking, and REM sleep behavior disorder (RBD). Confusional arousals and RBD were documented during the vPSG. This case had the added complexity of obstructive sleep apnea (OSA) playing a role in sleepwalking and sleep related eating, with good response to nasal continuous positive airway pressure (nCPAP). The sexsomnia did not respond to nCPAP but responded substantially to bedtime clonazepam therapy.
Citation:
Soca R, Keenan JC, Schenck CH. Parasomnia overlap disorder with sexual behaviors during sleep in a patient with obstructive sleep apnea. J Clin Sleep Med 2016;12(8):1189–1191.
Keywords: parasomnia overlap disorder, sexsomnia, sleepwalking, REM sleep behavior disorder
INTRODUCTION
Sleep-related abnormal sexual behaviors (sexsomnia, sleep-sex) are classified as a subtype of NREM parasomnias in the International Classification of Sleep Disorders, Third Edition.1 These sexual behaviors often emerge late in the course of a longstanding parasomnia history, and can be associated with obstructive sleep apnea (OSA) triggering confusional arousals with sexual behaviors.2,3 Nasal continuous positive airway pressure therapy (nCPAP) has been reported to control the sexsomnia as well as the OSA.2,3 Sexsomnia has been reported in two cases of parasomnia overlap disorder (POD),4 which consists of REM sleep behavior disorder (RBD) and a concurrent NREM sleep parasomnia.1 In these two reported cases, sexsomnia was one of five parasomnias affecting each patient.4 We present a third case of POD with sexsomnia as one of five parasomnias with the added complexity of severe OSA that also played a role in promoting two of the parasomnias.
REPORT OF CASE
A 42-year-old male presented due to “abnormal activity at night.” The patient first noticed these behaviors 7 to 10 years previously. In the morning, he would find food left out in the kitchen without recalling eating. Simultaneously he began to have witnessed sleepwalking episodes without any food consumption. These behaviors were intermittent, and he did not seek medical attention.
Concurrently he began talking during his sleep. The content was coherent but initially inappropriate for context and gradually developed sexual connotation 3 to 5 years prior to presentation. A bed partner told him that he was attempting to initiate sexual activities during sleep. With the exception of evident snoring, these activities resembled his usual wakeful sexual encounters.
Around the time of onset of his sexual behaviors, he was diagnosed with severe OSA (AHI = 41) and prescribed nCPAP of 10 cwp. His sleepwalking and sleep eating episodes improved substantially after using nCPAP; the nocturnal sexual activities did not change.
At the time of evaluation in the sleep clinic, the patient was having sexual episodes 4 to 5 nights per week. The most common activity was masturbation. He did not recall dreams with any sexual connotation. After becoming aware of an episode, he was able to resume sleep easily. He never achieved orgasm during sleep, nor did he continue masturbating after awakening, but rather he felt sleepy and annoyed.
Past medical history included generalized anxiety disorder, alcohol abuse, irritable bowel syndrome, arthralgias, esophageal reflux, type 2 diabetes, gout, and hypertension. There was no history of parasomnias during childhood. The alcohol abuse preceded any of the parasomnias and had resolved by the time he started having his first sleep symptoms. There was no history of drug abuse. His current medications were allopurinol, aspirin, vitamin D3, valproic acid, glipizide, metformin, ramipril, and liraglutide.
Physical exam was unremarkable. Coordination was normal. There were no tremors, cogwheeling, or any other parkinsonian signs.
Video Polysomnogram
vPSG was conducted with the prescribed nCPAP settings being utilized. Results from vPSG are summarized below:
There were no respiratory events during the night (AHI = 0)
Total recording time: 437.0 minutes
Total sleep time: 382.5 minutes
Sleep onset latency: 11 minutes
REM onset latency: 179 minutes
N1 = 5.4%, N2 = 71.1%, N3 = 18.4%, REM = 5.1%
PLM index: 0
Arousal index: 6.0
There were two notable parasomnia findings during the vPSG:
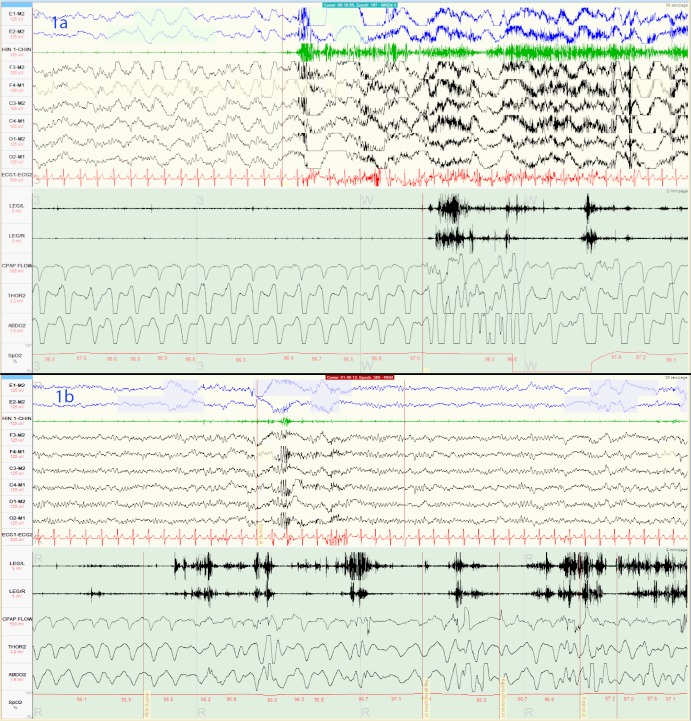
An arousal out of stage N3 sleep during which the patient moved his legs violently (Figure 1A)
Muscle tone was overall increased during stage REM sleep. There were several episodes of yelling profanities and kicking his legs during stage REM sleep (Figure 1B) During the epochs preceding these RBD events, there was no evidence of upper airway obstruction.
Figure 1.
(A) There is an abrupt arousal out of stage N3 sleep followed by prominent phasic EMG leg activity associated with vigorous bilateral leg kicking. (B) Stage REM epoch showing prominent excessive phasic EMG leg twitching associated with vigorous leg kicking. The heart rate is not increased despite the vigorous leg movements, which is typical for RBD, and in contrast to NREM arousal parasomnias. Chin atonia is generally preserved in this tracing.
Treatment
The patient was prescribed clonazepam 0.5 mg at bedtime, and the frequency of sexual episodes was reduced to 1–2 nights per week from a baseline of 4–5 nights per week. The nature of the sexual episodes remained the same (masturbation). He had a single episode of sleepwalking in the six months after treatment was initiated. A higher dose of clonazepam caused intolerable daytime sleepiness.
DISCUSSION
This is a patient with severe obstructive sleep apnea fully controlled with nCPAP who reported a history of five NREM and REM sleep parasomnias during the previous 8–10 years. His parasomnias included: RBD, sleepwalking, sleep-related eating, sleeptalking, and sexsomnia. The two cases reported by Cicolin et al. are the only other known cases of patients presenting with POD, and they each had a total of 5 parasomnias4; our case with POD also had five parasomnias, including sexsomnia, as well as the added complexity of severe obstructive sleep apnea that was promoting two of the parasomnias— sleepwalking and sleep-related eating.
In this case, POD was confirmed by vPSG with parasomnia behaviors emerging from both N3 sleep and REM sleep, including the rare finding of violent RBD leg kicking in a patient without any PLMs. Control of OSA comorbid with SW with nCPAP resulted in a substantial decrease in the frequency of SW (and sleep-related eating) in this patient, which has previously been documented in a large series of SW patients with OSA.5 Treatment of OSA, however, did not improve the sexsomnia. This is the first published report of a patient with sexsomnia and OSA in whom effective treatment of OSA did not also improve the sexsomnia; all other published cases had complete resolution.2,6 We hypothesize that the abnormal arousal phenomena, apart from OSA, responsible for NREM parasomnias was the basis for this patient's sexsomnia, which responded substantially to bedtime clonazepam therapy, closely corresponding to previously reported cases of sexsomnia with NREM parasomnias.2 However, the lack of sexual behaviors during vPSG does not allow for a definitive pathophysiologic understanding of the sexsomnia in this case.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest. This manuscript mentions the off-label use of clonazepam for treating parasomnias. However, the use of this drug for treating parasomnias is considered to be an accepted standard of care in the field of sleep medicine.
ABBREVIATIONS
- nCPAP
nasal continuous positive airway pressure
- OSA
obstructive sleep apnea
- POD
parasomnia overlap disorder
- RBD
REM sleep behavior disorder
- vPSG
video polysomnography
REFERENCES
- 1.American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 2.Schenck CH, Arnulf I, Mahowald MW. Sleep and sex: what can go wrong? A review of the literature on sleep related disorders and abnormal sexual behaviors and experiences. Sleep. 2007;30:683–702. doi: 10.1093/sleep/30.6.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schenck CH, Mahowald MW. Parasomnias associated with sleep-disordered breathing and its therapy, including sexsomnia as a recently recognized parasomnia. Somnology. 2008;12:38–49. [Google Scholar]
- 4.Cicolin A, Tribolo A, Giordano A, et al. Sexual behaviors during sleep associated with polysomnographically confirmed parasomnia overlap disorder. Sleep Med. 2011;12:523–8. doi: 10.1016/j.sleep.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Guilleminault C, Kirisoglu C, Bao G, Arias V, Chan A, Li KK. Adult chronic sleepwalking and its treatment based on polysomnography. Brain. 2005;128:1062–9. doi: 10.1093/brain/awh481. [DOI] [PubMed] [Google Scholar]
- 6.Schenck CH. Update on sexsomnia, sleep related sexual seizures, and forensic implications. NeuroQuantology. 2015;13:518–41. [Google Scholar]